Содержание
- 2. 17.1 Introduction to the Endocrine System Compare and contrast the actions of the endocrine system and
- 3. 17.1 Introduction to the Endocrine System Endocrine system Composed of ductless glands that synthesize and secrete
- 4. 17.1a Comparison of the Two Control Systems Both the endocrine and nervous system Release ligands—chemical messengers
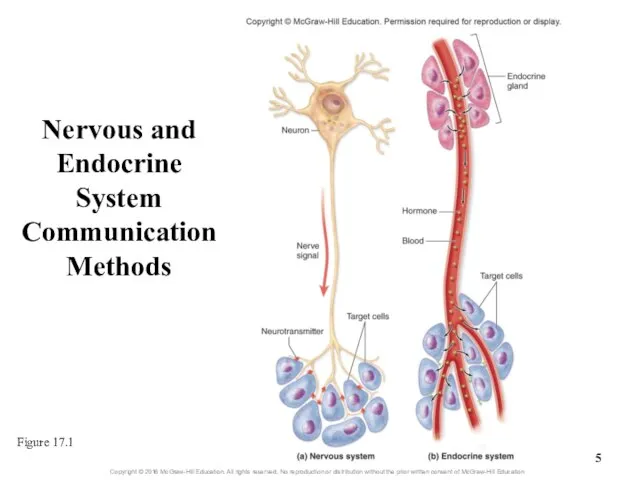
- 5. Nervous and Endocrine System Communication Methods Figure 17.1
- 6. 17.1b General Functions of the Endocrine System Regulating development, growth, and metabolism Hormones help regulate embryonic
- 7. What did you learn? Which control system typically has slower, longer-lasting effects? What general effects can
- 8. 17.2 Endocrine Glands Distinguish between the two types of organization of endocrine cells. Identify the major
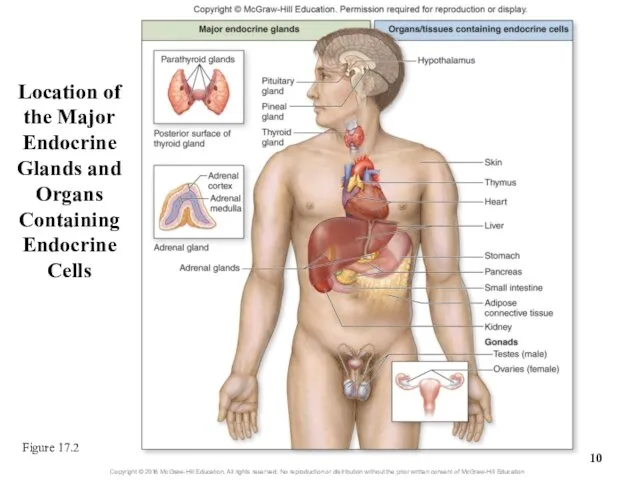
- 9. 17.2a Location of the Major Endocrine Glands Glands contain epithelial tissue that makes and releases hormones
- 10. Location of the Major Endocrine Glands and Organs Containing Endocrine Cells Figure 17.2
- 11. Pineal Gland Pituitary Gland Thyroid Gland Parathyroid Glands Adrenal Glands Endocrine Glands
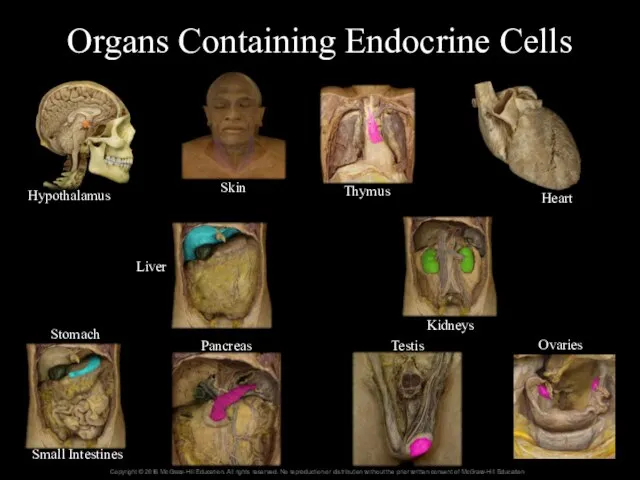
- 12. Organs Containing Endocrine Cells Hypothalamus Skin Thymus Heart Kidneys Liver Stomach Small Intestines Pancreas Testis Ovaries
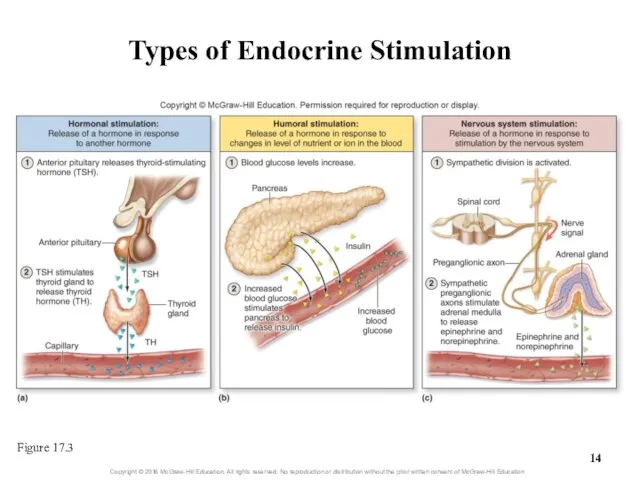
- 13. 17.2b Stimulation of Hormone Synthesis and Release Hormone release is regulated by reflexes to stimuli Hormonal,
- 14. Types of Endocrine Stimulation Figure 17.3
- 15. What did you learn? Is the entire pancreas an endocrine organ? Parathyroid hormone is secreted when
- 16. 17.3 Hormones Name the three structural categories of circulating hormones, and give examples within each category.
- 17. 17.3a Categories of Circulating Hormones Figure 17.4a Steroids Lipid-soluble molecules synthesized from cholesterol Includes gonadal steroids
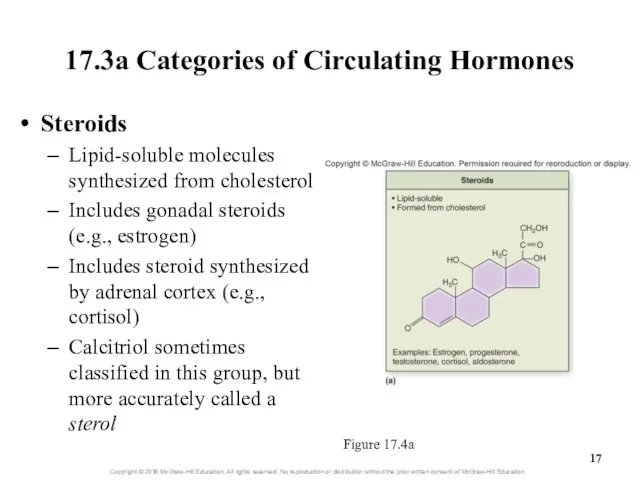
- 18. 17.3a Categories of Circulating Hormones Figure 17.4b Biogenic amines (monoamines) Modified amino acids Includes: catecholamines, thyroid
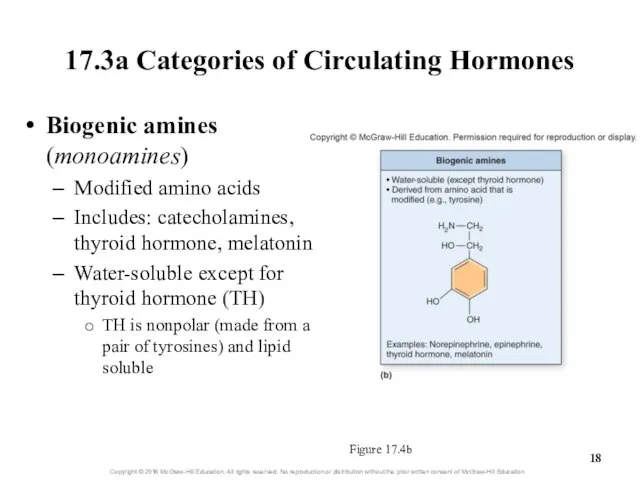
- 19. 17.3a Categories of Circulating Hormones Figure 17.4c Proteins Most hormones are in this category Water-soluble chains
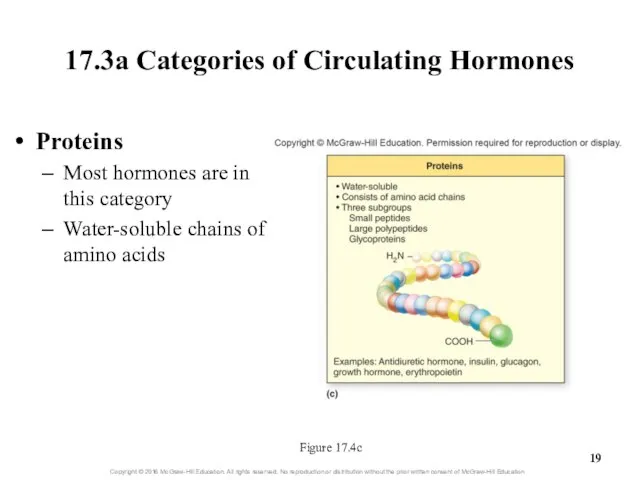
- 20. 17.3b Local Hormones Local hormones Signaling molecules that don’t circulate in blood Some biologists don’t consider
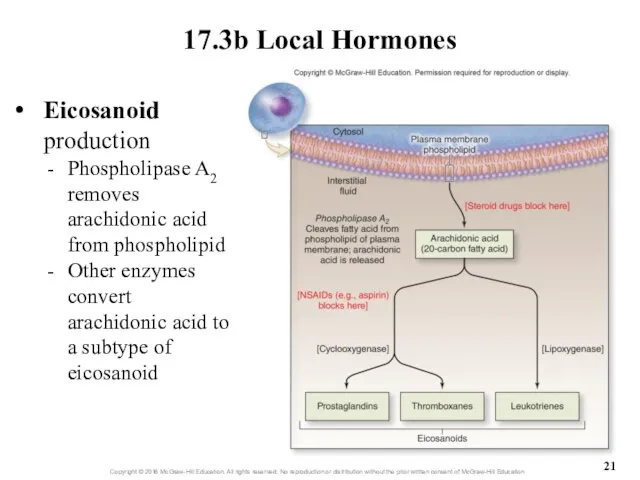
- 21. 17.3b Local Hormones Eicosanoid production Phospholipase A2 removes arachidonic acid from phospholipid Other enzymes convert arachidonic
- 22. 17.3b Local Hormones Eicosanoid effects Autocrine stimulation Effects on the same cell where messenger was formed
- 23. What did you learn? Insulin is made up of a chain of amino acids. What class
- 24. 17.4 Hormone Transport Compare the transport of lipid-soluble hormones with that of water-soluble hormones. Describe the
- 25. 17.4a Transport in the Blood Lipid-soluble hormones use carrier molecules Do not dissolve readily in blood
- 26. 17.4b Levels of Circulating Hormone A hormone’s blood concentration depends on how fast it is synthesized
- 27. 17.4b Levels of Circulating Hormone Half-Life—time necessary to reduce a hormone’s concentration to half of its
- 28. What did you learn? If hormone X and hormone Y had the same rate of synthesis,
- 29. 17.5 Target Cells: Interactions with Hormones Describe how lipid-soluble hormones reach their target cell receptors and
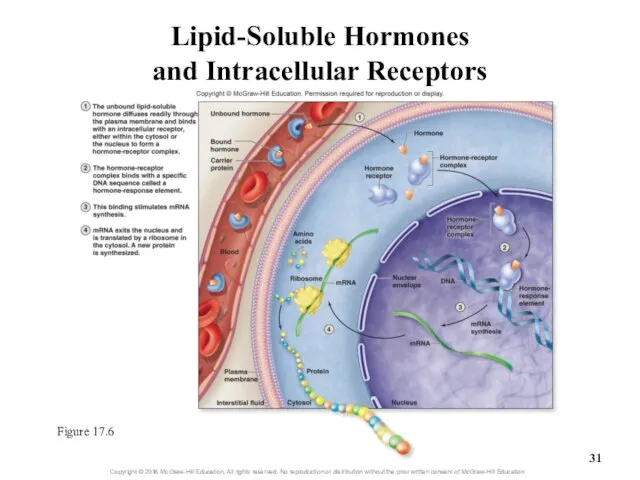
- 30. 17.5a Lipid-Soluble Hormones Lipid-soluble hormones can diffuse across target cell membrane Such hormones are small, nonpolar,
- 31. Lipid-Soluble Hormones and Intracellular Receptors Figure 17.6
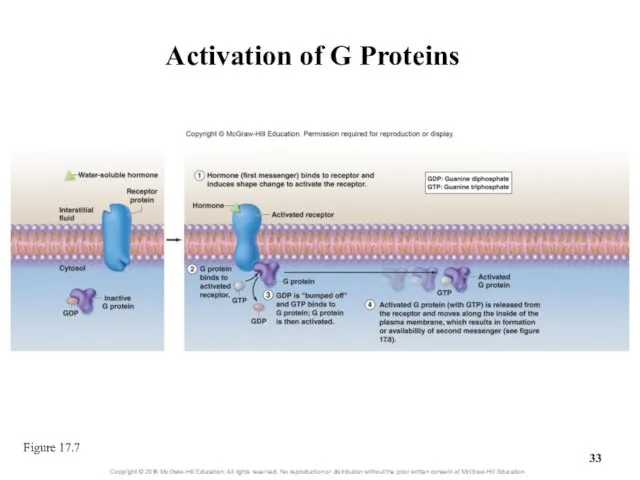
- 32. 17.5b Water-Soluble Hormones Water-soluble hormones use membrane receptors Such hormones are polar and can’t diffuse through
- 33. Activation of G Proteins Figure 17.7
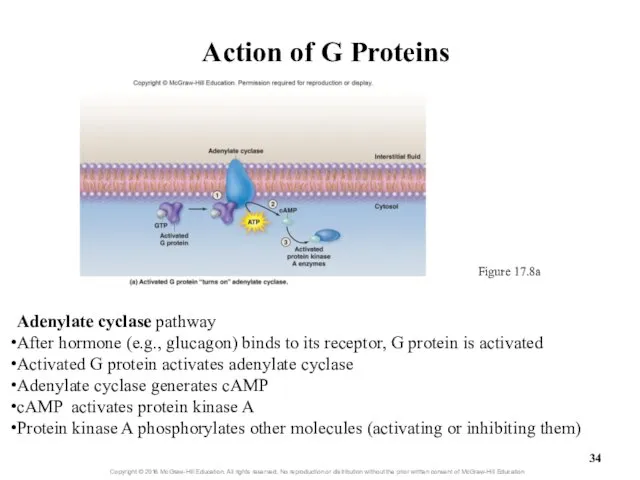
- 34. Action of G Proteins Figure 17.8a Adenylate cyclase pathway After hormone (e.g., glucagon) binds to its
- 35. 17.5b Water-Soluble Hormones Phospholipase C pathway After hormone (e.g., epinephrine) binds to its receptor, G protein
- 36. 17.5b Water-Soluble Hormones Phospholipase C pathway (continued) IP3 is a second messenger that leaves the membrane
- 37. Action of G Proteins Figure 17.8b Phospholipase C Pathway
- 38. 17.5b Water-Soluble Hormones Action of water-soluble hormones Multiple results possible with different signal transduction pathways Enzymes
- 39. 17.5b Water-Soluble Hormones Action of water-soluble hormones (continued) E.g., glucagon released from pancreas when blood sugar
- 40. 17.5b Water-Soluble Hormones Intracellular enzyme cascade and response amplification Signaling pathway advantages Signal is amplified at
- 41. What did you learn? Where are target cell receptors for lipophilic hormones located? What is protein
- 42. 17.6 Target Cells: Degree of Cellular Response Describe the conditions that influence the number of receptors
- 43. 17.6 Target Cells: Degree of Cellular Response A cell’s response to a hormone varies with Its
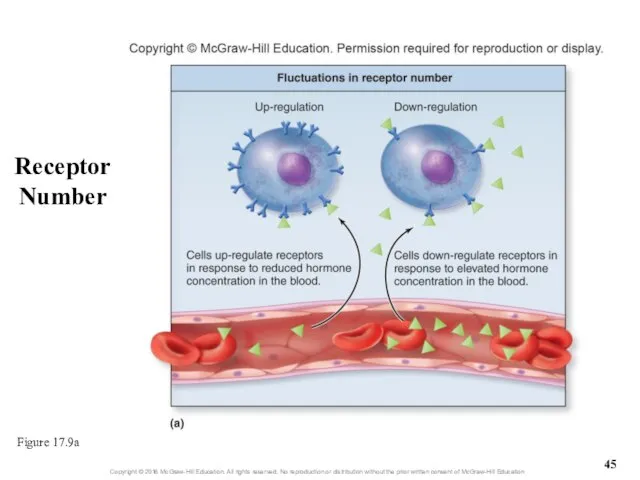
- 44. 17.6a Number of Receptors Receptor number fluctuates Up-regulation: increases number of receptors Increases sensitivity to hormone
- 45. Receptor Number Figure 17.9a
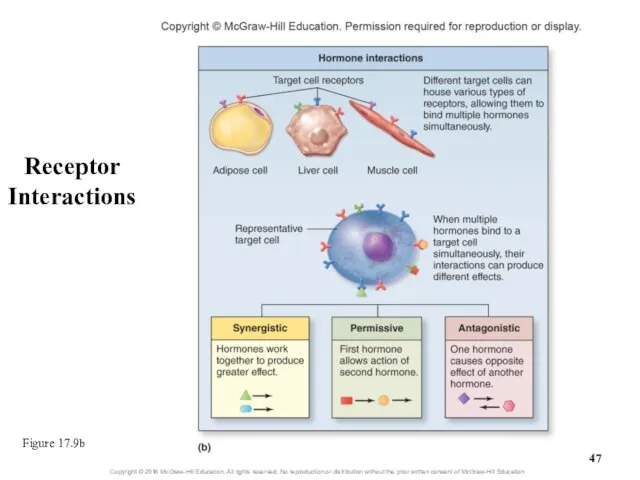
- 46. 17.6b Receptor Interactions Different hormones can simultaneously bind to a cell Synergistic interactions One hormone reinforces
- 47. Receptor Interactions Figure 17.9b
- 48. What did you learn? If someone were to take a large dose of artificial hormone, how
- 49. 17.7 The Hypothalamus and the Pituitary Gland Describe the anatomic relationship of the hypothalamus and the
- 50. 17.7a Anatomic Relationship of the Hypothalamus and the Pituitary Gland Hypothalamus controls pituitary, which controls thyroid,
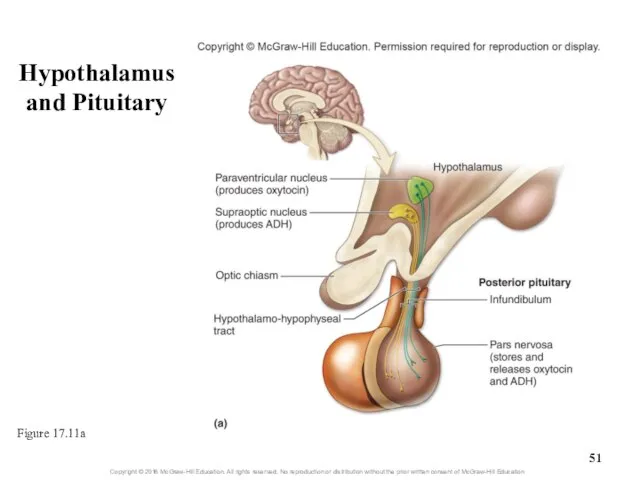
- 51. Hypothalamus and Pituitary Figure 17.11a
- 52. 17.7a Anatomic Relationship of the Hypothalamus and the Pituitary Gland Posterior pituitary (neurohypophysis) Smaller, neural part
- 53. 17.7a Anatomic Relationship of the Hypothalamus and the Pituitary Gland Anterior pituitary (adenohypophysis) Larger, glandular part
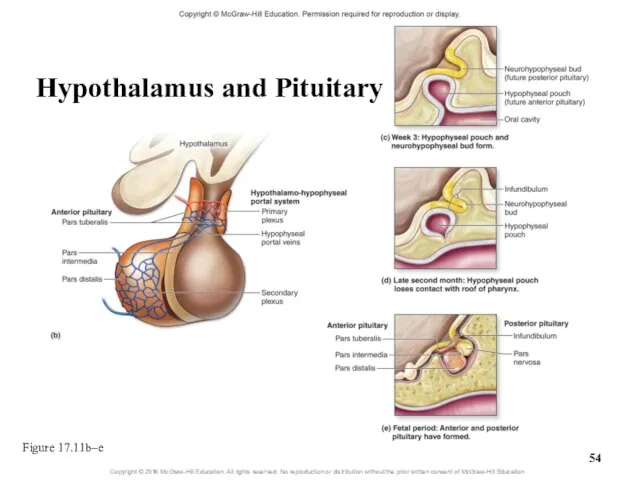
- 54. Figure 17.11b–e Hypothalamus and Pituitary
- 55. 17.7a Anatomic Relationship of the Hypothalamus and the Pituitary Gland Anterior pituitary (continued) Hypothalamo-hypophyseal portal system
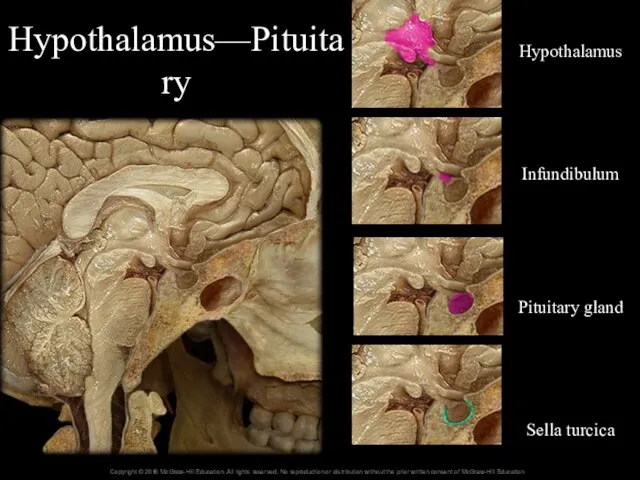
- 56. Hypothalamus—Pituitary Hypothalamus Infundibulum Pituitary gland Sella turcica
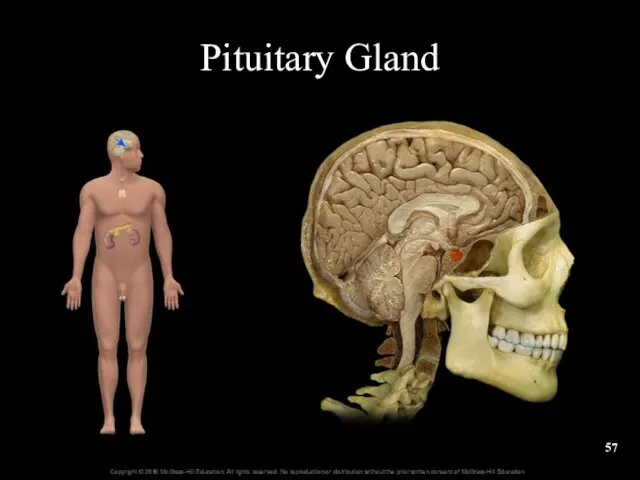
- 57. Pituitary Gland
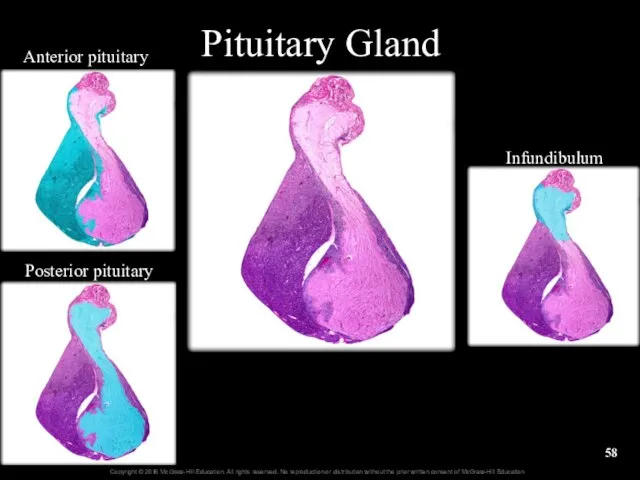
- 58. Pituitary Gland Anterior pituitary Posterior pituitary Infundibulum
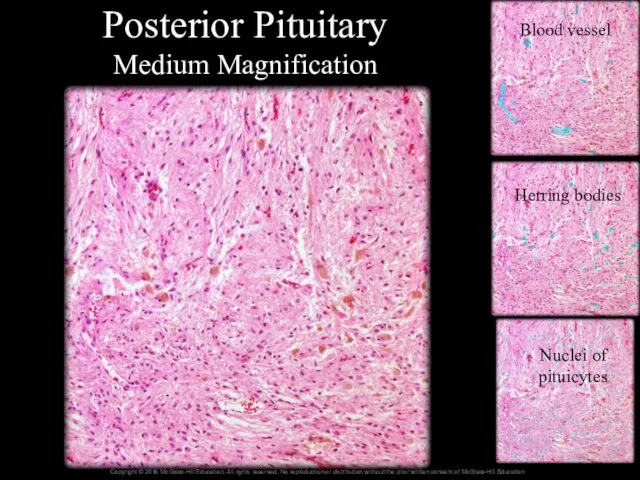
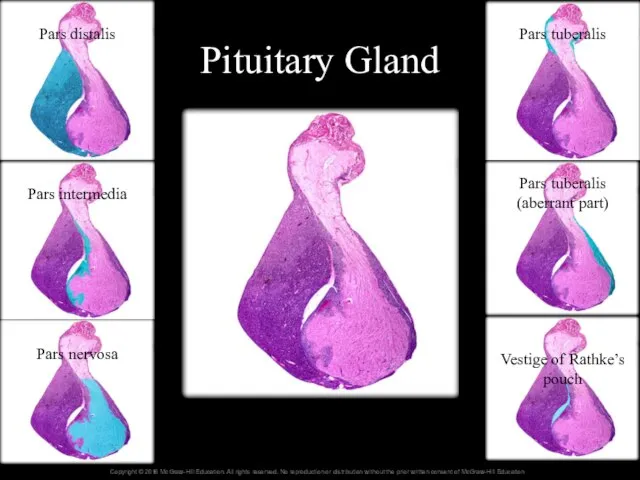
- 59. Posterior Pituitary Medium Magnification Blood vessel Herring bodies Nuclei of pituicytes
- 60. Pituitary Gland Pars distalis Pars intermedia Pars nervosa Pars tuberalis Pars tuberalis (aberrant part) Vestige of
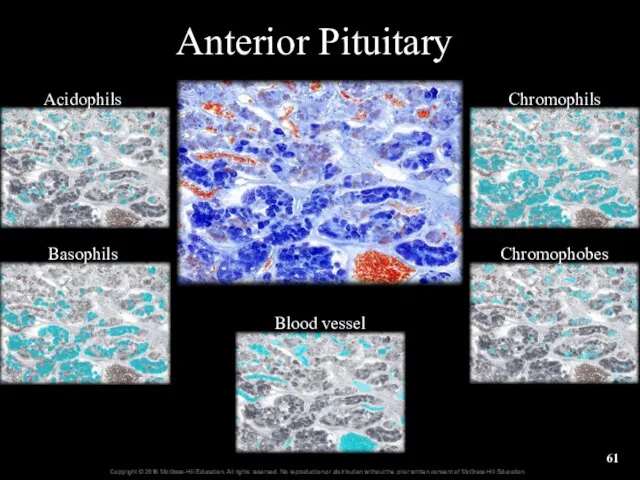
- 61. Anterior Pituitary Acidophils Basophils Blood vessel Chromophils Chromophobes
- 62. 17.7b Interactions Between the Hypothalamus and the Posterior Pituitary Gland Posterior pituitary is storage and release
- 63. 17.7c Interactions Between the Hypothalamus and the Anterior Pituitary Gland Hypothalamus hormonally stimulates anterior pituitary to
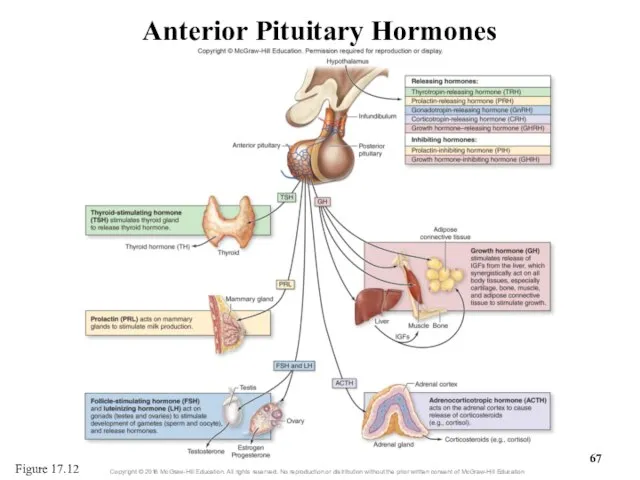
- 64. 17.7c Interactions Between the Hypothalamus and the Anterior Pituitary Gland Regulatory hormones of the hypothalamus Releasing
- 65. 17.7c Interactions Between the Hypothalamus and the Anterior Pituitary Gland Anterior pituitary—tropic hormones and prolactin Thyroid
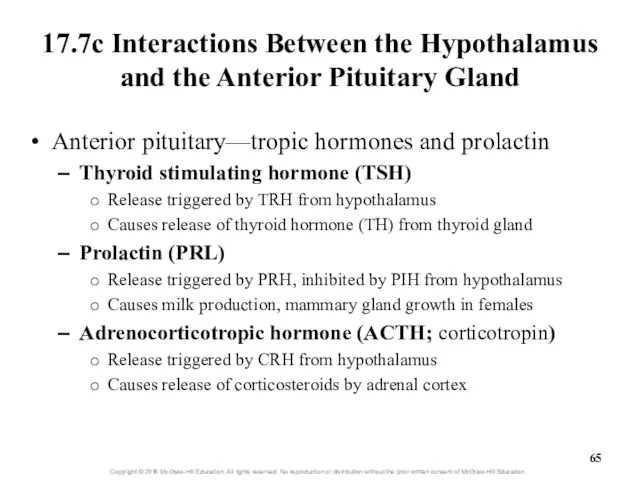
- 66. 17.7c Interactions Between the Hypothalamus and the Anterior Pituitary Gland Anterior pituitary—tropic hormones and prolactin (continued)
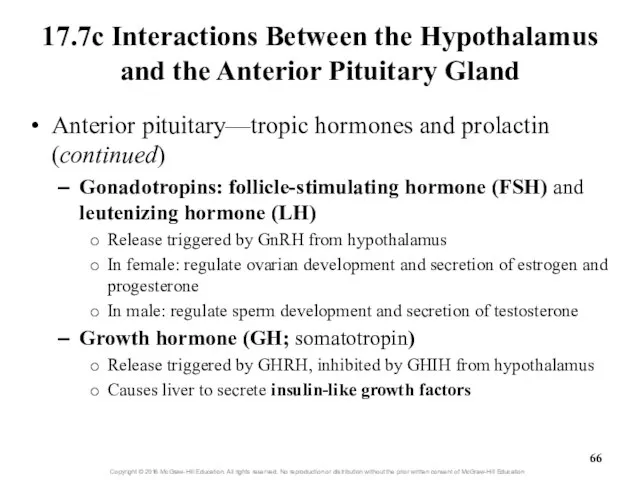
- 67. Anterior Pituitary Hormones Figure 17.12
- 68. Clinical View: Hypophysectomy Surgical removal of the pituitary gland because of tumors Preferred surgical approach through
- 69. What did you learn? Where are secondary plexus blood vessels located? Where are tropic hormones synthesized
- 70. 17.8 Representative Hormones Regulated by the Hypothalamus Describe the homeostatic system involving growth hormone. Describe thyroid
- 71. 17.8 Representative Hormones Regulated by the Hypothalamus (continued) Name the three zones of the adrenal cortex
- 72. 17.8a Growth Hormone Growth hormone (GH) functions include Stimulation of linear growth at epiphyseal plate Hypertrophy
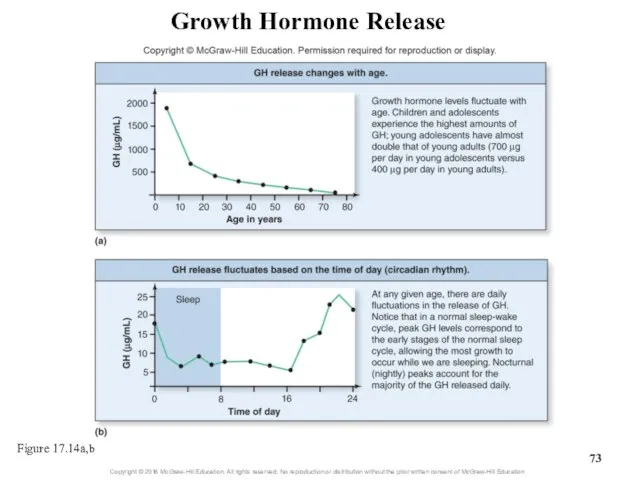
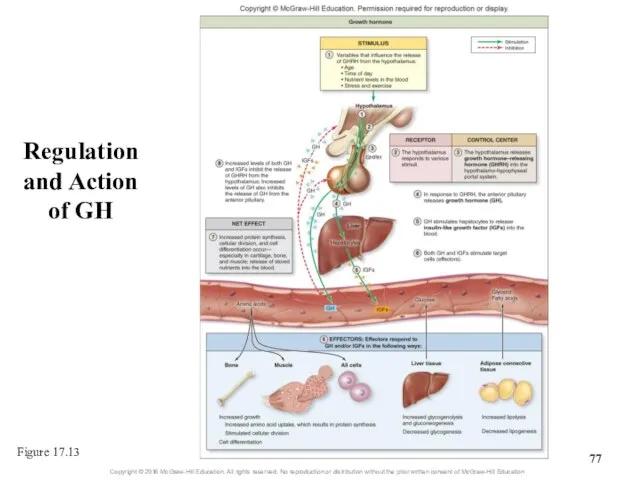
- 73. Growth Hormone Release Figure 17.14a,b
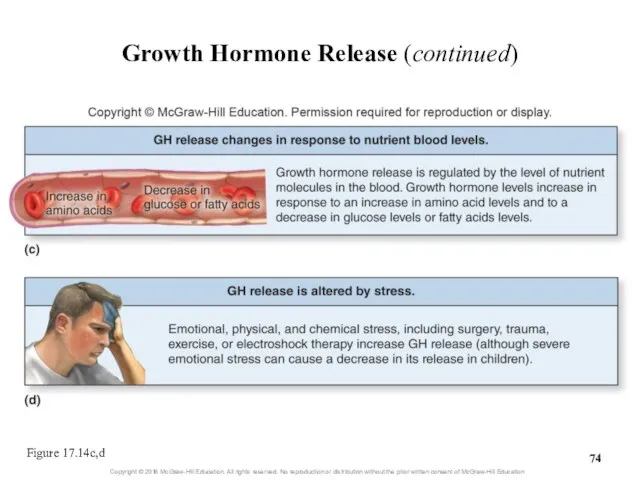
- 74. Growth Hormone Release (continued) Figure 17.14c,d
- 75. 17.8a Growth Hormone GH targets hepatocytes Hepatocytes release insulin-like growth factors (IGFs) IGFs work synergistically with
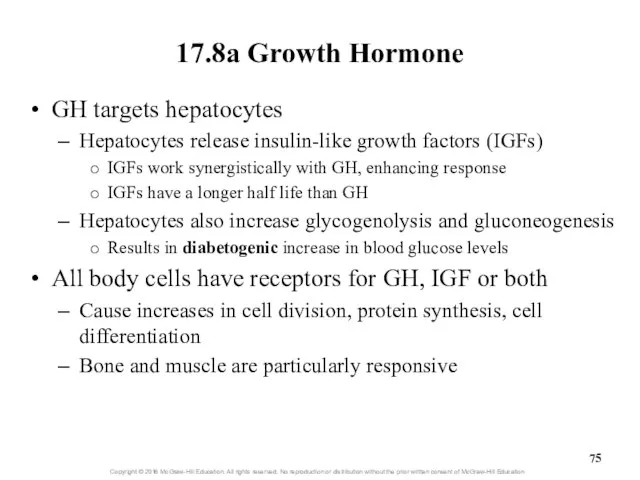
- 76. 17.8a Growth Hormone GH and IGFs cause adipose cells to release nutrients Cells increase lipolysis and
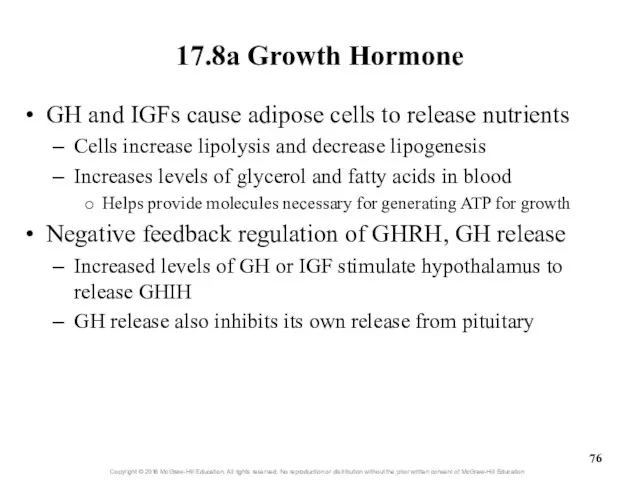
- 77. Regulation and Action of GH Figure 17.13
- 78. Clinical View: Disorders of Growth Hormone Secretion Growth hormone deficiency (pituitary dwarfism) Inadequate growth hormone production
- 79. Clinical View: Disorders of Growth Hormone Secretion (continued) Acromegaly Excessive growth hormone production in adult Enlargement
- 80. 17.8b Thyroid Gland and Thyroid Hormone Anatomy of the thyroid gland Sits inferior to thyroid cartilage
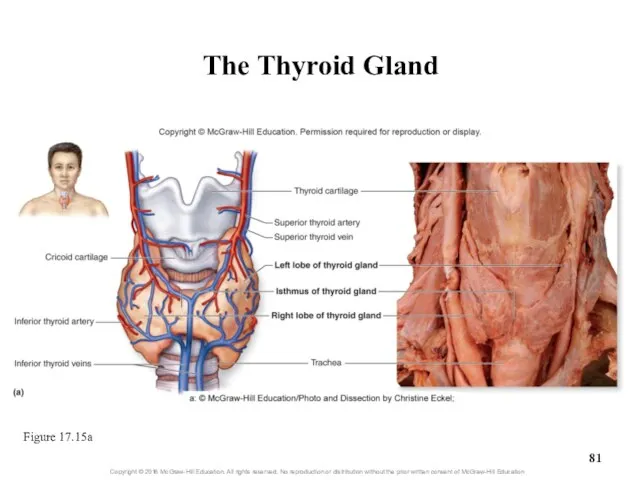
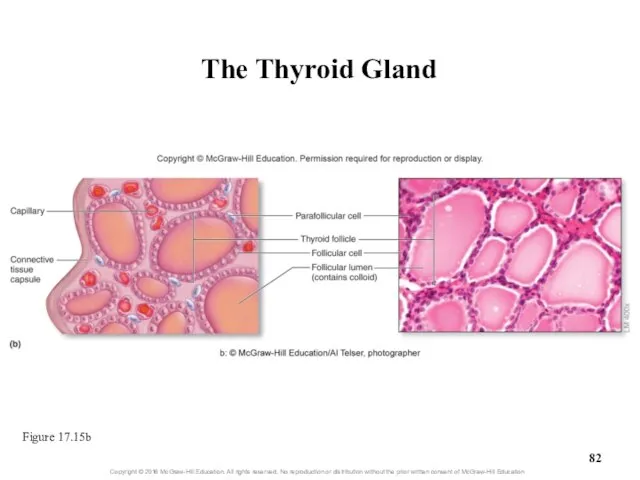
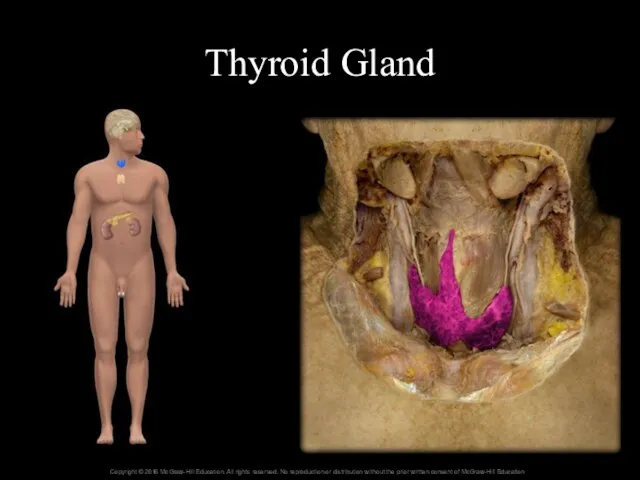
- 81. The Thyroid Gland Figure 17.15a
- 82. The Thyroid Gland Figure 17.15b
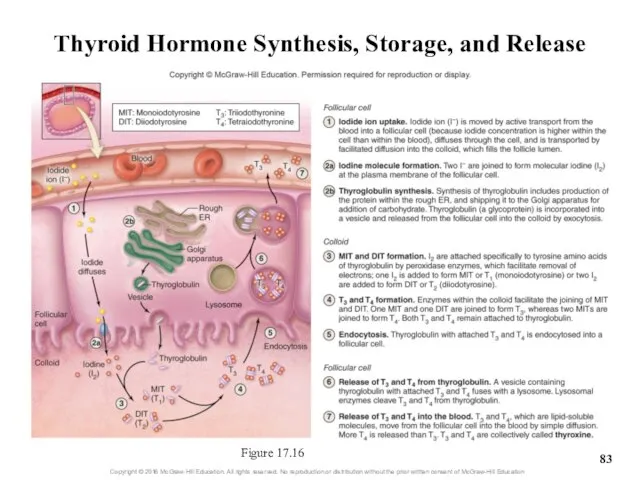
- 83. Thyroid Hormone Synthesis, Storage, and Release Figure 17.16
- 84. Thyroid Gland
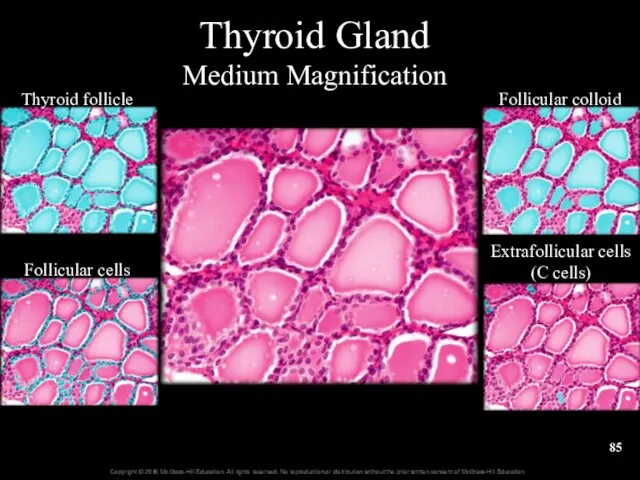
- 85. Thyroid Gland Medium Magnification Thyroid follicle Follicular cells Follicular colloid Extrafollicular cells (C cells)
- 86. Thyroid Gland High Magnification Thyroid follicle Nuclei of follicular cells Follicular colloid Extrafollicular cells (C cells)
- 87. 17.8b Thyroid Gland and Thyroid Hormone Action of thyroid hormone (TH) Hypothalamic-pituitary-thyroid axis Cold temperature, pregnancy,
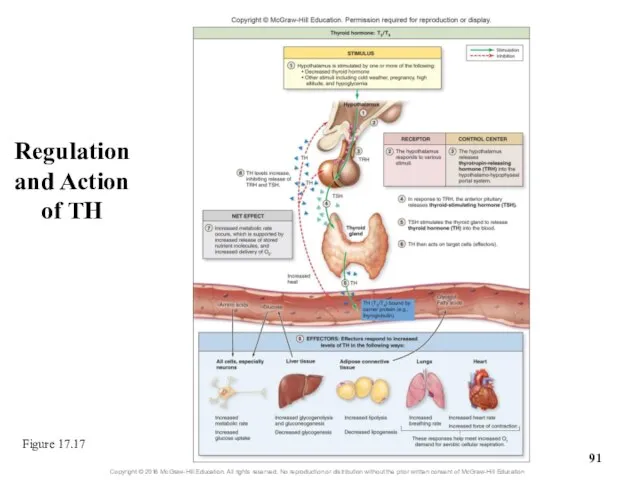
- 88. 17.8b Thyroid Gland and Thyroid Hormone Action of thyroid hormone (TH) (continued) Some TH dissociates from
- 89. 17.8b Thyroid Gland and Thyroid Hormone Action of Thyroid Hormone (TH) (continued) Fosters energy (ATP) production
- 90. 17.8b Thyroid Gland and Thyroid Hormone Negative feedback regulation of TH release Increases in TH cause
- 91. Regulation and Action of TH Figure 17.17
- 92. Clinical View: Disorders of Thyroid Hormone Secretion Hyperthyroidism Results from excessive production of TH Increased metabolic
- 93. Clinical View: Disorders of Thyroid Hormone Secretion (continued) Goiter Enlargement of thyroid Typically due to insufficient
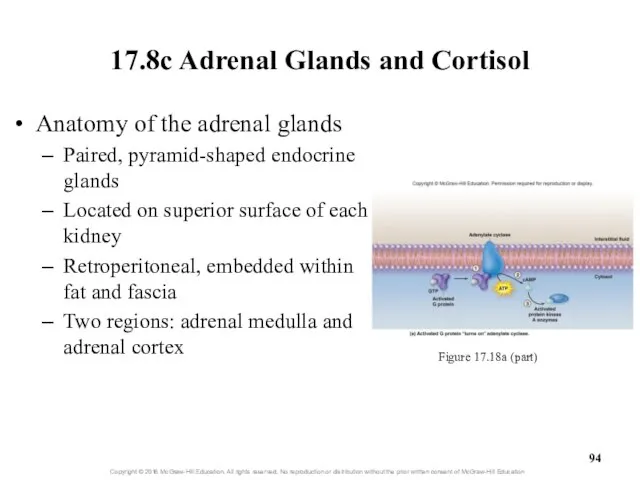
- 94. 17.8c Adrenal Glands and Cortisol Anatomy of the adrenal glands Paired, pyramid-shaped endocrine glands Located on
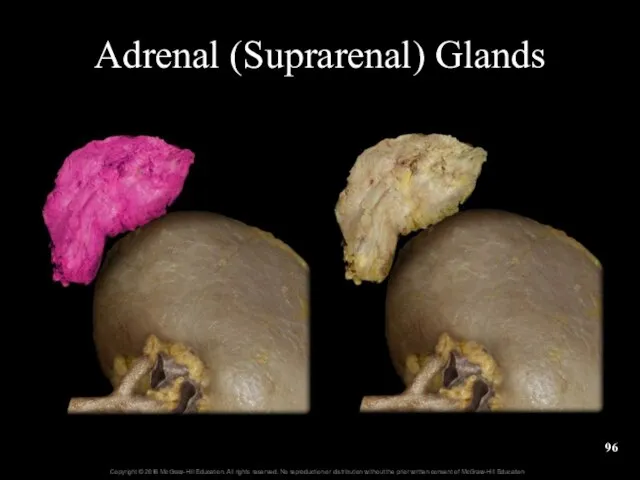
- 95. Adrenal Glands
- 96. Adrenal (Suprarenal) Glands
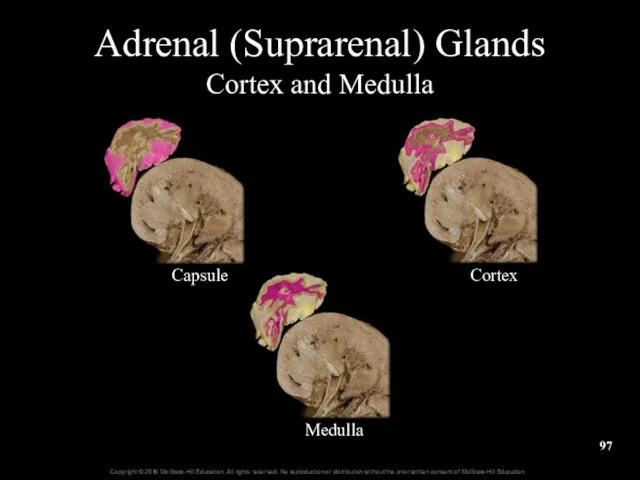
- 97. Adrenal (Suprarenal) Glands Cortex and Medulla Capsule Cortex Medulla
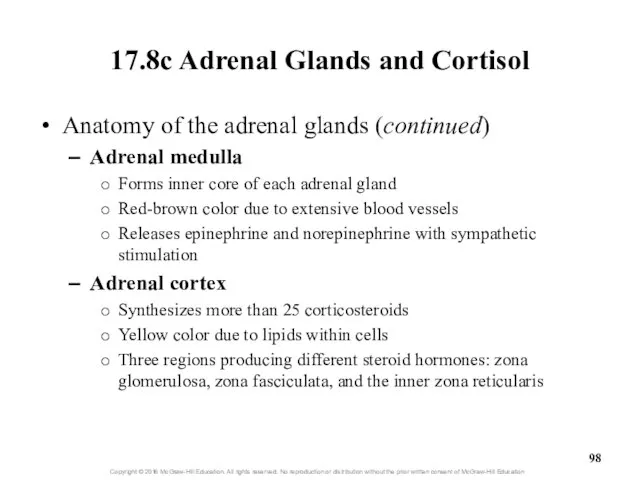
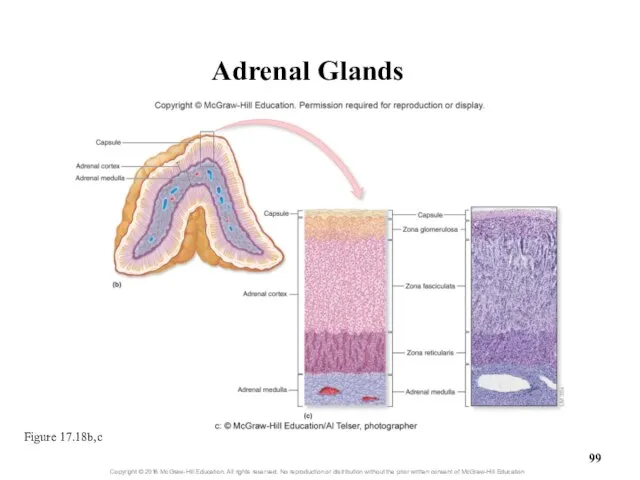
- 98. 17.8c Adrenal Glands and Cortisol Anatomy of the adrenal glands (continued) Adrenal medulla Forms inner core
- 99. Adrenal Glands Figure 17.18b,c
- 100. 17.8c Adrenal Glands and Cortisol Hormones of the adrenal cortex Mineralocorticoids: hormones that regulate electrolyte levels
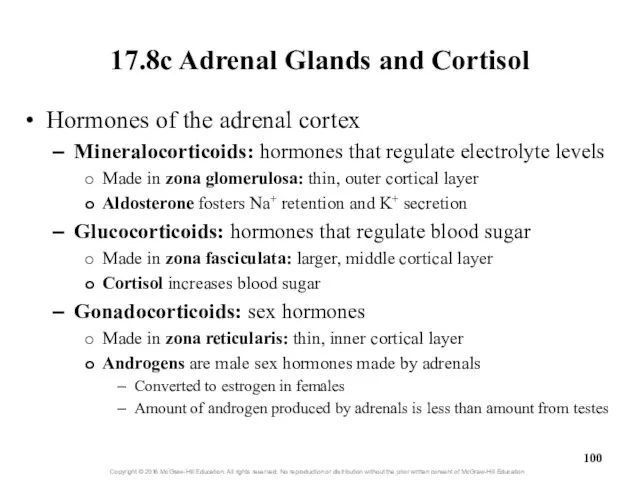
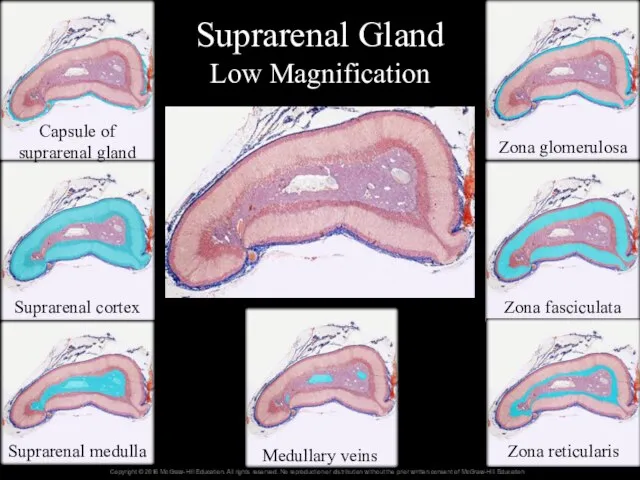
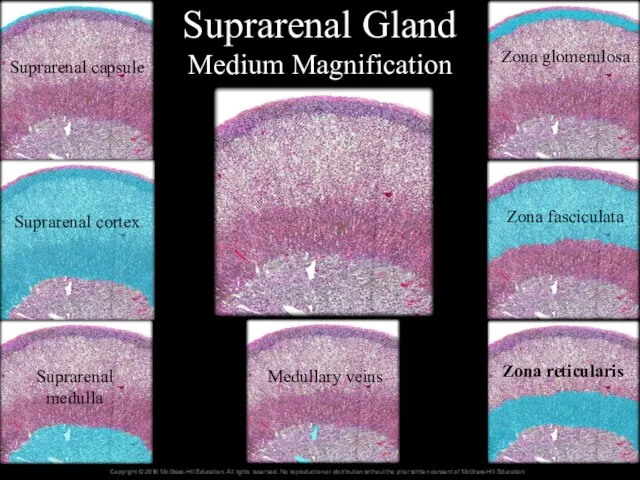
- 101. Suprarenal Gland Low Magnification Capsule of suprarenal gland Suprarenal cortex Suprarenal medulla Medullary veins Zona glomerulosa
- 102. Suprarenal Gland Medium Magnification Suprarenal capsule Suprarenal cortex Suprarenal medulla Medullary veins Zona glomerulosa Zona fasciculata
- 103. 17.8c Adrenal Glands and Cortisol Action of cortisol Cortisol and corticosterone increase nutrient levels in blood
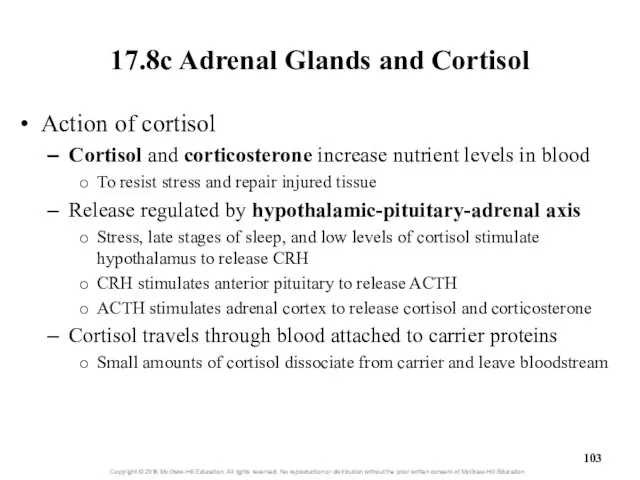
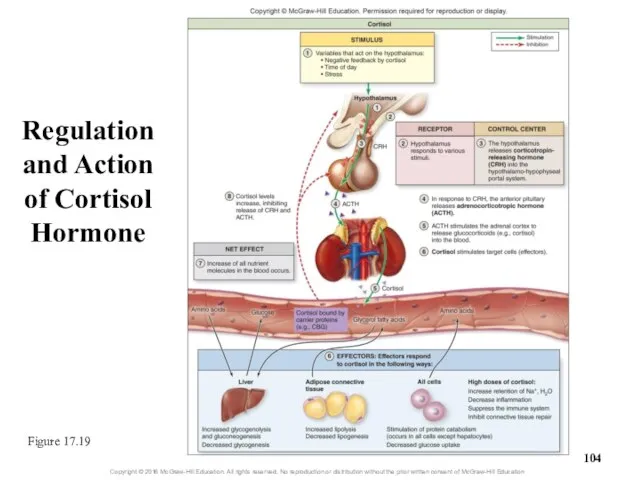
- 104. Regulation and Action of Cortisol Hormone Figure 17.19
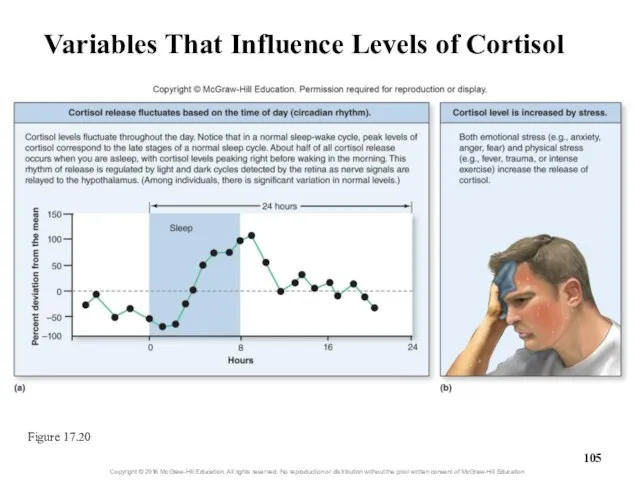
- 105. Variables That Influence Levels of Cortisol Figure 17.20
- 106. 17.8c Adrenal Glands and Cortisol Action of cortisol (continued) Cortisol diffuses through target cell’s membrane and
- 107. 17.8c Adrenal Glands and Cortisol Cortisol levels are regulated by negative feedback Cortisol inhibits release of
- 108. Clinical View: Disorders in Adrenal Cortex Hormone Secretion Cushing syndrome Chronic exposure to excessive glucocorticoid hormones
- 109. Clinical View: Disorders in Adrenal Cortex Hormone Secretion (continued) Adrenogenital syndrome (congenital adrenal hyperplasia) Begins in
- 110. Clinical View: Stress Response Stressors elicit a stress response Hypothalamus initiates neuroendocrine response Three stages Alarm
- 111. What did you learn? At what time of day are growth hormone levels highest? What is
- 112. 17.9 Pancreatic Hormones Describe the gross anatomy and cellular structure of the pancreas. Identify the primary
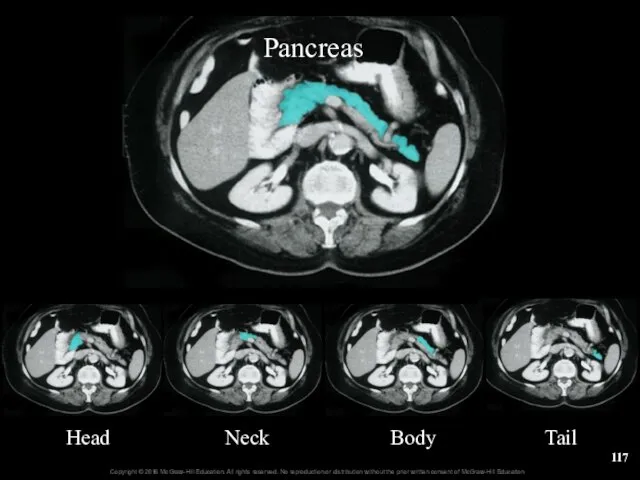
- 113. 17.9a Anatomy of the Pancreas Sits behind stomach, between duodenum and spleen Pancreas has endocrine and
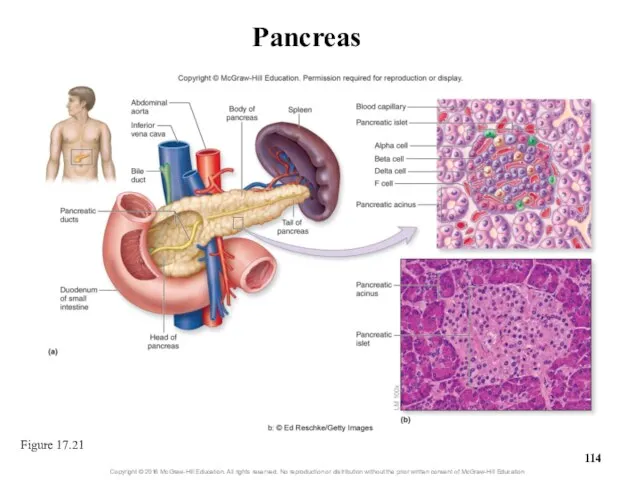
- 114. Pancreas Figure 17.21
- 115. Pancreas
- 116. Pancreas Head Neck Body Tail Pancreas
- 117. Pancreas Head Neck Body Tail
- 118. Pancreas Low Magnification Endocrine pancreas Exocrine pancreas (acini)
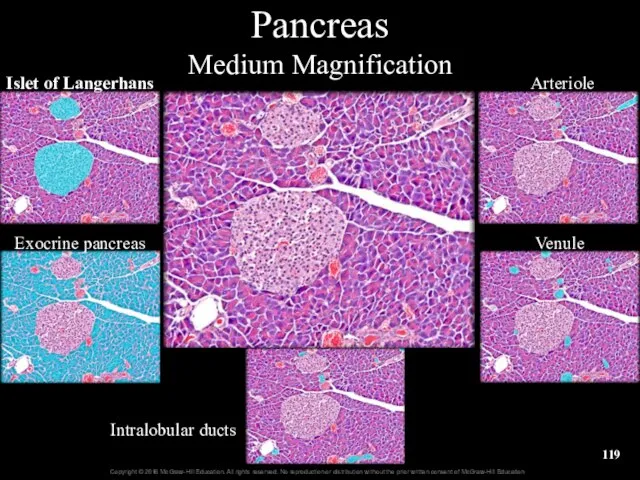
- 119. Pancreas Medium Magnification Islet of Langerhans Exocrine pancreas Arteriole Venule Intralobular ducts
- 120. Pancreas High Magnification Islet of Langerhans Exocrine pancreas Capillaries in pancreatic islet of Langerhans
- 121. Pancreas—Alpha Cells Pancreatic Islet of Langerhans Exocrine pancreas Alpha cells
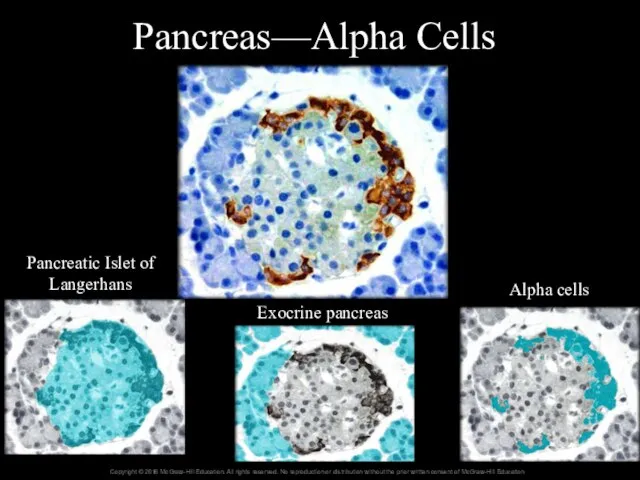
- 122. Pancreas—Beta Cells Islet of Langerhans Exocrine pancreas Beta cells
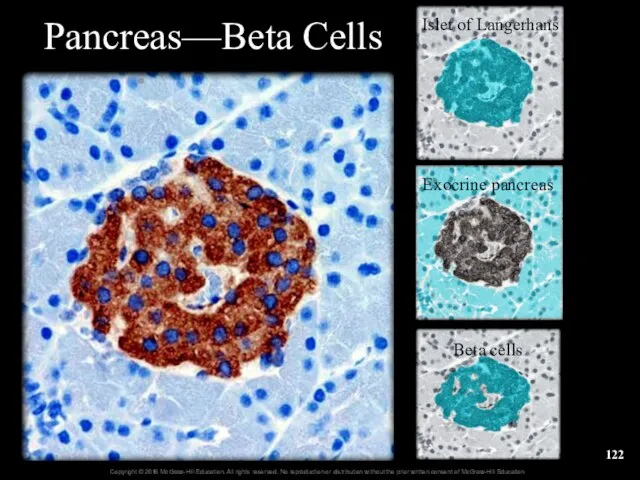
- 123. 17.9b Effects of Pancreatic Hormones Pancreatic hormones help maintain blood glucose Normal range is 70 to
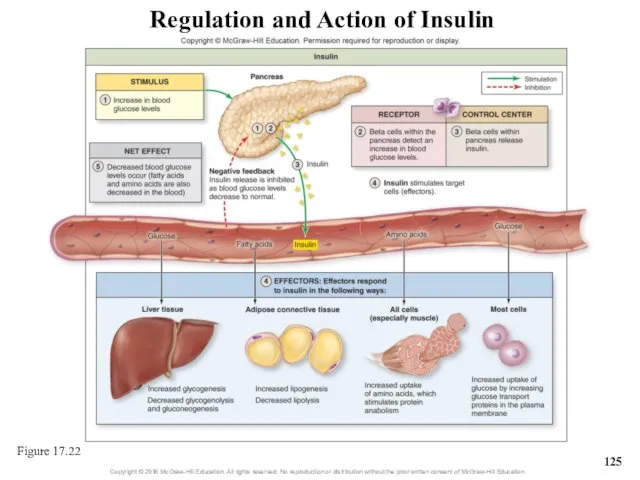
- 124. 17.9b Effects of Pancreatic Hormones How insulin lowers blood glucose Hepatocytes remove glucose from blood; store
- 125. Regulation and Action of Insulin Figure 17.22
- 126. Clinical View: Conditions Resulting in Abnormal Glucose Levels Diabetes mellitus Inadequate uptake of glucose from blood
- 127. Clinical View: Conditions Resulting in Abnormal Glucose Levels (continued) Type 2 diabetes From decreased insulin release
- 128. Clinical View: Conditions Resulting in Abnormal Glucose Levels (continued) Hypoglycemia Glucose levels below 60 mg/DL Numerous
- 129. 17.9b Effects of Pancreatic Hormones Glucagon raises blood glucose Alpha cells detect drop in blood glucose
- 130. Regulation and Action of Glucagon Figure 17.23
- 131. What did you learn? What function is served by the pancreatic islets? What effect would a
- 132. 17.10 Other Endocrine Glands Describe the general structure, location, and function of the pineal gland. Describe
- 133. 17.10a Pineal Gland Pineal gland is a small unpaired body in the epithalamus of the diencephalon
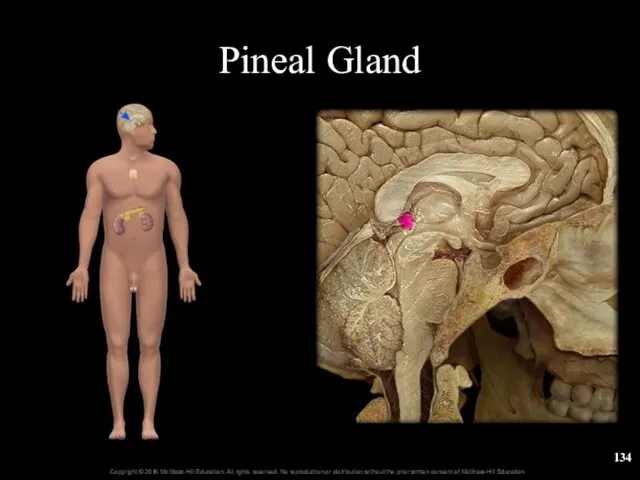
- 134. Pineal Gland
- 135. 17.10b Parathyroid Glands Parathyroid glands are small structures on the back of the thyroid gland There
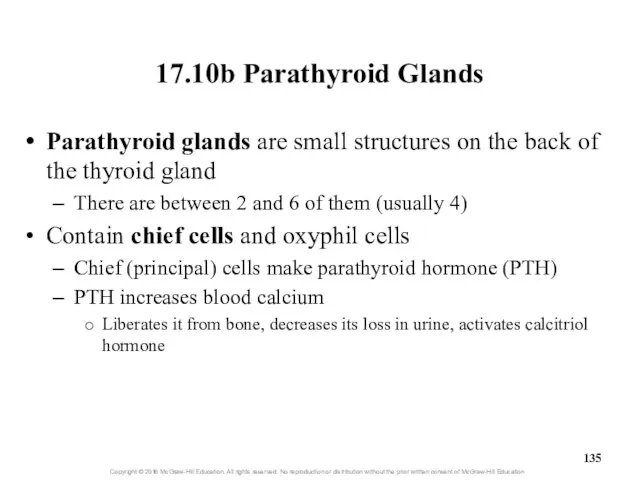
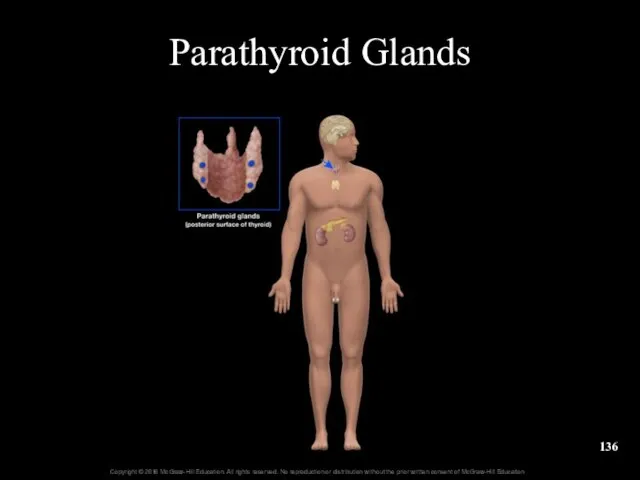
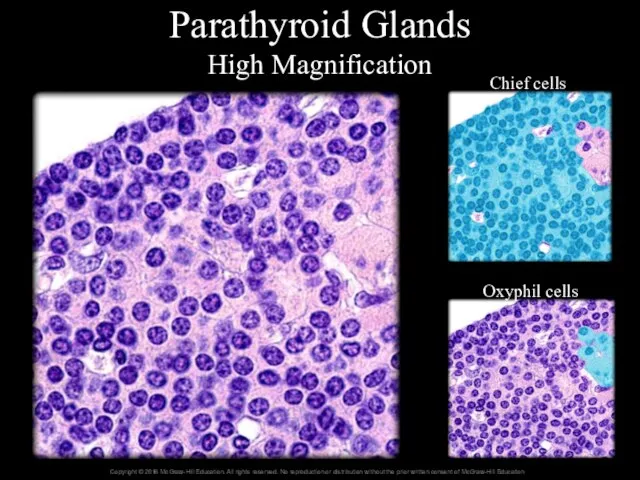
- 136. Parathyroid Glands
- 137. Parathyroid Glands High Magnification Chief cells Oxyphil cells
- 138. 17.10c Structures with an Endocrine Function Thymus epithelial cells secrete thymic hormones Located anterior to top
- 139. 17.10c Structures with an Endocrine Function Liver secretions include insulin-like growth factors and the inactive hormone
- 140. 17.10c Structures with an Endocrine Function Small intestine secretes secretin and cholecystokinin (CCK) into blood Secretin
- 141. 17.10c Structures with an Endocrine Function Adipose connective tissue secretes leptin Leptin controls appetite by binding
- 142. What did you learn? What gland secretes melatonin and what is its effect? What effect does
- 143. 17.11 Aging and the Endocrine System Describe how endocrine activity changes as people age. Learning Objectives:
- 144. 17.11 Aging and the Endocrine System Endocrine changes with aging Secretory activity wanes with age Reduces
- 146. Скачать презентацию

















 Органные врожденные пороки
Органные врожденные пороки Скорая помощь для кожи и волос: серия средств со змеиным жиром
Скорая помощь для кожи и волос: серия средств со змеиным жиром Личная гигиена
Личная гигиена Магнитно-резонансная томография
Магнитно-резонансная томография Тауарлар қорының құрылымы және классификациясы
Тауарлар қорының құрылымы және классификациясы Егулерді ұйымдастыру. Вакцинация
Егулерді ұйымдастыру. Вакцинация Кровь человека
Кровь человека Серьезный разговор о серьезной проблеме. ВИЧ
Серьезный разговор о серьезной проблеме. ВИЧ Патология периферической нервной системы
Патология периферической нервной системы Естің бұзылыстары. Нарушения памяти
Естің бұзылыстары. Нарушения памяти Планирование работы ТБМК на портале НМО в 2020г году
Планирование работы ТБМК на портале НМО в 2020г году Семиотика поражения органов дыхания у детей
Семиотика поражения органов дыхания у детей Болезни и травмы кожи
Болезни и травмы кожи Четырехугольники
Четырехугольники Острая диарея
Острая диарея Антигени. Шляхи надходження антигенів в організм
Антигени. Шляхи надходження антигенів в організм Угревая болезнь
Угревая болезнь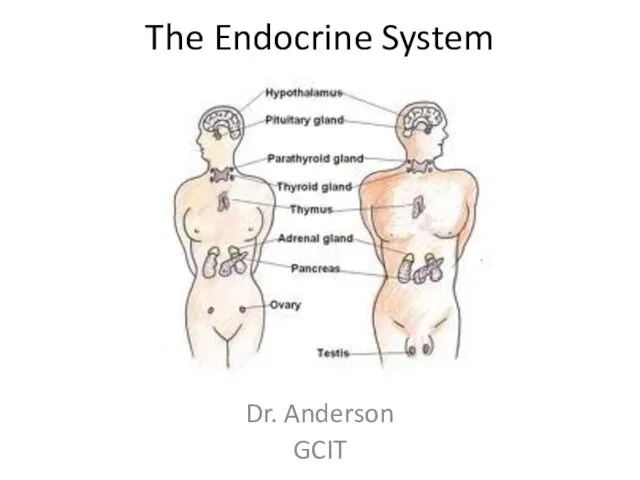 The Endocrine System
The Endocrine System Клинико-анатомические особенности расположения слепой кишки и червеобразного отростка
Клинико-анатомические особенности расположения слепой кишки и червеобразного отростка СПИД – что это такое?
СПИД – что это такое? Патофизиология внешнего дыхания. (Лекция 1)
Патофизиология внешнего дыхания. (Лекция 1) Моноклонды антиденелер, оның гибридионды технологиясы. Моноклонды антиденелердің иммунологиядағы негізгі қолдану аймағы
Моноклонды антиденелер, оның гибридионды технологиясы. Моноклонды антиденелердің иммунологиядағы негізгі қолдану аймағы Микробиологическая диагностика гнойно-воспалительных заболеваний, вызванных грамотрицательными аэробными бактериями
Микробиологическая диагностика гнойно-воспалительных заболеваний, вызванных грамотрицательными аэробными бактериями Қан айналымының бұзылыстары
Қан айналымының бұзылыстары Здоровая земля, здоровые растения и люди
Здоровая земля, здоровые растения и люди Тема 5. Хвороби крови. Анемії
Тема 5. Хвороби крови. Анемії АИТВ. Ауру қоздырғышы - Т-лимфотропты ретровирус
АИТВ. Ауру қоздырғышы - Т-лимфотропты ретровирус Инструментальные методы диагностики
Инструментальные методы диагностики