Содержание
- 2. Parameters Classification, etiology and mechanism of hypoxia Alterations of metabolism and function in the body Pathophysiological
- 3. parameters PO2 CO2max CO2 SO2 P50
- 4. PO2 partial pressure of oxygen PO2 is the tension produced by the oxygen molecules physically dissolved
- 5. CO2max oxygen binding capacity of hemoglobin CO2max refers to the maximal amount of oxygen that could
- 6. CO2 oxygen content CO2 includes oxygen that is bound to hemoglobin and physically dissolved in the
- 7. SO2 oxygen saturation SO2 is the percentage of hemoglobin present as oxyhemoglobin . Normal value: SaO2:
- 8. The relation between oxygen partial pressure and oxygen saturation is shown as oxygen dissociation curve (ODC).
- 9. P50 means the oxygen partial pressure required to saturate 50% of the hemoglobin, which reflects the
- 10. Classification, etiology, mechanism of hypoxia Hypotonic hypoxia Hemic hypoxia Circulatory hypoxia Histogenous hypoxia
- 11. Hypotonic hypoxia hypoxic hypoxia Hypotonic hypoxia is characterized by the decrease of PaO2(less than 60mmHg).
- 12. Etiology and mechanism Decreased PO2 of inspired air high altitude External respiratory dysfunction hypoventilation impaired diffusion
- 13. Characteristics of blood oxygen PaO2↓, SaO2↓, CaO2 ↓, CO2max N, CaO2-CvO2 ↓/N Cyanosis refers to the
- 14. Hemic hypoxia isotonic hypoxia Hemic hypoxia refers to the altered affinity of Hb for oxygen or
- 15. Etiology and mechanism Anemia Carbon monoxide poisoning CO can react with Hb to form carboxyhemoglobin which
- 16. Methemoglobinemia The ferrous state (Fe2+) in Hb may be oxidized to the ferric state (Fe3+) under
- 17. when a lot of pickled vegetables containing nitrate are taken, the reabsorbed nitrite reacts with HbFe2+
- 18. High affinity of Hb for O2 Alkaline solution Depot blood
- 19. Characteristics of blood oxygen PaO2 N, SaO2N, CaO2 ↓/N, CO2max ↓/N, CaO2-CvO2 ↓ CaO2-CvO2 is below
- 20. Circulatory hypoxia hypokinetic hypoxia Circulatory hypoxia refers to inadequate blood flow leading to inadequate oxygenation of
- 21. Etiology and mechanism Tissue ischemia shock, left heart failure, thrombosis, arterial stenosis Tissue congestion shock, right
- 22. PaO2N, SaO2N, CaO2 N, CO2max N, CaO2-CvO2 ↑ Characteristics of blood oxygen Because the blood flows
- 23. Histogenous hypoxia Histogenous hypoxia refers to the tissue cells can not make use of the oxygen
- 24. Etiology and mechanism Inhibition of oxidative phosphorylation - tissue intoxicity cyanides, sulphuret, rotenone, ( cytochrome oxidase)
- 25. Characteristics of blood oxygen PaO2 N, SaO2N, CaO2 N, CO2max N, CaO2-CvO2 ↓ Oxygen content in
- 26. Alterations of metabolism and function Respiratory system Circulatory system Hematologic system Central nervous system Tissues and
- 27. Respiratory system Compensatory response Low PaO2 stimulates the chemoreceptor in carotid and aortic body, which reflexly
- 28. High altitude pulmonary edema Central respiratory failure respiratory inhibition, irregular respiratory rhythm and frequency, hypoventilation, e.g.
- 29. Circulatory system Compensatory response Increased cardiac output hyperventilation and pulmonary expansion stimulate lung stretch receptors, which
- 30. Redistribution of blood vasodilatation : heart and brain hypoxia metabolites, lactic acid, adenosine Ca2+ influx↓ vasoconstriction
- 31. Injury manifestation Pulmonary hypertension Decreased diastolic and systolic myocardial function Arrhythmia Vagus Nerve Decreased venous return
- 32. Hematologic system Compensatory response Increase in the amount of RBCs and Hb More EPO produced and
- 33. Plasma viscosity↑, blood flow resistance ↑, afterload of heart ↑ When PO2 is low markedly, 2,3-DPG
- 34. Central nervous system Acute hypoxia: headache, agitation, poor faculty of memory, inability to make judgment, depress
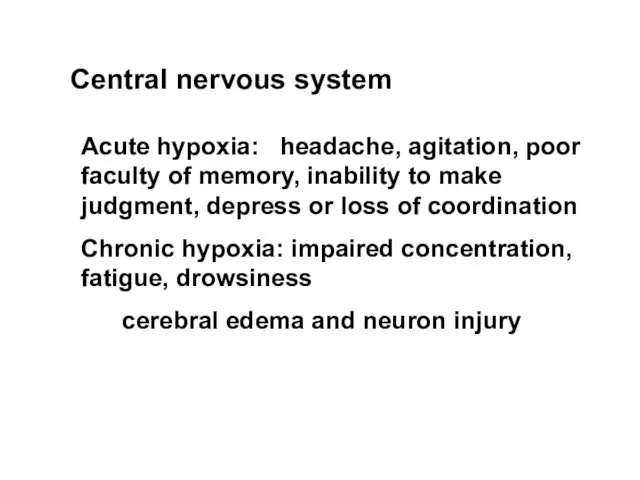
- 35. Tissues and cells Compensatory response Enhanced cell capacity for use of oxygen number and membrane surface
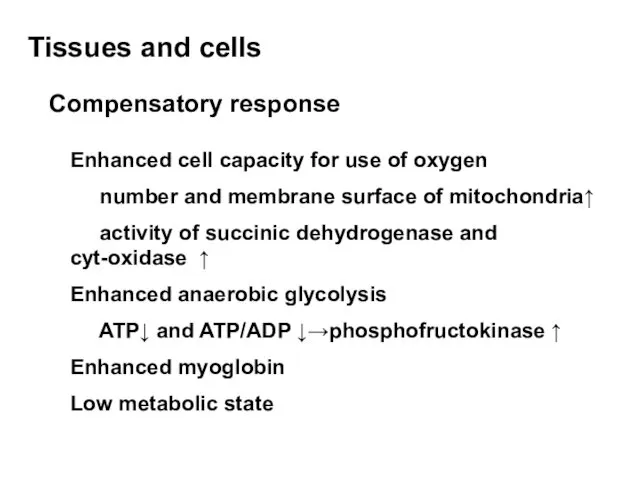
- 36. Injury manifestation Cell membrane injury Na+ influx cell swelling K+ efflux synthetic disorder Ca2+ influx phospholipase
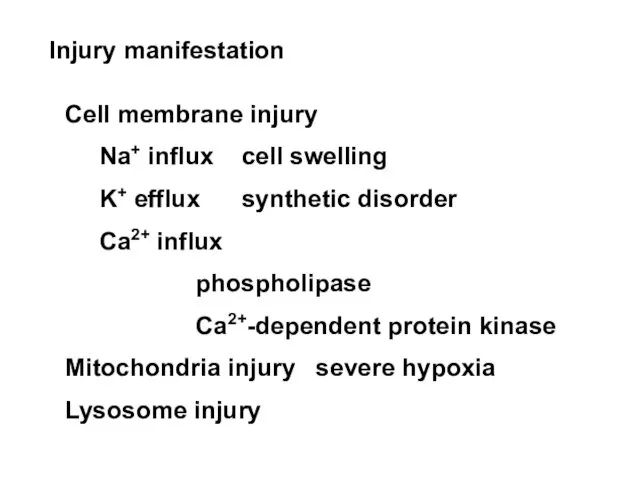
- 38. Скачать презентацию
 Стоматологические проявления при ЖДА
Стоматологические проявления при ЖДА Заболевания ротовой полости, вызванные микроорганизмами
Заболевания ротовой полости, вызванные микроорганизмами Детские инфекции
Детские инфекции Законы, регулирующие лечение психически больных в государстве израиль
Законы, регулирующие лечение психически больных в государстве израиль Цитокины, основные характеристики. Перспективы и проблемы цитокиновой/антицитокиновой терапии
Цитокины, основные характеристики. Перспективы и проблемы цитокиновой/антицитокиновой терапии Управление талантами, как стратегия регионального развития
Управление талантами, как стратегия регионального развития Инфекция. Инфекционный процесс
Инфекция. Инфекционный процесс Организация системы сбора и удаления медицинских отходов
Организация системы сбора и удаления медицинских отходов Аутоиммунные заболевания кожи
Аутоиммунные заболевания кожи Эпилепсия. Патогенез. Этиология
Эпилепсия. Патогенез. Этиология Введение в фармацевтическую биоэтику
Введение в фармацевтическую биоэтику Хейлопластикаға көрсеткіш,реабилитация, диспансеризация
Хейлопластикаға көрсеткіш,реабилитация, диспансеризация Роговица глаза. Аномалии развития роговицы
Роговица глаза. Аномалии развития роговицы Хроническое воспаление слюнных желез
Хроническое воспаление слюнных желез Здоровый образ жизни и правильное питание студентов
Здоровый образ жизни и правильное питание студентов Колесо и Белка: как простроить взаимоотношения
Колесо и Белка: как простроить взаимоотношения Перитонит. Формы перитонита
Перитонит. Формы перитонита Психиатрия. Ситуационная задача
Психиатрия. Ситуационная задача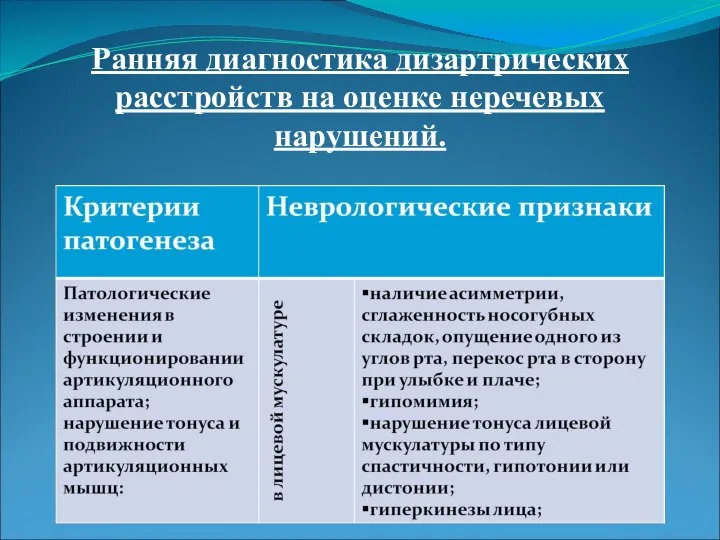 Ранняя диагностика дизартрических расстройств на оценке неречевых нарушений
Ранняя диагностика дизартрических расстройств на оценке неречевых нарушений Первая медицинская помощь при кровотечении
Первая медицинская помощь при кровотечении Эффективное применение ультразвуковых инструментов в современной эндодонтии
Эффективное применение ультразвуковых инструментов в современной эндодонтии Аденовирусная инфекция крупного рогатого скота (аденовирусная пневмония телят, аденовирусный пневмоэнтерит телят)
Аденовирусная инфекция крупного рогатого скота (аденовирусная пневмония телят, аденовирусный пневмоэнтерит телят) Физиологическое и психологическое развитие подростков
Физиологическое и психологическое развитие подростков Рентген аппарат
Рентген аппарат Оценка стойких нарушений функций организма и ограничений жизнедеятельности при установлении категории ребенок-инвалид
Оценка стойких нарушений функций организма и ограничений жизнедеятельности при установлении категории ребенок-инвалид Персональный брендинг. Авторский курс-мастерская
Персональный брендинг. Авторский курс-мастерская Доброкачественные и злокачественные опухоли органов дыхания
Доброкачественные и злокачественные опухоли органов дыхания Внутренняя картина болезни
Внутренняя картина болезни