Содержание
- 2. General characteristics The disease typically follows a biphasic pattern in 72–87% of patients and the median
- 3. TBE is caused by tick-borne encephalitis virus, a member of the genus Flavivirus in the family
- 4. TRANSMISSION Sheep ticks (Ixodes ricinus), such as this engorged female, transmit the disease It is transmitted
- 6. Transmission
- 7. Epidemiology As of 2011, the disease was most common in Central and Eastern Europe, and Northern
- 8. Treatment The disease is incurable once manifested, so there is no specific drug therapy for TBE.
- 10. Clinical Signs Canine TBE The incubation period for canine TBE in most cases is between 7
- 11. Human Tick Paralysis In humans, tick paralysis is most likely to be seen in children. The
- 12. A recent CDC report showed that vector-borne diseases -- those transmitted by ticks, mosquitoes, and fleas
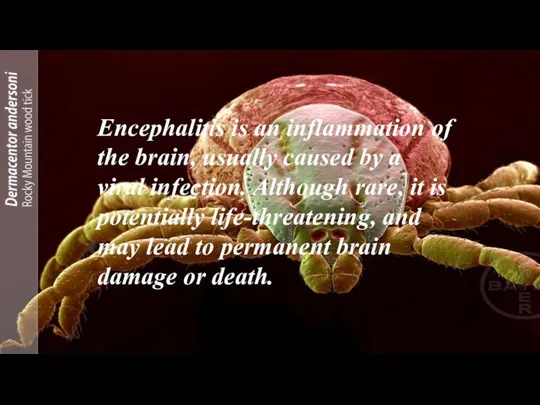
- 13. Encephalitis is an inflammation of the brain, usually caused by a viral infection. Although rare, it
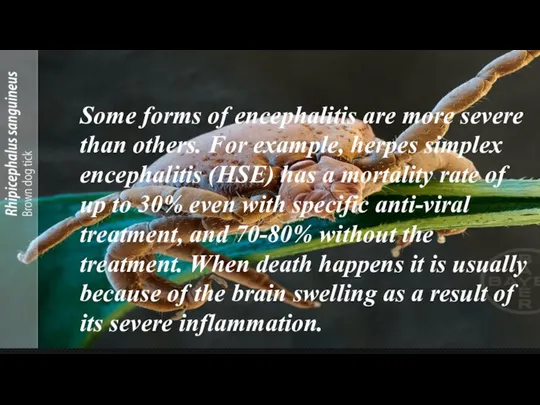
- 14. Some forms of encephalitis are more severe than others. For example, herpes simplex encephalitis (HSE) has
- 15. Lyme encephalopathy is a rare neuropsychiatric disorder, predominantly affecting memory and concentration [3–7]. Other associated symptoms
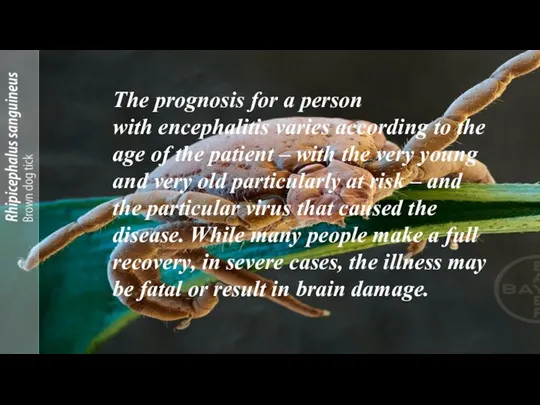
- 16. The prognosis for a person with encephalitis varies according to the age of the patient –
- 17. The contagious period and incubation period for encephalitis depends on the underlying cause of encephalitis. For
- 18. LINKS AND REFRENCES https://youtu.be/5bEimiIZ9dA https://youtu.be/Bv3hQZVtE6Y https://youtu.be/ENmVXtwsKE8
- 19. Further information Edlow JA, McGillicuddy DC: Tick paralysis. Inf Dis Clin North Am. 2008, 22, 397-414
- 21. Скачать презентацию
General characteristics
The disease typically follows a biphasic pattern in 72–87% of
General characteristics
The disease typically follows a biphasic pattern in 72–87% of
In dogs, the disease also manifests as a neurological disorder with signs varying from tremors to seizures and death.[3]
In ruminants, neurological disease is also present, and animals may refuse to eat, appear lethargic, and also develop respiratory signs.
TBE is caused by tick-borne encephalitis virus, a member of the genus Flavivirus in
TBE is caused by tick-borne encephalitis virus, a member of the genus Flavivirus in
Russia and Europe report about 5,000–7,000 human cases annually.[1][8]
The former Soviet Union conducted research on tick-borne diseases, including the TBE viruses
Causes
TRANSMISSION
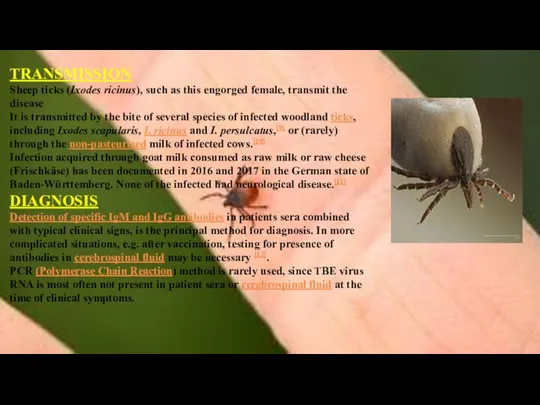
Sheep ticks (Ixodes ricinus), such as this engorged female, transmit the
TRANSMISSION
Sheep ticks (Ixodes ricinus), such as this engorged female, transmit the
It is transmitted by the bite of several species of infected woodland ticks, including Ixodes scapularis, I. ricinus and I. persulcatus,[9] or (rarely) through the non-pasteurized milk of infected cows.[10]
Infection acquired through goat milk consumed as raw milk or raw cheese (Frischkäse) has been documented in 2016 and 2017 in the German state of Baden-Württemberg. None of the infected had neurological disease.[11]
DIAGNOSIS
Detection of specific IgM and IgG antibodies in patients sera combined with typical clinical signs, is the principal method for diagnosis. In more complicated situations, e.g. after vaccination, testing for presence of antibodies in cerebrospinal fluid may be necessary [12].
PCR (Polymerase Chain Reaction) method is rarely used, since TBE virus RNA is most often not present in patient sera or cerebrospinal fluid at the time of clinical symptoms.
Transmission
Transmission
Epidemiology
As of 2011, the disease was most common in Central and Eastern Europe, and
Epidemiology
As of 2011, the disease was most common in Central and Eastern Europe, and
In Germany, during the 2010s, there have been a minimum of 95 (2012) and a maximum of 584 cases (2018) of TBE (or FSME as it is known in German). More than half of the reported cases from 2019 had meningitis, encephalitis or myelitis. The risk of infection was noted to be increasing with age, especially in people older than 40 years and it was greater in men than women. Most cases were acquired in Bavaria (46 %) and Baden-Württemberg (37%), much less in Saxonia, Hesse, Niedersachsen and other states. Altogether 164 Landkreise are designated FSME-risk areas, including all of Baden-Württemberg except for the city of Heilbronn.[11]
In Sweden, most cases of TBE occur in a band running from Stockholm to the west, especially around lakes and the nearby region of the Baltic sea.[18][19] It reflects the greater population involved in outdoor activities in these areas. Overall, for Europe, the estimated risk is roughly 1 case per 10,000 human-months of woodland activity. Although in some regions of Russia and Slovenia, the prevalence of cases can be as high as 70 cases per 100,000 people per year. [17][20] Travelers to endemic regions do not often become cases, with only 5 cases reported among U.S. travelers returning from Eurasia between 2000 and 2011, a rate so low that as of 2016 the U.S. Centers for Disease Control and Prevention recommended vaccination only for those who will be extensively exposed in high risk areas.[21]
Treatment
The disease is incurable once manifested, so there is no specific drug
Treatment
The disease is incurable once manifested, so there is no specific drug
Since there is no chemotherapy or specific treatment available targeting the TBE virus itself, symptomatic or supportive treatment (e.g. maintenance of the water and electrolyte balances) is required. This lack of targeting treatment emphasizes the necessity of tick prophylaxis. Repellent parasiticides may be the right choice to minimize attachment and subsequent feeding of the tick vector.
In the case of diseased dogs emphasis has to be put on preventing secondary harm to the patient itself as well as the owner during convulsions and aggressive behavior. For that reason, therapy should include resting as well as anticonvulsive and sedative medication (Pfeffer and Dobler, 2011). Non-steroidal anti-inflammatory drugs (NSAID) are best used to combat the high fever, and antibiotics should be given to prevent secondary bacterial infections, in particular pneumonia (Kritz et al., 2001). Most of the few dogs, that survived a clinical TBE needed between a hal
Clinical Signs
Canine TBE
The incubation period for canine TBE in most cases
Clinical Signs
Canine TBE
The incubation period for canine TBE in most cases
In general the risk for a tick-infected dog to develop clinical manifest TBE is very small. A serological survey performed in dogs from Sweden in 1992 proved 18 of 225 dogs (8%) to be seropositive and 16 of these 18 dogs showing neurological signs (Bjöersdorff, 2002).
Human TBE
The incubation period is between 3 and 28 days. The course of disease is often asymptomatic. An estimated 30% will exhibit clinical disease, mainly as a feverish flu-like disease. 10-15% of cases (increasing rate with age) will have neurological disorders with the most severe form of persisting paresis and psychiatric sequelae.
In central Europe, the typical case of encephalitis has a biphasic course, with an early, viremic, flu-like stage, followed about a week later by the appearance of signs of meningoencephalitis. CNS disease is relatively mild, but occasional severe motor dysfunction and permanent disability occur. The case fatality rate is 1% to 5%.
Russian spring-summer encephalitis (sometimes referred to as the "Far Eastern form") normally does not show a biphasic course but is characterized by massive headache, high fever, nausea, and vomiting. Delirium, coma, paralysis, and death may follow; the mortality rate is approximately 25% to 30%.
Louping ill infection is generally mild and also displays a biphasic pattern. The virus infects sheep; few cases are reported in humans.
Human Tick Paralysis
In humans, tick paralysis is most likely to be
Human Tick Paralysis
In humans, tick paralysis is most likely to be
A recent CDC report showed that vector-borne diseases -- those transmitted by
A recent CDC report showed that vector-borne diseases -- those transmitted by
How many tick borne diseases are there?
Encephalitis is an inflammation of the brain, usually caused by a viral infection. Although rare, it
Encephalitis is an inflammation of the brain, usually caused by a viral infection. Although rare, it
Some forms of encephalitis are more severe than others. For example,
Some forms of encephalitis are more severe than others. For example,
Lyme encephalopathy is a rare neuropsychiatric disorder, predominantly affecting memory and concentration
Lyme encephalopathy is a rare neuropsychiatric disorder, predominantly affecting memory and concentration
The prognosis for a person with encephalitis varies according to the age of the patient
The prognosis for a person with encephalitis varies according to the age of the patient
The contagious period and incubation period for encephalitis depends on the underlying cause of encephalitis. For
The contagious period and incubation period for encephalitis depends on the underlying cause of encephalitis. For
LINKS AND REFRENCES
https://youtu.be/5bEimiIZ9dA
https://youtu.be/Bv3hQZVtE6Y
https://youtu.be/ENmVXtwsKE8
LINKS AND REFRENCES
https://youtu.be/5bEimiIZ9dA
https://youtu.be/Bv3hQZVtE6Y
https://youtu.be/ENmVXtwsKE8
Further information
Edlow JA, McGillicuddy DC: Tick paralysis. Inf Dis Clin North
Further information
Edlow JA, McGillicuddy DC: Tick paralysis. Inf Dis Clin North
Gordon BM, Giza CC: Tick paralysis presenting in an urban environment. Pediatr Neurol. 2004, 30, 122-4
Malik R, Farrow BR: Tick paralysis in North America and Australia. Vet Clin North Am Small Anim Pract. 1991, 21, 157-71
Wright IG, Stone BF, Neish AL: Tick (Ixodes holocyclus) paralysis in the dog – induction of immunity by injection of toxin. Aust Vet J. 1983, 60, 69-70







 Презентация на тему "Забота о потомстве у Рыб" - скачать бесплатно презентации по Биологии
Презентация на тему "Забота о потомстве у Рыб" - скачать бесплатно презентации по Биологии Открытый урок по биологии Размножение и развитие лягушки. Учитель: Шиляева Вера Анатольевна
Открытый урок по биологии Размножение и развитие лягушки. Учитель: Шиляева Вера Анатольевна Тип Саркодовые
Тип Саркодовые Историческое развитие растительного мира на Земле
Историческое развитие растительного мира на Земле Генетика человека
Генетика человека ЁЖ обыкновенный Виноградова Инга 5«а» класс
ЁЖ обыкновенный Виноградова Инга 5«а» класс  Зрительный аппарат хищных птиц
Зрительный аппарат хищных птиц Презентация Богомол
Презентация Богомол Значение и многообразие растений. Мифы и легенды о растениях
Значение и многообразие растений. Мифы и легенды о растениях 64432-48
64432-48 Красная книга. Амурский тигр
Красная книга. Амурский тигр Презентация по биологии Рабдовирусы. (Rhabdoviridae) Возбудители бешенства и вазикулярного стоматита.
Презентация по биологии Рабдовирусы. (Rhabdoviridae) Возбудители бешенства и вазикулярного стоматита.  ГМО Генетически модифицированный организм
ГМО Генетически модифицированный организм  Тема урока: Высшие споровые. Плауны, хвощи, папоротники Цель урока: - изучить представителей современных папоротникообразных; -
Тема урока: Высшие споровые. Плауны, хвощи, папоротники Цель урока: - изучить представителей современных папоротникообразных; -  Продолговатый мозг. Лекция 5
Продолговатый мозг. Лекция 5 Презентация на тему Системы органов человека
Презентация на тему Системы органов человека  Самая курлыкающая птица. Серый журавль
Самая курлыкающая птица. Серый журавль Закономерности наследования признаков, установленные Г.Менделем. Первый и второй законы Менделя
Закономерности наследования признаков, установленные Г.Менделем. Первый и второй законы Менделя Значение опорнодвигательной системы. Строение костей
Значение опорнодвигательной системы. Строение костей Презентация ученика 5 «б» КЛАССА Хоменко руслана На тему : Тигры
Презентация ученика 5 «б» КЛАССА Хоменко руслана На тему : Тигры  Хамелеон. Дивовижні факти
Хамелеон. Дивовижні факти Человек, личность, индивид, индивидуальность
Человек, личность, индивид, индивидуальность Островки патогенности. Универсальность факторов патогенности
Островки патогенности. Универсальность факторов патогенности Движущие силы эволюции: борьба за существование, наследственная изменчивость, естественный отбор
Движущие силы эволюции: борьба за существование, наследственная изменчивость, естественный отбор Морфология человека. Мягкие части лица. Тотальные размеры тела
Морфология человека. Мягкие части лица. Тотальные размеры тела Экологические группы птиц
Экологические группы птиц Влияние норм минеральных удобрений на урожайность и качество озимой пшеницы в условиях Орловской области
Влияние норм минеральных удобрений на урожайность и качество озимой пшеницы в условиях Орловской области Осложнения при укусах домашних и диких животных
Осложнения при укусах домашних и диких животных