Содержание
- 2. Sudden coronary death Angina pectoris Acute myocardial infarction Painless myocardial ischaemia Heart failure Disturbences of rhythm
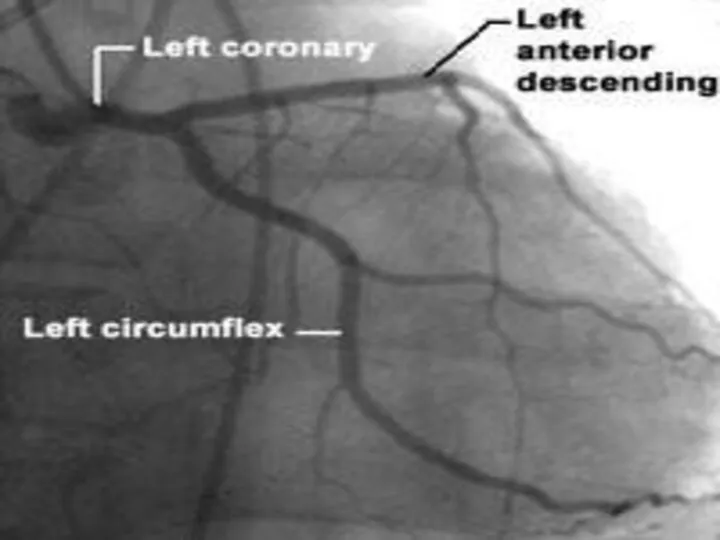
- 3. Ischaemic heart disease . Anterior Heart Arteries The coronary arteries supply blood to the heart muscle.
- 4. Ischaemic heart disease . Posterior Heart Arteries The coronary arteries supply blood to the heart muscle.
- 5. Ischaemic heart disease Ischaemic heart disease (Coronary artery disease) – is the most common form of
- 6. ANGINA PECTORIS-DEFINITION Angina pectoris is the clinical symptom complex caused by transient myocardial ischaemia and may
- 7. ANGINA PECTORIS-DEFINITION Angina pectoris is the medical term used to describe chest pains caused by poor
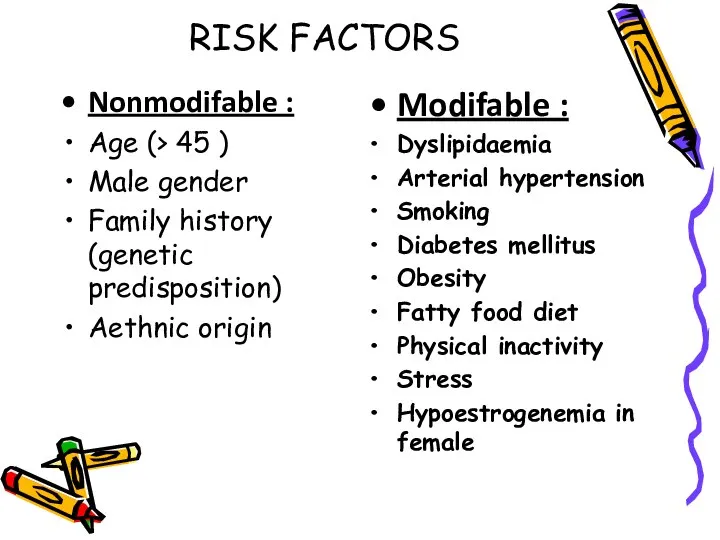
- 9. RISK FACTORS Nonmodifable : Age (> 45 ) Male gender Family history (genetic predisposition) Aethnic origin
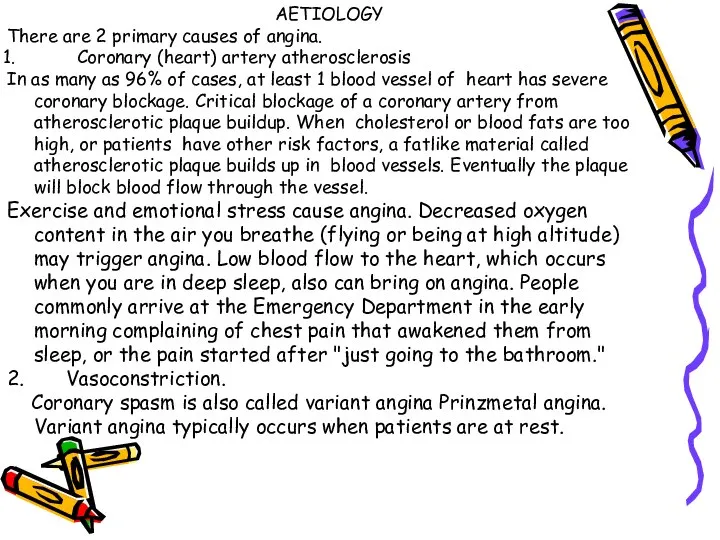
- 11. AETIOLOGY There are 2 primary causes of angina. Coronary (heart) artery atherosclerosis In as many as
- 13. INCIDENCE The incidence of angina continuously rises with age in women while in men the incidence
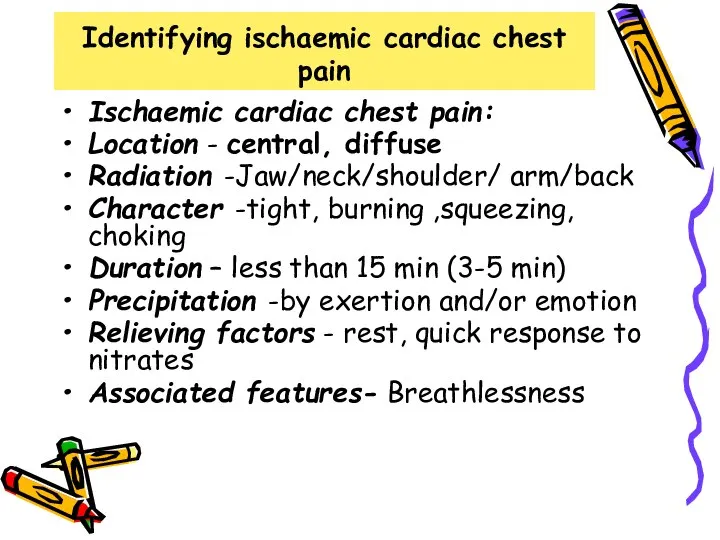
- 14. Identifying ischaemic cardiac chest pain Ischaemic cardiac chest pain: Location - central, diffuse Radiation -Jaw/neck/shoulder/ arm/back
- 15. SIGNS N SYMPTOMS These are signs and symptoms of angina as well: An uncomfortable pressure, fullness,
- 20. CLASSIFICATION Types of Angina Pectoris Stable Angina Unstable Angina Prinzmetal’s or variant angina Microvascular angina
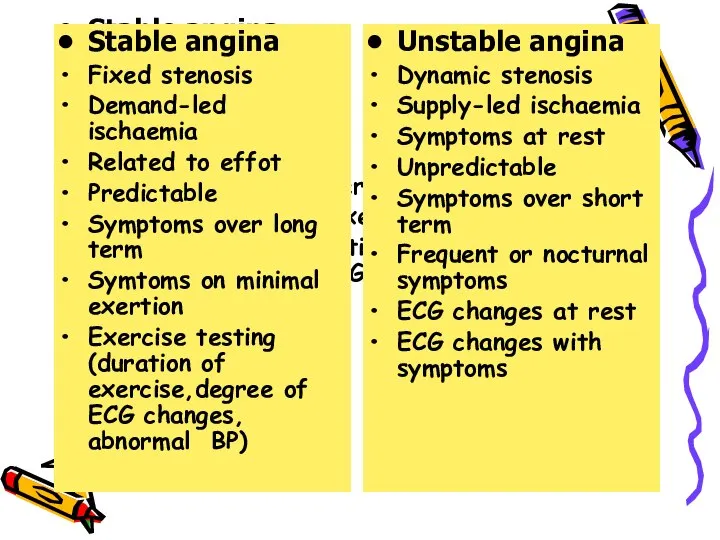
- 21. Stable Angina Stable angina is a repeating pattern of chest pain which has not changed in
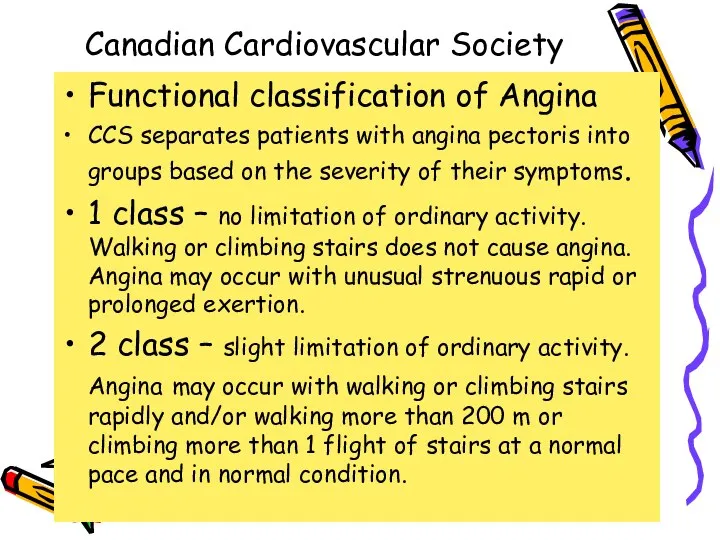
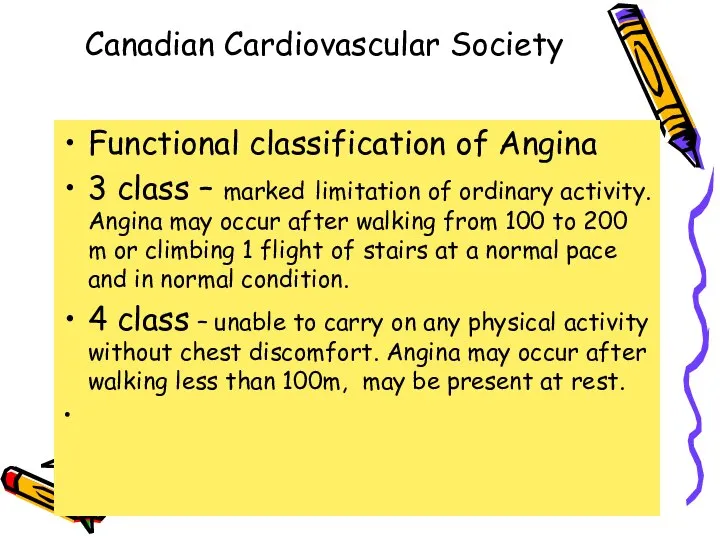
- 22. Сanadian Cardiovascular Society Functional classification of Angina ССS separates patients with angina pectoris into groups based
- 23. Сanadian Cardiovascular Society Functional classification of Angina 3 class – marked limitation of ordinary activity. Angina
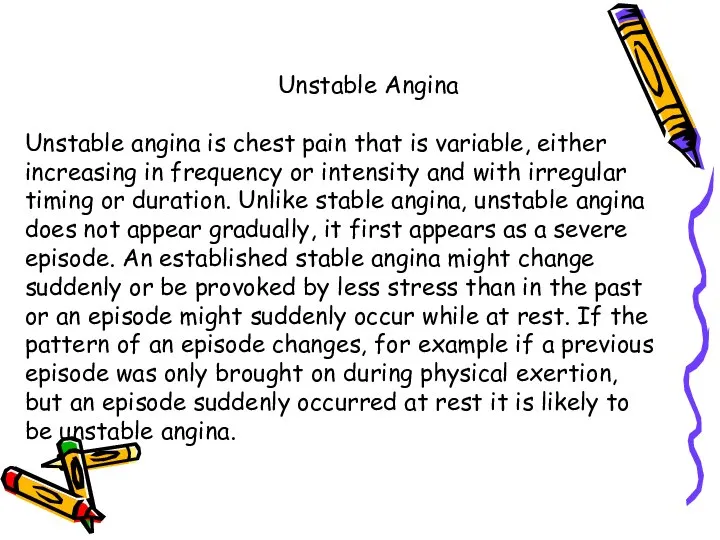
- 25. Unstable Angina Unstable angina is chest pain that is variable, either increasing in frequency or intensity
- 26. Unstable angina New onset angina pectoris – from first clinical signs of substernal anginal pain or
- 27. Stable angina Fixed stenosis Demand-led ischaemia Related to effot Predictable Symptoms over long term Symtoms on
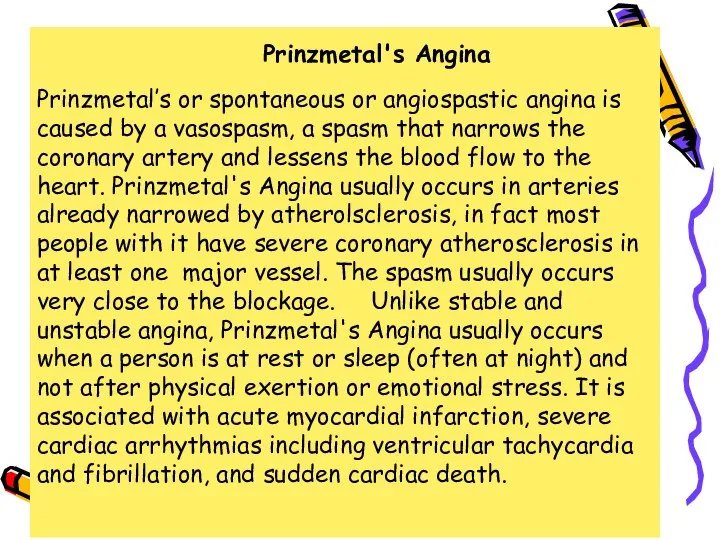
- 28. Prinzmetal's Angina Prinzmetal’s or spontaneous or angiospastic angina is caused by a vasospasm, a spasm that
- 29. Microvascular Angina or Stable Angina Pectoris on angiographycally intact vessels or Coronary Syndrome X Microvascular angina,
- 30. Coronary Syndrome X Characterized by 3 specific, typical signs as : Classic anginal chest pain ST
- 31. Terminology Clarification One major association between microvascular angina and the insulin resistance syndrome has arisen from
- 32. Diabetes and Angina Insulin resistance and secondary hyperinsulinemia are recognized risk factors for development of atherosclerosis.
- 33. Diagnosis The diagnosis of angina pectoris usually involves a careful assessment and history of signs and
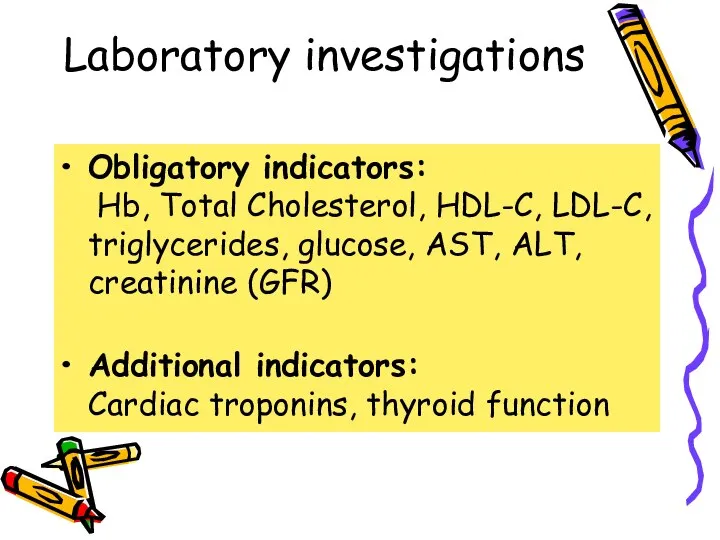
- 34. Laboratory investigations Obligatory indicators: Hb, Total Cholesterol, HDL-C, LDL-C, triglycerides, glucose, AST, ALT, creatinine (GFR) Additional
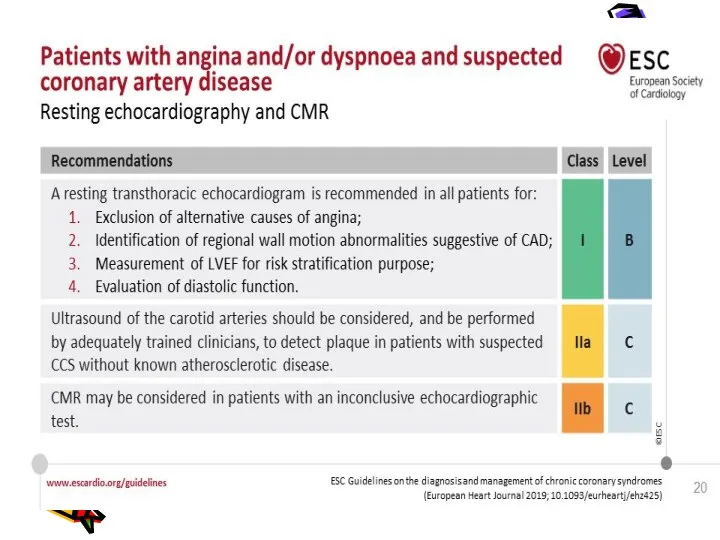
- 35. Investigations Resting ECG – reversible ST depression or elevation with or without T-wave inversion at the
- 36. Investigations Stress echocardiography – to identify ischaemic segments of myocardium and areas of infarction ( exhibit
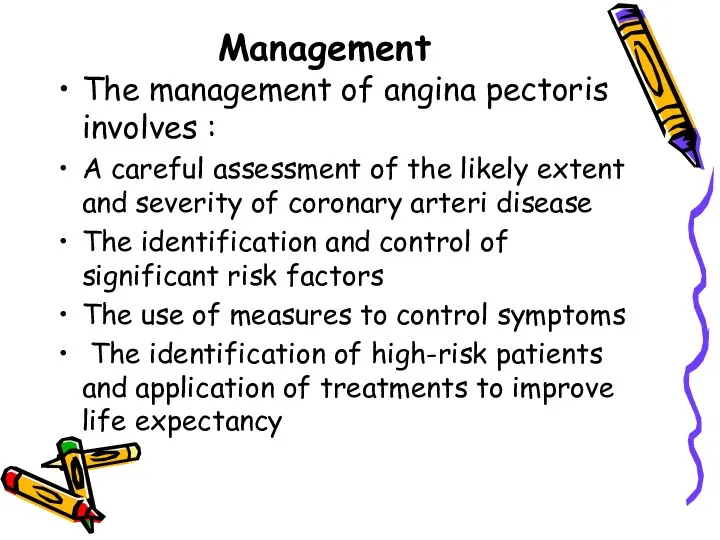
- 41. Management The management of angina pectoris involves : A careful assessment of the likely extent and
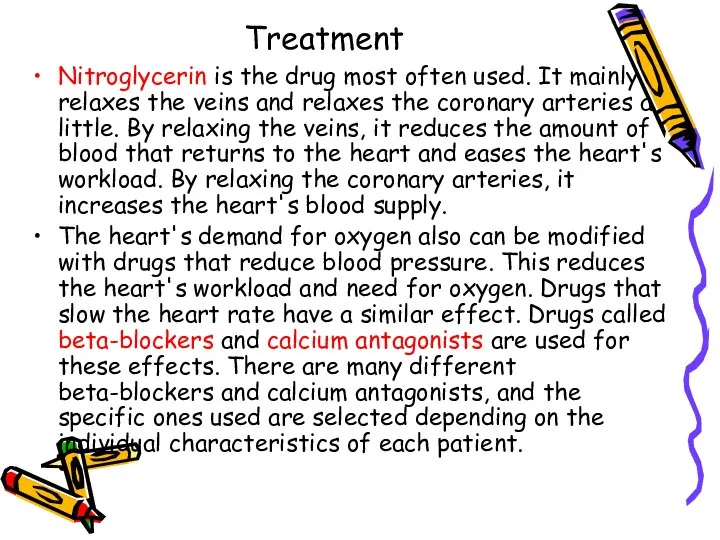
- 46. Treatment Nitroglycerin is the drug most often used. It mainly relaxes the veins and relaxes the
- 47. Anti-anginals - B- blockers -1st line (metoprolol,bisoprolol,nebivolol,carvedilol) - Calcium antagonists (verapamil , amlodipin,diltiazem if b-blockers contraindicated)
- 48. Treatment ANTI-ANGINAL DRUG TREATMENT – GROUPS OF DRUGS ARE USED TO HELP RELIEVE OR PREVENT THE
- 49. Drugs,which improve prognosis - Antiplatelet drugs (aspirin,clopidogrel ) - Statins (lovastatin,simvastatin, atorva-statin,rosuvastatin ) - B-blockers (atenolol,metaprolol,bisoprolol,nebivolol,
- 50. Treatment Controlling the risk factors for angina pectoris, such as high blood pressure, cigarette smoking, high
- 51. What procedures are used to treat angina? Invasive techniques that improve the heart and the heart's
- 52. Coronary artery bypass graft surgery is also used. In it, a blood vessel is used to
- 53. How is variant angina or Prinzmetal's angina treated? Calcium antagonists are extremely effective in preventing the
- 54. Medical Treatment If you have come to the hospital emergency department, you may be sent to
- 55. Medical Treatment Regardless of where you are sent, several basic treatments may be started. Which are
- 56. Medical Treatment Treatment will depend on the severity of symptoms, severity of the underlying disease, and
- 57. Medical Treatment You may be given medication to lower blood pressure or heart rate. Beta blockers,
- 58. Metabolic therapy - Trimetazidine (preductal) - Riboxin - Mildronate (vasonate) - Tiotriozaline - Vitamins - Antioxidantes
- 59. Medical Treatment After reviewing your immediate test results, the hospital health care provider will make a
- 60. Medical Treatment If you keep having symptoms or your condition is unstable, you will be admitted
- 61. INVASIVE TREATMENT Angioplasty is a treatment used for people whose angina does not get better with
- 62. INVASIVE TREATMENT The catheter is threaded through the arteries and into the artery where the narrowing
- 63. Percutaneous transluminal angioplasty (1, 2)
- 64. Percutaneous transluminal angioplasty (3, 4)
- 72. Скачать презентацию







































 Физиология послеродового периода
Физиология послеродового периода Профилактика курения
Профилактика курения Профилактика употребления ПАВ в подростковой среде
Профилактика употребления ПАВ в подростковой среде Аноректальные пороки развития у детей
Аноректальные пороки развития у детей Инфекция. Бактериялар мен вирустардың патогендігі және вируленттігі
Инфекция. Бактериялар мен вирустардың патогендігі және вируленттігі Сымбат пиелонефрит
Сымбат пиелонефрит Аптека под ногами
Аптека под ногами Родительские послания: 10 фраз, которые определяют жизнь человека
Родительские послания: 10 фраз, которые определяют жизнь человека ЛФК при переломах
ЛФК при переломах Этиология и патогенез лихорадки
Этиология и патогенез лихорадки Общая патология, как отрасль медицины
Общая патология, как отрасль медицины Лимфатическая система. Кровь. Тема 21. ч1
Лимфатическая система. Кровь. Тема 21. ч1 Болезни желудочно-кишечного тракта
Болезни желудочно-кишечного тракта Скелет головы
Скелет головы Пероральные сахароснижающие ЛС
Пероральные сахароснижающие ЛС Измерение артериального давления
Измерение артериального давления Дифференциальная диагностика при гепатомегалии
Дифференциальная диагностика при гепатомегалии Взаимосвязь толерантности и агрессивности
Взаимосвязь толерантности и агрессивности Клінічні прояви психічних захворювань і їх судово-психіатрична оцінка. Тема 3
Клінічні прояви психічних захворювань і їх судово-психіатрична оцінка. Тема 3 Авторская психотерапевтическая программа «дизайн человека совершенного»
Авторская психотерапевтическая программа «дизайн человека совершенного» Препараты гормонов и их синтетические аналоги
Препараты гормонов и их синтетические аналоги Терапия. Задача. Диагноз: ХОБЛ, GOLD II, mMRC-2, степень риска В, вне обострения
Терапия. Задача. Диагноз: ХОБЛ, GOLD II, mMRC-2, степень риска В, вне обострения Психологическая уравновешенность. Стресс и его влияние на человека
Психологическая уравновешенность. Стресс и его влияние на человека Оттискные материалы
Оттискные материалы Хронічна серцева недостатність. Визначення. Класифікація. Клініка. Діаганостика. Лікування
Хронічна серцева недостатність. Визначення. Класифікація. Клініка. Діаганостика. Лікування Функциональная биохимия нервной ткани
Функциональная биохимия нервной ткани ВИЧ-инфекция. Термины, открытие, устойчивость вируса
ВИЧ-инфекция. Термины, открытие, устойчивость вируса Рациональное вскармливание детей первого года жизни
Рациональное вскармливание детей первого года жизни