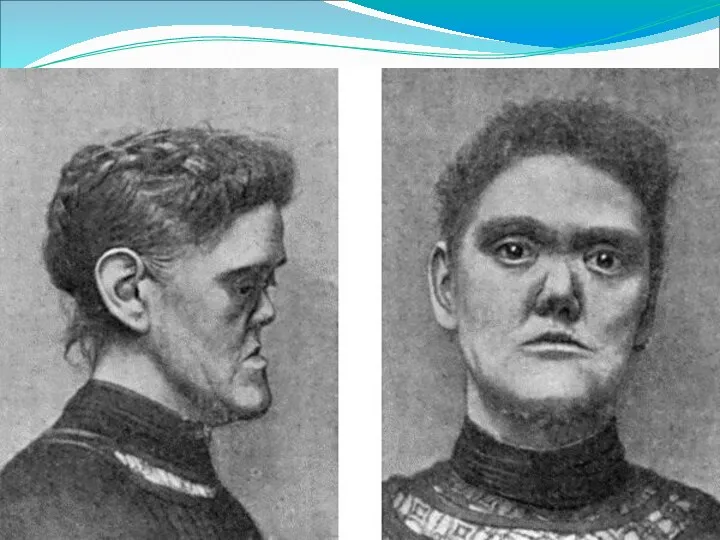
Слайд 67

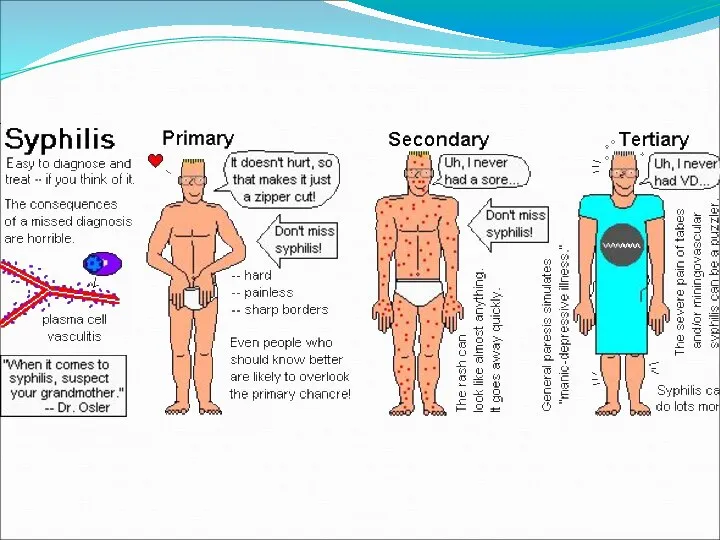
Primary syphilis
After an incubation period of 2 to 6 weeks following
exposure, a papule develops at the site of inoculation, which will then ulcerate into the characteristic syphilitic chancre (figure 9-11). The classic chancre is a painless, indurated ulcer with well-defined borders and a clean base. A chancre can develop on the oral (figure 11) or anorectal mucosa as well as in the genital mucosa (figure 9-10). Prior application of topical antibiotics or the use of systemic antimicrobials, may change the typical appearance of the lesion. Non-tender lymphadenopathy may be present.
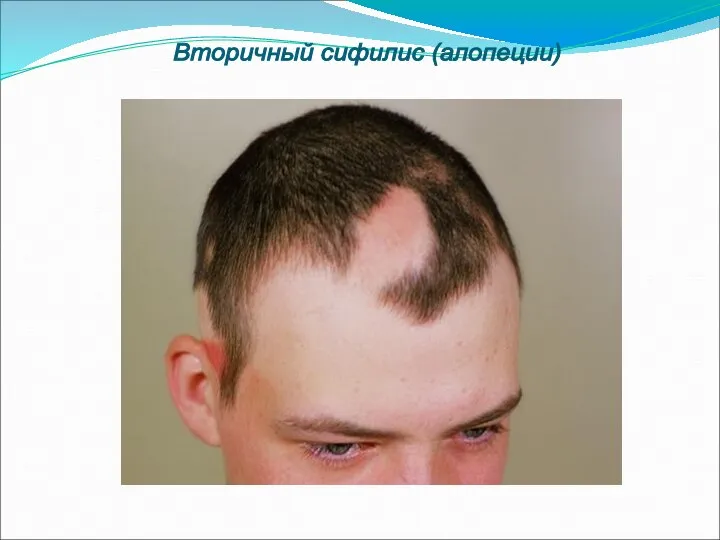
Secondary syphilis
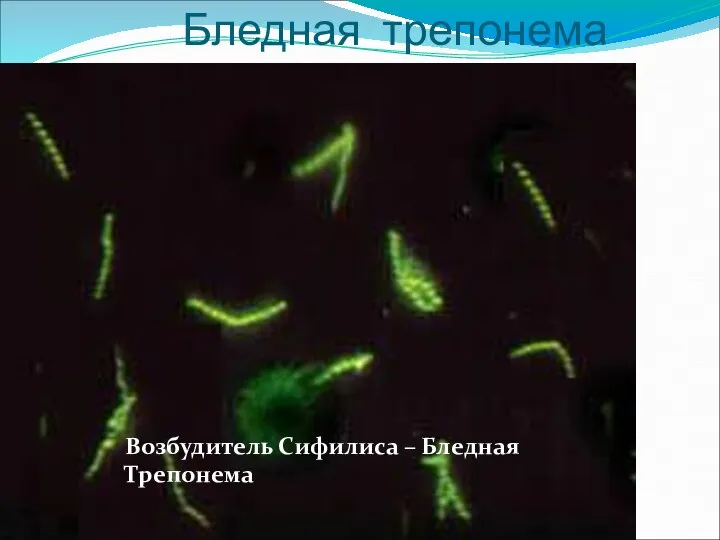
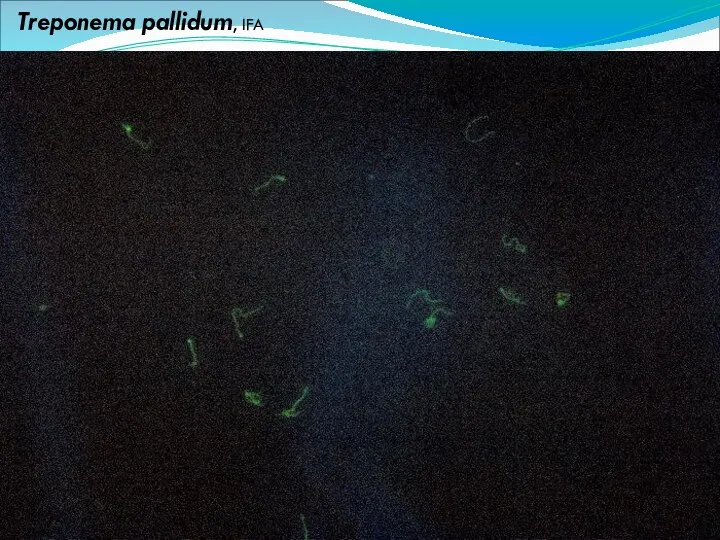
Approximately 60% to 90% of patients with untreated primary syphilis will develop manifestations of secondary syphilis. Secondary syphilis is a systemic disease that results from dissemination of the treponemes. Systemic symptoms include generalized lymphadenopathy, fever, headache, sore throat and arthralgias. Numerous clinical manifestations occur 4 to 10 weeks after the chancre disappears (or 2 to 6 months after sexual contact). These involve dermatologic (figure 12-13), central nervous system (aseptic meningitis, cranial neuropathy), ocular (iritis, uveitis or conjunctivitis), hepatic (hepatitis) and renal (immune complex glomerulonephritis) systems.
The most common manifestation of secondary syphilis is the skin rash characterized by maculesThe most common manifestation of secondary syphilis is the skin rash characterized by macules and papules The most common manifestation of secondary syphilis is the skin rash characterized by macules and papules distributed on the head and neck, the trunk and extremities including the palms and soles. The rash may be confused with pityriasis roseaThe most common manifestation of secondary syphilis is the skin rash characterized by macules and papules distributed on the head and neck, the trunk and extremities including the palms and soles. The rash may be confused with pityriasis rosea, psoriasis or drug eruption. Condyloma lata are large, raised whitish lesions that are seen in warm, moist areas which occur before or soon after the rash and are highly infectious. These need to be distinguished from condyloma acuminata of human papillomavirus infections. Mucous patches are shallow, painless ulcerations that can be found on the oral or anorectal mucosa.
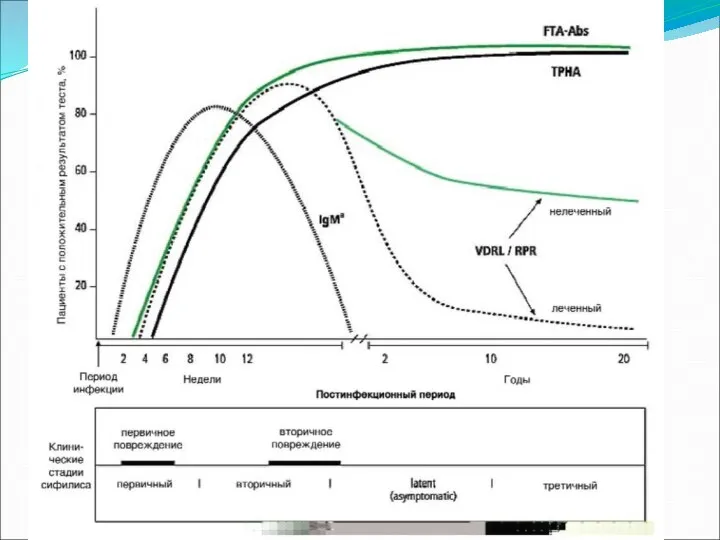
Latent syphilis
Latent syphilis is defined by reactive serology in the absence of clinical signs or symptoms. After resolution of early (primary or secondary) syphilis, mucocutaneous lesions can recur for up to 1 to 2 years in 25% of the patients. Early latent syphilis is defined as the first year from the suspected exposure when the patient is still at risk for relapse of the manifestations of secondary syphilis. Late latent syphilis is defined as a time period of one year or more after the primary infection and before the onset of tertiary syphilis.
Tertiary syphilis
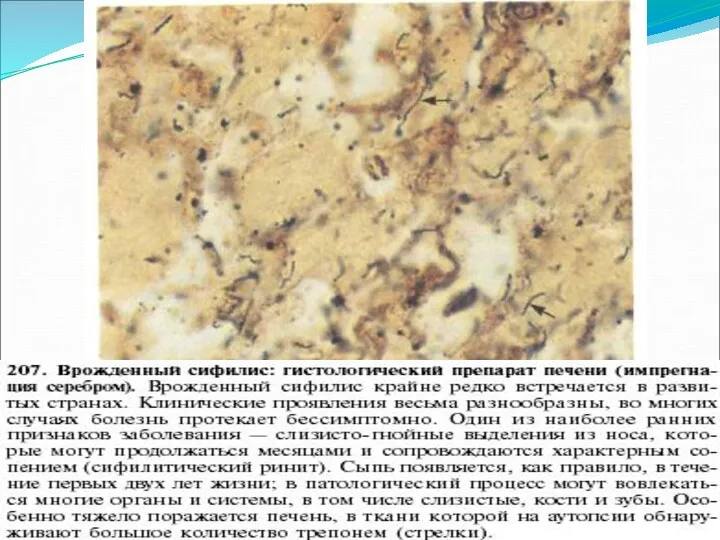
Tertiary syphilis or late syphilis can occur after primary, secondary or latent syphilis. In the pre-antibiotic era, 25% to 40% of all patients with syphilis developed tertiary syphilis. It may present with cardiovascular manifestations, gummatousTertiary syphilis or late syphilis can occur after primary, secondary or latent syphilis. In the pre-antibiotic era, 25% to 40% of all patients with syphilis developed tertiary syphilis. It may present with cardiovascular manifestations, gummatous lesions or CNS disease. Cardiovascular manifestations include aortic aneurysms, aortic insufficiency or coronary stenosis. Gummatous lesions are focal inflammatory areas that can involve any organ (e.g. the liver, figure 17) but usually involve the skin (figure 15-16) and bones. Neurological disease during the tertiary stage presents as general paresisTertiary syphilis or late syphilis can occur after primary, secondary or latent syphilis. In the pre-antibiotic era, 25% to 40% of all patients with syphilis developed tertiary syphilis. It may present with cardiovascular manifestations, gummatous lesions or CNS disease. Cardiovascular manifestations include aortic aneurysms, aortic insufficiency or coronary stenosis. Gummatous lesions are focal inflammatory areas that can involve any organ (e.g. the liver, figure 17) but usually involve the skin (figure 15-16) and bones. Neurological disease during the tertiary stage presents as general paresis or tabes dorsalis.
Neurosyphilis
Infection of the CNS by the treponemes can occur at any time during the course of syphilis infection. In 15% to 40% of patients with untreated primary and secondary syphilis, T. pallidum was found in the CSF by animal inoculation studies. Treponemal invasion of the CNS during untreated early syphilis may have the following outcomes: spontaneous resolution, asymptomatic neurosyphilis (at any time during syphilis infection), acute syphilitic meningitis (in the first year), meningovascular syphilis (5 to 12 years after primary infection), and parenchymatous neurosyphilis (18 to 25 years after primary infection).






























































 Ями на дорогах
Ями на дорогах Циклические алгоритмы. Оператор цикла For.Тело цикла
Циклические алгоритмы. Оператор цикла For.Тело цикла Sonja Gerhardt
Sonja Gerhardt Крест и крестное знамение
Крест и крестное знамение Повторение прошедших тем. Логические выражения
Повторение прошедших тем. Логические выражения Функции элементов нервной системы
Функции элементов нервной системы  Инновационная деятельность в образовании
Инновационная деятельность в образовании  Структура учебно-тренировочного процесса
Структура учебно-тренировочного процесса ГТО – это спорт! Спорт – это жизнь!
ГТО – это спорт! Спорт – это жизнь! коллекция русских икон
коллекция русских икон ТАКТИЧЕСКИЕ ХАРАКТЕРИСТИКИ, ВОЗМОЖНОСТИ И ОСОБЕННОСТИ ЭКСПЛУАТАЦИИ БРОНЕТЕХНИКИ, МОТОЦИКЛОВ, САМОЛЁТОВ И ВЕРТОЛЁТОВ, ИСПОЛЬЗУЕМ
ТАКТИЧЕСКИЕ ХАРАКТЕРИСТИКИ, ВОЗМОЖНОСТИ И ОСОБЕННОСТИ ЭКСПЛУАТАЦИИ БРОНЕТЕХНИКИ, МОТОЦИКЛОВ, САМОЛЁТОВ И ВЕРТОЛЁТОВ, ИСПОЛЬЗУЕМ Синдром жировой эмболии Проф. Н.Е.Буров
Синдром жировой эмболии Проф. Н.Е.Буров Анализ педагогических результатов на основе мониторинга учащихся средней школы ТИНУС ВАЛЕНТИНА МИХАЙЛОВНА учитель физической
Анализ педагогических результатов на основе мониторинга учащихся средней школы ТИНУС ВАЛЕНТИНА МИХАЙЛОВНА учитель физической Азбука архитектуры
Азбука архитектуры Презентация Фотографические принадлежности. Характеристика, классификация, ассортимент
Презентация Фотографические принадлежности. Характеристика, классификация, ассортимент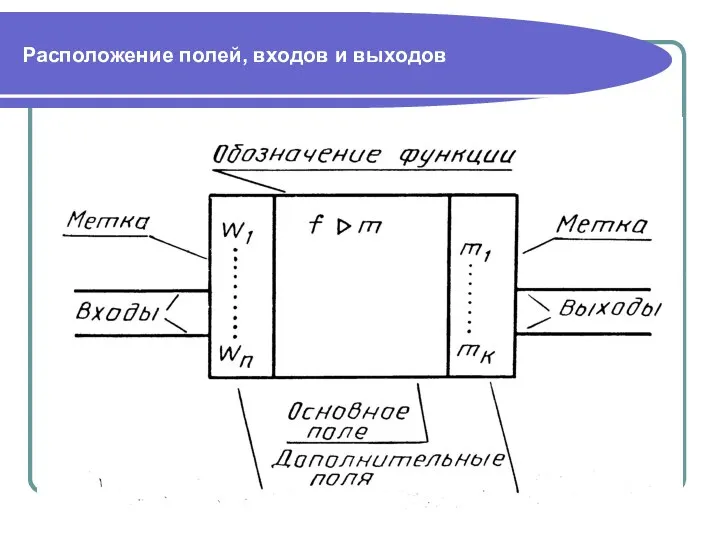 Аналоговые элементы
Аналоговые элементы Noel et Nouvel An en France. Traditions et coutumes
Noel et Nouvel An en France. Traditions et coutumes Единый урок прав человека
Единый урок прав человека Морфофункциональные особенности строения брюшины
Морфофункциональные особенности строения брюшины Земельные, водные и биологические ресурсы России Подготовила Студентка группы Э122б Арсёнова В.
Земельные, водные и биологические ресурсы России Подготовила Студентка группы Э122б Арсёнова В. Реорганизация структурных подразделений ОТ, ТБ и ООС КПО
Реорганизация структурных подразделений ОТ, ТБ и ООС КПО Формы правления. Формы государственно-территориального устройства. Политические режимы
Формы правления. Формы государственно-территориального устройства. Политические режимы Народные промыслы Центрального района России
Народные промыслы Центрального района России К доске
К доске Предмет исторической
Предмет исторической 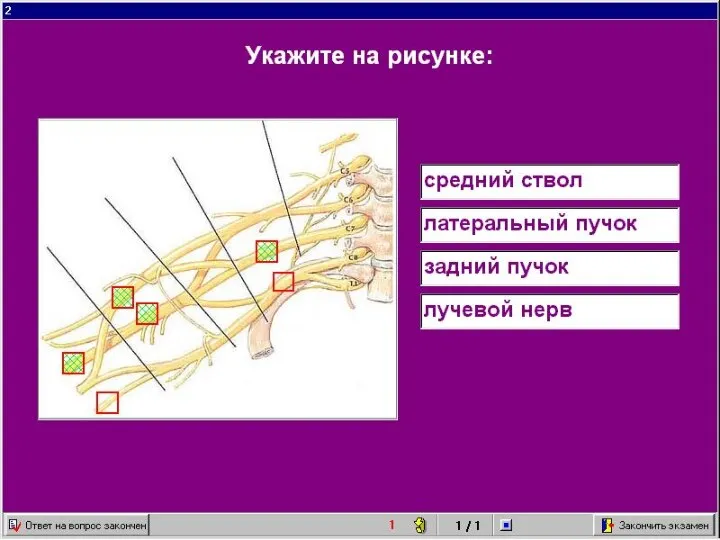 ангиология неврология
ангиология неврология 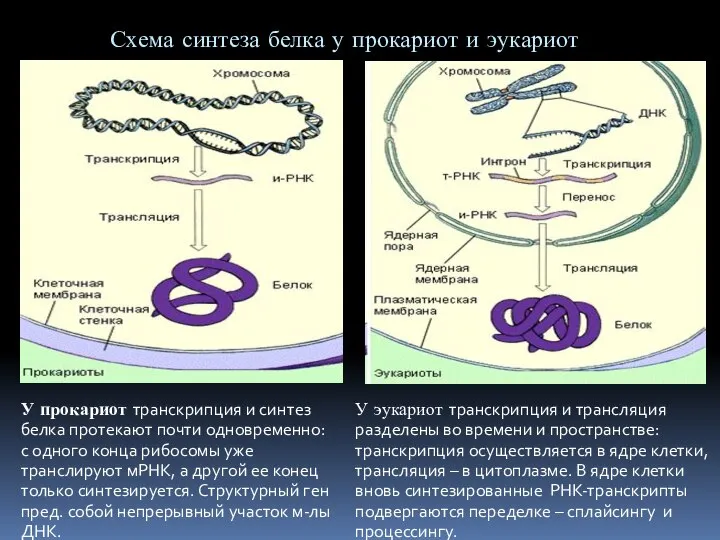 Регуляция синтеза белка
Регуляция синтеза белка Структура команд и режимы адресации на примере PDP-11
Структура команд и режимы адресации на примере PDP-11