Содержание
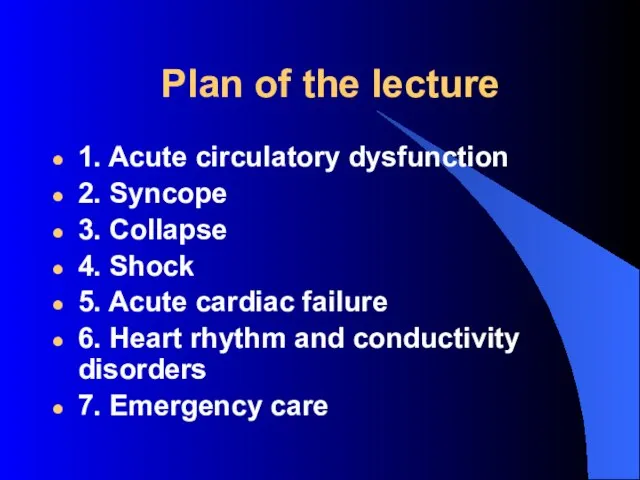
- 2. Plan of the lecture 1. Acute circulatory dysfunction 2. Syncope 3. Collapse 4. Shock 5. Acute
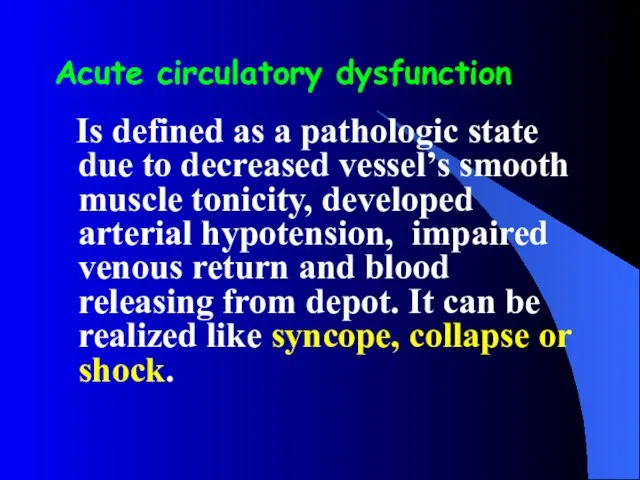
- 3. Acute circulatory dysfunction Is defined as a pathologic state due to decreased vessel’s smooth muscle tonicity,
- 4. Syncope - Is sudden short-term loss of conscience with muscle tonicity loss due to transient cerebral
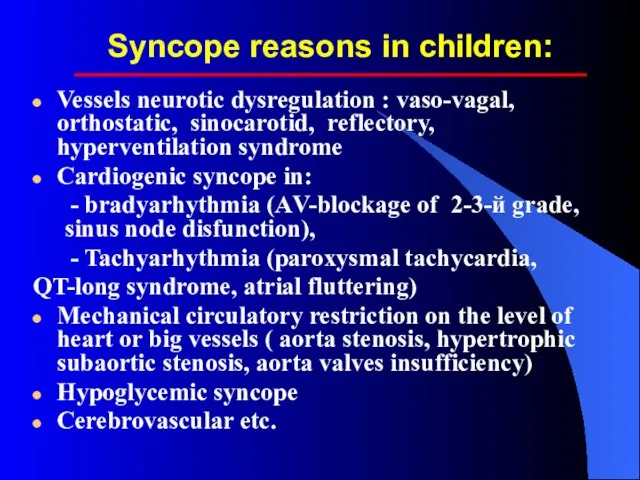
- 5. Syncope reasons in children: Vessels neurotic dysregulation : vaso-vagal, orthostatic, sinocarotid, reflectory, hyperventilation syndrome Cardiogenic syncope
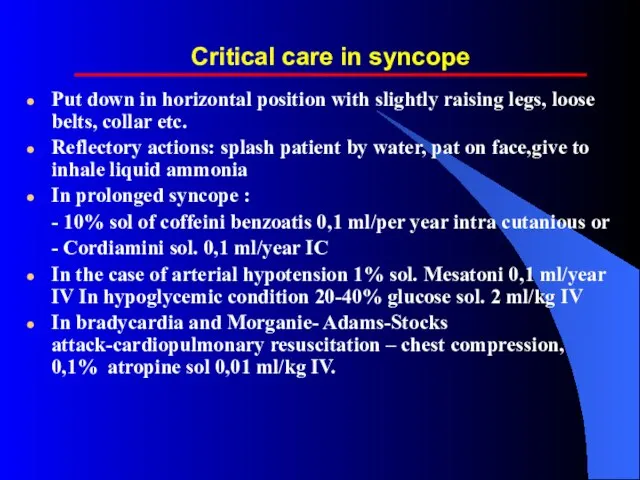
- 6. Critical care in syncope Put down in horizontal position with slightly raising legs, loose belts, collar
- 7. Collapse - Life threatening acute vascular insufficiency with acute vessel dystonia, circulatory blood volume decrease, signs
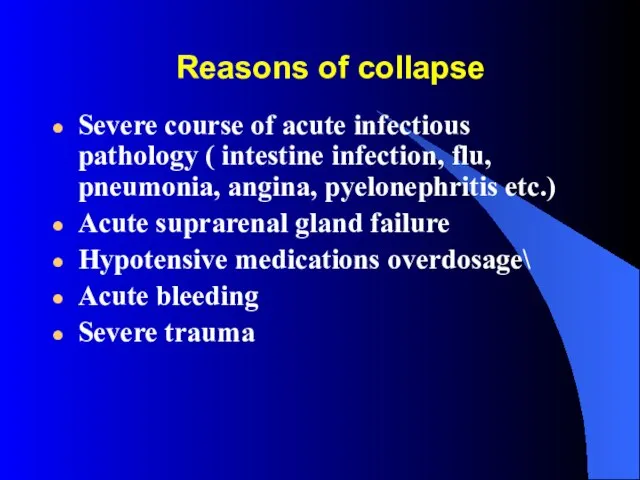
- 8. Reasons of collapse Severe course of acute infectious pathology ( intestine infection, flu, pneumonia, angina, pyelonephritis
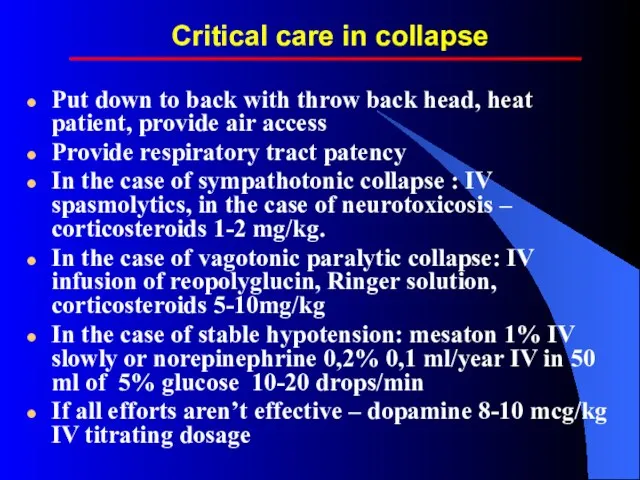
- 9. Critical care in collapse Put down to back with throw back head, heat patient, provide air
- 10. SHOCK Acute threatening life pathologic process characterized by progressive tissue perfusion diminishing, subsequent CNS impaired functioning,
- 11. Reasons of shock Decreasing of circulatory volume (hypovolemic shock): due to bleeding, dehydration, burns, etc. Main
- 12. Critical care in shock Put down in horizontal position with slightly raising legs, moisturized oxygen To
- 13. Acute cardiac failure Pathologic condition characterized by cardiac output decreasing due to myocardial pumping function reduction
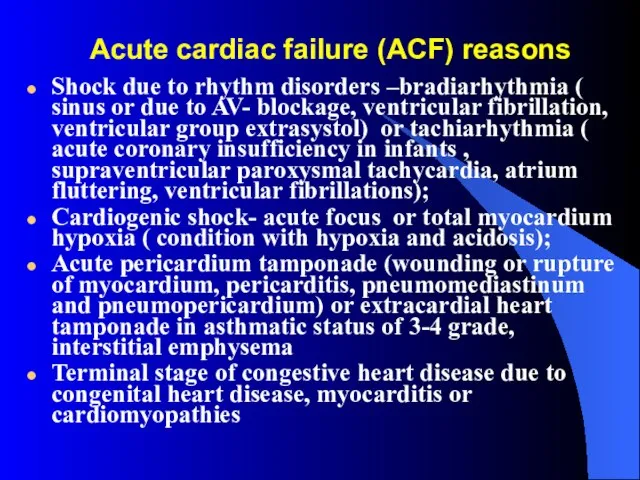
- 14. Acute cardiac failure (ACF) reasons Shock due to rhythm disorders –bradiarhythmia ( sinus or due to
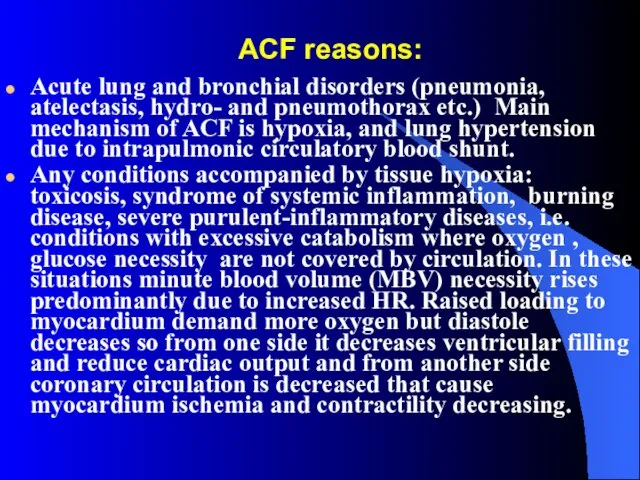
- 15. ACF reasons: Acute lung and bronchial disorders (pneumonia, atelectasis, hydro- and pneumothorax etc.) Main mechanism of
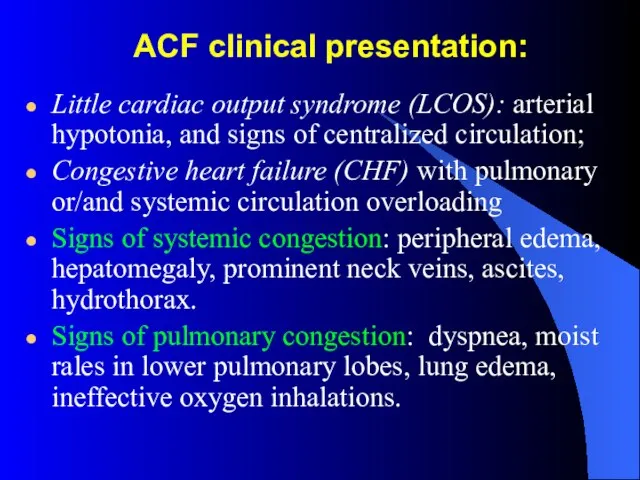
- 16. ACF clinical presentation: Little cardiac output syndrome (LCOS): arterial hypotonia, and signs of centralized circulation; Congestive
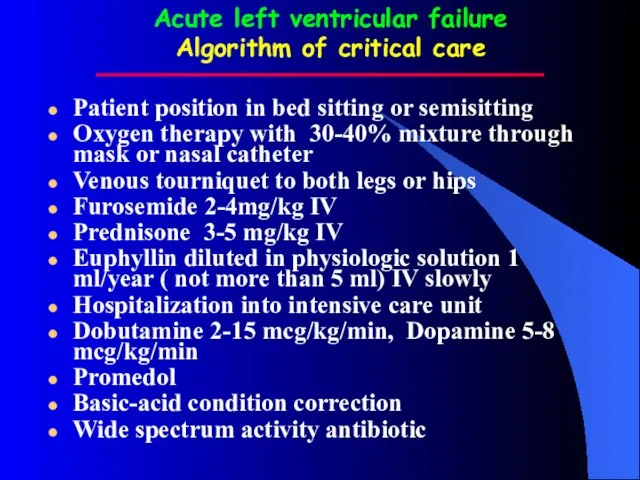
- 17. Acute left ventricular failure Algorithm of critical care Patient position in bed sitting or semisitting Oxygen
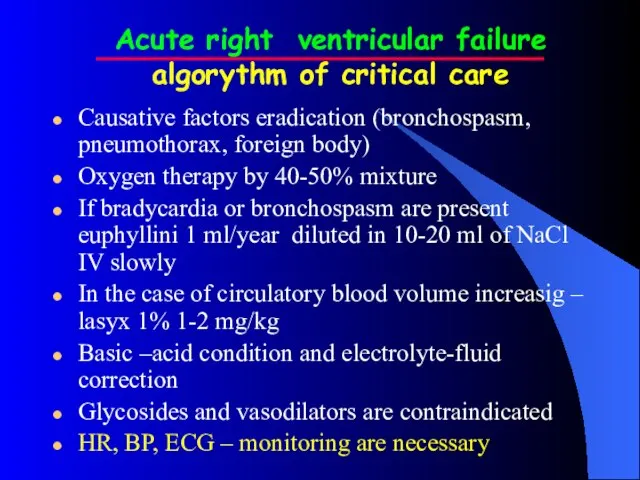
- 18. Acute right ventricular failure algorythm of critical care Causative factors eradication (bronchospasm, pneumothorax, foreign body) Oxygen
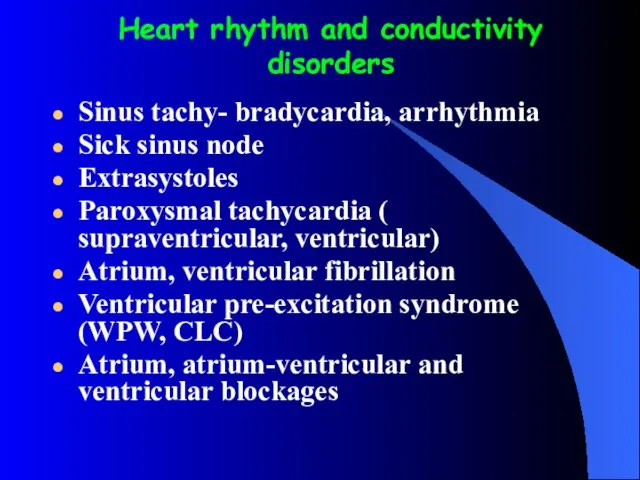
- 19. Heart rhythm and conductivity disorders Sinus tachy- bradycardia, arrhythmia Sick sinus node Extrasystoles Paroxysmal tachycardia (
- 20. Arrhythmia treatment Pharmacologic medications Reflectory methods Psycho-physical methods Electrical methods Surgical methods
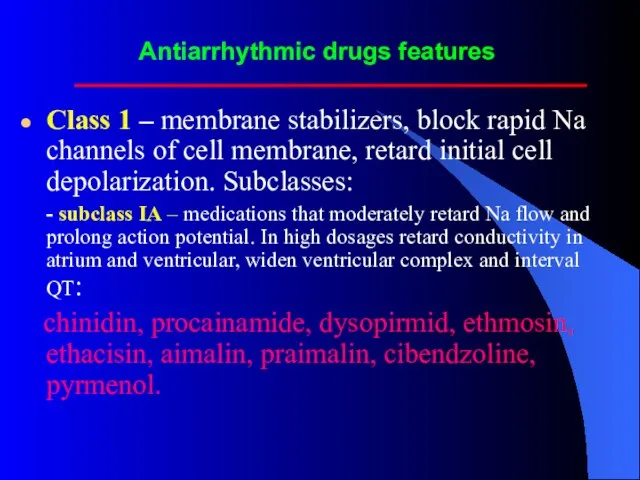
- 21. Antiarrhythmic drugs features Class 1 – membrane stabilizers, block rapid Na channels of cell membrane, retard
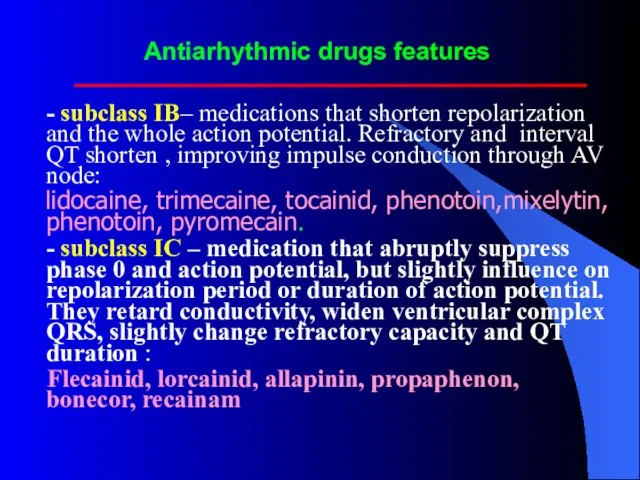
- 22. Antiarhythmic drugs features - subclass IВ– medications that shorten repolarization and the whole action potential. Refractory
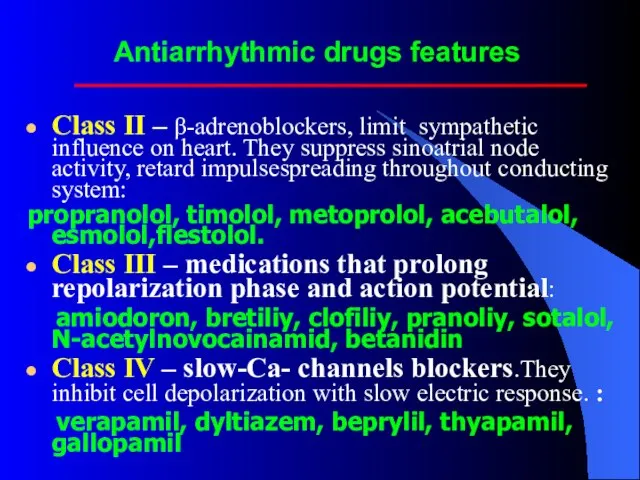
- 23. Antiarrhythmic drugs features Class II – β-adrenoblockers, limit sympathetic influence on heart. They suppress sinoatrial node
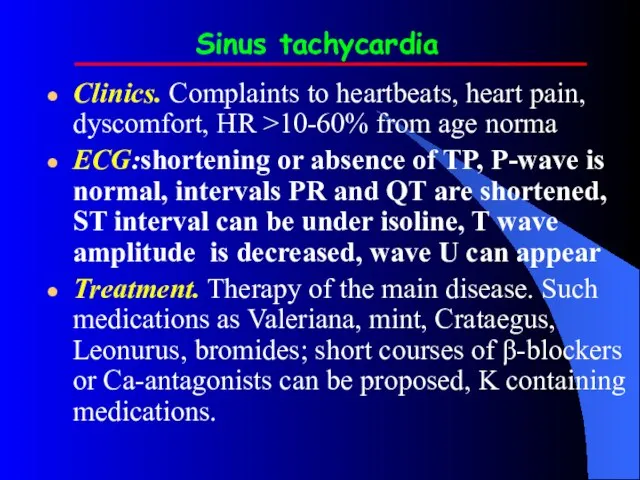
- 24. Sinus tachycardia Clinics. Complaints to heartbeats, heart pain, dyscomfort, HR >10-60% from age norma ECG:shortening or
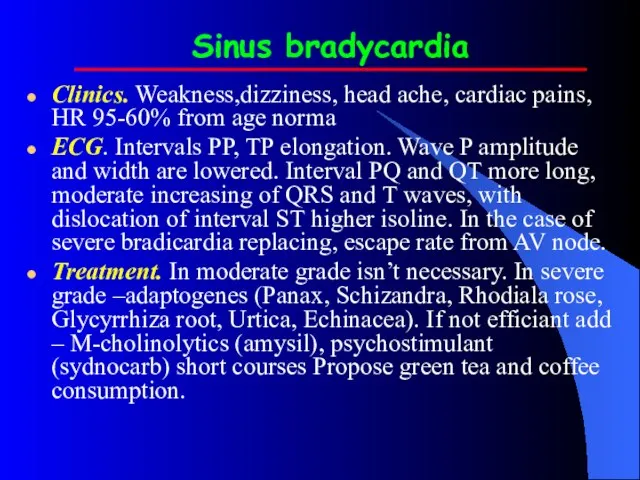
- 25. Sinus bradycardia Clinics. Weakness,dizziness, head ache, cardiac pains, HR 95-60% from age norma ECG. Intervals РР,
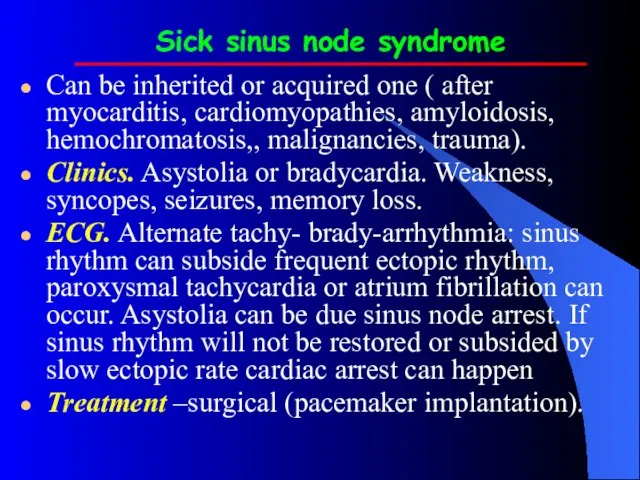
- 26. Sick sinus node syndrome Can be inherited or acquired one ( after myocarditis, cardiomyopathies, amyloidosis, hemochromatosis,,
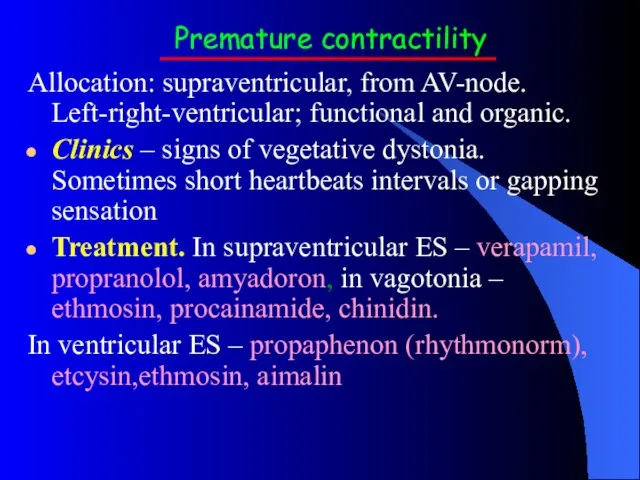
- 27. Premature contractility Allocation: supraventricular, from AV-node. Left-right-ventricular; functional and organic. Clinics – signs of vegetative dystonia.
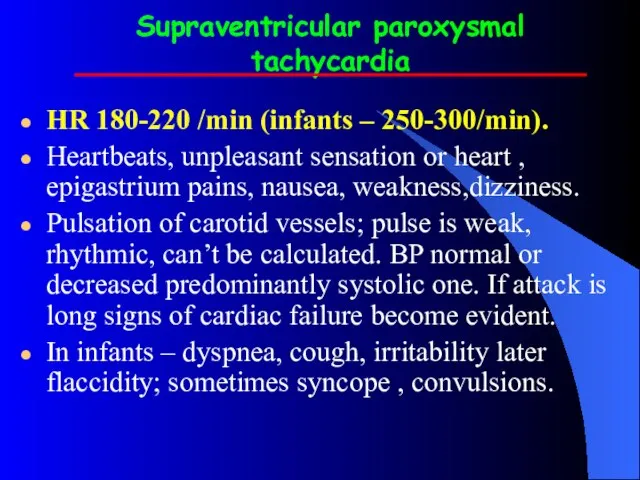
- 28. Supraventricular paroxysmal tachycardia HR 180-220 /min (infants – 250-300/min). Heartbeats, unpleasant sensation or heart , epigastrium
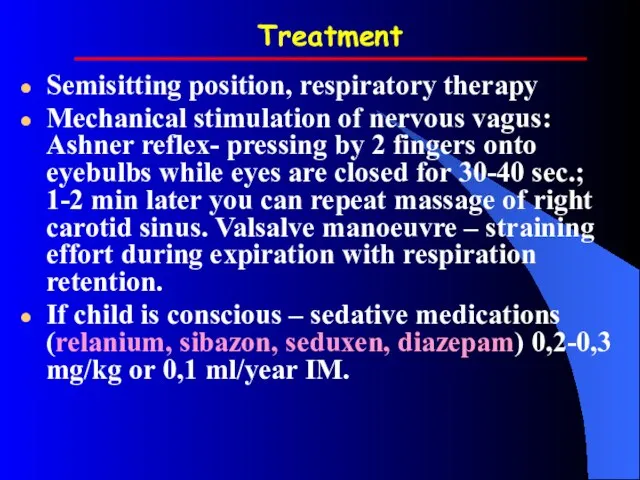
- 29. Treatment Semisitting position, respiratory therapy Mechanical stimulation of nervous vagus: Ashner reflex- pressing by 2 fingers
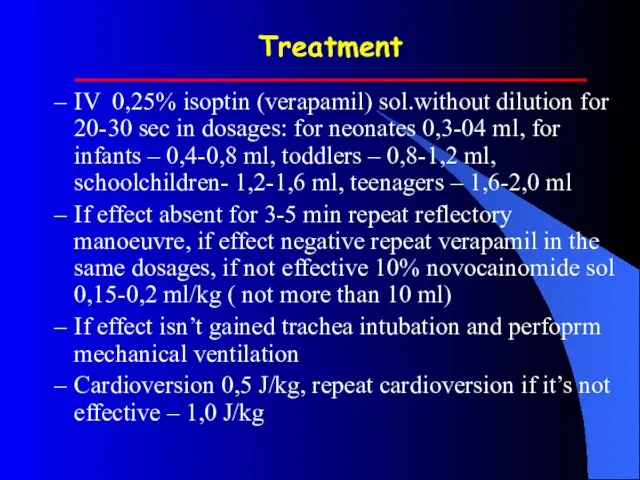
- 30. Treatment IV 0,25% isoptin (verapamil) sol.without dilution for 20-30 sec in dosages: for neonates 0,3-04 ml,
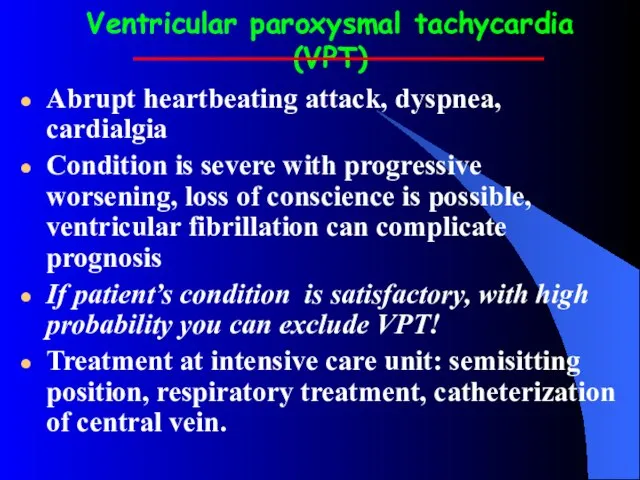
- 31. Ventricular paroxysmal tachycardia (VPT) Abrupt heartbeating attack, dyspnea, cardialgia Condition is severe with progressive worsening, loss
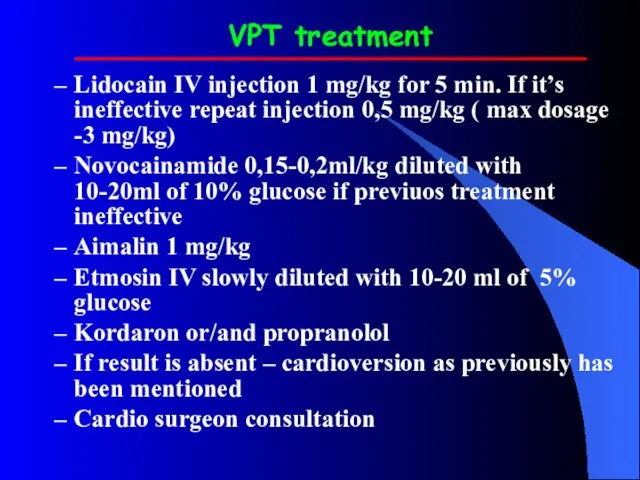
- 32. VPT treatment Lidocain IV injection 1 mg/kg for 5 min. If it’s ineffective repeat injection 0,5
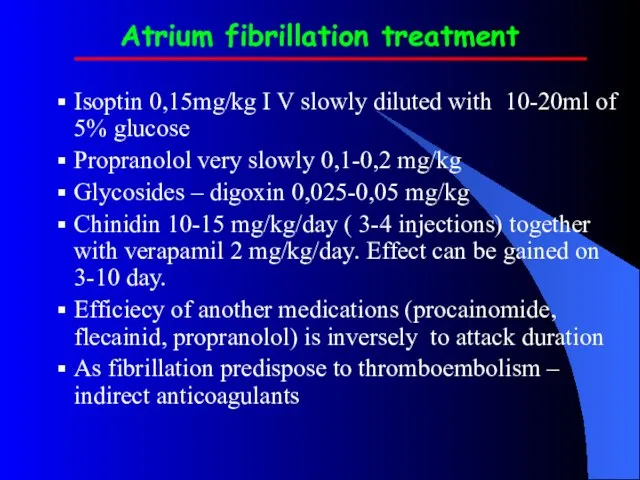
- 33. Atrium fibrillation treatment Isoptin 0,15mg/kg I V slowly diluted with 10-20ml of 5% glucose Propranolol very
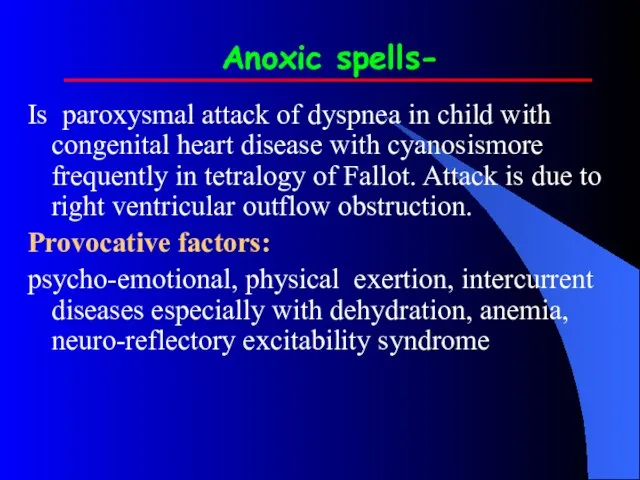
- 34. Anoxic spells- Is paroxysmal attack of dyspnea in child with congenital heart disease with cyanosismore frequently
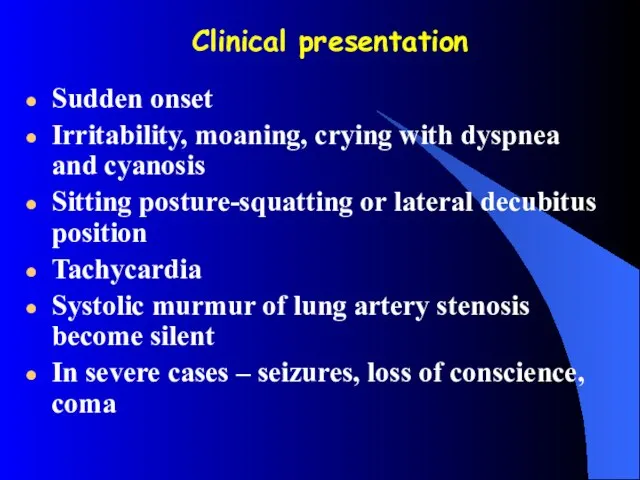
- 35. Clinical presentation Sudden onset Irritability, moaning, crying with dyspnea and cyanosis Sitting posture-squatting or lateral decubitus
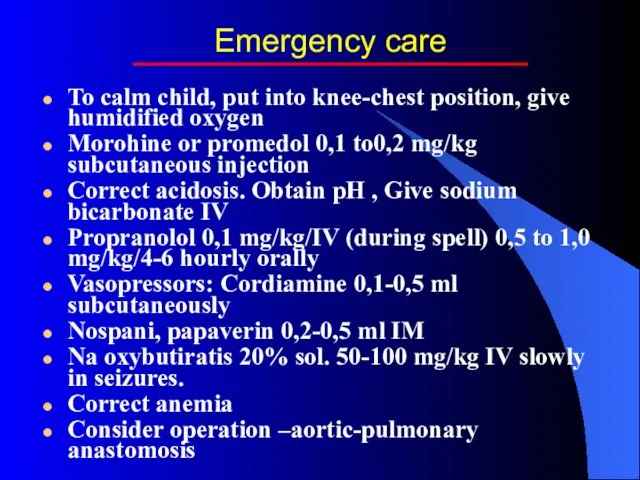
- 36. Emergency care To calm child, put into knee-chest position, give humidified oxygen Morohine or promedol 0,1
- 38. Скачать презентацию
 Санитарно-гигиенические требования к организации питания в организациях для детей-сирот
Санитарно-гигиенические требования к организации питания в организациях для детей-сирот Основные варианты задержки психического развития
Основные варианты задержки психического развития Функции участкового педиатра
Функции участкового педиатра Типичная форма (ангинозный)
Типичная форма (ангинозный) Тест по теме: Эндокринная система
Тест по теме: Эндокринная система Тест на определение темперамента
Тест на определение темперамента Информация по компании Интертич для ТОО Болашак Атырау
Информация по компании Интертич для ТОО Болашак Атырау Психология семейных отношений
Психология семейных отношений Практика графологического исследования
Практика графологического исследования Основные факторы, влияющие на уровень материнской смертности
Основные факторы, влияющие на уровень материнской смертности Алгоритм при обнаружении очаговых образований в легких
Алгоритм при обнаружении очаговых образований в легких Crimea state medical academy named
Crimea state medical academy named Патологическая физиология пищеварения
Патологическая физиология пищеварения Мед.катастроф Лекция №8 СДС
Мед.катастроф Лекция №8 СДС Презентация по медицине Сахарный диабет»
Презентация по медицине Сахарный диабет»  Витамин K
Витамин K Urok_zdorovya_v_3V_red
Urok_zdorovya_v_3V_red Оценка тяжести состояния пациентов с острым панкреатитом
Оценка тяжести состояния пациентов с острым панкреатитом Болезни губ и языка у детей
Болезни губ и языка у детей Введение в неонатологию. Организация медицинской помощи новорожденным детям
Введение в неонатологию. Организация медицинской помощи новорожденным детям Патофизиология клетки. Гипоксия
Патофизиология клетки. Гипоксия Гастростомия
Гастростомия Трихофития
Трихофития Ультразвуковая ангиология. Некоторые особенности диагностики и лечения ХНМК
Ультразвуковая ангиология. Некоторые особенности диагностики и лечения ХНМК Акушерский перитонит
Акушерский перитонит Лекция №4. Патология реактивности нарушения иммунной системы, аллергия
Лекция №4. Патология реактивности нарушения иммунной системы, аллергия Проблема создания единых представлений об условиях труда
Проблема создания единых представлений об условиях труда Перитонит
Перитонит