Содержание
- 2. Definition Arterial hypertension (WHO, 1999) is a constantly increased systolic (≥140 mmHg) and/or diastolic BP (≥90
- 3. Definition Hypertension is defined as values ≥140 mmHg SBP and/or ≥90 mmHg DBP, based on the
- 4. Why do we take care of arterial hypertension? “Silent killer of XXI century” Major cardiovascular risk
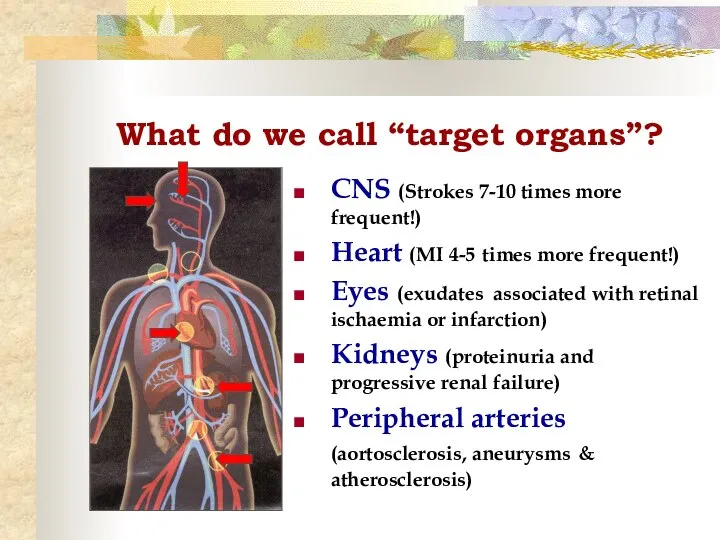
- 5. What do we call “target organs”? CNS (Strokes 7-10 times more frequent!) Heart (MI 4-5 times
- 6. Hypertension in the world 33% of the population in USA, 43-44% in Russia,more than 41,5 million.
- 7. Prevalence of hypertension Overall the prevalence of hypertension appears to be around 30–45% of the general
- 8. Report of World Health Organization In 2020 AD, 2.6 million Indians are predicted to die due
- 9. Hypertension in Nigeria Prevalence of hypertension -28.7%. Hypertension prevalence was comparable in men and women (29.9%
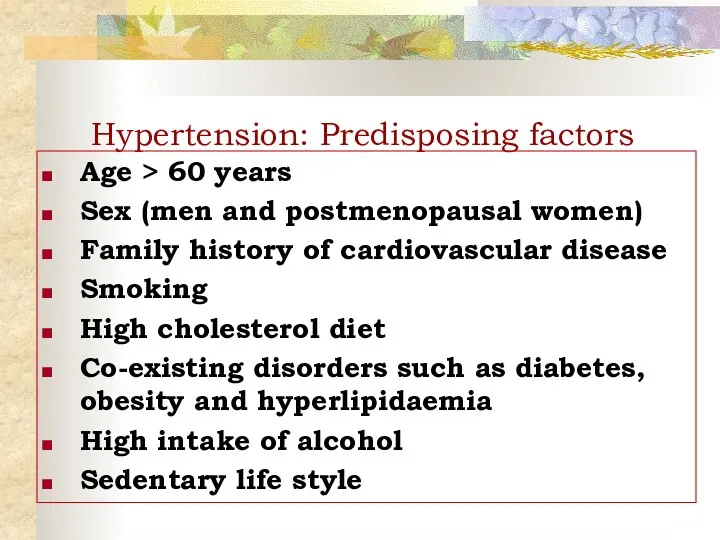
- 10. Hypertension: Predisposing factors Age > 60 years Sex (men and postmenopausal women) Family history of cardiovascular
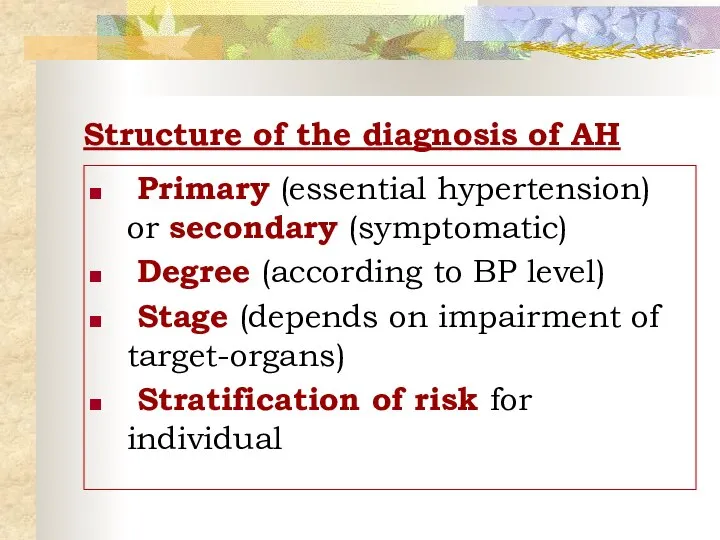
- 11. Structure of the diagnosis of AH Primary (essential hypertension) or secondary (symptomatic) Degree (according to BP
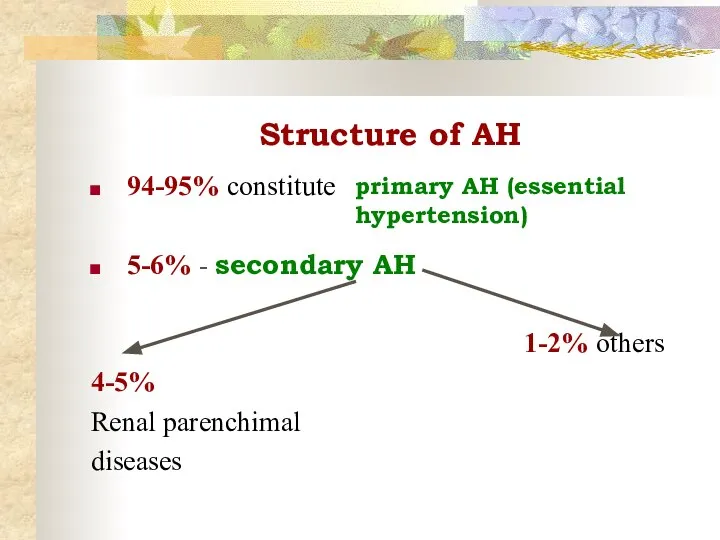
- 12. Structure of AH 94-95% constitute 5-6% - secondary AH 4-5% Renal parenchimal diseases 1-2% others primary
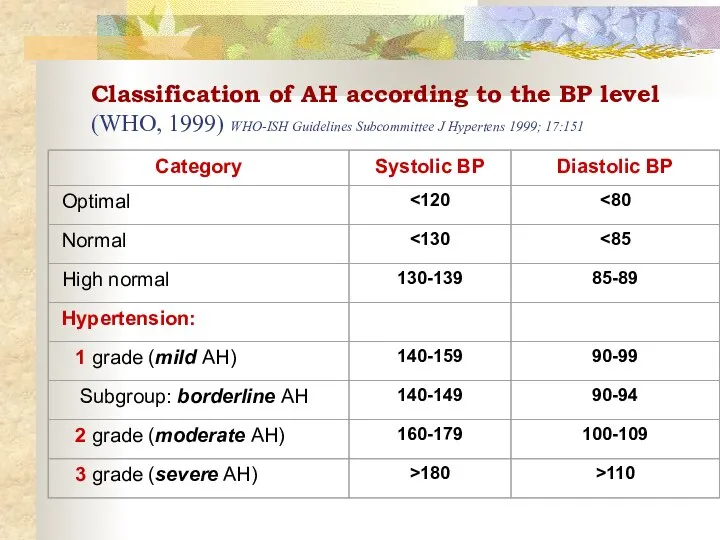
- 13. Classification of AH according to the BP level (WHO, 1999) WHO-ISH Guidelines Subcommittee J Hypertens 1999;
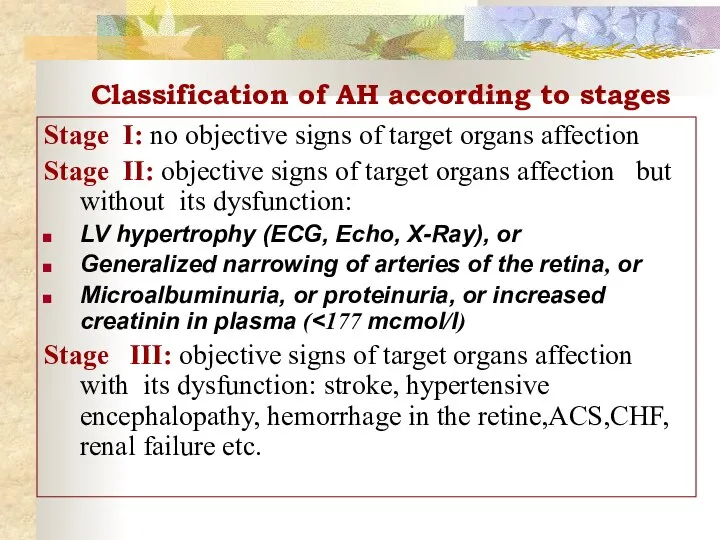
- 14. Classification of AH according to stages Stage I: no objective signs of target organs affection Stage
- 15. Assessment of total cardiovascular risk The concept is based on the fact that only a small
- 16. Assessment of total cardiovascular risk Estimation of total CV risk is easy in particular subgroups of
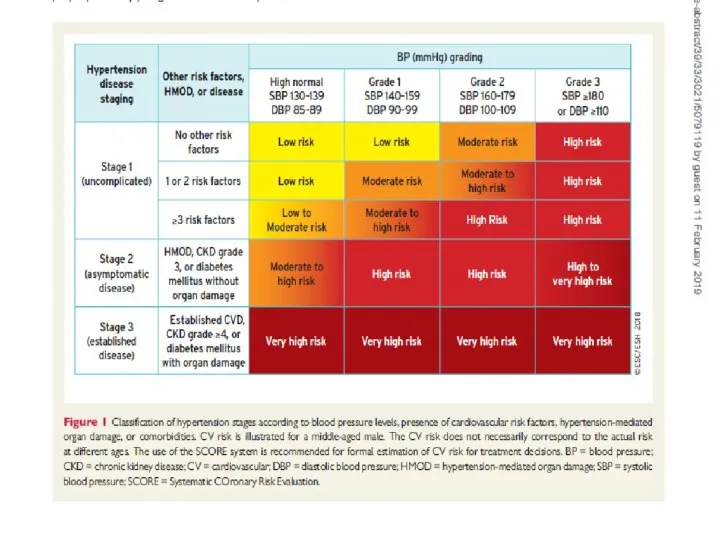
- 17. Assessment of total cardiovascular risk The classification in low, moderate, high and very high risk is
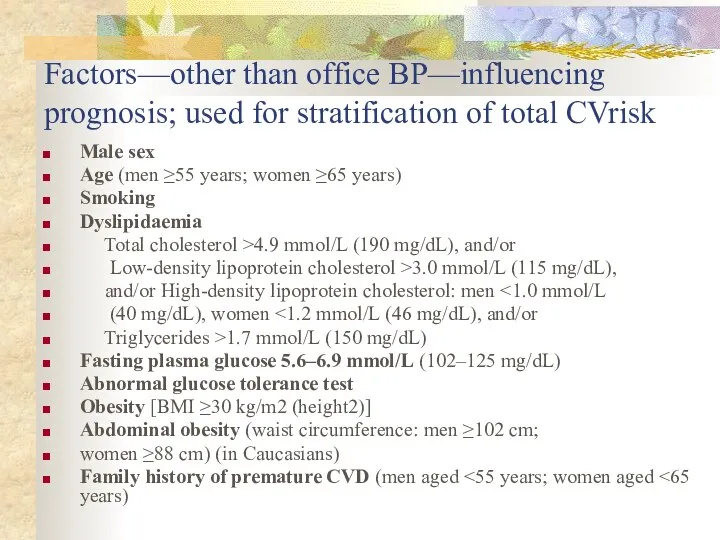
- 18. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk Male sex Age (men ≥55
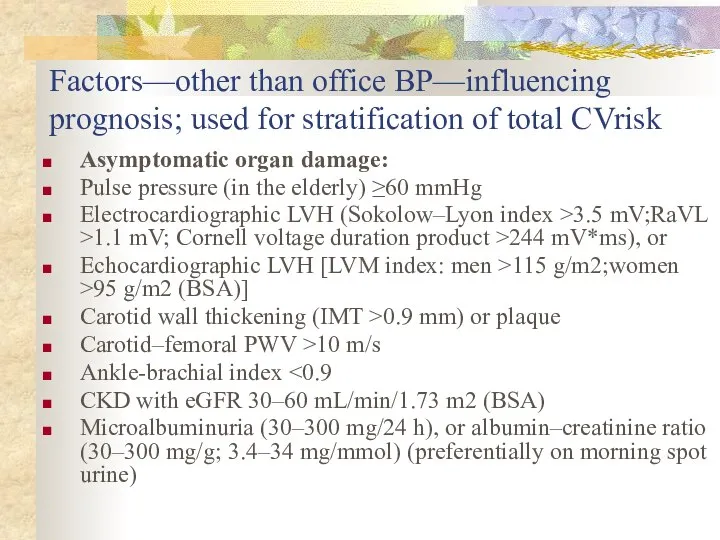
- 19. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk Asymptomatic organ damage: Pulse pressure
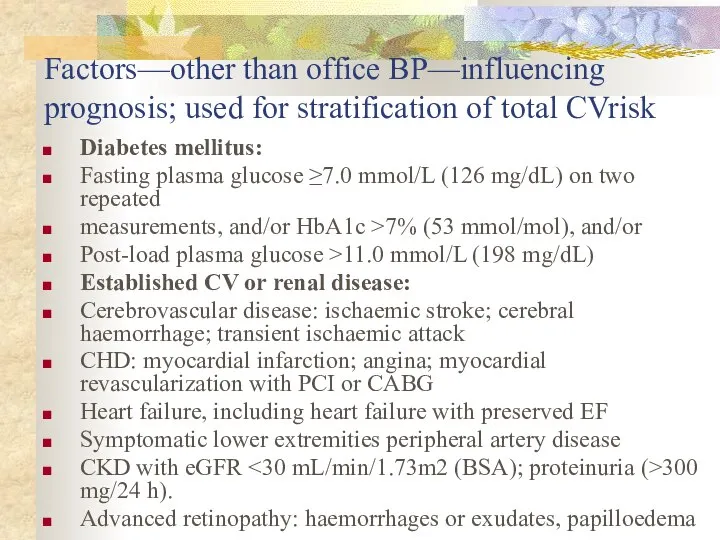
- 20. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk Diabetes mellitus: Fasting plasma glucose
- 22. MEASUREMENT OF BLOOD PRESSURE Use a machine that has been validated, well maintained and properly calibrated
- 23. Types of measurement: Office BP Home BP Daily monitoring of BP!!!
- 24. ‘White coat‘ hypertension? Up to 13-15% of apparent hypertension in the clinic may 'normal BP' when
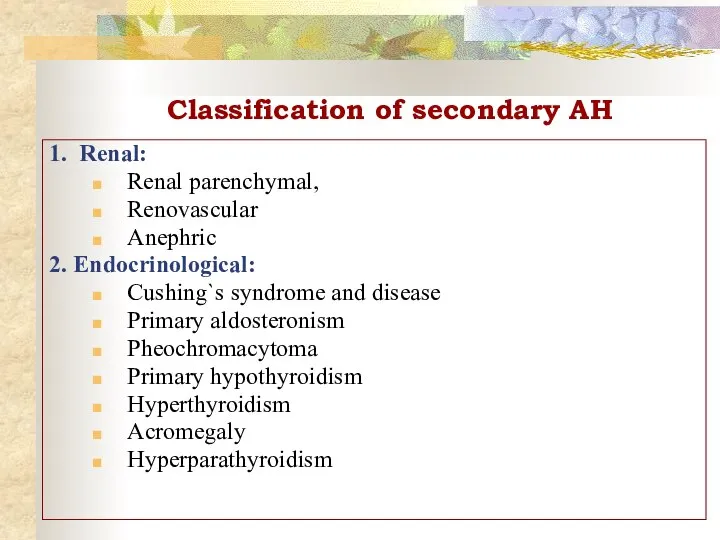
- 25. Classification of secondary AH 1. Renal: Renal parenchymal, Renovascular Anephric 2. Endocrinological: Cushing`s syndrome and disease
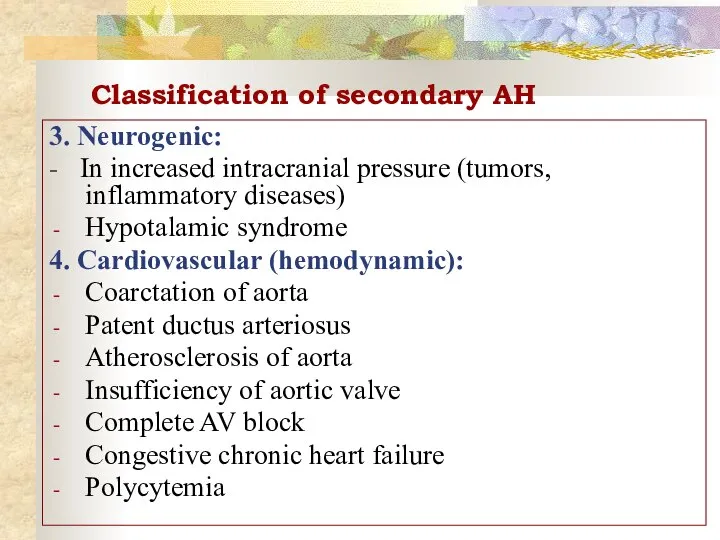
- 26. Classification of secondary AH 3. Neurogenic: - In increased intracranial pressure (tumors, inflammatory diseases) Hypotalamic syndrome
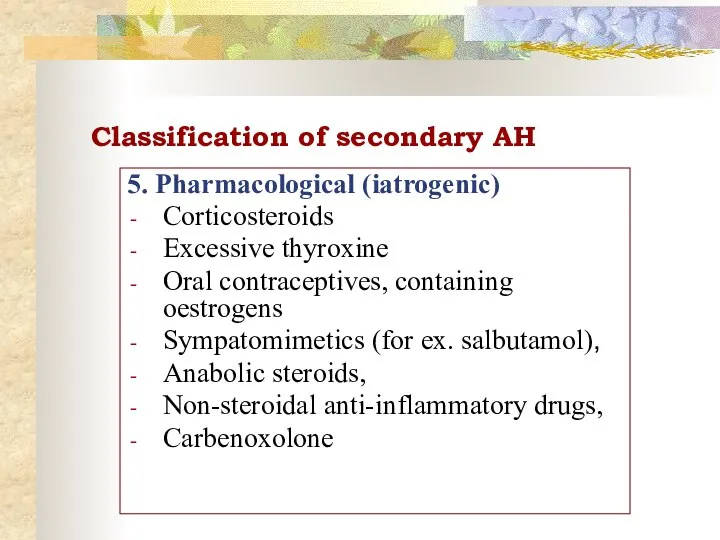
- 27. Classification of secondary AH 5. Pharmacological (iatrogenic) Corticosteroids Excessive thyroxine Oral contraceptives, containing oestrogens Sympatomimetics (for
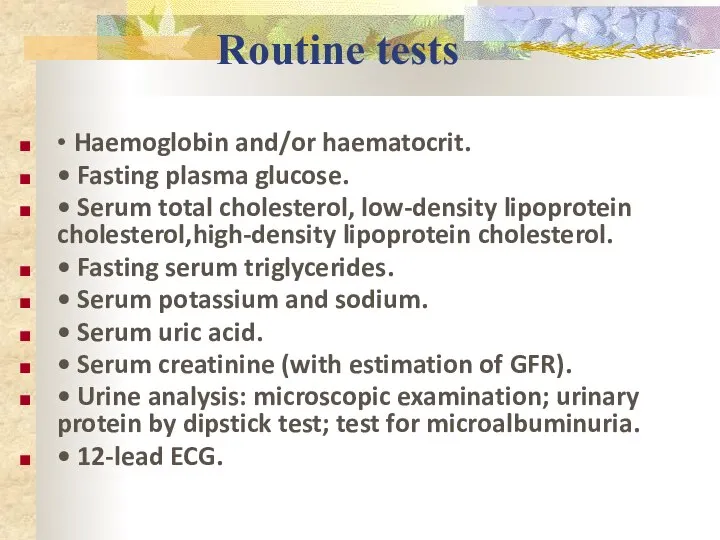
- 28. Routine tests • Haemoglobin and/or haematocrit. • Fasting plasma glucose. • Serum total cholesterol, low-density lipoprotein
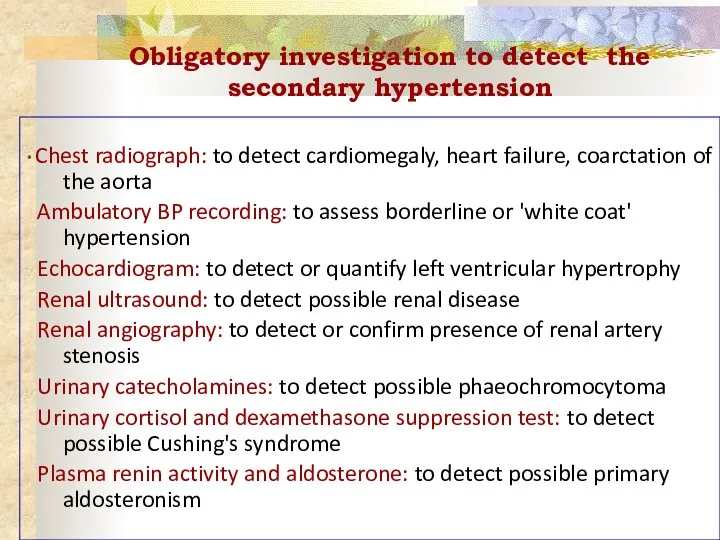
- 29. Obligatory investigation to detect the secondary hypertension • Chest radiograph: to detect cardiomegaly, heart failure, coarctation
- 30. Life style modifications Lose weight, if overweight Limit alcohol intake Increase physical activity Reduce salt intake
- 31. Principles of treatment 1. Etiological: elimination of causes 2. Non-pharmacological treatment: weight reduction, stop alcogol and
- 32. Treatment strategies 1) Treatment is permanent and continuous 2) Begin treatment with a minimal dose and
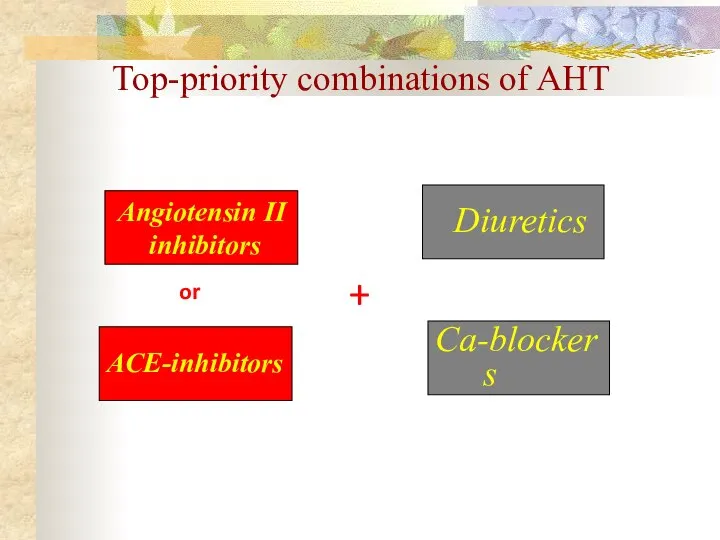
- 33. Angiotensin II inhibitors ACE-inhibitors Diuretics Ca-blockers or + Top-priority combinations of AHT
- 34. Renal parenchymal AH: chronic glomerulonephritis, pyelonephritis, polycystic renal disease, diabetic nephropathy, congenital diseases of kidneys, vasculitis
- 35. Diagnostics of renal parenchymal diseases urinary syndrome (proteinuria, leucocyturia, hematuria, cylindruria, bacteriuria), testing of the renal
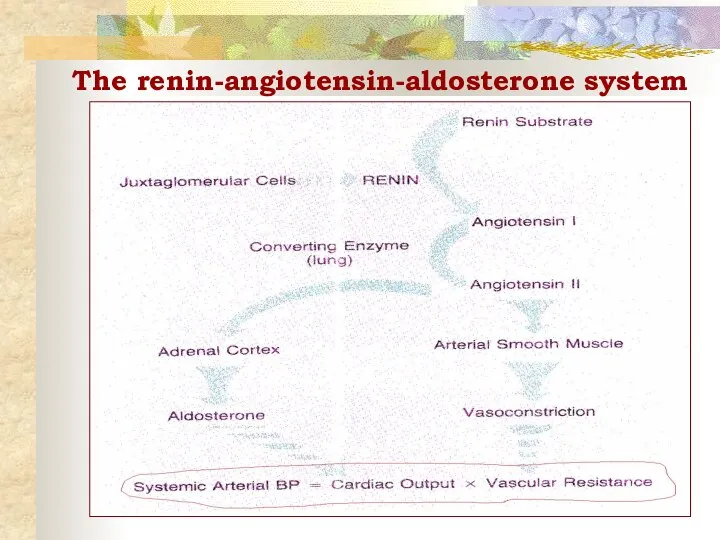
- 36. The renin-angiotensin-aldosterone system
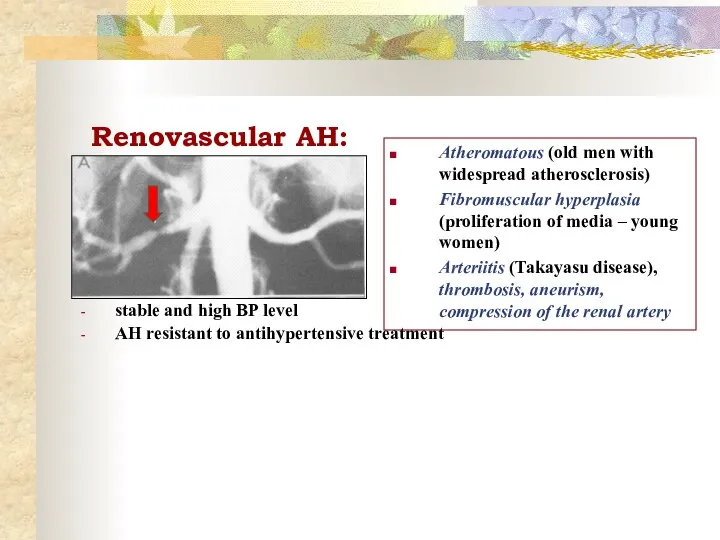
- 37. Renovascular AH: stable and high BP level AH resistant to antihypertensive treatment Atheromatous (old men with
- 38. Diagnostics and treatment of renovascular desease Auscultation: murmur in the paraumbilical region Renal arteriogram Doppler-echocardiography of
- 39. Pheochromacytoma Rare tumor of chromaffin cells (adrenal medulla of the kidneys or the sympathetic ganglia in
- 40. Diagnostics and treatment of Pheochromacytoma Diagnosis: Elevated urinary excretion of vanillylmandelic acid (VMA) and metanephrine Hyperglycemia,
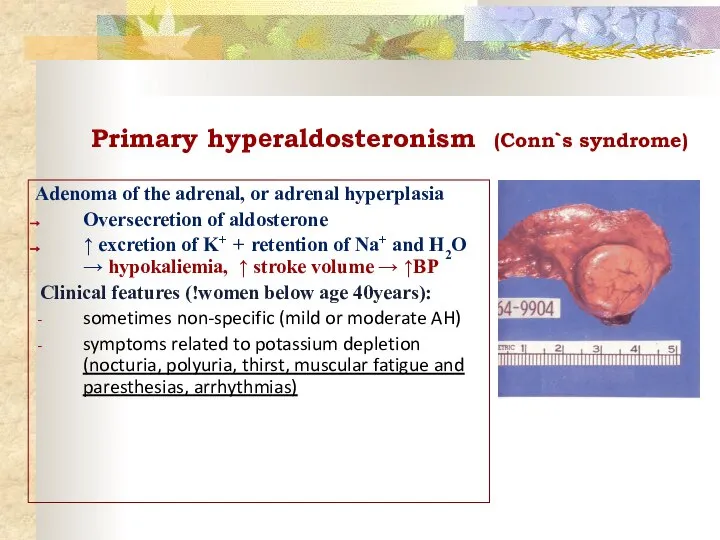
- 41. Primary hypеraldosteronism (Conn`s syndrome) Adenoma of the adrenal, or adrenal hyperplasia Oversecretion of aldosterone ↑ excretion
- 42. Diagnostics and treatment of Conn`s syndrome Diagnosis: Hypokaliemia ( ↓ Renin, ↑ Aldosterone in plasma Identification
- 43. Cushing`s disease & Cushing`s syndrome Cushing`s disease is a primary tumor of the anterior pituitary gland
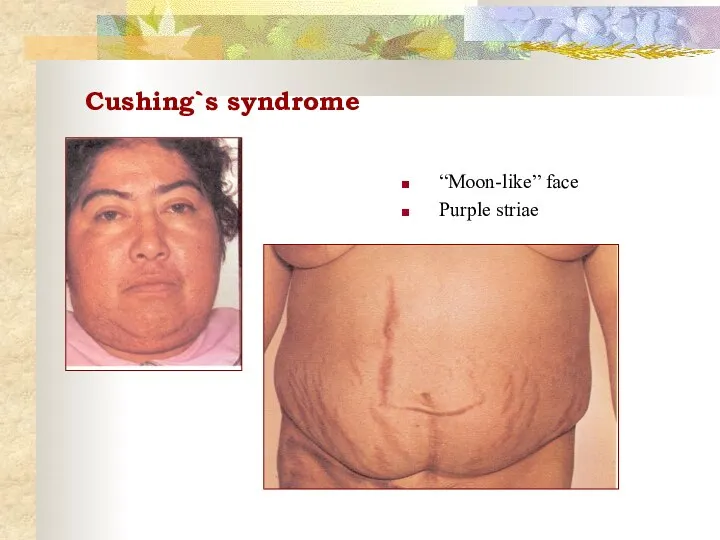
- 44. Cushing`s syndrome “Moon-like” face Purple striae
- 45. Diagnostics and treatment of Cushing`s disease Diagnosis: ↑ ACTH and Cortisol level in the blood Visualization
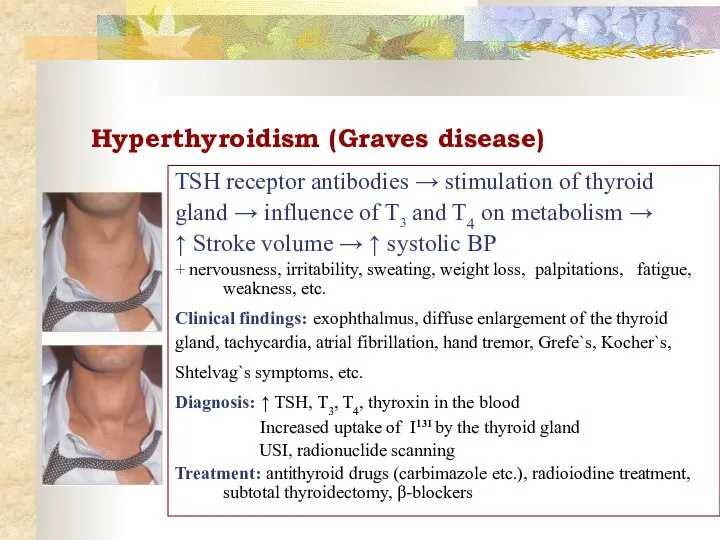
- 46. Hyperthyroidism (Graves disease) TSH receptor antibodies → stimulation of thyroid gland → influence of T3 and
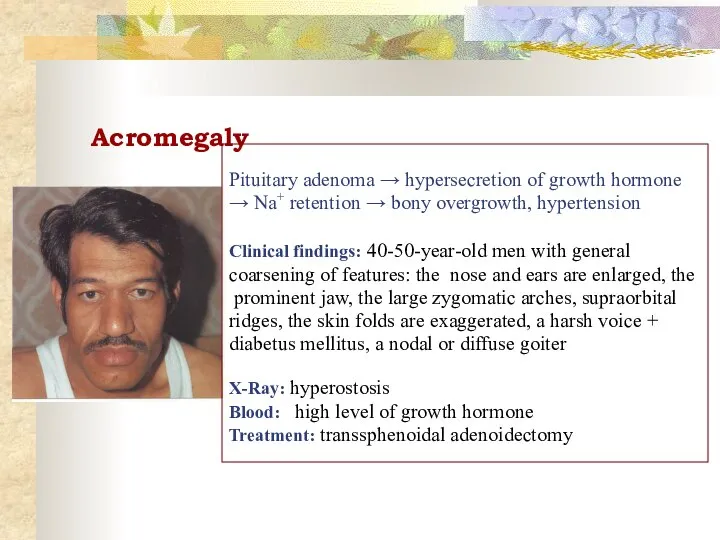
- 47. Acromegaly Pituitary adenoma → hypersecretion of growth hormone → Na+ retention → bony overgrowth, hypertension Clinical
- 48. Cardiovascular (hemodynamic) AH: 1. Atherosclerosis of the aorta (↑ regidity of aorta) - elderly and senile
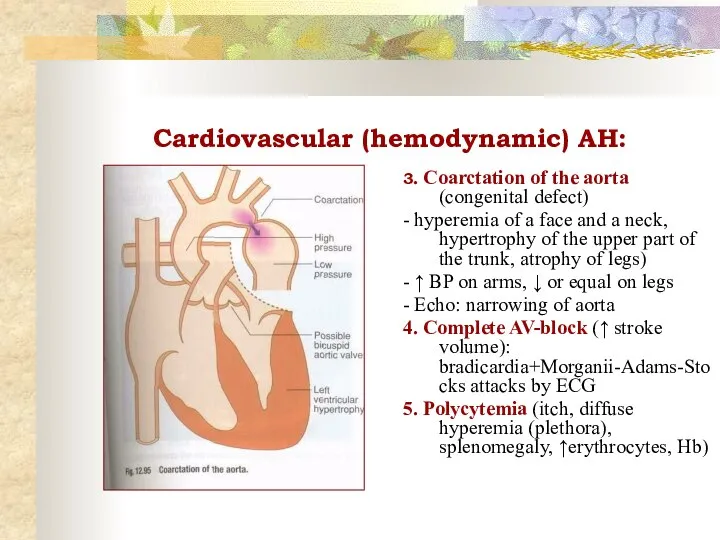
- 49. Cardiovascular (hemodynamic) AH: 3. Coarctation of the aorta (congenital defect) - hyperemia of a face and
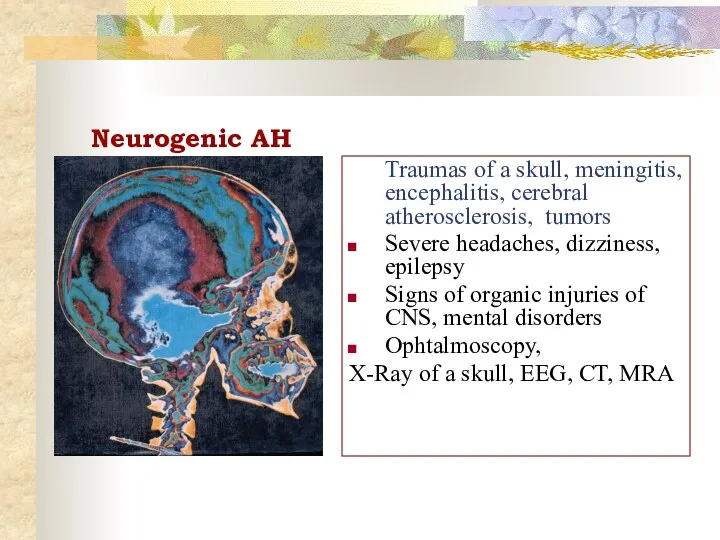
- 50. Neurogenic AH Traumas of a skull, meningitis, encephalitis, cerebral atherosclerosis, tumors Severe headaches, dizziness, epilepsy Signs
- 52. Скачать презентацию
 Healthy lifestyle
Healthy lifestyle домашние часы _ by Artem Morozov
домашние часы _ by Artem Morozov Процесс прохождения клиента (нарушения рабочего листа). Злоупотребления при сдаче а/м по системе Трейд-ин
Процесс прохождения клиента (нарушения рабочего листа). Злоупотребления при сдаче а/м по системе Трейд-ин Випускова робота Особливості застосування дощувальної техніки на чорноземних грунтах Горностаївського району
Випускова робота Особливості застосування дощувальної техніки на чорноземних грунтах Горностаївського району Чайные сервиз
Чайные сервиз Гимнастика для глаз
Гимнастика для глаз 3D телевидение
3D телевидение Село родное в объективе
Село родное в объективе Электрические схемы
Электрические схемы La tour Еiffel
La tour Еiffel Anketa_Knigi_stilya_2
Anketa_Knigi_stilya_2 Тренажёр Личные местоимения 3 класс
Тренажёр Личные местоимения 3 класс Уфа. Фото-кастинг
Уфа. Фото-кастинг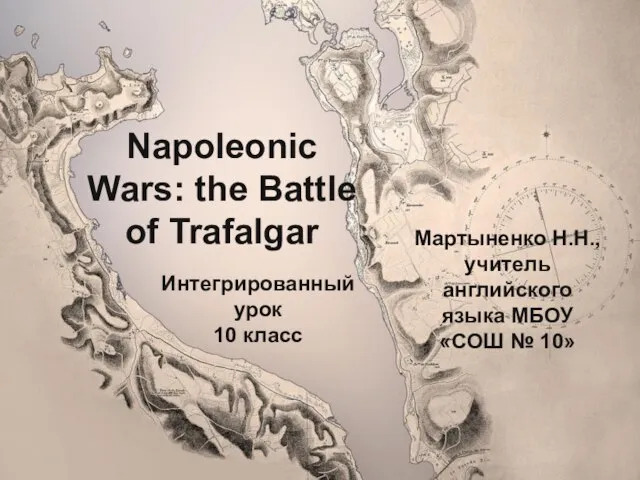 20120514_trafalgar
20120514_trafalgar Stagioni nel cinema
Stagioni nel cinema Lesson_1_Этапы_процесса_разработки
Lesson_1_Этапы_процесса_разработки Що читають знаменитості
Що читають знаменитості Нитинол
Нитинол South Korea
South Korea Изготовление крышек центрального отверстия автомобильных дисков с применением аддитивных технологий
Изготовление крышек центрального отверстия автомобильных дисков с применением аддитивных технологий блоксхема1
блоксхема1 Расчет основания фундамента на несущую способность
Расчет основания фундамента на несущую способность Производство. Выполняемые работы и услуги
Производство. Выполняемые работы и услуги Дороги которые мы выбираем
Дороги которые мы выбираем pREZENT-1
pREZENT-1 Материалы применяемые в машино и приборостроении
Материалы применяемые в машино и приборостроении BAE Systems, Inc. Sectors at a Glance
BAE Systems, Inc. Sectors at a Glance Көліктік моторлардың қалдық газдарының уыттылығын төмендетудің негізгі әдістері
Көліктік моторлардың қалдық газдарының уыттылығын төмендетудің негізгі әдістері