Содержание
- 2. The Advanced Trauma Life Support (ATLS) Safe and reliable method for the immediate treatment of injured
- 3. ABCDE: Airway with cervical spine protection Breathing Circulation, stop the bleeding Disability or neurologic status Exposure
- 4. A and B: Speech
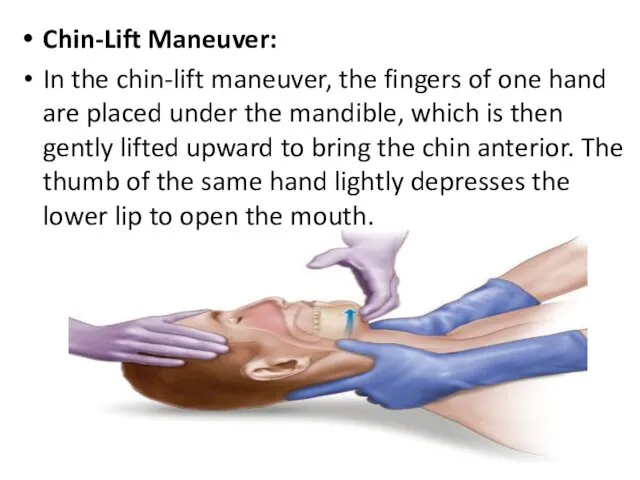
- 7. Chin-Lift Maneuver: In the chin-lift maneuver, the fingers of one hand are placed under the mandible,
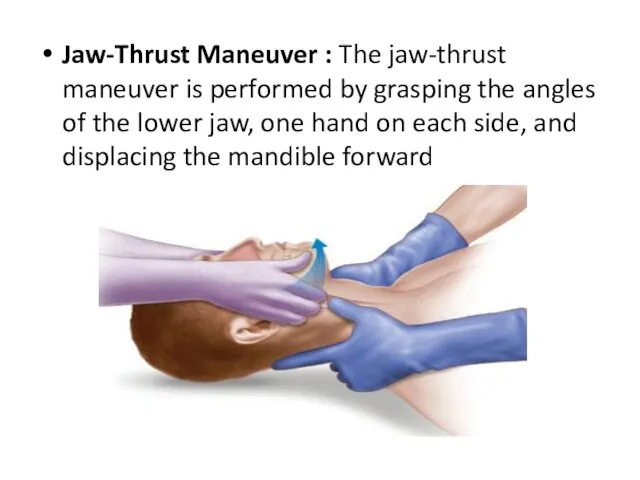
- 8. Jaw-Thrust Maneuver : The jaw-thrust maneuver is performed by grasping the angles of the lower jaw,
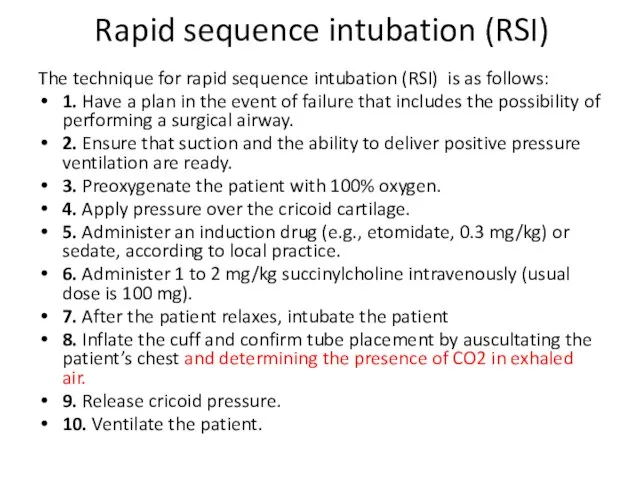
- 10. Rapid sequence intubation (RSI) The technique for rapid sequence intubation (RSI) is as follows: 1. Have
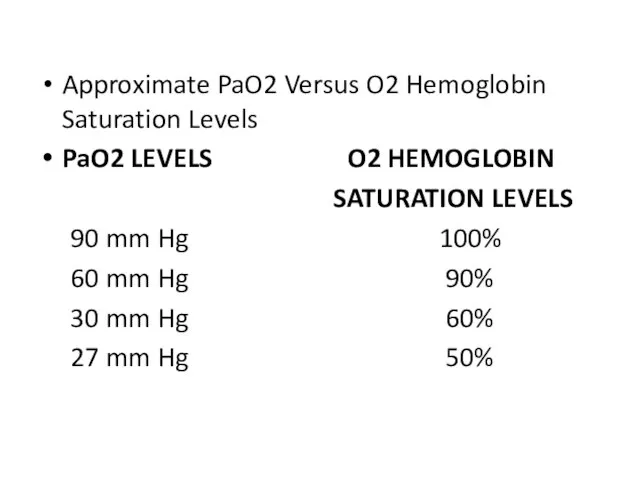
- 11. Approximate PaO2 Versus O2 Hemoglobin Saturation Levels PaO2 LEVELS O2 HEMOGLOBIN SATURATION LEVELS 90 mm Hg
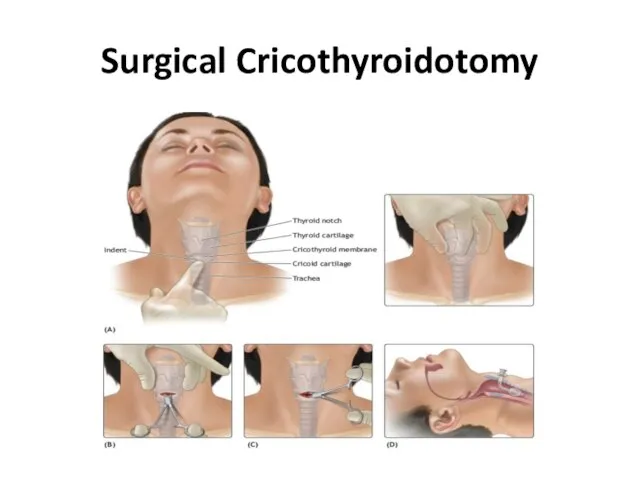
- 12. Surgical Cricothyroidotomy
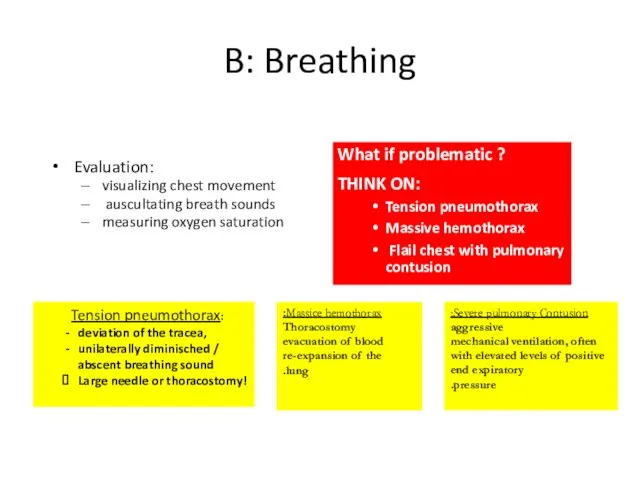
- 13. B: Breathing Evaluation: visualizing chest movement auscultating breath sounds measuring oxygen saturation What if problematic ?
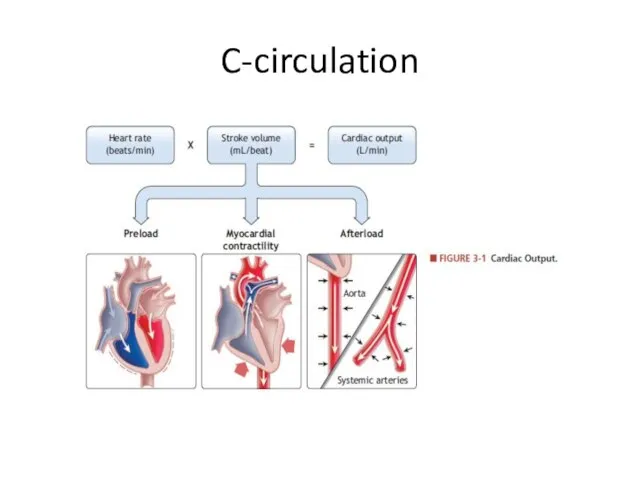
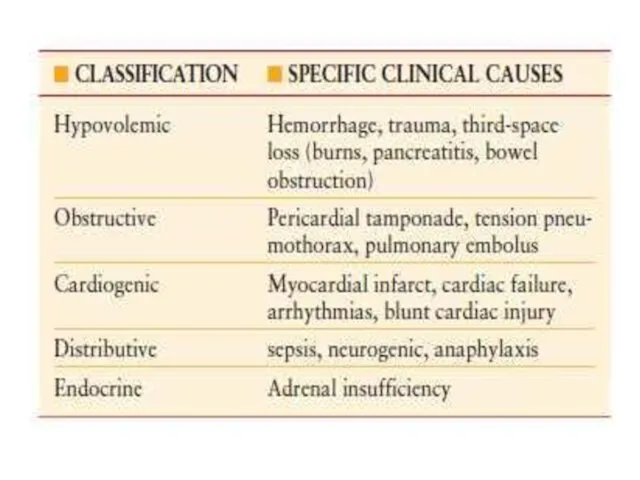
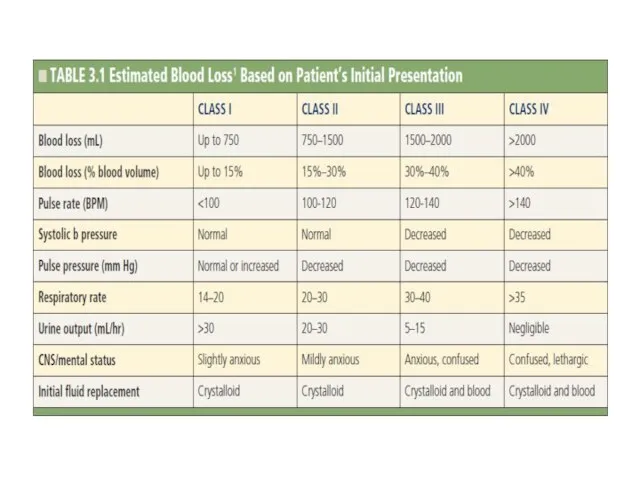
- 14. C-circulation
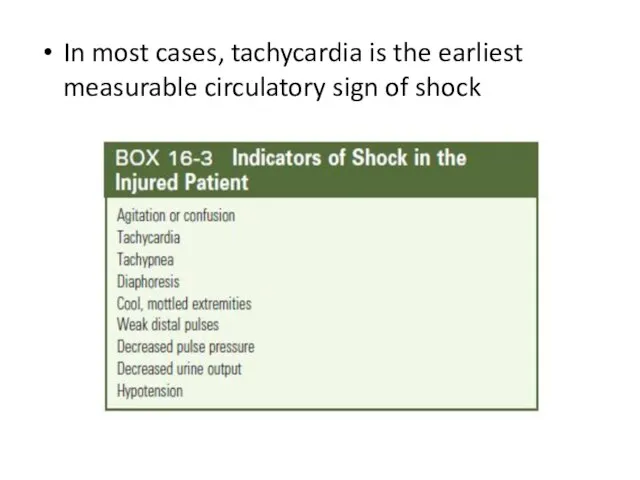
- 15. In most cases, tachycardia is the earliest measurable circulatory sign of shock
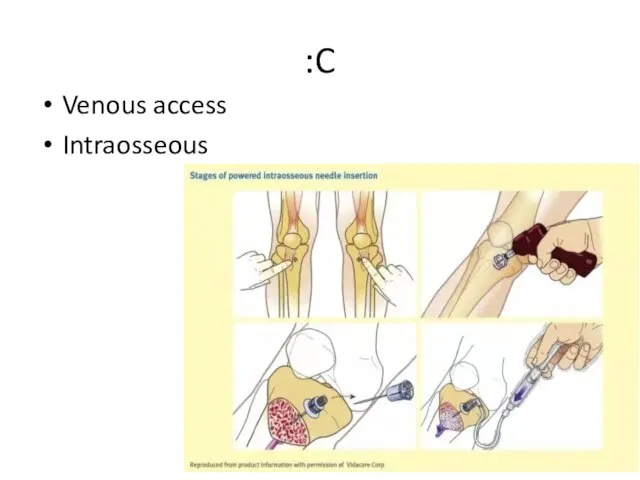
- 19. C: Venous access Intraosseous
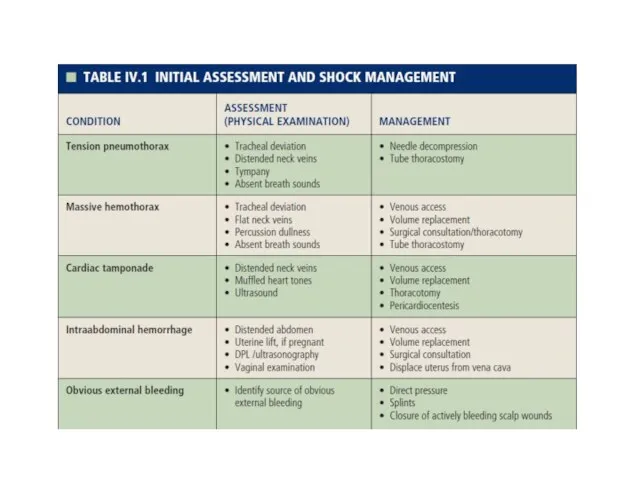
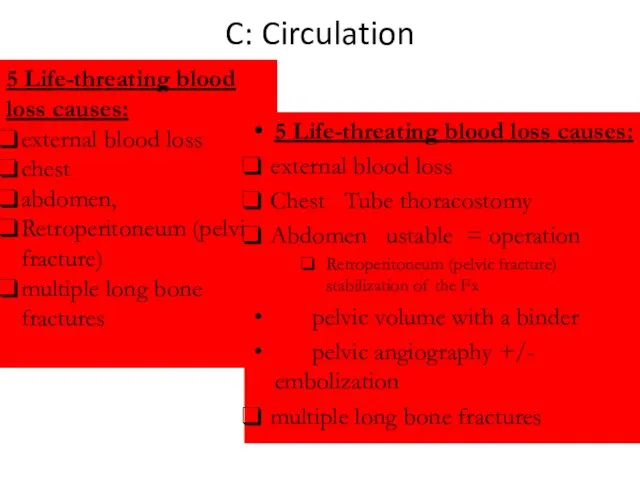
- 20. C: Circulation 5 Life-threating blood loss causes: external blood loss chest abdomen, Retroperitoneum (pelvic fracture) multiple
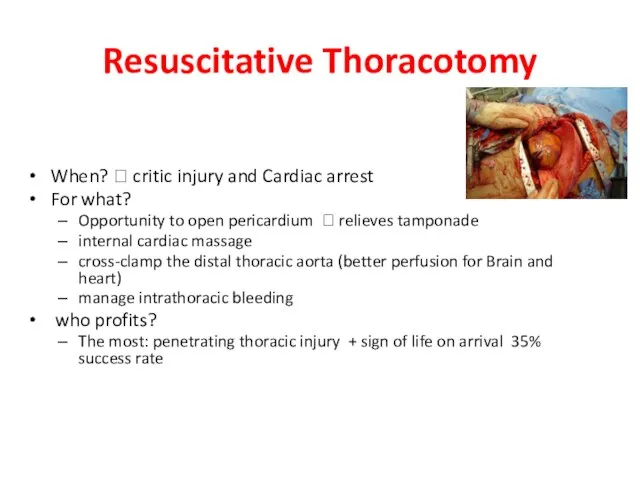
- 21. Resuscitative Thoracotomy When? ? critic injury and Cardiac arrest For what? Opportunity to open pericardium ?
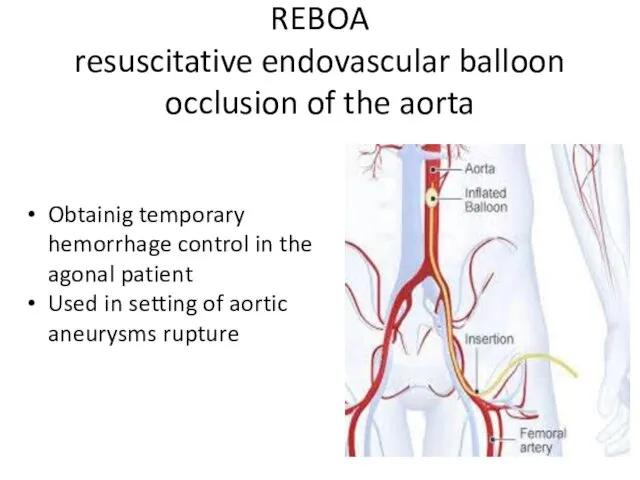
- 23. REBOA resuscitative endovascular balloon occlusion of the aorta Obtainig temporary hemorrhage control in the agonal patient
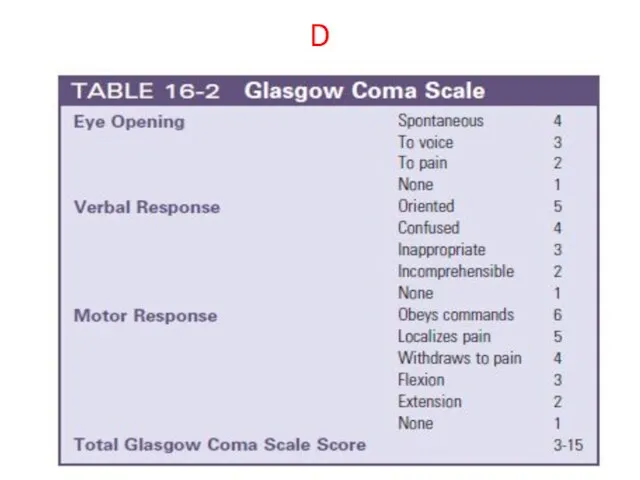
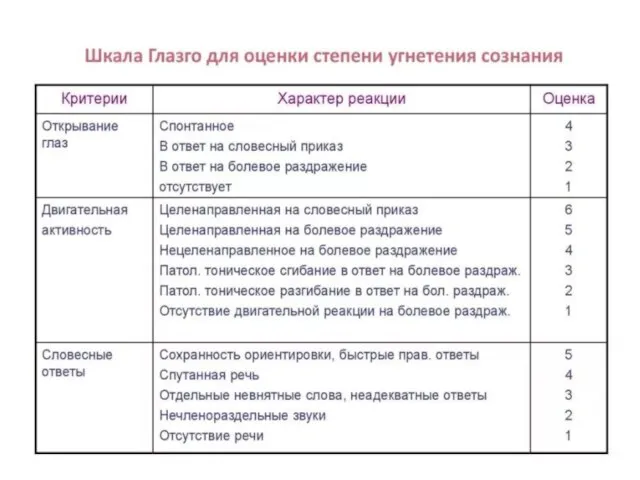
- 24. D
- 26. D: Disability Neurological function evaluation: Neurogenic shock? Spinal cord injury? Body temprature? ? Keep the patient
- 27. :E Head to toe PR Xray FAST NGT Urine catheter
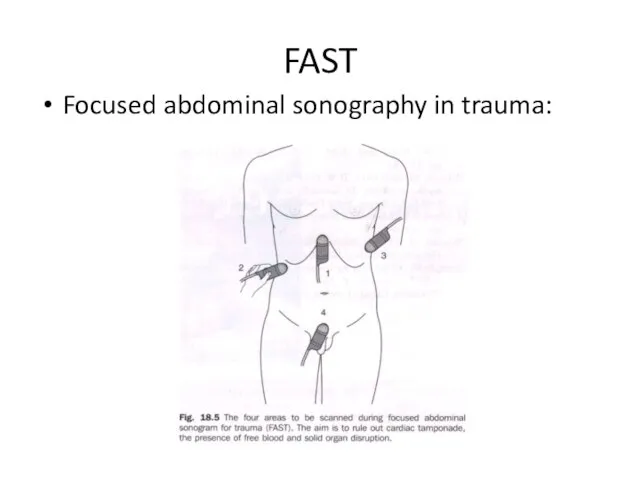
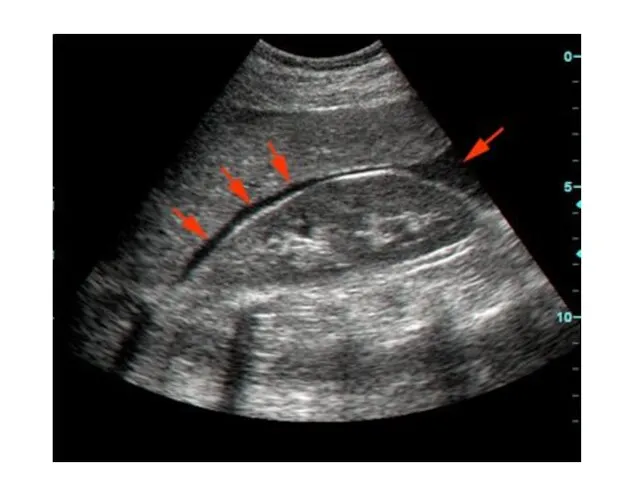
- 34. FAST Focused abdominal sonography in trauma:
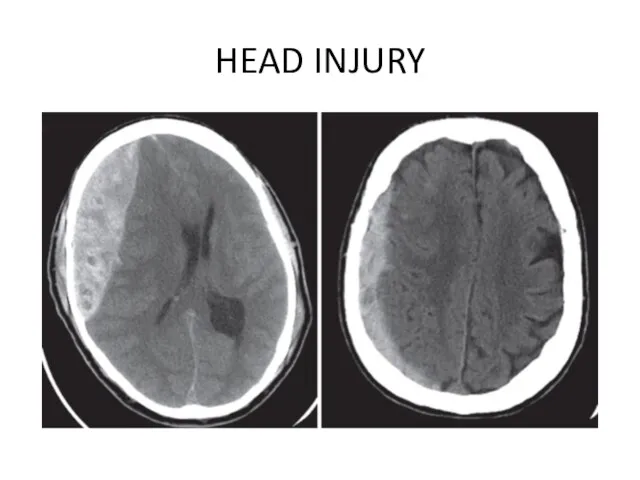
- 37. HEAD INJURY
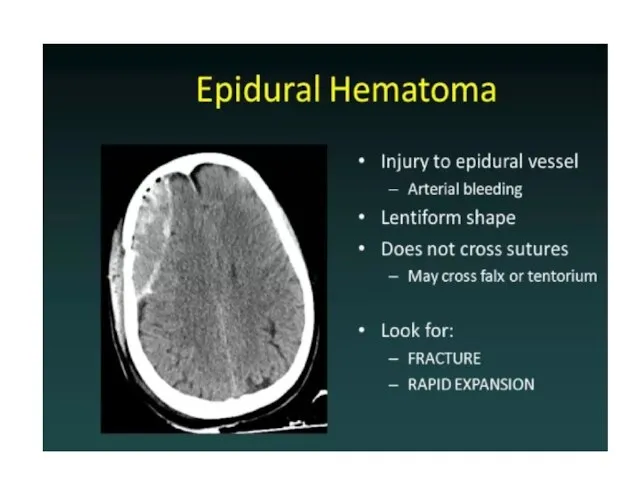
- 39. Epidural hematomas typically result from a lateral fracture of the cranium causing bleeding from the middle
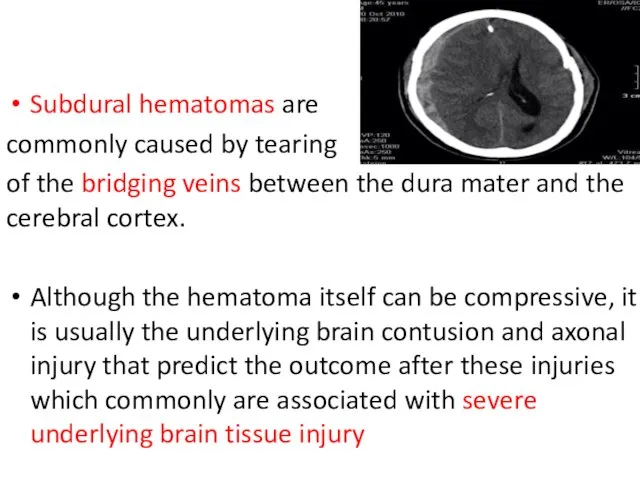
- 40. Subdural hematomas are commonly caused by tearing of the bridging veins between the dura mater and
- 42. Parenchymal contusions of brain tissue result from the direct transmission of energy to the cranium and
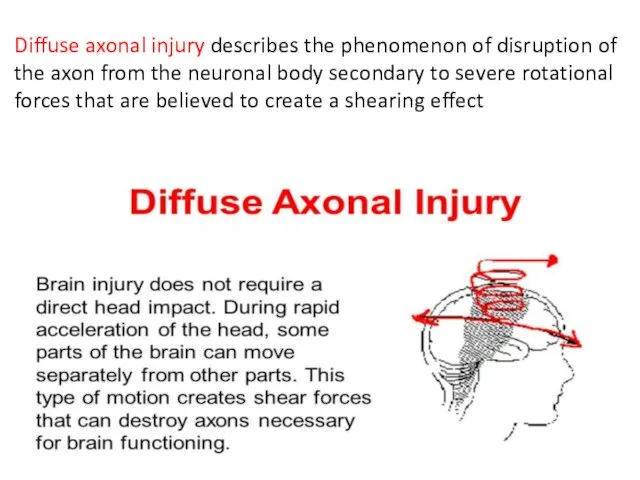
- 43. Diffuse axonal injury describes the phenomenon of disruption of the axon from the neuronal body secondary
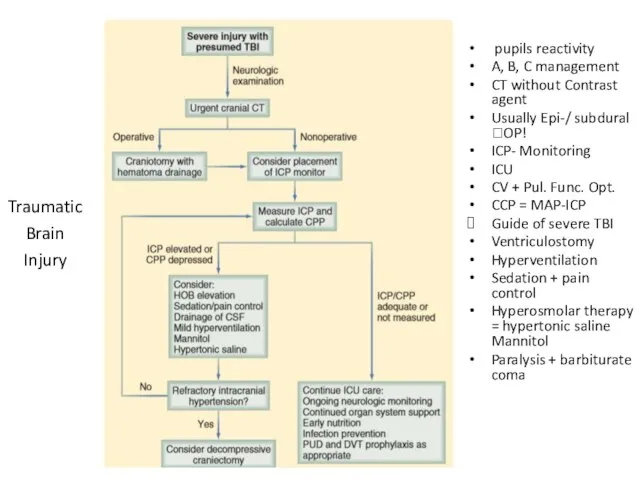
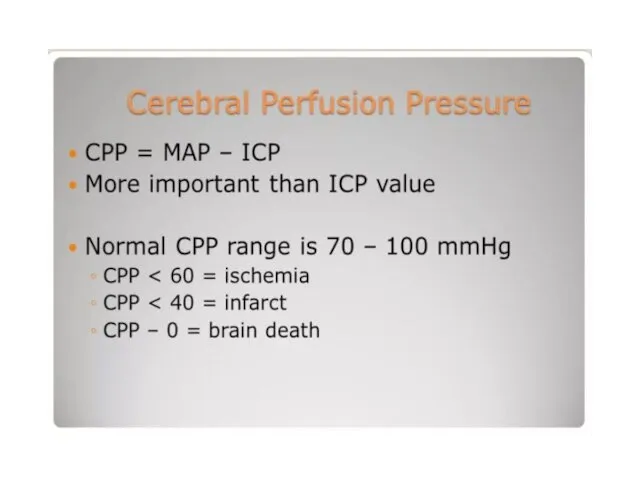
- 45. pupils reactivity A, B, C management CT without Contrast agent Usually Epi-/ subdural ?OP! ICP- Monitoring
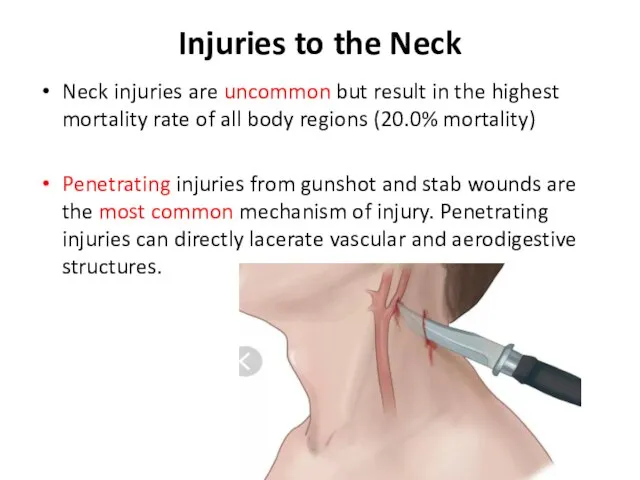
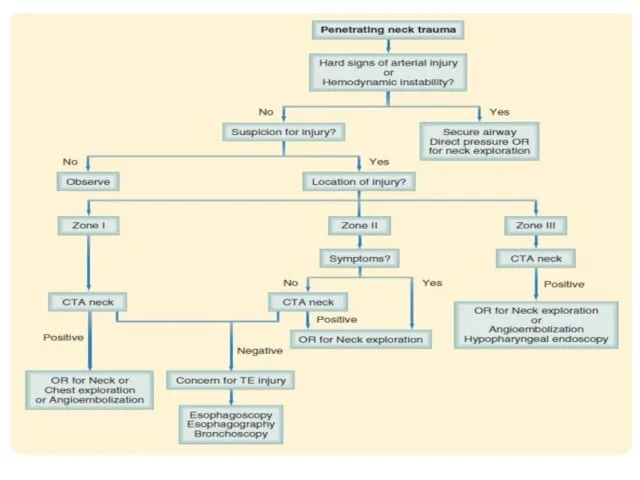
- 47. Injuries to the Neck Neck injuries are uncommon but result in the highest mortality rate of
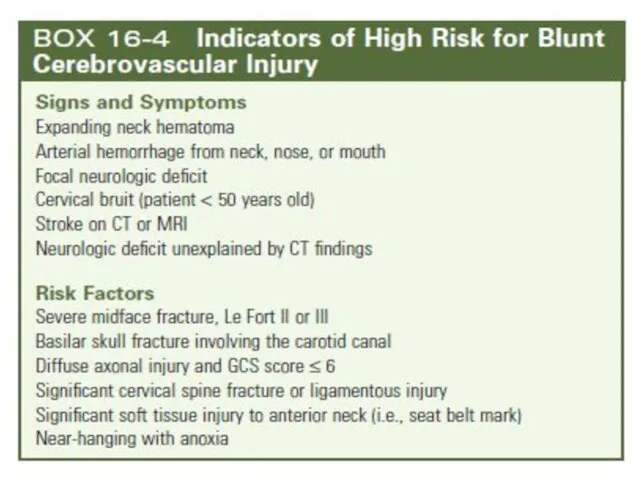
- 48. Blunt mechanisms can cause compression, with fracture of the larynx or trachea. Blunt pharyngeal or esophageal
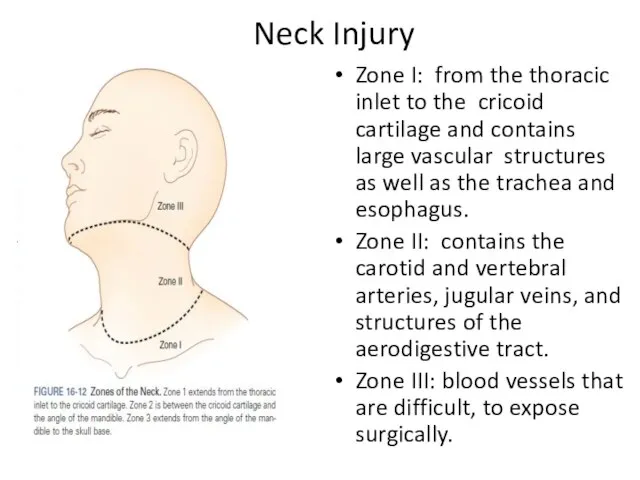
- 51. Neck Injury Zone I: from the thoracic inlet to the cricoid cartilage and contains large vascular
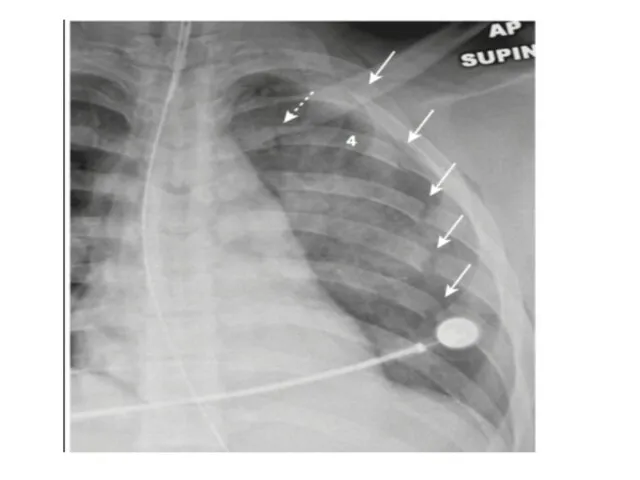
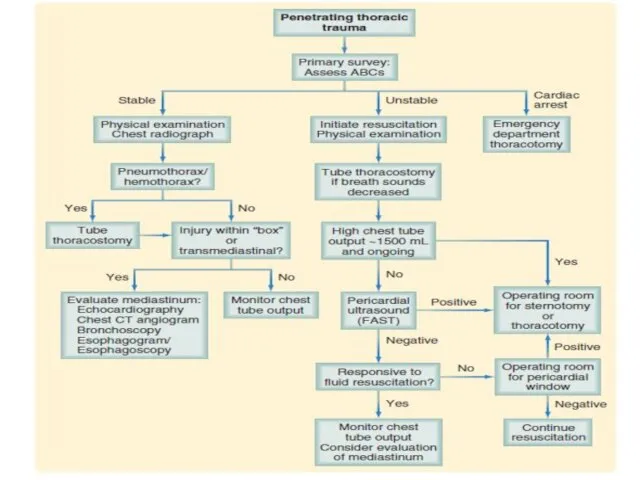
- 53. CHEST INJURY With more than 65% of blunt trauma patients sustaining one or more rib fractures,
- 54. Flail Chest : This condition usually results from trauma associated with multiple rib fractures—that is, two
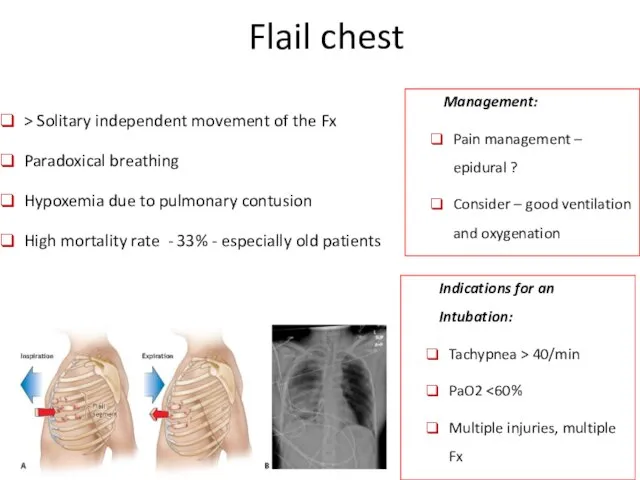
- 55. Flail chest > Solitary independent movement of the Fx Paradoxical breathing Hypoxemia due to pulmonary contusion
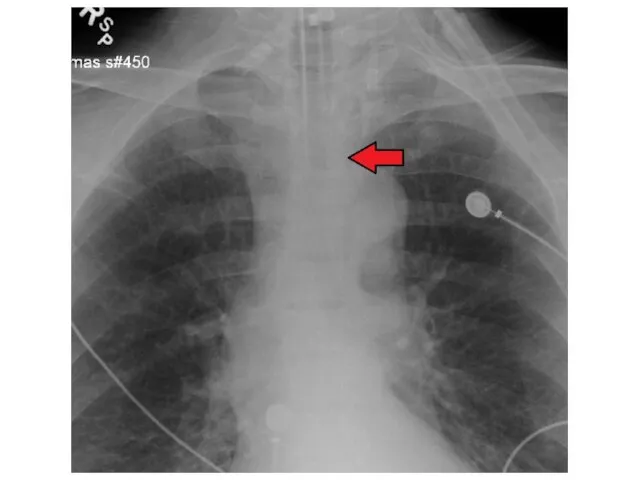
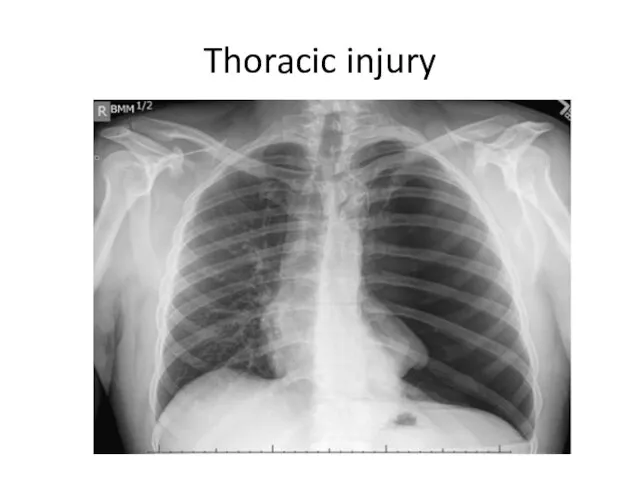
- 57. Thoracic injury
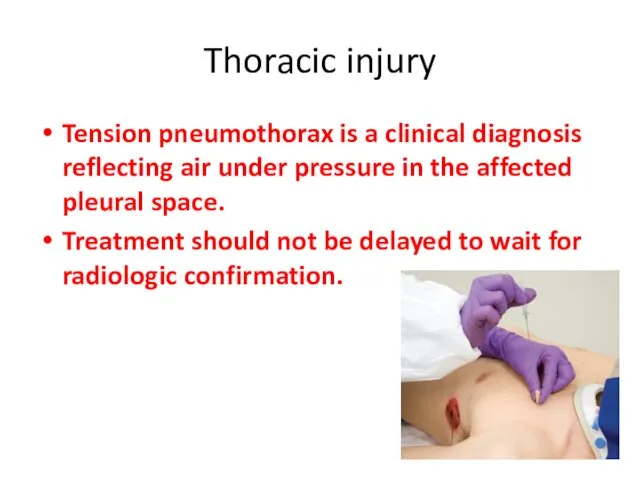
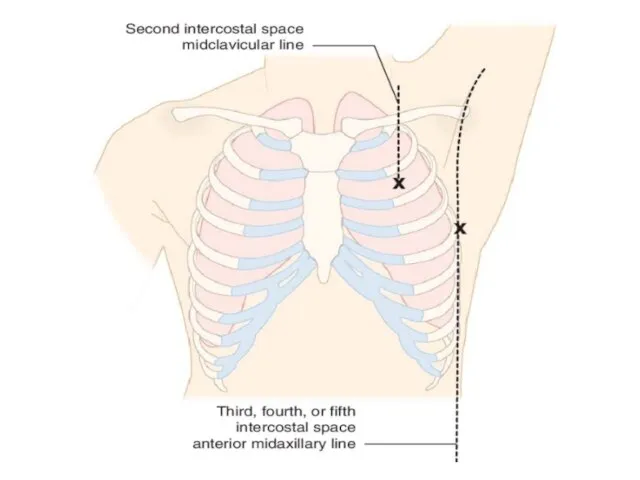
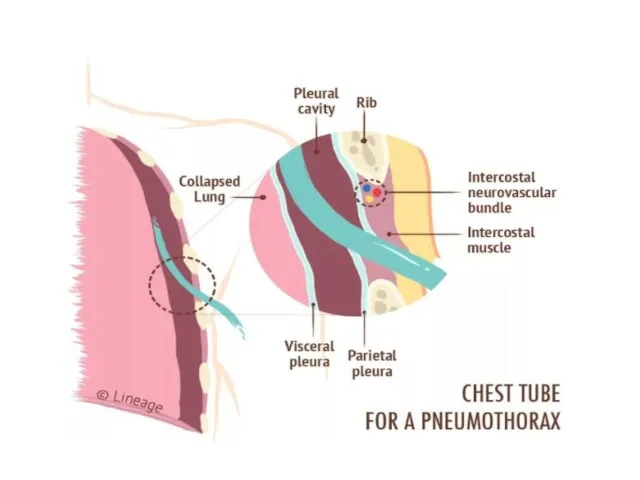
- 58. Thoracic injury Tension pneumothorax is a clinical diagnosis reflecting air under pressure in the affected pleural
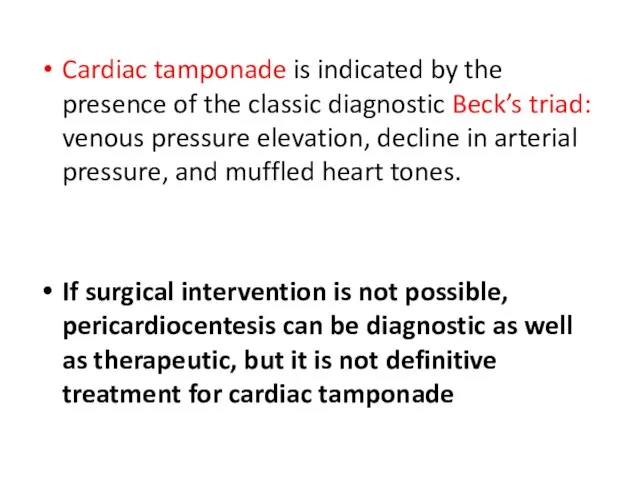
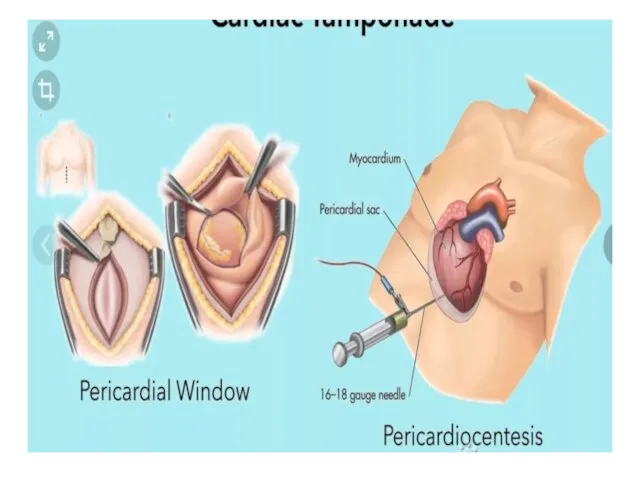
- 61. Cardiac tamponade is indicated by the presence of the classic diagnostic Beck’s triad: venous pressure elevation,
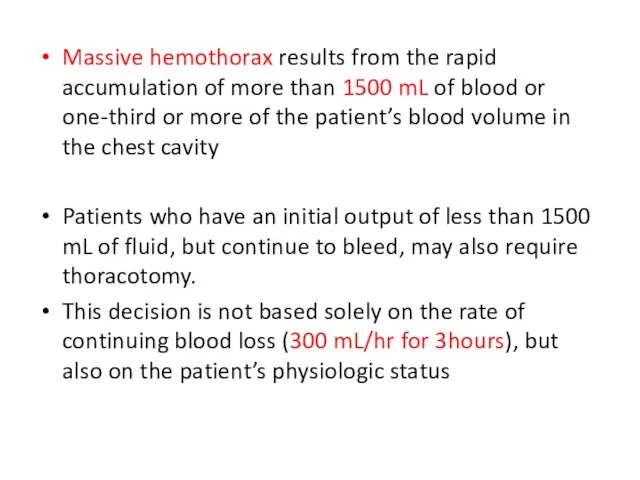
- 63. Massive hemothorax results from the rapid accumulation of more than 1500 mL of blood or one-third
- 65. Thoracic injury Pulmonary injuries. Lung injuries are common after chest trauma, with 31.9% of patients Mortality
- 66. Cardiac injuries uncommon, but most severe injuries sustained by patients after penetrating and blunt trauma. Penetrating
- 67. Blunt injury to the heart occurs less commonly, being seen in only 2.2% of blunt chest
- 68. Tracheobronchial injuries Tracheobronchial tree injuries are uncommon but are associated with significant morbidity and mortality. Penetrating
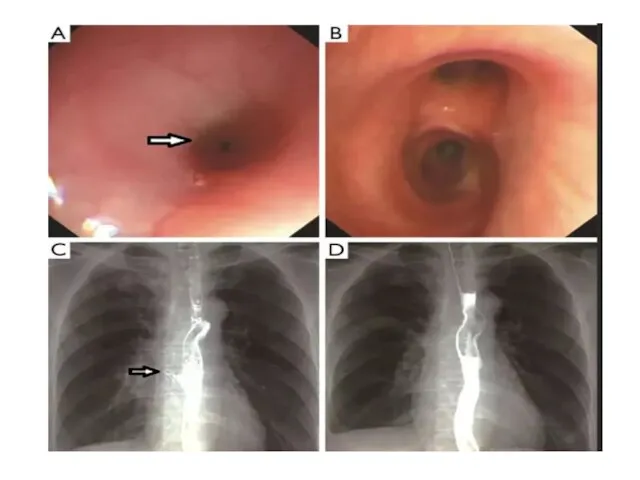
- 69. Esophageal injuries: The thoracic esophagus is uncommonly injured Penetrating injury is more common, but only 1.6%
- 70. The esophagus is best evaluated through a combination of contrast esophagography and esophagoscopy Together these two
- 72. The upper and midthoracic esophagus is best approached through a right posterolateral thoracotomy through the fourth
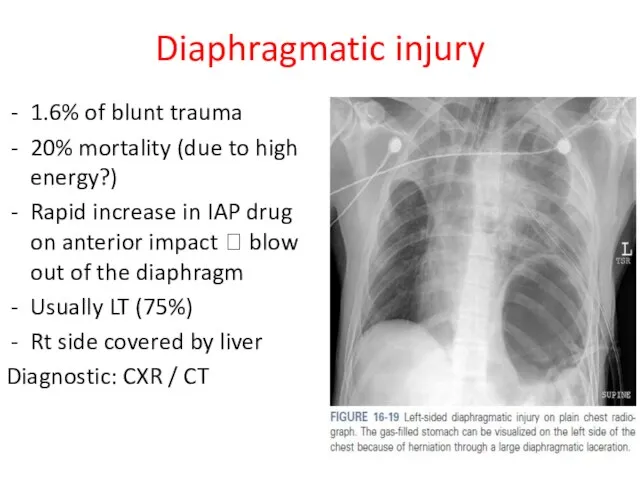
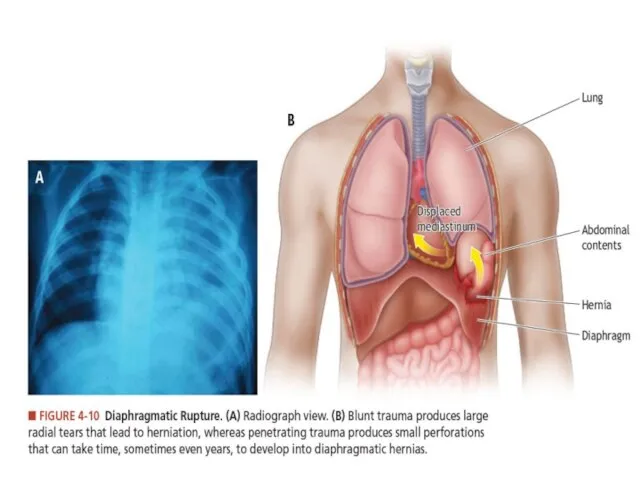
- 73. Diaphragmatic injury 1.6% of blunt trauma 20% mortality (due to high energy?) Rapid increase in IAP
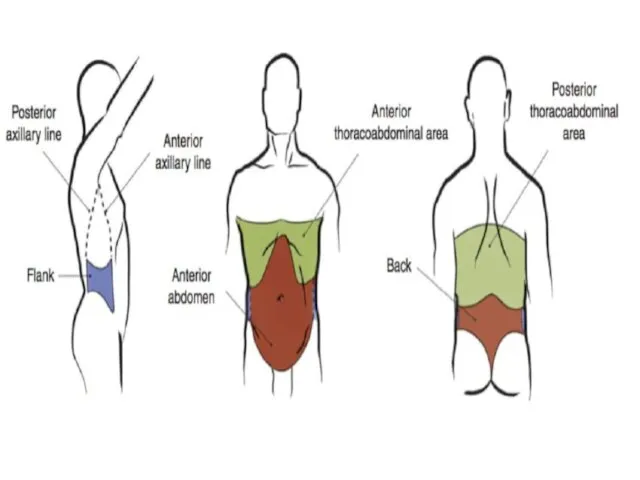
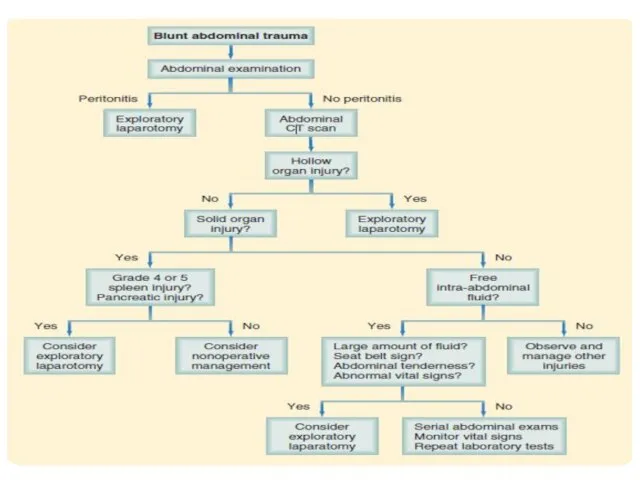
- 75. Abdominal trauma
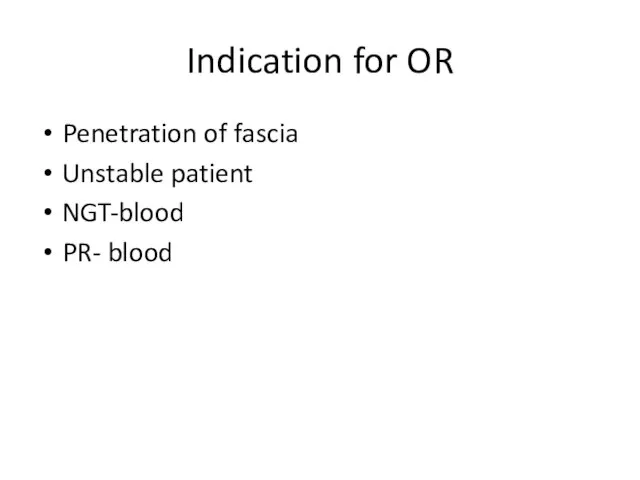
- 78. Indication for OR Penetration of fascia Unstable patient NGT-blood PR- blood
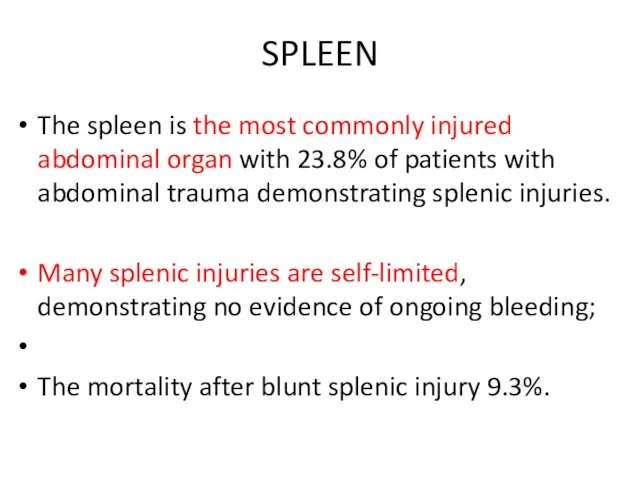
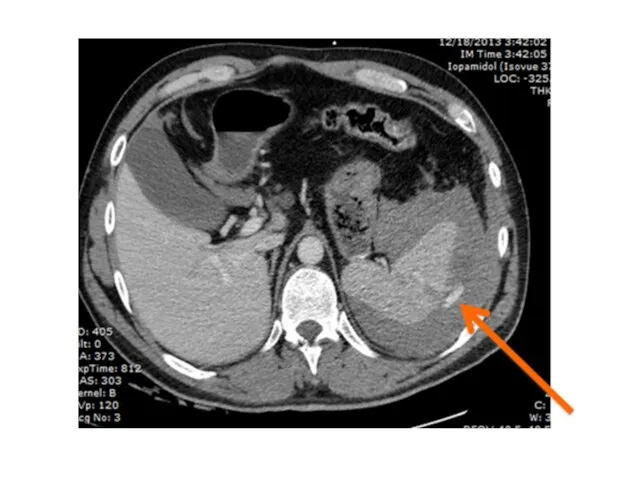
- 80. SPLEEN The spleen is the most commonly injured abdominal organ with 23.8% of patients with abdominal
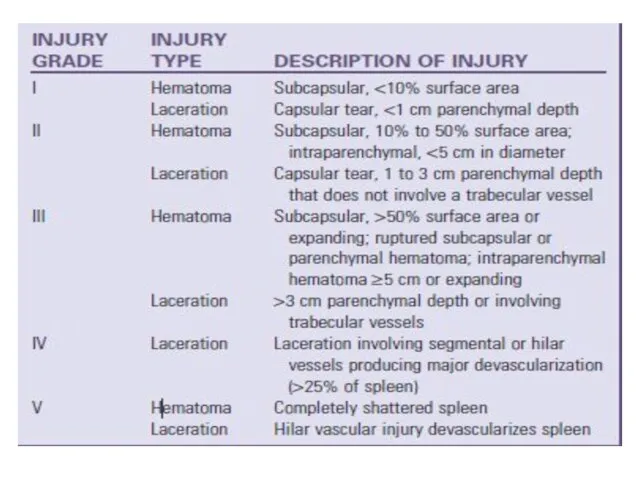
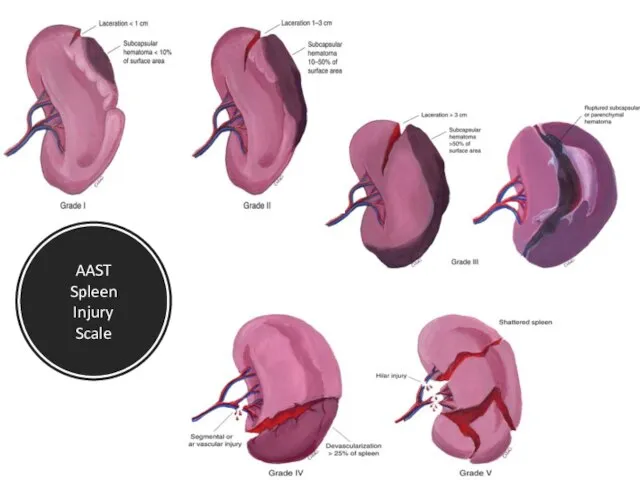
- 82. AAST Spleen Injury Scale
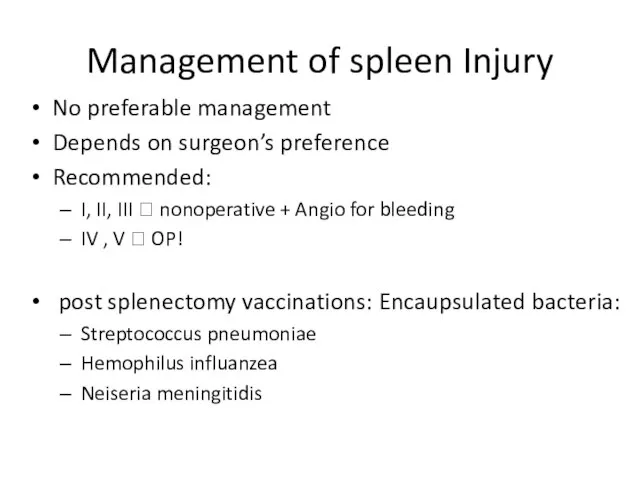
- 84. Management of spleen Injury No preferable management Depends on surgeon’s preference Recommended: I, II, III ?
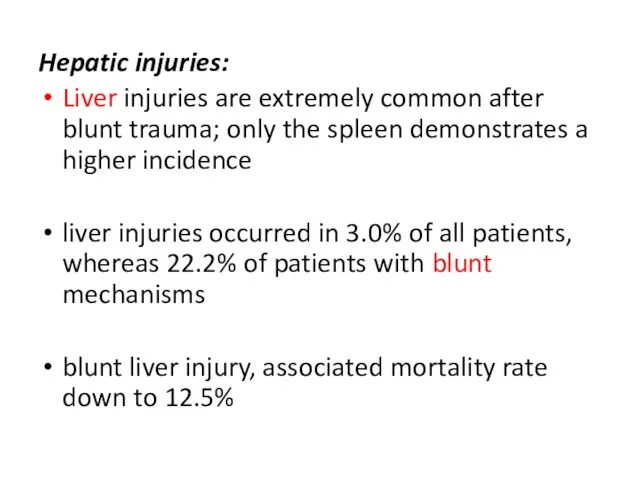
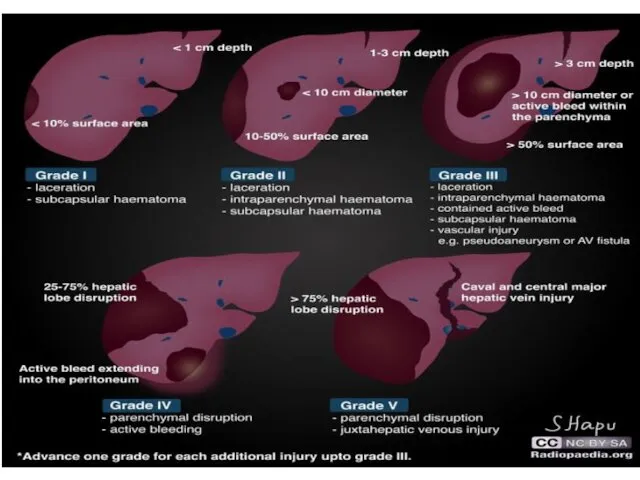
- 85. Hepatic injuries: Liver injuries are extremely common after blunt trauma; only the spleen demonstrates a higher
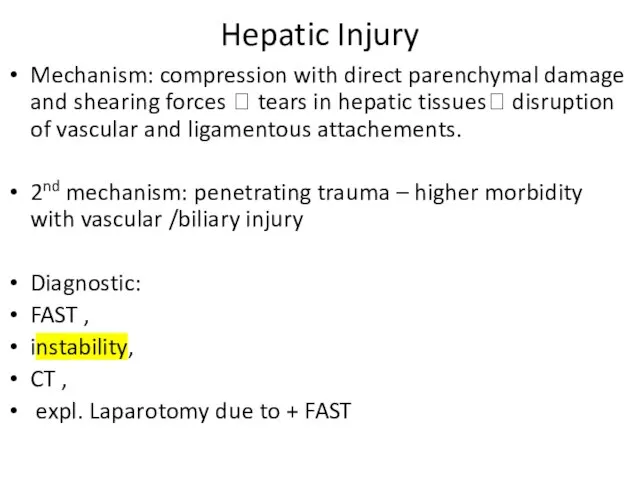
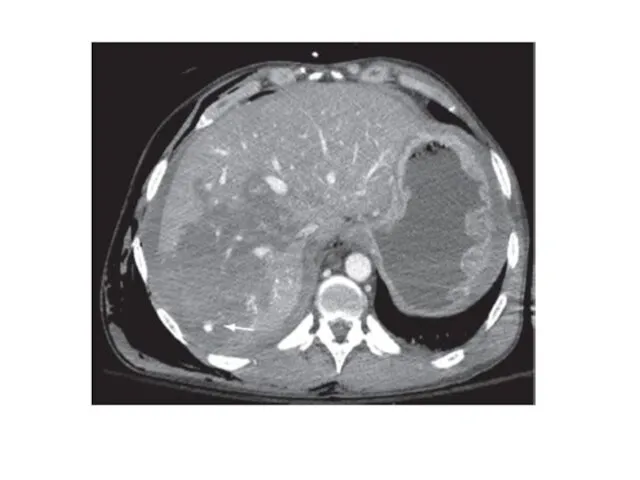
- 88. Hepatic Injury Mechanism: compression with direct parenchymal damage and shearing forces ? tears in hepatic tissues?
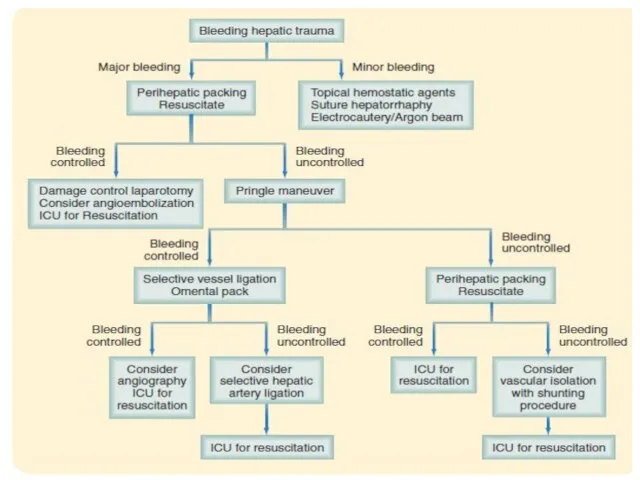
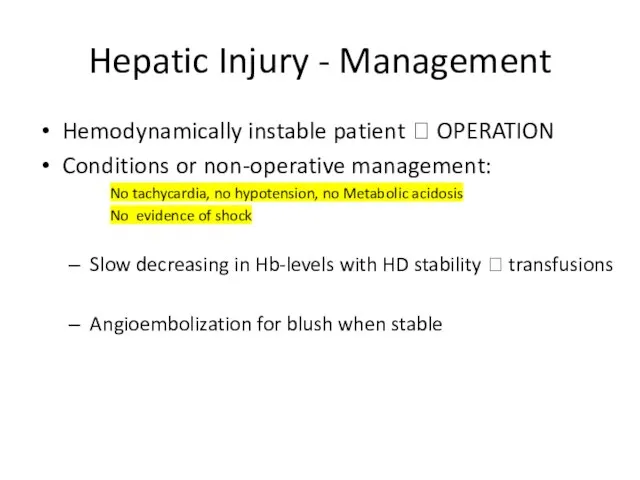
- 91. Hepatic Injury - Management Hemodynamically instable patient ? OPERATION Conditions or non-operative management: No tachycardia, no
- 92. Non-surgical hepatic injury treatment Complications abdominal compartment syndrome bile duct injury leading to bile peritonitis or
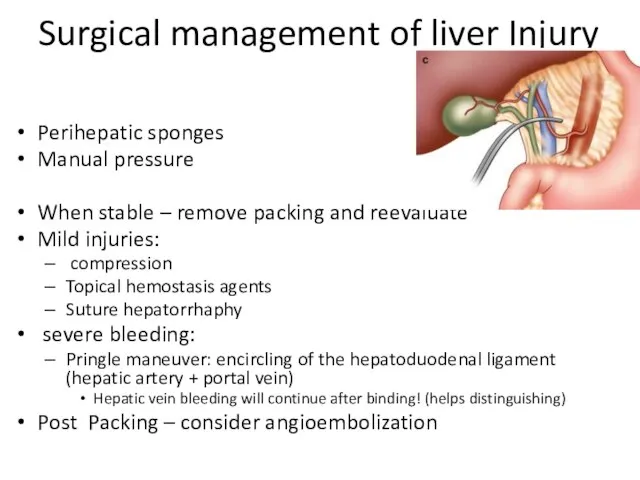
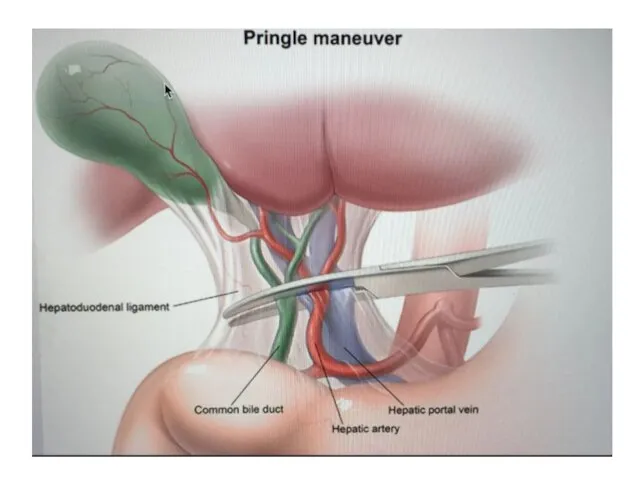
- 93. Surgical management of liver Injury options Packing Pringle Push Plug
- 94. Surgical management of liver Injury Perihepatic sponges Manual pressure When stable – remove packing and reevaluate
- 96. Gastric injuries Penetrating mechanisms are the most common cause of injuries to the stomach, with these
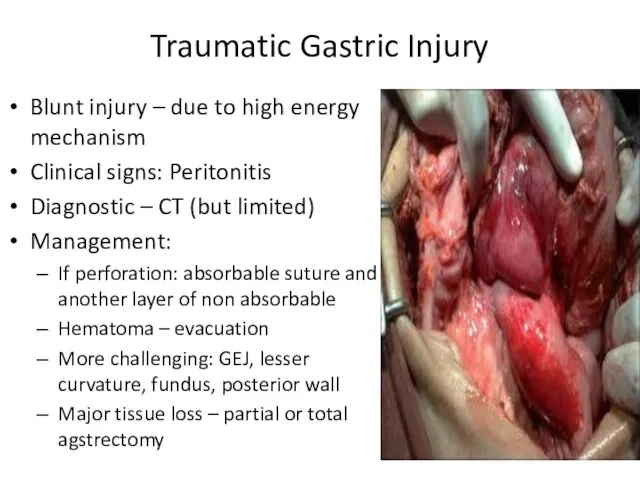
- 97. Traumatic Gastric Injury Blunt injury – due to high energy mechanism Clinical signs: Peritonitis Diagnostic –
- 98. Duodenal injuries Duodenal injuries are uncommon after blunt and penetrating trauma but can pose a diagnostic
- 99. Duodenal injury Children bicycle handlebar or steering wheel stucking in drivers Clinic: Do not expect peritonitis!
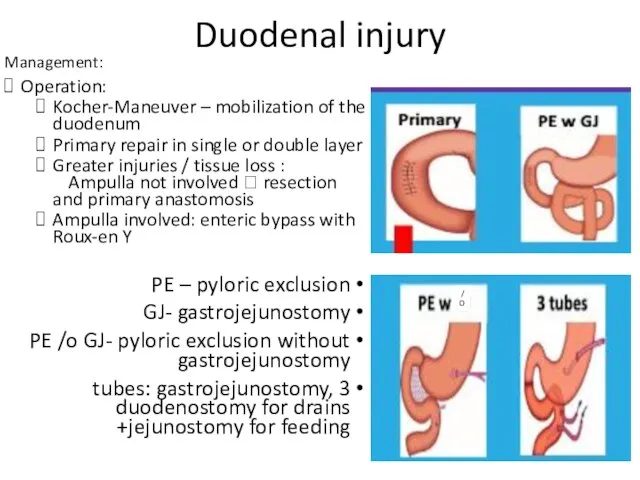
- 100. Duodenal injury Management: Operation: Kocher-Maneuver – mobilization of the duodenum Primary repair in single or double
- 101. Small bowel injuries The small intestine is one of the more frequently injured organs after penetrating
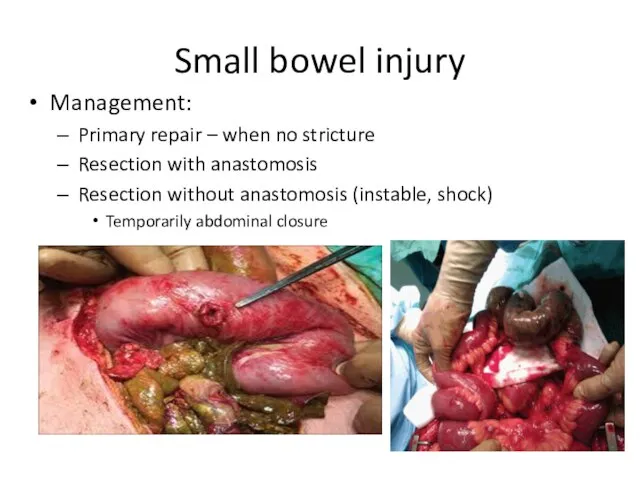
- 102. Small bowel injury Management: Primary repair – when no stricture Resection with anastomosis Resection without anastomosis
- 103. Colon injuries Colon and rectal injuries occur most commonly after penetrating abdominal trauma and rarely after
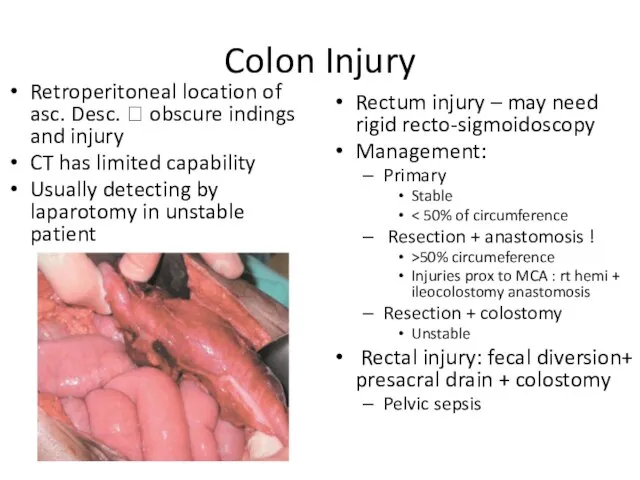
- 104. Colon Injury Retroperitoneal location of asc. Desc. ? obscure indings and injury CT has limited capability
- 105. Pancreatic injuries Pancreatic injuries commonly occur in association with injury to the duodenum because of their
- 106. Pancreas tissue injury can result from direct laceration of the organ or through the transmission of
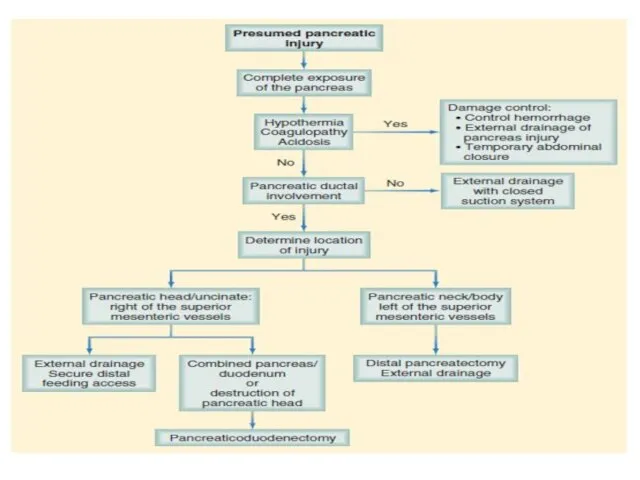
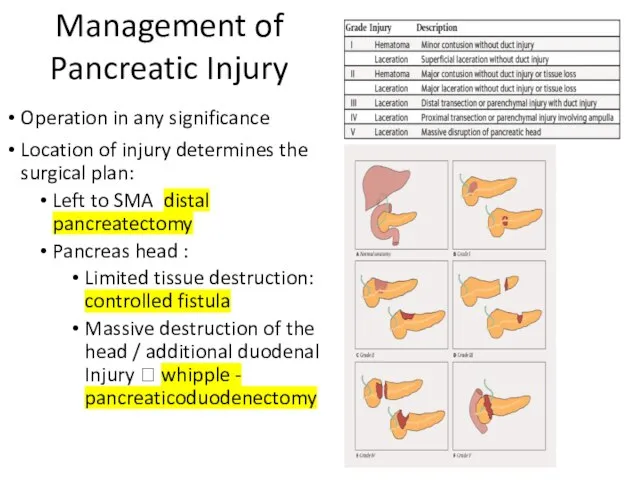
- 108. Management of Pancreatic Injury Operation in any significance Location of injury determines the surgical plan: Left
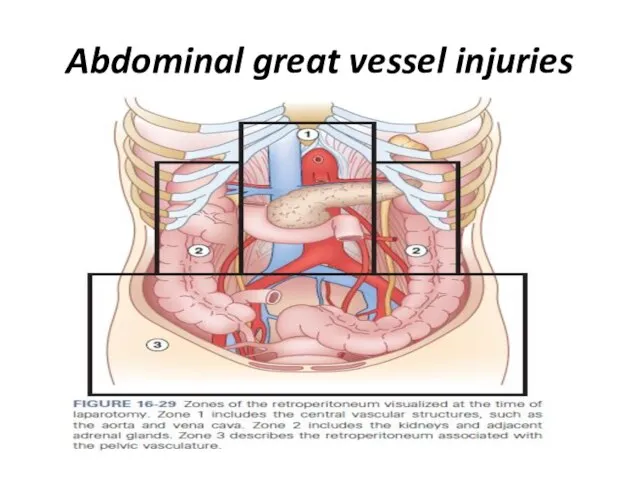
- 109. Abdominal great vessel injuries
- 110. The major blood vessels of the abdomen are predominantly located within the retroperitoneum, with some larger
- 111. The retroperitoneum can be divided into three zones: Zone 1 hematomas require exploration because these frequently
- 112. A hematoma in the region of zone 2, which predominantly contains the kidneys, should be explored
- 113. Abdominal great vessel Injuries I – central hematoma Aorta, prox. visceral vessels, inferior vena cava Always
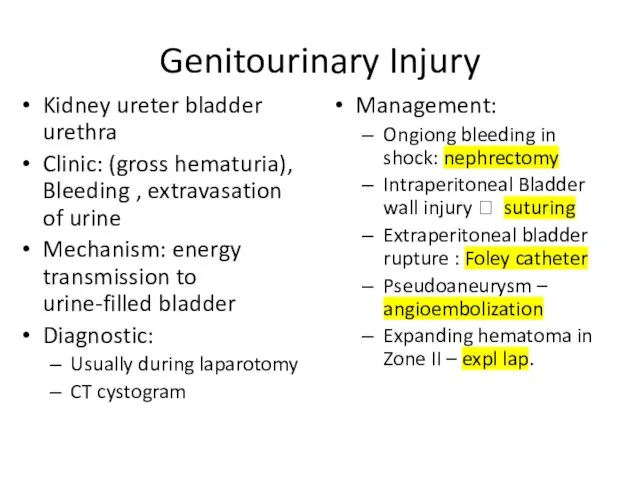
- 114. Genitourinary injuries The genitourinary organs include the kidneys, ureters, bladder, and urethra, all of which are
- 115. Intraperitoneal bladder injuries can be repaired in two layers of absorbable suture and the bladder drained
- 116. Genitourinary Injury Kidney ureter bladder urethra Clinic: (gross hematuria), Bleeding , extravasation of urine Mechanism: energy
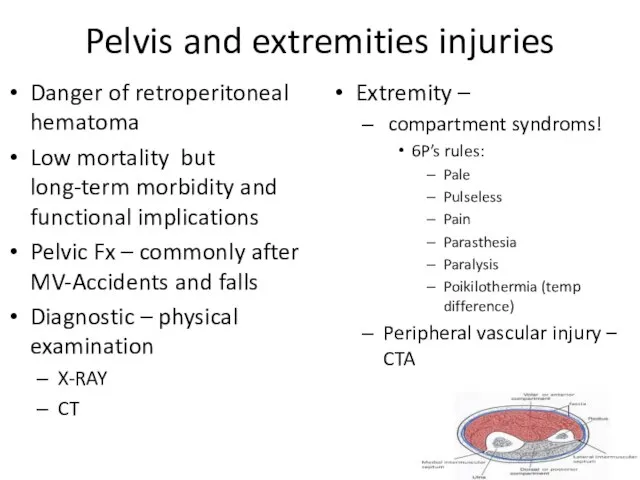
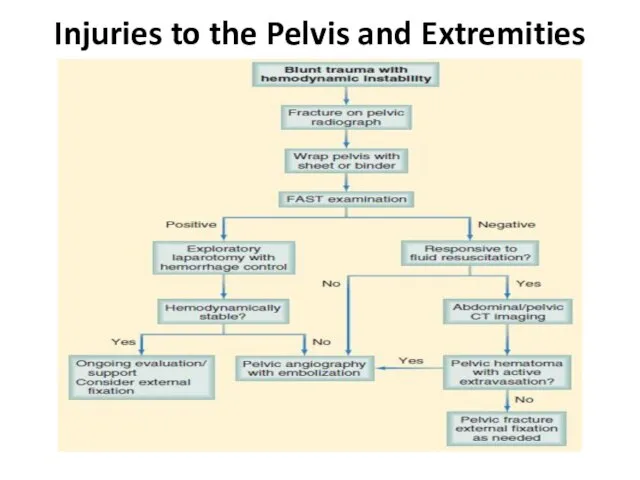
- 117. Pelvis and extremities injuries Danger of retroperitoneal hematoma Low mortality but long-term morbidity and functional implications
- 118. Injuries to the Pelvis and Extremities
- 119. In which of the following the pulse pressure is normal? A. Shock class I B. Shock
- 120. A 30 - year - old male is brought to the trauma unit due to chest
- 121. 22 - year - old male is brought to the trauma unit following a gun -
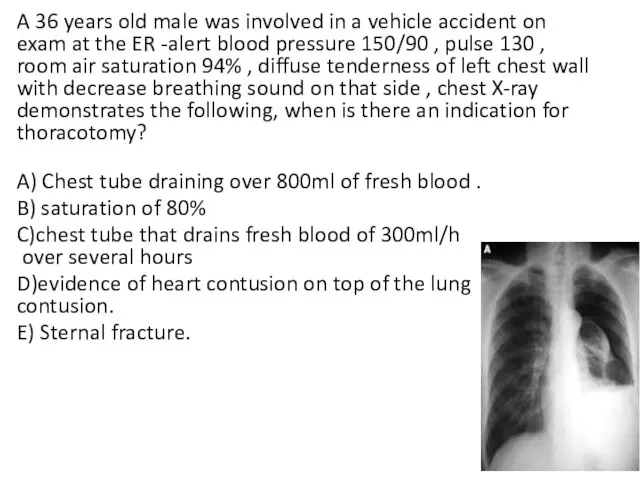
- 122. A 36 years old male was involved in a vehicle accident on exam at the ER
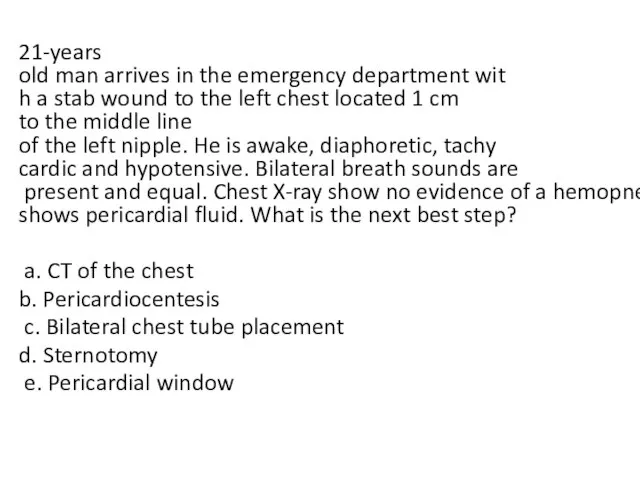
- 123. 21-years old man arrives in the emergency department with a stab wound to the left chest
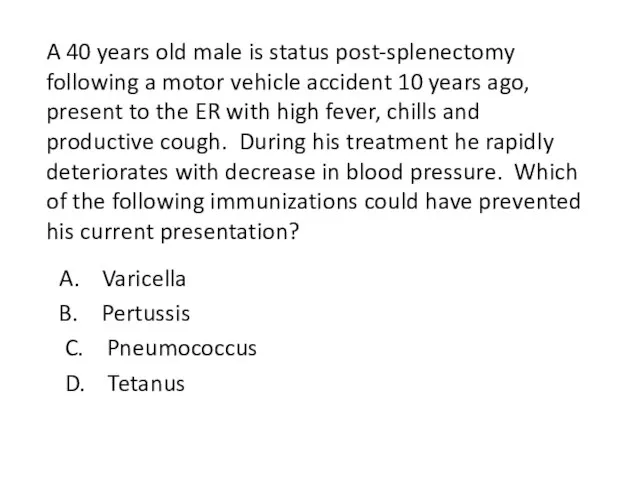
- 124. A 40 years old male is status post-splenectomy following a motor vehicle accident 10 years ago,
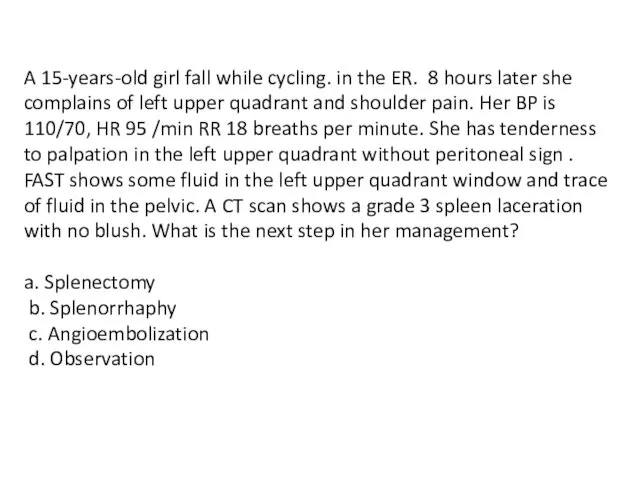
- 125. A 15-years-old girl fall while cycling. in the ER. 8 hours later she complains of left
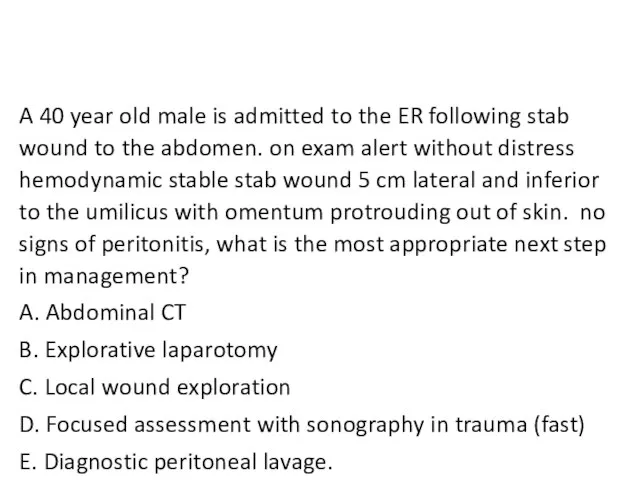
- 126. A 40 year old male is admitted to the ER following stab wound to the abdomen.
- 128. Скачать презентацию













 КНИГА ПАМЯТИ 1 класса
КНИГА ПАМЯТИ 1 класса Онлайн-голосование по отбору общественных территорий. Формирование комфортной городской среды
Онлайн-голосование по отбору общественных территорий. Формирование комфортной городской среды Workforce Circa
Workforce Circa лит чт 04 02
лит чт 04 02 Сверление стен
Сверление стен Очистка сточных вод и характеристика очистных сооружений Свердловской области
Очистка сточных вод и характеристика очистных сооружений Свердловской области Вольфрамовые электроды
Вольфрамовые электроды М. И. Карасев Муха-Цокотуха
М. И. Карасев Муха-Цокотуха Дорогая Гузель!
Дорогая Гузель! Промышленность Свердловской области
Промышленность Свердловской области Виды тканей
Виды тканей Постройка и фантазия
Постройка и фантазия Основные сведения о древесине
Основные сведения о древесине Иллюстрация к произведению Чехова
Иллюстрация к произведению Чехова Сепсис новорождённого
Сепсис новорождённого Газобаллонное оборудование 5 поколения
Газобаллонное оборудование 5 поколения Исследование напряженно-деформированного состояния дискретно армированного стеклопластика на основе термопластичной матрицы
Исследование напряженно-деформированного состояния дискретно армированного стеклопластика на основе термопластичной матрицы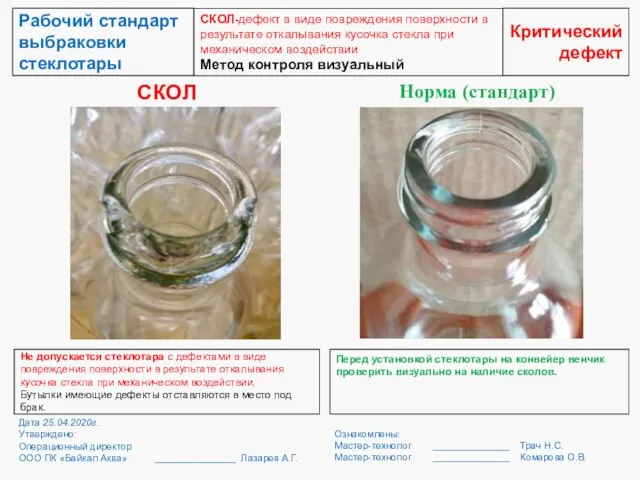 Рабочий стандарт выбраковки стеклотары
Рабочий стандарт выбраковки стеклотары ОС_Презентація_особливої_сесії_EdCamp_in_a_Box_6_0_14_05_21_1
ОС_Презентація_особливої_сесії_EdCamp_in_a_Box_6_0_14_05_21_1 Отчетная документация по педагогической практике
Отчетная документация по педагогической практике Поэты, не вернувшиеся с войны, или До последнего дыхания
Поэты, не вернувшиеся с войны, или До последнего дыхания Электромонтажные и проектные работы. Лаборатория электроизмерений АВС-электро
Электромонтажные и проектные работы. Лаборатория электроизмерений АВС-электро модные часы _ by Artem Morozov
модные часы _ by Artem Morozov Судовое обеспечение подводных работ
Судовое обеспечение подводных работ Основные этапы развития электронной техники
Основные этапы развития электронной техники Современная Российская система образования
Современная Российская система образования О благословении князя Дмитрия Донского на Куликовскую битву
О благословении князя Дмитрия Донского на Куликовскую битву Путешествие в мир сказок
Путешествие в мир сказок