Содержание
- 2. General anaesthetics (GAs) are drugs which produce reversible loss of all sensation and consciousness. The cardinal
- 3. Mechanism of action of anaesthetics Anaesthetic potency correlates well with lipid solubility. Anaesthetics might dissolve in
- 4. Properties of an ideal anaesthetic A. For the patient: It should be pleasant, nonirritating, should not
- 5. C. For the anaesthetist: Its administration should be easy, controllable. Heart, liver and other organs should
- 6. Stages of general anaesthesia I. Stage of analgesia starts from beginning of anaesthetic inhalation and lasts
- 8. General anaesthesia usually involves the administration of different drugs For premedication, For induction of anaesthesia, and
- 9. CLASSIFICATION Inhalational Gas: Nitrous oxide Volatile liquids: Ether, Halothane, Enflurane, Isoflurane, Desflurane, Sevoflurane Intravenous Fast acting
- 10. Nitrous oxide is not potent enough to use as a sole anaesthetic agent, but it is
- 11. Isoflurane is more soluble in blood than sevoflurane or enflurane and so onset and recovery are
- 12. Propofol is the most widely used intravenous anaesthetic. It induces anaesthesia within 30 s and is
- 13. Ketamine may be given by intramuscular or intravenous injection. It is analgesic in subanaesthetic doses, but
- 14. COMPLICATIONS OF GENERAL ANAESTHESIA A. During anaesthesia Respiratory depression. Cardiac arrhythmias, asystole. Fall in BP. Salivation,
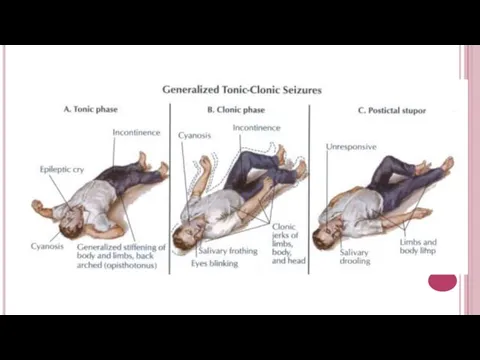
- 15. ANTIEPILEPTIC DRUGS Epilepsy is a chronic disease in which seizures result from the abnormal discharge of
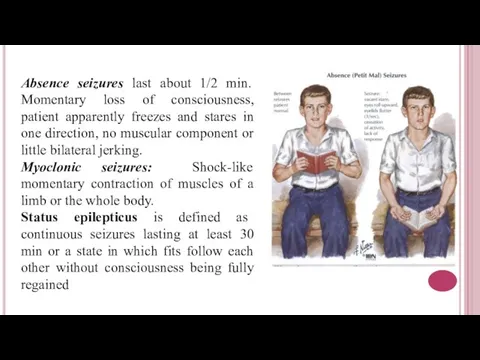
- 17. Absence seizures last about 1/2 min. Momentary loss of consciousness, patient apparently freezes and stares in
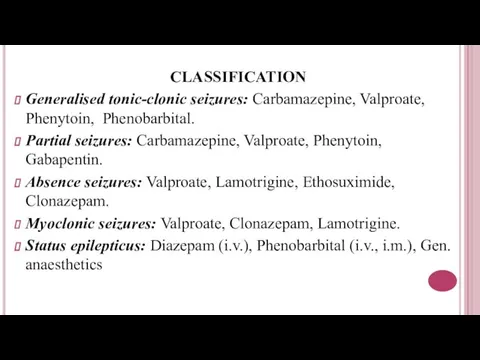
- 18. CLASSIFICATION Generalised tonic-clonic seizures: Carbamazepine, Valproate, Phenytoin, Phenobarbital. Partial seizures: Carbamazepine, Valproate, Phenytoin, Gabapentin. Absence seizures:
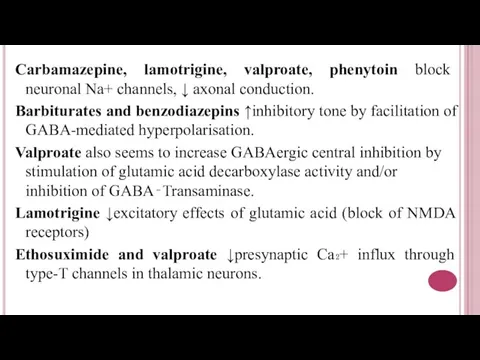
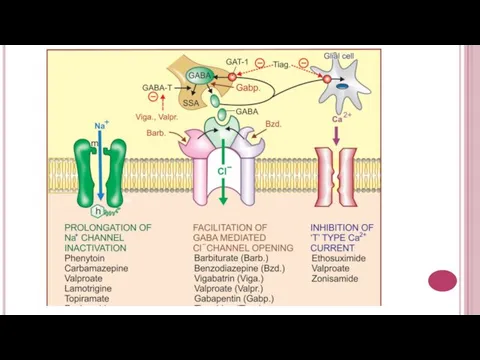
- 19. Carbamazepine, lamotrigine, valproate, phenytoin block neuronal Na+ channels, ↓ axonal conduction. Barbiturates and benzodiazepins ↑inhibitory tone
- 21. Phenytoin. Pharmacokinetics – variable absorption, induction of P450s; Side effects: CNS depression, gingival hyperplasia, osteomalacia (↓
- 22. Valproate can be used for migraines. Inhibits P450s. Side effects: hepatotoxicity, thrombocytopenia, pancretitis, alopecia, teratogenicity (spinal
- 23. Antiparkinsonian Drugs. These are drugs that have a therapeutic effect in parkinsonism. Parkinsonism. It is an
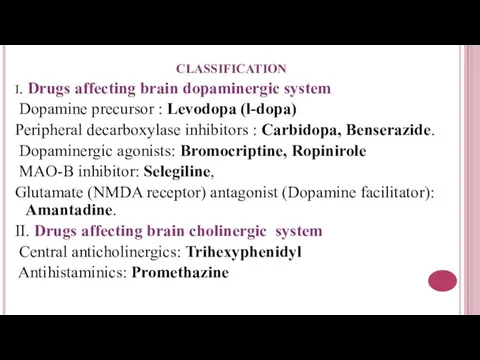
- 26. CLASSIFICATION I. Drugs affecting brain dopaminergic system Dopamine precursor : Levodopa (l-dopa) Peripheral decarboxylase inhibitors :
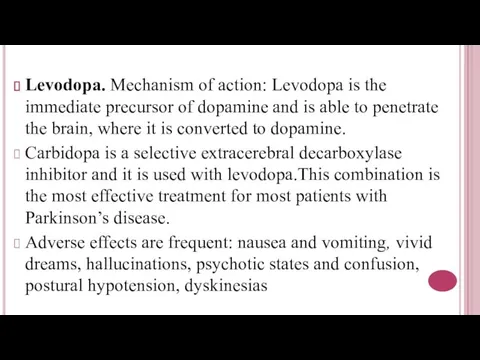
- 28. Levodopa. Mechanism of action: Levodopa is the immediate precursor of dopamine and is able to penetrate
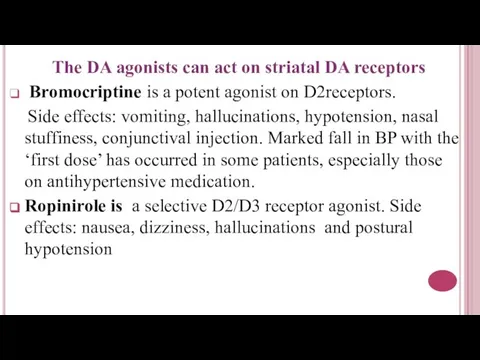
- 30. The DA agonists can act on striatal DA receptors Bromocriptine is a potent agonist on D2receptors.
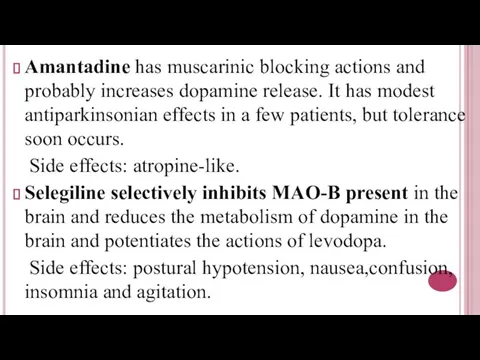
- 31. Amantadine has muscarinic blocking actions and probably increases dopamine release. It has modest antiparkinsonian effects in
- 33. Скачать презентацию






 Проектирование подстанции 110/10 кВ в г. Пермь
Проектирование подстанции 110/10 кВ в г. Пермь Зачем искусство
Зачем искусство Сварочные выпрямители и их эксплуатация
Сварочные выпрямители и их эксплуатация Встречные забои
Встречные забои Проектирование и организация работы отделения по ремонту роликовых подшипников
Проектирование и организация работы отделения по ремонту роликовых подшипников Связующие для неводных окрасочных составов. Тема № 4. Растительные масла
Связующие для неводных окрасочных составов. Тема № 4. Растительные масла Выпуск 2008 представляет
Выпуск 2008 представляет История Обществознание
История Обществознание 20120225_nabokov_poseshchenie_muzeya
20120225_nabokov_poseshchenie_muzeya игра Собери фрукты
игра Собери фрукты Критическая и максимально применяемая частоты. Методы исследования ионосферы
Критическая и максимально применяемая частоты. Методы исследования ионосферы Победа ковалась в тылу
Победа ковалась в тылу Технология и организация высокотехнологичного производства
Технология и организация высокотехнологичного производства 20120305_velikiy_dar_tvorchestva
20120305_velikiy_dar_tvorchestva Пламенный Серафим
Пламенный Серафим Приемы работы_2017
Приемы работы_2017 Event DJ AndRave pres-2
Event DJ AndRave pres-2 Технология возведения работ нулевого цикла
Технология возведения работ нулевого цикла Автоматическое регулирование расхода природного газа в двухванном сталеплавильном агрегате ДСПА-32
Автоматическое регулирование расхода природного газа в двухванном сталеплавильном агрегате ДСПА-32 Производство хлебобулочных изделий
Производство хлебобулочных изделий Алгоритмы и исполнители
Алгоритмы и исполнители Волшебный мир коми сказок
Волшебный мир коми сказок Маленькие истории о больших музыкантах
Маленькие истории о больших музыкантах Тварина - живий організм
Тварина - живий організм ПрезентацияБайкалЮгповерпоинт (1)
ПрезентацияБайкалЮгповерпоинт (1) Когда музыка не нуждается в словах
Когда музыка не нуждается в словах Термическая обработка металлов и сплавов
Термическая обработка металлов и сплавов Основы производственных процессов. Офсетные печатные формы
Основы производственных процессов. Офсетные печатные формы