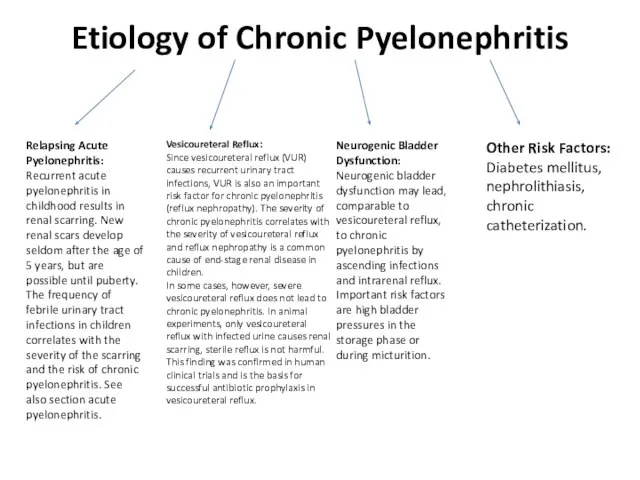
Etiology of Chronic Pyelonephritis
Relapsing Acute Pyelonephritis:
Recurrent acute pyelonephritis in childhood results
in renal scarring. New renal scars develop seldom after the age of 5 years, but are possible until puberty. The frequency of febrile urinary tract infections in children correlates with the severity of the scarring and the risk of chronic pyelonephritis. See also section acute pyelonephritis.
Vesicoureteral Reflux:
Since vesicoureteral reflux (VUR) causes recurrent urinary tract infections, VUR is also an important risk factor for chronic pyelonephritis (reflux nephropathy). The severity of chronic pyelonephritis correlates with the severity of vesicoureteral reflux and reflux nephropathy is a common cause of end-stage renal disease in children.
In some cases, however, severe vesicoureteral reflux does not lead to chronic pyelonephritis. In animal experiments, only vesicoureteral reflux with infected urine causes renal scarring, sterile reflux is not harmful. This finding was confirmed in human clinical trials and is the basis for successful antibiotic prophylaxis in vesicoureteral reflux.
Neurogenic Bladder Dysfunction:
Neurogenic bladder dysfunction may lead, comparable to vesicoureteral reflux, to chronic pyelonephritis by ascending infections and intrarenal reflux. Important risk factors are high bladder pressures in the storage phase or during micturition.
Other Risk Factors:
Diabetes mellitus, nephrolithiasis, chronic catheterization.

 Bronchial asthma
Bronchial asthma СПИД и его профилактика
СПИД и его профилактика Неотложные состояния в эндокринологии
Неотложные состояния в эндокринологии Спортивный массаж
Спортивный массаж Язвенная болезнь
Язвенная болезнь Результаты применения ремаксола при проведении полихимиотерапии
Результаты применения ремаксола при проведении полихимиотерапии Современные методы обследования и диагностики больного в клинике ортопедической стоматологии. Психотерапевтическая подготовка
Современные методы обследования и диагностики больного в клинике ортопедической стоматологии. Психотерапевтическая подготовка Заболевания печени
Заболевания печени Невропатология детского возраста. Частная невропатология
Невропатология детского возраста. Частная невропатология Периодонтиты
Периодонтиты Острая зоонозная инфекция лептоспироз
Острая зоонозная инфекция лептоспироз Гигиена-основная профилактическая дисциплина
Гигиена-основная профилактическая дисциплина Личная гигиена пациента
Личная гигиена пациента Общая классификация психотропных средств
Общая классификация психотропных средств Этические проблемы ВИЧ-инфекции
Этические проблемы ВИЧ-инфекции Балалардағы ходжкин лимфомасы. Заманауи анықтау және емдеу әдістері
Балалардағы ходжкин лимфомасы. Заманауи анықтау және емдеу әдістері Оказания первой помощи при переломах
Оказания первой помощи при переломах Детский алкоголизм
Детский алкоголизм Климактерический синдром
Климактерический синдром Болезнь Брилля
Болезнь Брилля Постембріональний розвиток людини
Постембріональний розвиток людини Особенности реабилитации спортсменов после травм и заболеваний опорно-двигательного аппарата
Особенности реабилитации спортсменов после травм и заболеваний опорно-двигательного аппарата Первая медицинская помощь пострадавшим от АХОВ
Первая медицинская помощь пострадавшим от АХОВ Риногенные орбитальные и внутричерепные осложнения
Риногенные орбитальные и внутричерепные осложнения Память и основная методика запоминания информации
Память и основная методика запоминания информации Логические диаграммы (методы) для развития умственных способностей
Логические диаграммы (методы) для развития умственных способностей Фантомный курс. Биомеханизм родов
Фантомный курс. Биомеханизм родов Применение стимулирующих макроэлектродов (лекция 6)
Применение стимулирующих макроэлектродов (лекция 6)