Содержание
- 2. Case 1 Your next patient in general practice is a 45 year old Mr. Snider who
- 3. history I’m sorry that your brother passed away recently. I know that it is hard. Assess
- 4. History Diet: what kind of food you eat What is your level of exercise? SAD and
- 5. Physical examination General Appearance - Acromegaly- bossing of forehead, Cyanosis Vitals – Normal BMI – normal
- 6. Investigations FBE, U&E, BSL lipid profile, serum uric acid, TFTs, ECG Stress test
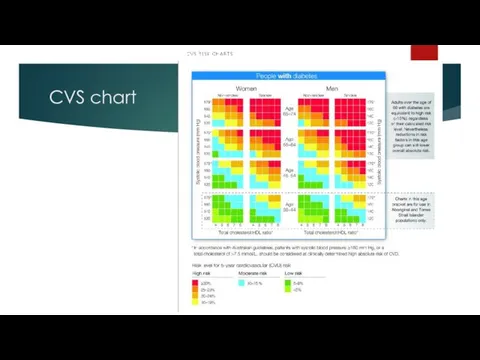
- 7. CVS chart
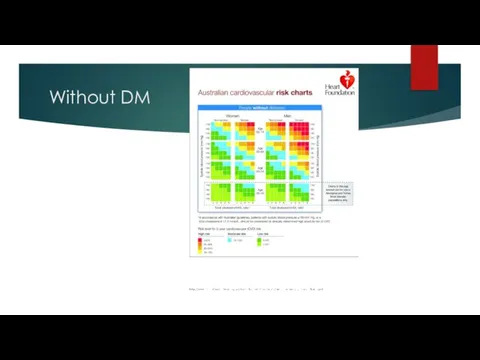
- 8. Without DM
- 9. Management All the investigations are normal. I could not find any abnormality in physical examination.. But
- 10. Management Alcohol – up to 2 standard drinks for 5 days a week Physical activity –
- 11. Case 2 A 63 year old car sales man, John, presents to the emergency department with
- 12. History John was woken up from an afternoon nap by sudden onset of severe, tearing pain
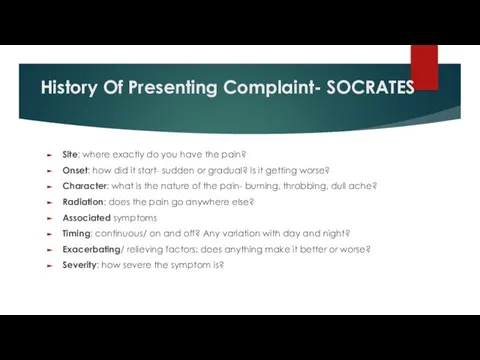
- 13. History Of Presenting Complaint- SOCRATES Site: where exactly do you have the pain? Onset: how did
- 14. Previous Episodes Is this the first episode or have you had similar episodes before? If previous
- 15. physical examination BP 155/100, no BP difference between right and left arm, P 78, RR 18,
- 16. Causes risk factors Bicuspid aortic disease Marfan syndrome and Ehlers-Danlos syndrome Other connective tissue disorders (Marfanoid)
- 17. Thoracic aortic dissection Aortic dissection is the tearing of the inner layer of the aortic wall,
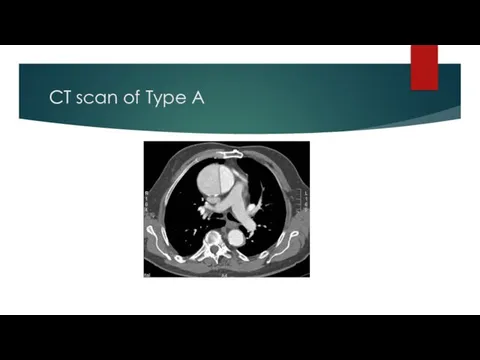
- 19. Management Supportive: A B C Oxygen Analgesia Monitoring Arterial/CVP lines Medical Management: BP reduction to 100
- 20. CT scan of Type A
- 21. Case 3 You have a middle-aged clerical male coming to your GP practice with a 1-day
- 22. Differentials PSGN IgA Nephropathy Bladder cancer Renal cell cancer PCKD
- 23. History How bad is it? When did it start? What is the kind of pain? Is
- 24. History Have you noticed bleeding from anywhere else such as bruising or nosebleed? Any problem with
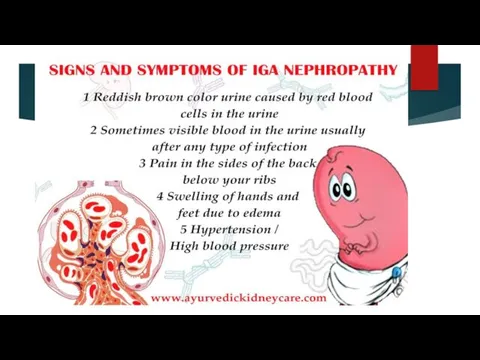
- 25. Explanation From the history most likely you have a condition called IgA nephropathy. Do you know
- 26. Mechanism
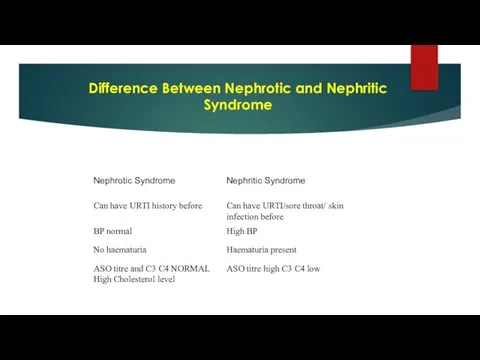
- 27. Difference Between Nephrotic and Nephritic Syndrome
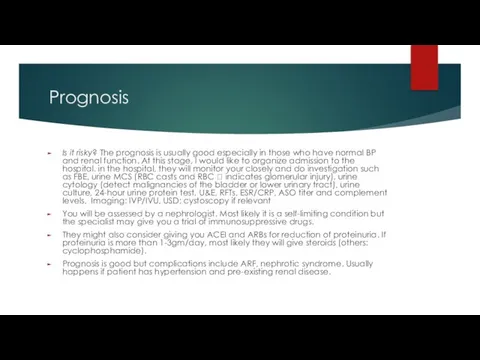
- 30. Prognosis Is it risky? The prognosis is usually good especially in those who have normal BP
- 31. Case 4 76 year old Mr. Aaron Samuels, who is your patient for last 7 years
- 32. AAA
- 33. Guideline
- 34. 5 A’s approach Hello Aaron, How have been from last week? Hmm, you are excited about
- 35. Risk factors Can be completely asymptomatic, but occasionally can give back or tummy pain. Familial Smoking
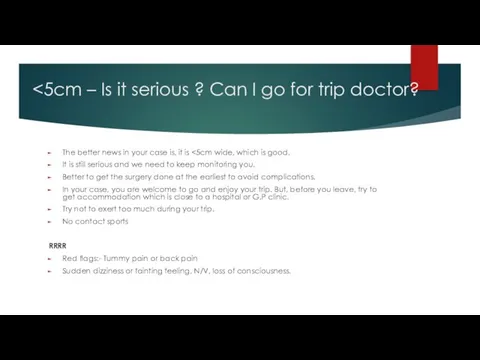
- 36. The better news in your case is, it is It is still serious and we need
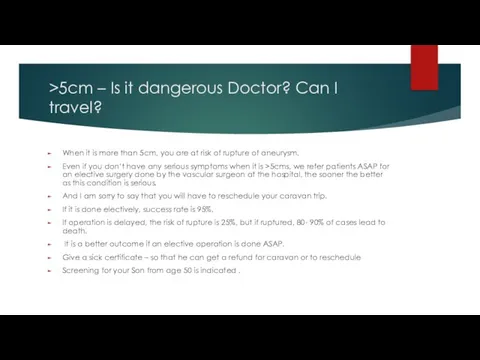
- 37. >5cm – Is it dangerous Doctor? Can I travel? When it is more than 5cm, you
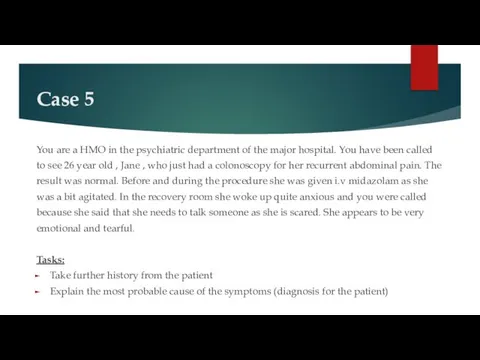
- 38. Case 5 You are a HMO in the psychiatric department of the major hospital. You have
- 39. History CONFIDENTIALITY HOPC Psychiatry H/O - PTSD, depression, suicidal ideas HEADSS – alcohol, drug use is
- 40. Acute Stress Disorder is the term used when symptoms develop within the first month after a
- 41. Management DO YOU WANT TO REPORT THIS TO THE POLICE, so that the person who assaulted
- 42. Case 6 GP, 24 years old woman who is pregnant come to see you complain of
- 43. History Any injury, any infection, any pain any exposure to very loud noise Did you need
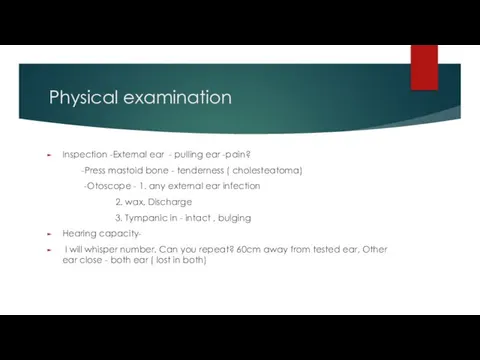
- 44. Physical examination Inspection -External ear - pulling ear -pain? -Press mastoid bone - tenderness ( cholesteatoma)
- 45. Examination Special test -Tunning fork ( 256 Hz) -Rinnie -mastoid and ear which one better? -Weber
- 47. weber’s test
- 48. causes of Sensorineural deafness -Cochlear degeneration -Acoustic neuroma -Drug -Ototoxicity - Streptomycin -Fracture of petrous temporal
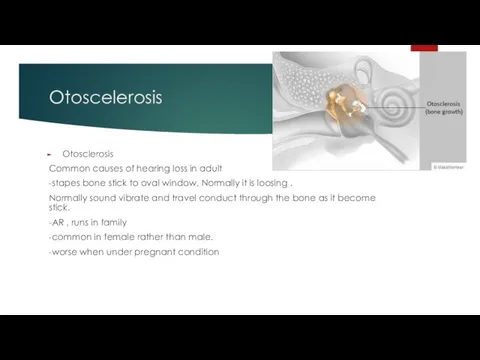
- 49. Otoscelerosis Otosclerosis Common causes of hearing loss in adult -stapes bone stick to oval window, Normally
- 50. Management hearing contain 2 parts - air conduction and nerve conduction. your cases is air conduction
- 51. Case 7 A young woman at 10 weeks’ gestational age comes to see you in your
- 52. History GM, I am Dr. XYZ… how are you today? I understand that you are here
- 53. History Reassure her that she will be monitored. Antenatal screening should be discussed with all pregnant
- 54. First trimester screening test Combined Test- ■ A non-fasting blood test which is done at 9-13
- 55. risk factor Information from the ultrasound scan is reported to the pathology laboratory to allow the
- 56. 2nd trimester screening test 15 -17 weeks-solely blood tests. – Triple test (a, b, e) (detection
- 57. In high-risk pregnancies, diagnostic tests: ■ CVS – Done ideally at 11-14 weeks. – A needle
- 58. patient questions Are the tests painful? Many women find the diagnostic tests uncomfortable, and they are
- 59. Case 8 In a GP setting. An 17 year-old boy complaining of pain in the tummy
- 60. Differential Duodenal injury Local abdominal hematoma Gall bladder injury Testicular torison UTI Gall stone Strangulated inguinal
- 61. History Vital stability of the child – B.P. -100/60, P.R- 120, RR- 35 & O2 –
- 62. History BINDS – Heel prick test was done ?( thyroid) Any concern about development? Family situation
- 63. Physical examination General appearance – distress & in pain , no signs of dehydration VS: -
- 64. Explanation Your son has a Duodenal injury in the tummy as I could see bruise patch
- 65. Case: 10 26 year old John has been brought by the police from a local pub
- 66. Assess patient’s injury, offer pain management CONFIDENTIALITY History Can you tell me what happened at the
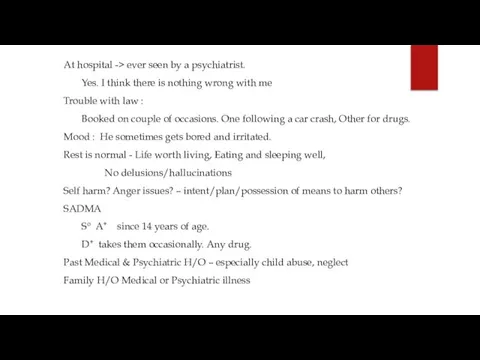
- 67. At hospital -> ever seen by a psychiatrist. Yes. I think there is nothing wrong with
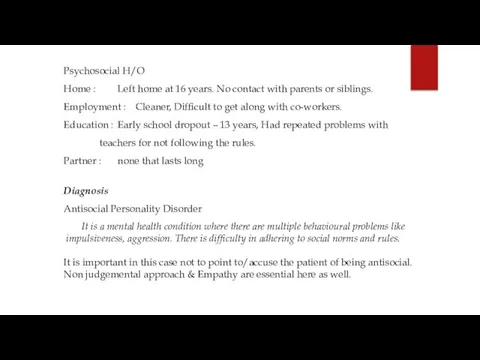
- 68. Psychosocial H/O Home : Left home at 16 years. No contact with parents or siblings. Employment
- 69. Management Difficulty to treat because of late presentation and lack of insight In this patient, get
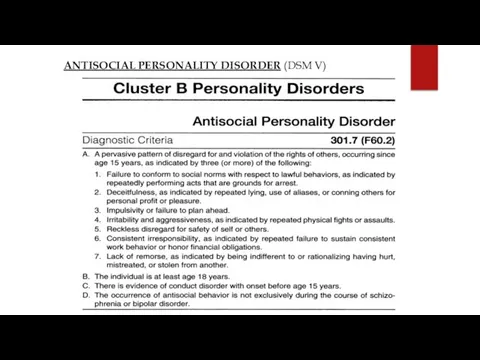
- 70. ANTISOCIAL PERSONALITY DISORDER (DSM V)
- 71. a mental disorder where a person shows no regard for right or wrong and is not
- 72. Symptoms Deceitfulness Non Conformity no respect for the law and have no boundaries. Impulsivity Aggression Irresponsibility
- 73. Reference https://wayahead.org.au/mental-health-information/fact-sheets/ mental-illness-and-related/antisocial-personality-disorder/
- 75. Скачать презентацию











































 Основы формирования здоровья детей: от 1 года до 3 лет
Основы формирования здоровья детей: от 1 года до 3 лет Сестринская помощь при вегетососудистой дистонии. Лекция 10
Сестринская помощь при вегетососудистой дистонии. Лекция 10 Энтеровирусная инфекция (ЭВИ) у детей
Энтеровирусная инфекция (ЭВИ) у детей Ультразвуковая диагностика заболеваний молочных желёз
Ультразвуковая диагностика заболеваний молочных желёз Синдром Бругада
Синдром Бругада Жировая эмболия
Жировая эмболия Партнерские роды
Партнерские роды Психика и сознание
Психика и сознание Еңбек жағдайын гигиеналықфизиологиялық бағалау: еңбектің ауырлығымен қарқындылығын, зияндылығы мен қауіптілігін
Еңбек жағдайын гигиеналықфизиологиялық бағалау: еңбектің ауырлығымен қарқындылығын, зияндылығы мен қауіптілігін Кумарины. Лекарственные растения и сырье, содержащие кумарины
Кумарины. Лекарственные растения и сырье, содержащие кумарины Вклад научных достижений кафедры хирургии в повышении качества медико-социальной экспертизы
Вклад научных достижений кафедры хирургии в повышении качества медико-социальной экспертизы Кровотечения в последовом и раннем послеродовом периодах
Кровотечения в последовом и раннем послеродовом периодах Миеломная болезнь (плазмоцитома)
Миеломная болезнь (плазмоцитома) Общение как взаимодействие. Интерактивная сторона общения
Общение как взаимодействие. Интерактивная сторона общения Основы микробиологии, санитарии и гигиены в пищевом производстве
Основы микробиологии, санитарии и гигиены в пищевом производстве Теория мотивации Д. Катца и Р. Кана
Теория мотивации Д. Катца и Р. Кана Парацельс – основатель ятрохимии
Парацельс – основатель ятрохимии Оптимизация процесса предоставления медицинской услуги в республиканской стоматологии
Оптимизация процесса предоставления медицинской услуги в республиканской стоматологии Первая помощь при прочих состояниях (ожоги, обморожения, отравления)
Первая помощь при прочих состояниях (ожоги, обморожения, отравления) О вкусном и полезном питании
О вкусном и полезном питании Виды лечения опухолей
Виды лечения опухолей Нановакцины и нанолекарства
Нановакцины и нанолекарства Трансплантация тарихы
Трансплантация тарихы Профилактика рака желудка
Профилактика рака желудка Сестринская помощь при артериальной гипертонии. Тема 4.2
Сестринская помощь при артериальной гипертонии. Тема 4.2 Анатомия, кровоснабжение, иннервация, физиология поджелудочной железы
Анатомия, кровоснабжение, иннервация, физиология поджелудочной железы Психология управленческой деятельности
Психология управленческой деятельности Наркомания
Наркомания