Содержание
- 2. Disproportion, in relation to the pelvis, is a state where the normal proportion between the size
- 3. Contracted outlet is suspected when the interischial tuberous diameter is 8 cm or less. A contracted
- 4. As the head is the largest part of the fetus, it is more important to know
- 5. DIAGNOSIS OF CEPHALOPELVIC DISPROPORTION (CPD) AT THE BRIM The presence and degree of cephalopelvic disproportion at
- 6. Inferences: The head can be pushed down in the pelvis without overlapping of the parietal
- 7. Abdominovaginal method (Muller-Munro Kerr): This bimanual method is superior to the abdominal method as the pelvic
- 8. Inferences: (1) The head can be pushed down up to the level of ischial spines and
- 9. X-ray pelvimetry: Lateral X-ray view with the patient in standing position is helpful in assessing cephalopelvic
- 10. Degree of disproportion and contracted pelvis: Based on the clinical and supplemented by imaging pelvimetry, the
- 11. Management: Unlike inlet disproportion, clinical diagnosis of midpelvic and outlet disproportion can only be made after
- 13. Скачать презентацию
Disproportion, in relation to the pelvis, is a state where the
Disproportion, in relation to the pelvis, is a state where the
Contracted outlet is suspected when the interischial tuberous diameter is 8
Contracted outlet is suspected when the interischial tuberous diameter is 8
Disproportion at the outlet may not give rise to severe dystocia, but may cause perineal tears. The head is pushed backwards as it cannot be accommodated beneath the symphysis pubis.
As the head is the largest part of the fetus, it
As the head is the largest part of the fetus, it
DIAGNOSIS OF CEPHALOPELVIC DISPROPORTION (CPD) AT THE BRIM The presence and
DIAGNOSIS OF CEPHALOPELVIC DISPROPORTION (CPD) AT THE BRIM The presence and
Inferences: The head can be pushed down in the pelvis
Inferences: The head can be pushed down in the pelvis
The abdominal method can be used as a screening procedure. At times, it is difficult to elicit due to deflexed head, thick abdominal wall, irritable uterus and high-floating head.
Abdominovaginal method (Muller-Munro Kerr): This bimanual method is superior to the
Abdominovaginal method (Muller-Munro Kerr): This bimanual method is superior to the
Inferences: (1) The head can be pushed down up to the
Inferences: (1) The head can be pushed down up to the
Limitations of clinical assessment: (1) The method is only applicable to note the presence or absence of disproportion at the brim and not at all applicable to elicit midpelvic or outlet contraction; (2) The fetal head can be used as a pelvimeter to elicit only the contraction in the anteroposterior plane of the inlet but when the contraction affects the transverse diameter of the inlet, it is of less use
X-ray pelvimetry: Lateral X-ray view with the patient in standing position
X-ray pelvimetry: Lateral X-ray view with the patient in standing position
Cephalometry: While a rough estimation of the size of the head can be assessed clinically, accurate measurement of the biparietal diameter would have been ideal to elicit its relation with the diameters of the planes of a given pelvis through which it has to pass. In this respect, ultrasonographic measurement of the biparietal diameter or Magnetic Resonance Imaging (MRI) gives superior information. The average biparietal diameter measures 9.4–9.8 cm at term.
Magnetic Resonance Imaging (MRI): MRI is useful to assess the pelvic capacity at different planes. It is equally informative to assess the fetal size, fetal head volume and pelvic soft tissues which are also important for successful vaginal delivery.
Degree of disproportion and contracted pelvis: Based on the clinical and
Degree of disproportion and contracted pelvis: Based on the clinical and
Management: Unlike inlet disproportion, clinical diagnosis of midpelvic and outlet disproportion
Management: Unlike inlet disproportion, clinical diagnosis of midpelvic and outlet disproportion
(2) To allow vaginal delivery: In otherwise uncomplicated cases with minor contraction, vaginal delivery is allowed under supervision with watchful expectancy. Molding and adaptation of the head and “give” of the pelvis may allow the head to pass through the contracted zone. Delivery is accomplished by forceps or ventouse with deep episiotomy to prevent perineal injuries, especially with narrow pubic arch. Labor progress should be mapped with a partograph to make an early diagnosis of dysfunctional labor due to disproportion. Oxytocin may be used to augment labor for adequate uterine contractions. If there is no dilatation of cervix or descent of the fetal head after a period of 2 hours in the active phase of labor, arrest of labor is considered. Once arrest disorder is diagnosed, cesarean delivery is the option.
 Юные экологи - краеведы
Юные экологи - краеведы Austria, Kirillova Alina 342 group
Austria, Kirillova Alina 342 group Sredstvo-upravleniya
Sredstvo-upravleniya Электроэнергетика России
Электроэнергетика России Использование новых видов деревьев в озеленении петербурга в условиях потепления климата
Использование новых видов деревьев в озеленении петербурга в условиях потепления климата Расчет прочности наклонных сечений изгибаемых элементов
Расчет прочности наклонных сечений изгибаемых элементов Арт.Родина_Карта_25.07 — копия
Арт.Родина_Карта_25.07 — копия 35e4f50ff12c8d471433d164663eb0fd
35e4f50ff12c8d471433d164663eb0fd Регистрация электронный журнал (2)
Регистрация электронный журнал (2) Обзор возможностей календаря Google
Обзор возможностей календаря Google Коллаж фото от встречи до свадьбы
Коллаж фото от встречи до свадьбы Revoland Presentation
Revoland Presentation Преза для сайта
Преза для сайта 20120310_predl_k_ot.ppt_5
20120310_predl_k_ot.ppt_5 Изучение требований профессиональных стандартов к работникам сферы электроэнергетики и электротехники
Изучение требований профессиональных стандартов к работникам сферы электроэнергетики и электротехники Путь поэта
Путь поэта Времена года
Времена года Сюрприз для Виталика
Сюрприз для Виталика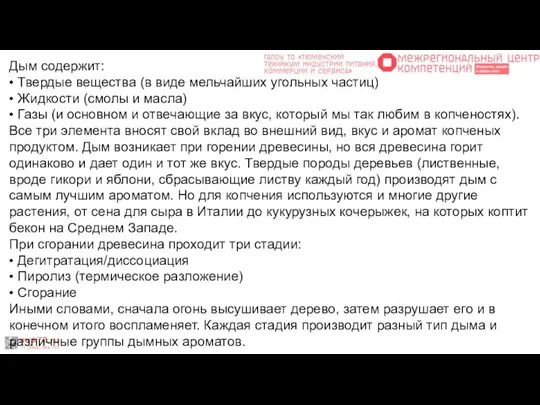 Что такое дым и почему копчености такие вкусные
Что такое дым и почему копчености такие вкусные Загадки для мальчиков. С днём защитника отечества
Загадки для мальчиков. С днём защитника отечества Народный календарь на апрель месяц
Народный календарь на апрель месяц Prezentatsia1
Prezentatsia1 Основы религиозных культур и светской этики
Основы религиозных культур и светской этики Мой класс и моя школа. (1 класс)
Мой класс и моя школа. (1 класс) Производственная практика
Производственная практика Шашлык по-кавказки
Шашлык по-кавказки 20170822_opasnye_internet_soobshchestva
20170822_opasnye_internet_soobshchestva 20160205_mumu_moya_prezentatsiya
20160205_mumu_moya_prezentatsiya