Содержание
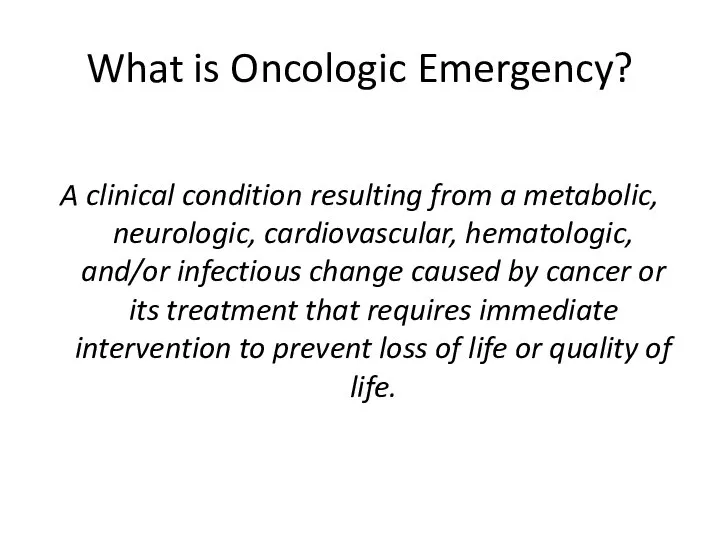
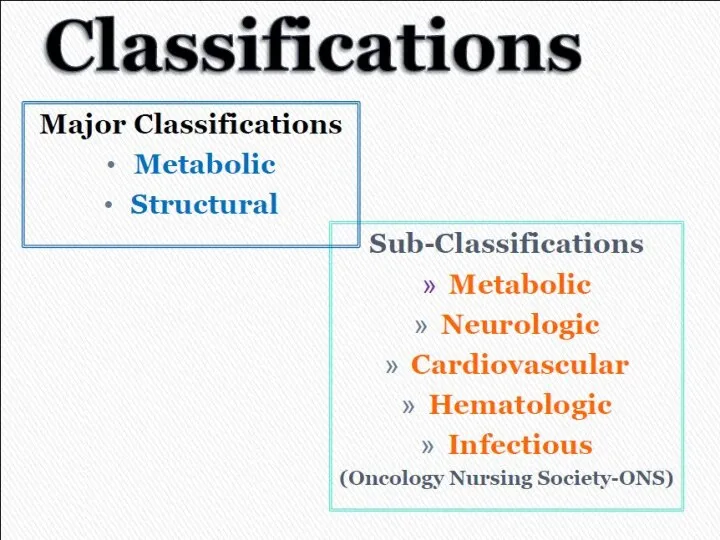
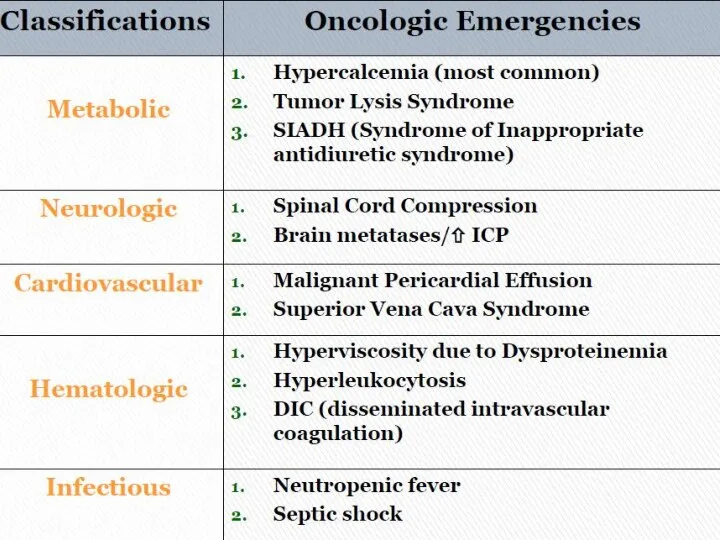
- 2. What is Oncologic Emergency? A clinical condition resulting from a metabolic, neurologic, cardiovascular, hematologic, and/or infectious
- 5. METABOLIC
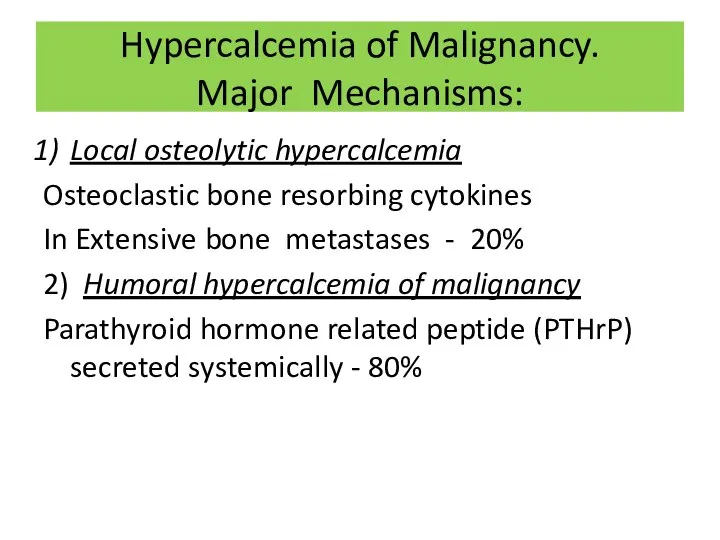
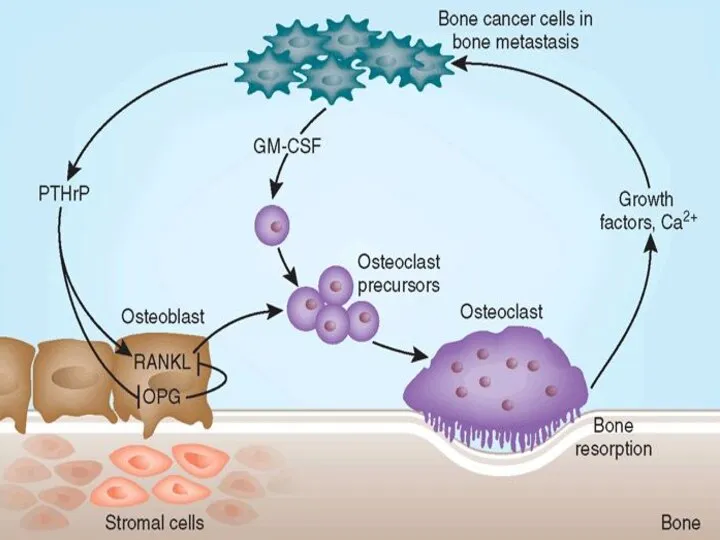
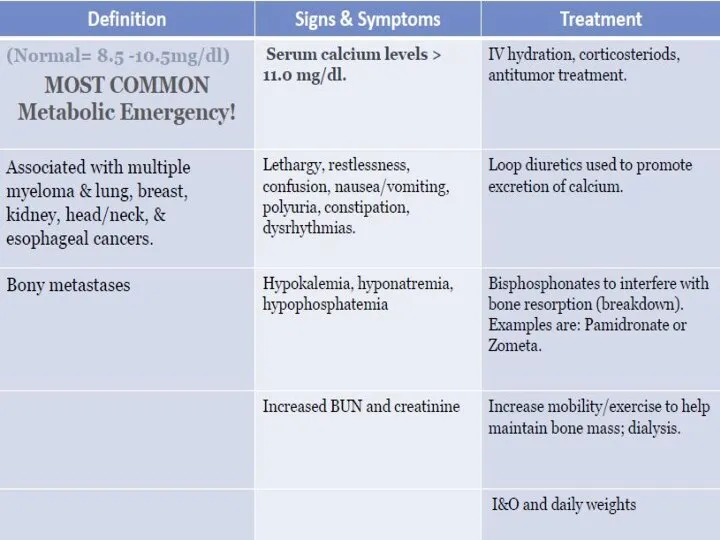
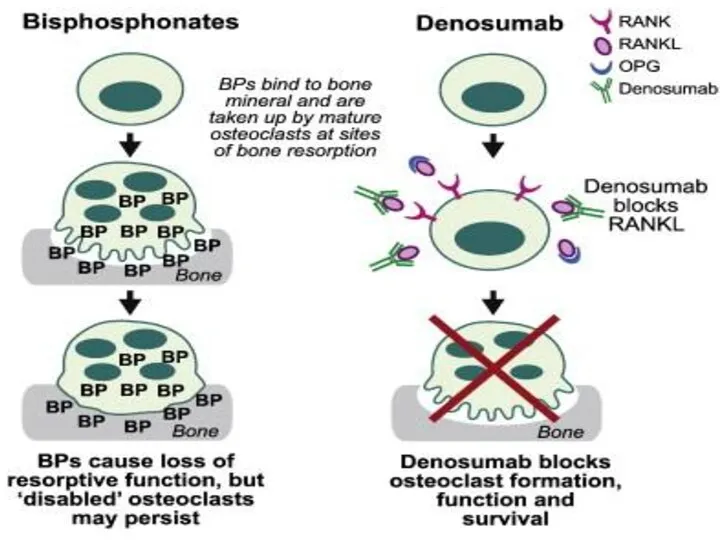
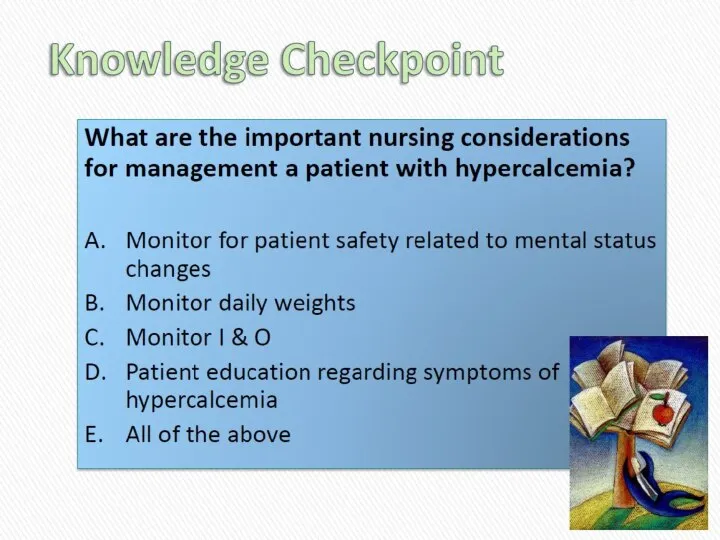
- 6. Hypercalcemia of Malignancy. Major Mechanisms: Local osteolytic hypercalcemia Osteoclastic bone resorbing cytokines In Extensive bone metastases
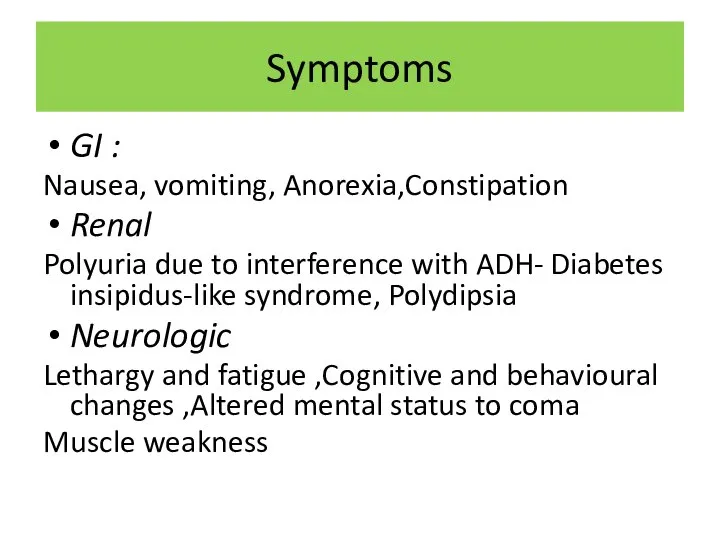
- 8. Symptoms GI : Nausea, vomiting, Anorexia,Constipation Renal Polyuria due to interference with ADH- Diabetes insipidus-like syndrome,
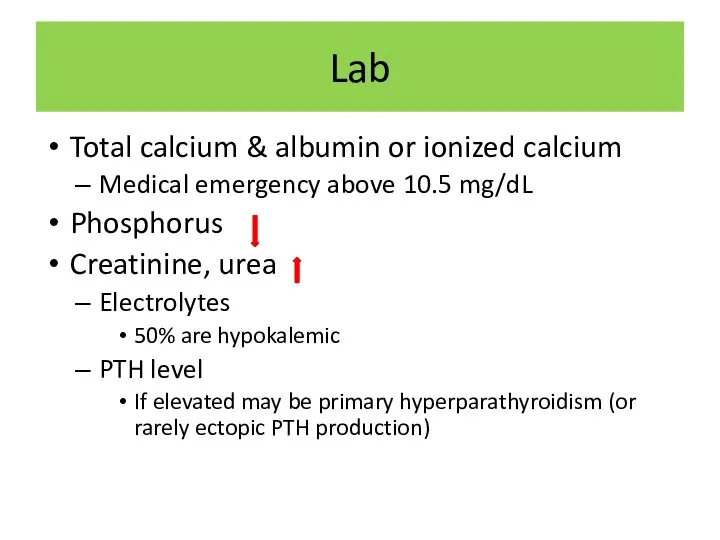
- 9. Lab Total calcium & albumin or ionized calcium Medical emergency above 10.5 mg/dL Phosphorus Creatinine, urea
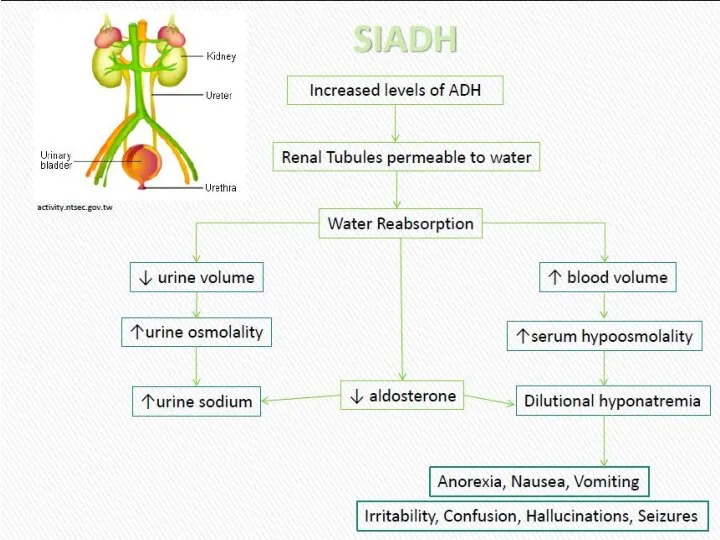
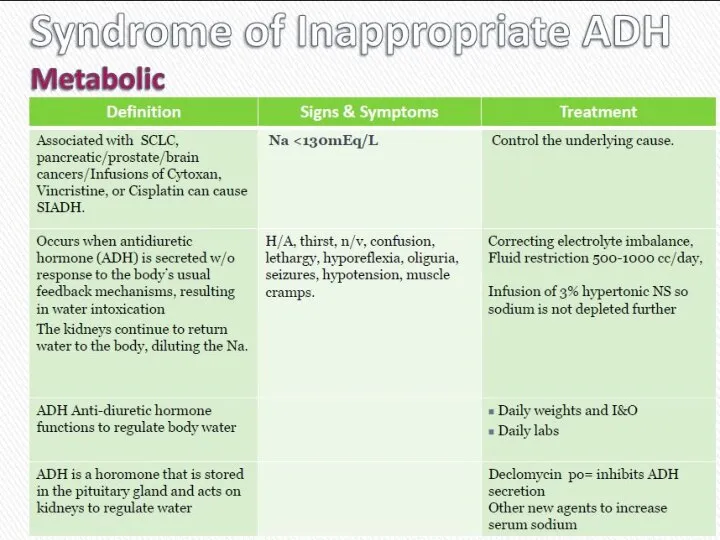
- 13. Cиндром неадекватной секреции антидиуретического гормона (SIADH)
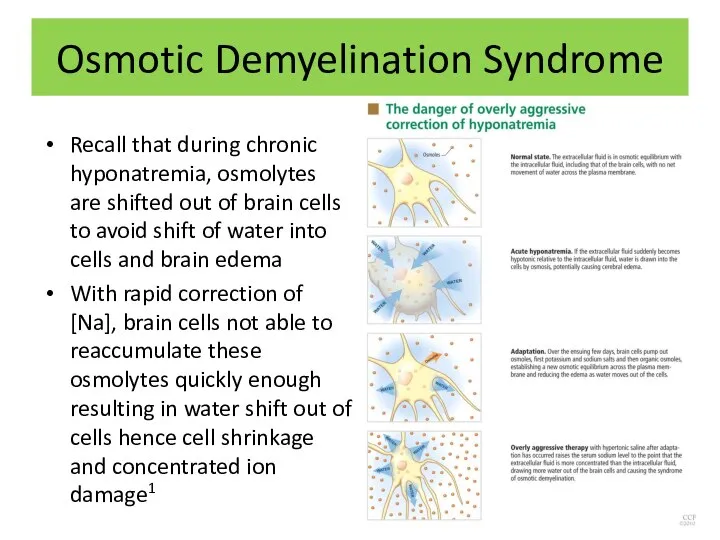
- 15. Osmotic Demyelination Syndrome Recall that during chronic hyponatremia, osmolytes are shifted out of brain cells to
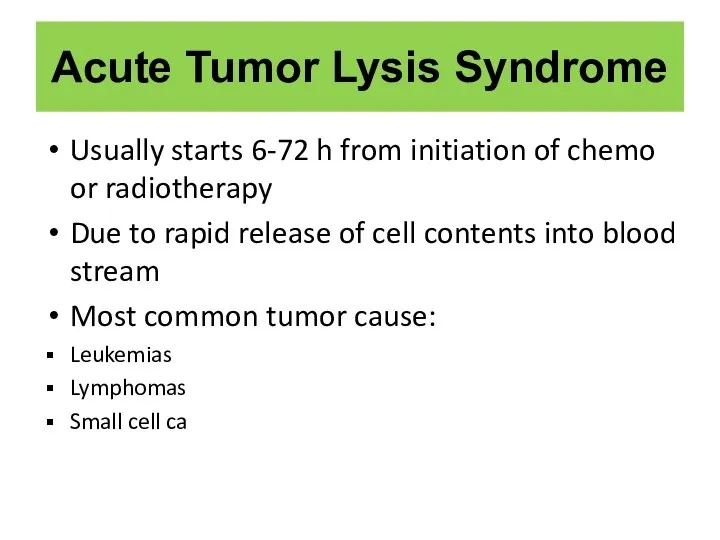
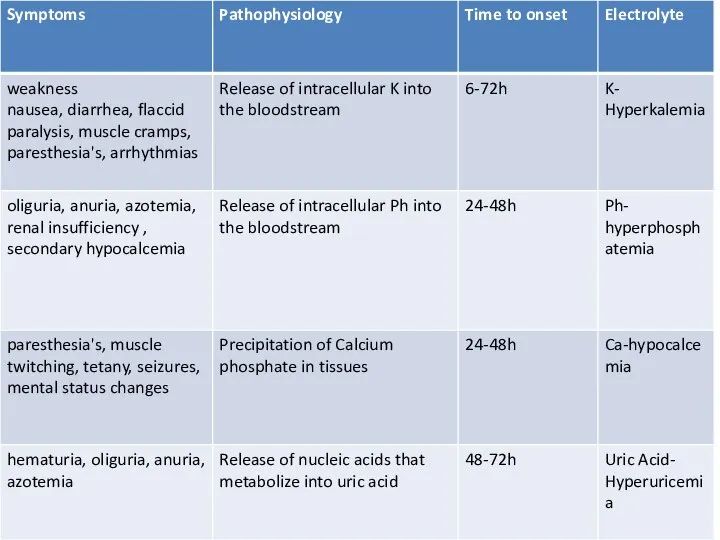
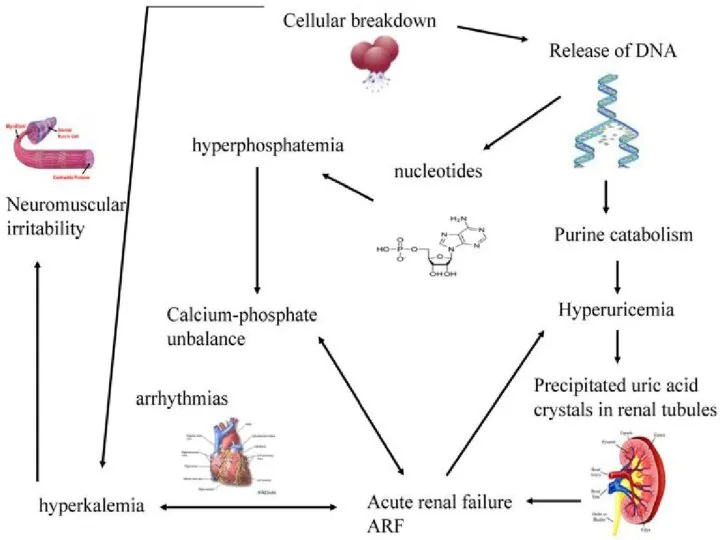
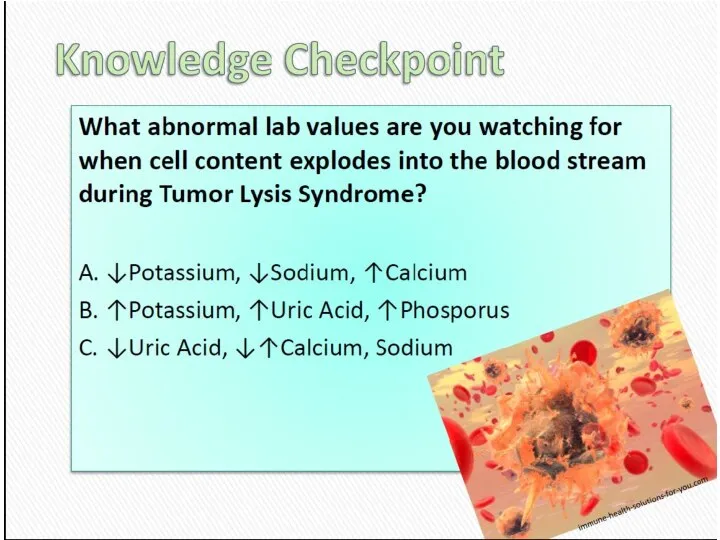
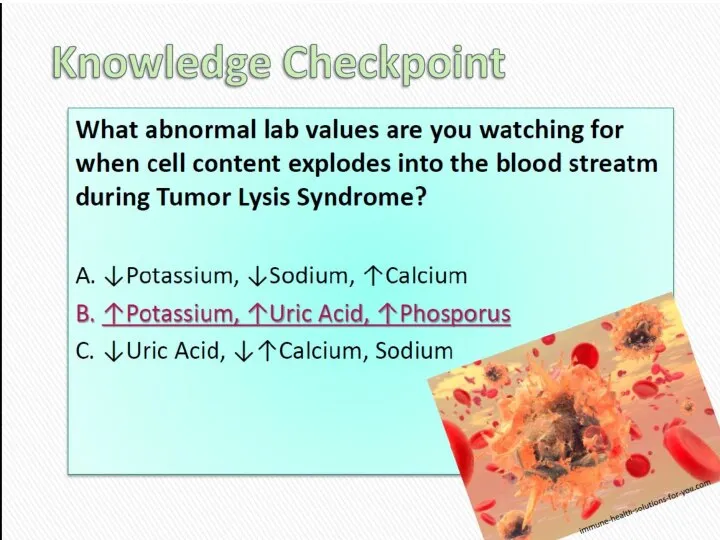
- 18. Acute Tumor Lysis Syndrome Usually starts 6-72 h from initiation of chemo or radiotherapy Due to
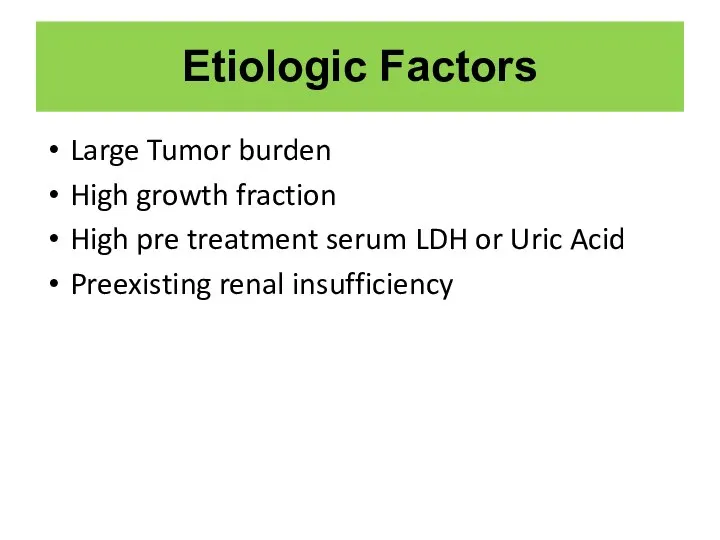
- 19. Etiologic Factors Large Tumor burden High growth fraction High pre treatment serum LDH or Uric Acid
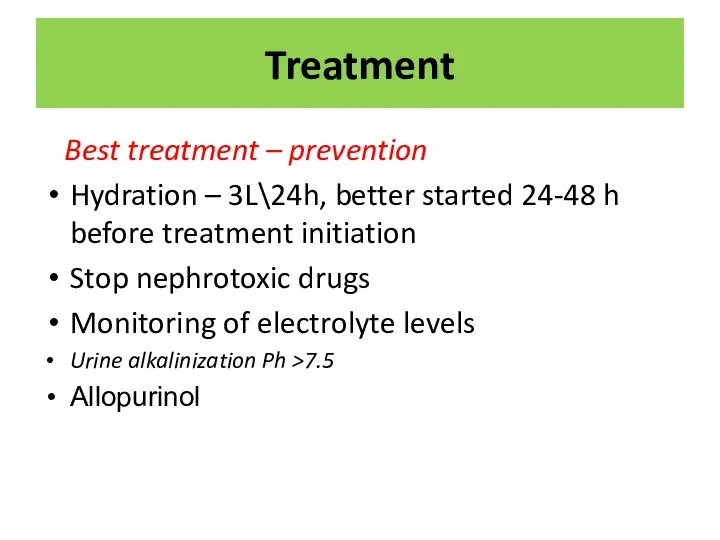
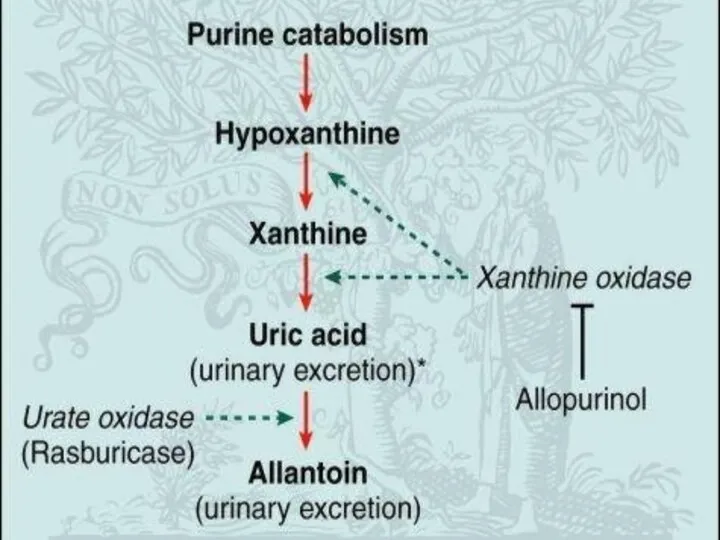
- 22. Treatment Best treatment – prevention Hydration – 3L\24h, better started 24-48 h before treatment initiation Stop
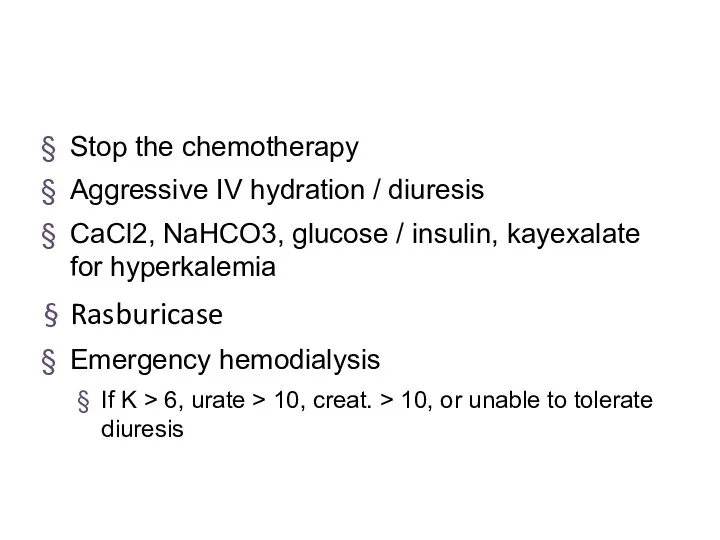
- 23. Stop the chemotherapy Aggressive IV hydration / diuresis CaCl2, NaHCO3, glucose / insulin, kayexalate for hyperkalemia
- 27. STRUCTURAL: Neurologic emergencies
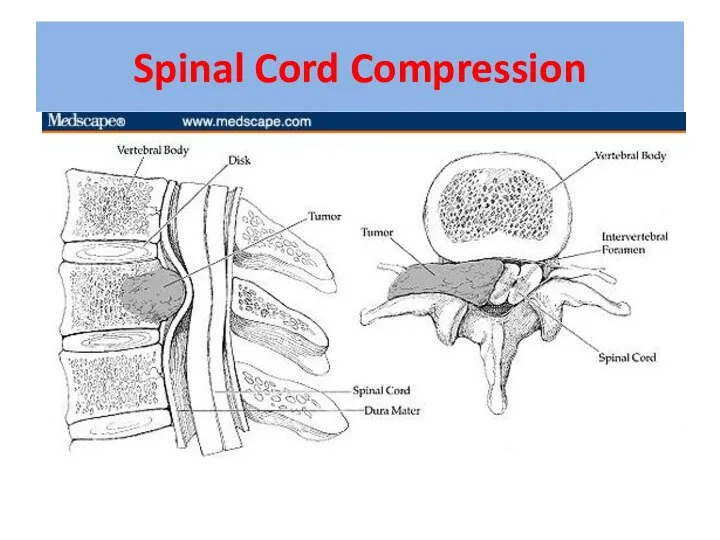
- 28. Spinal Cord Compression
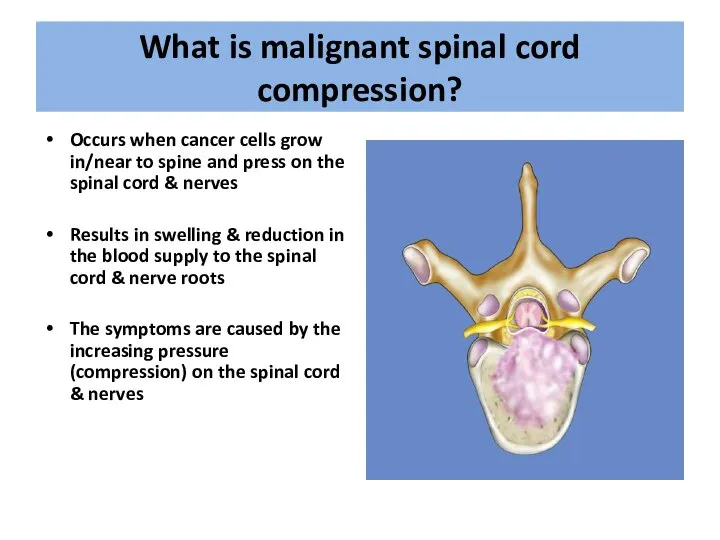
- 29. What is malignant spinal cord compression? Occurs when cancer cells grow in/near to spine and press
- 30. Most commonly seen in Breast Lung Prostate Lymphoma Myeloma About 10% of patients with cancer overall
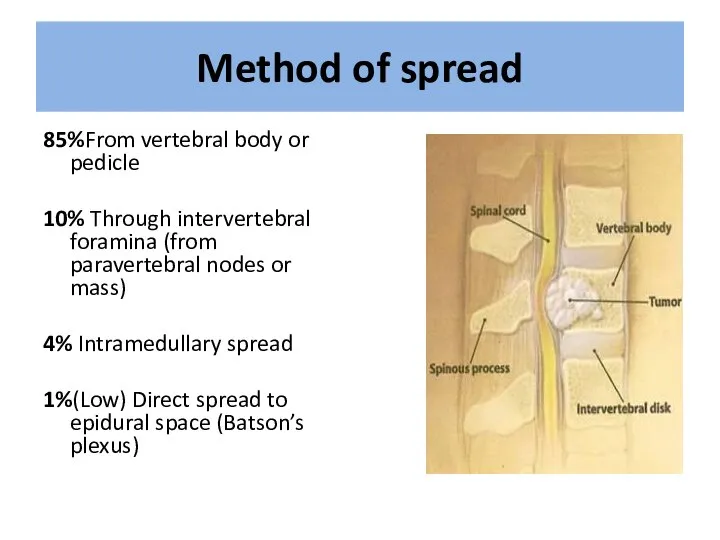
- 31. Method of spread 85%From vertebral body or pedicle 10% Through intervertebral foramina (from paravertebral nodes or
- 32. Location Thoracic spine 60-70% Lumbosacral spine 20-30% Cervical and sacral spine less then 10% each
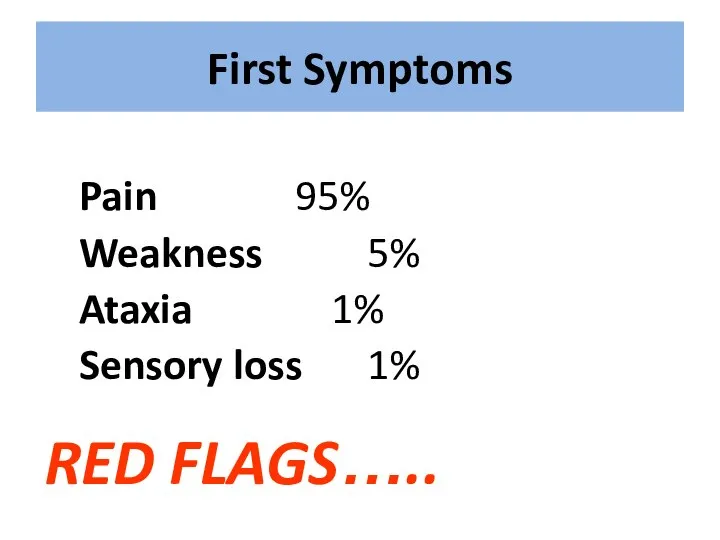
- 34. First Symptoms Pain 95% Weakness 5% Ataxia 1% Sensory loss 1% RED FLAGS…..
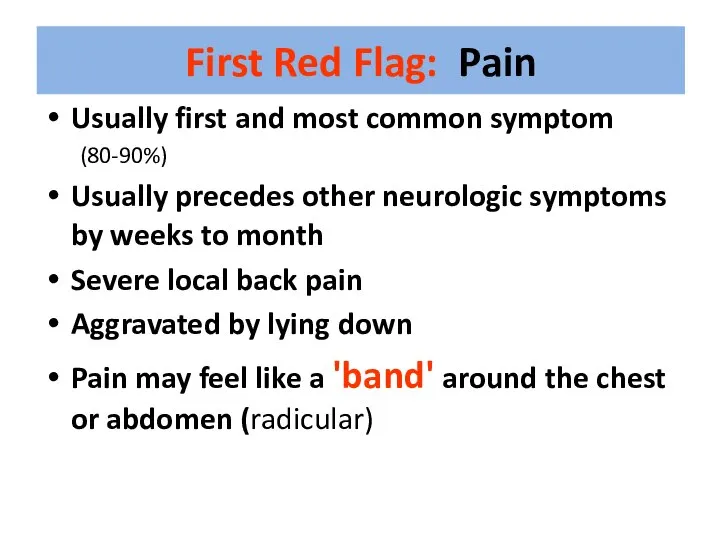
- 35. First Red Flag: Pain Usually first and most common symptom (80-90%) Usually precedes other neurologic symptoms
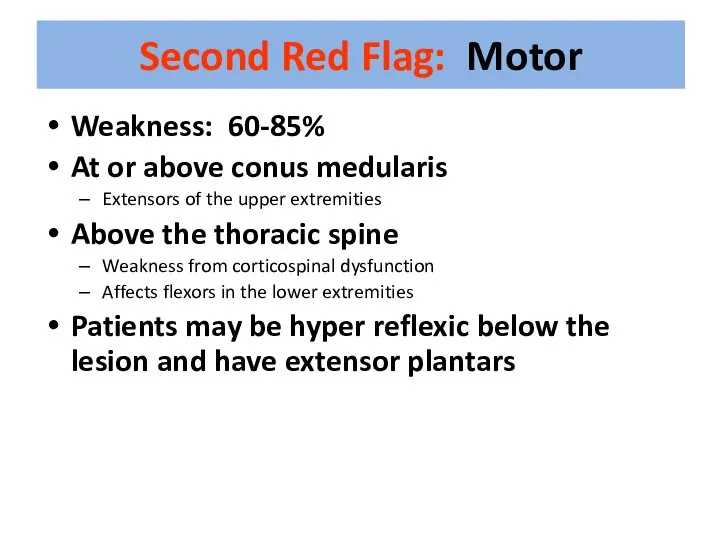
- 36. Second Red Flag: Motor Weakness: 60-85% At or above conus medularis Extensors of the upper extremities
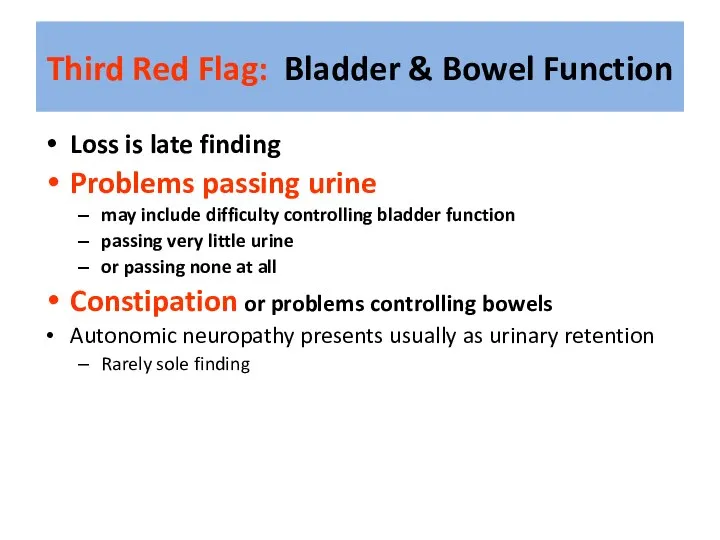
- 37. Third Red Flag: Bladder & Bowel Function Loss is late finding Problems passing urine may include
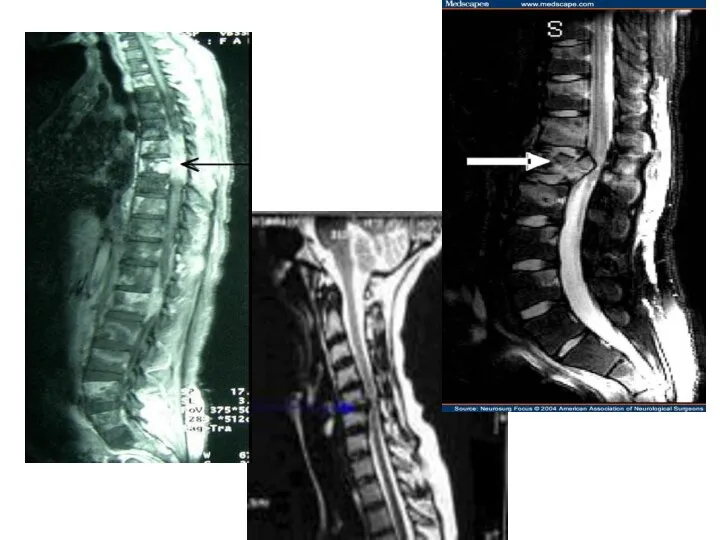
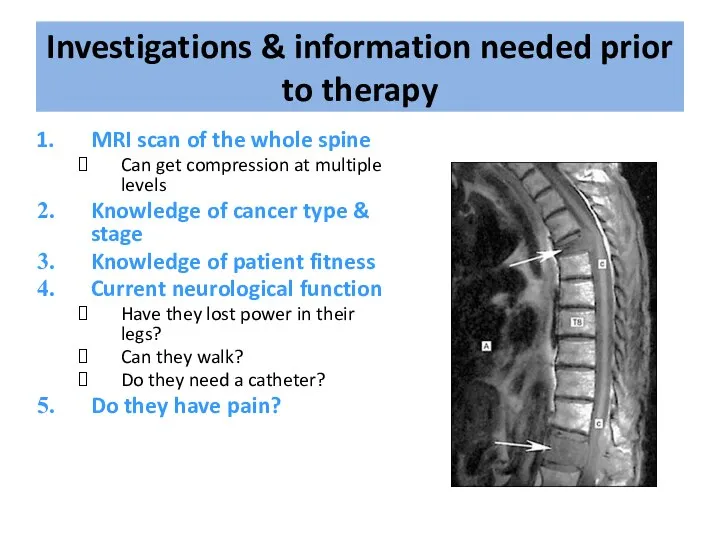
- 38. Investigations & information needed prior to therapy MRI scan of the whole spine Can get compression
- 39. Treatment options include: Immobilisation Steroids & gastric protection Analgesia Surgery – decompression & stabilisation of the
- 40. Indications for Surgery • Unknown primary tumour • Relapse post RT • Progression while on RT
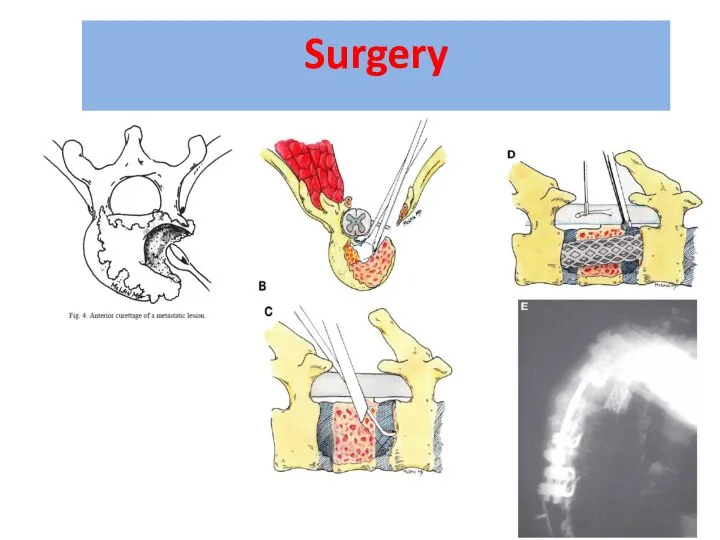
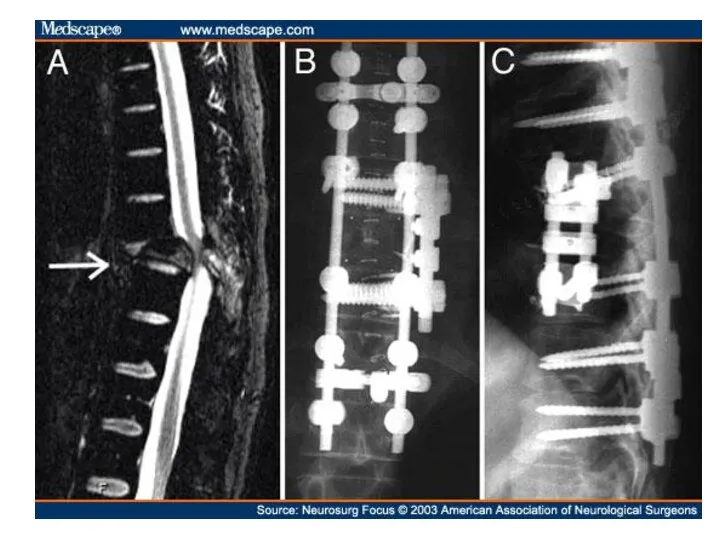
- 41. Surgery
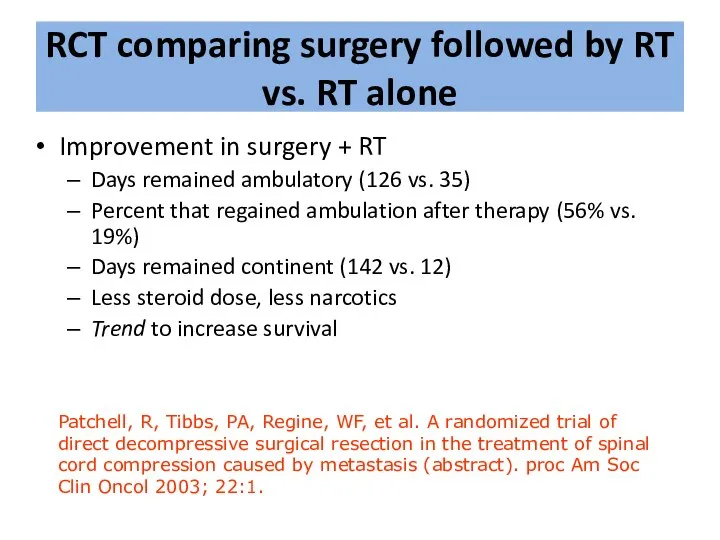
- 45. Improvement in surgery + RT Days remained ambulatory (126 vs. 35) Percent that regained ambulation after
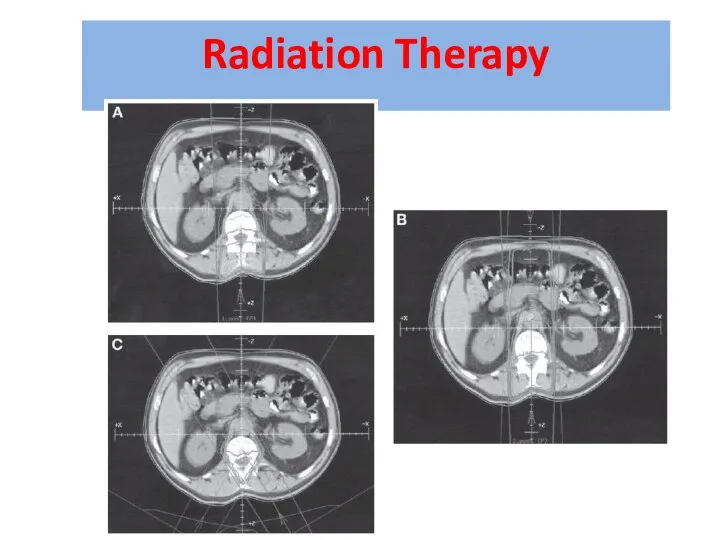
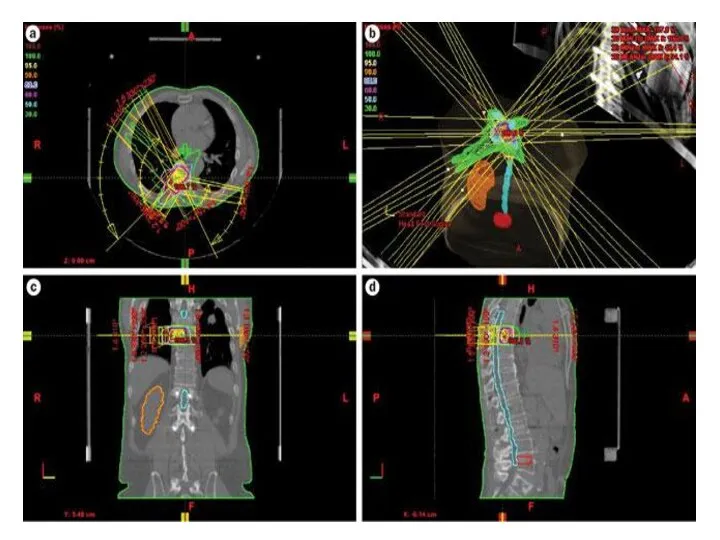
- 46. Radiation Therapy
- 48. Prognosis Median survival with MSCC is 6 months Ambulatory patients with radiosensitive tumours have the best
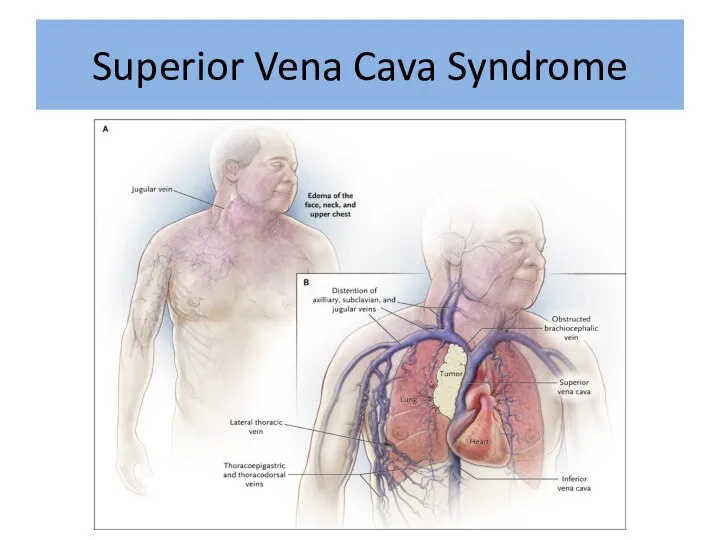
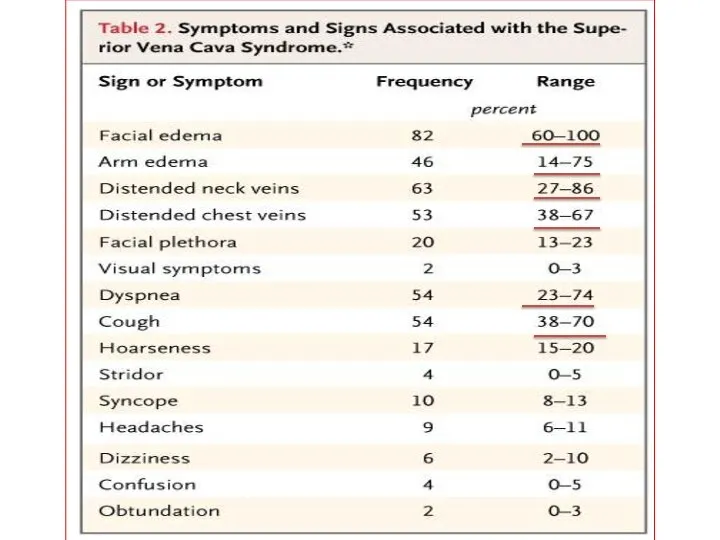
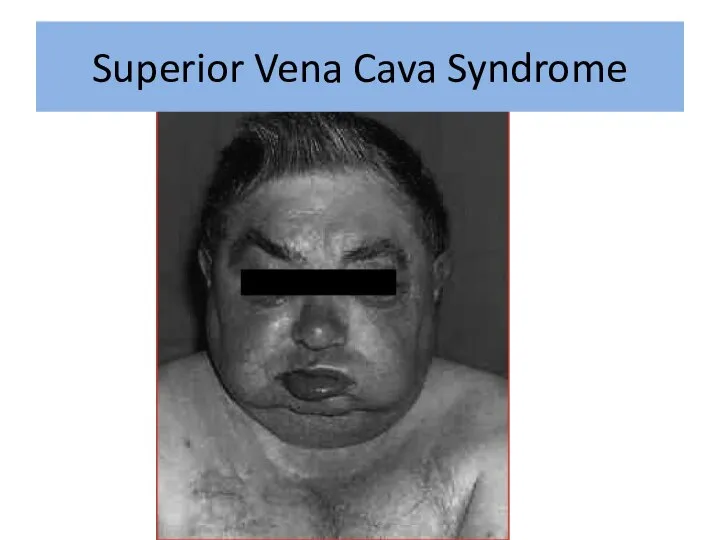
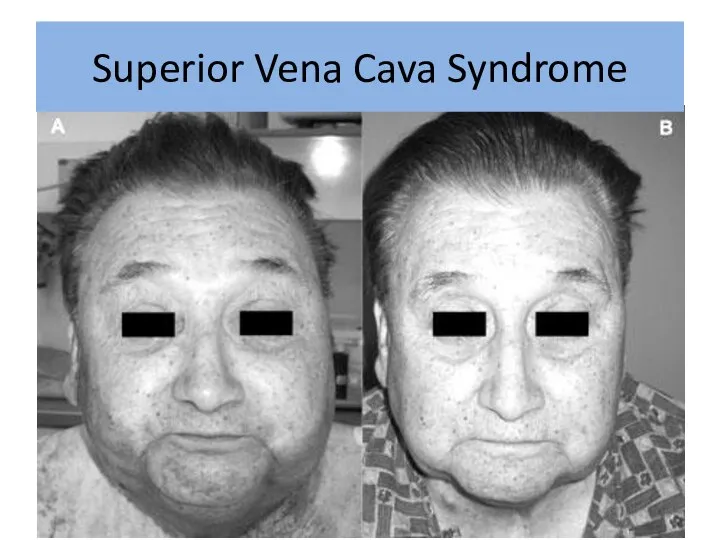
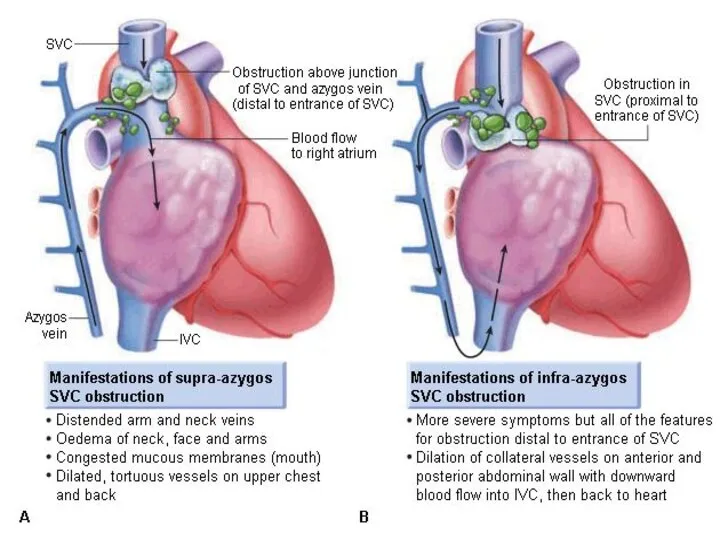
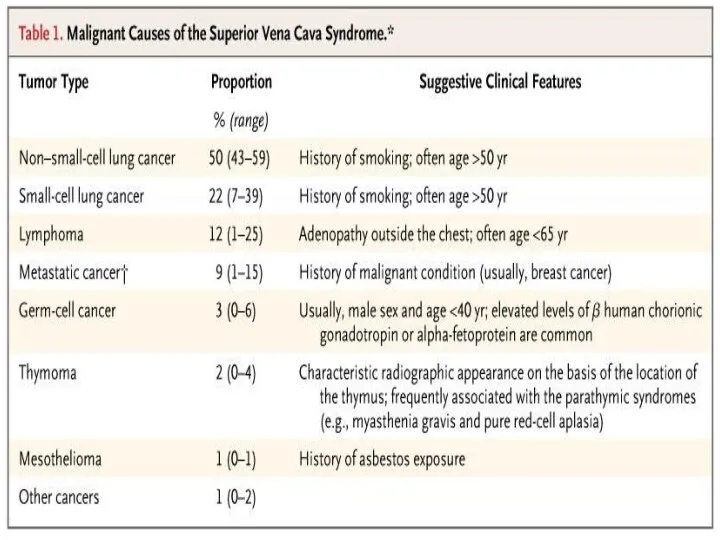
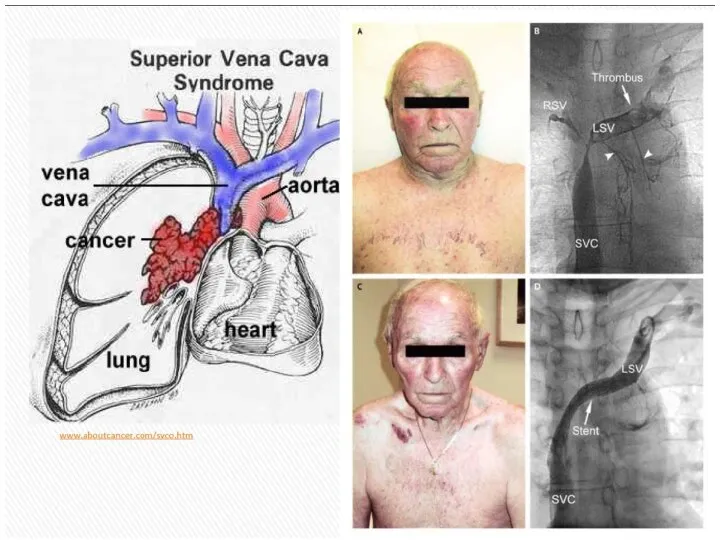
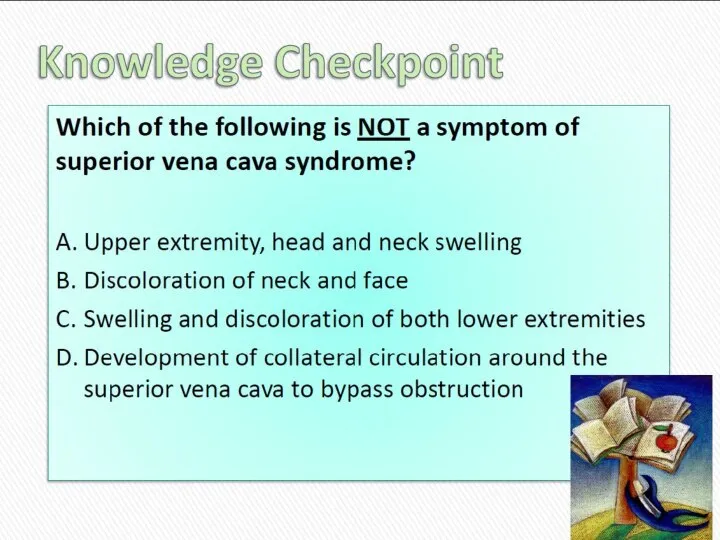
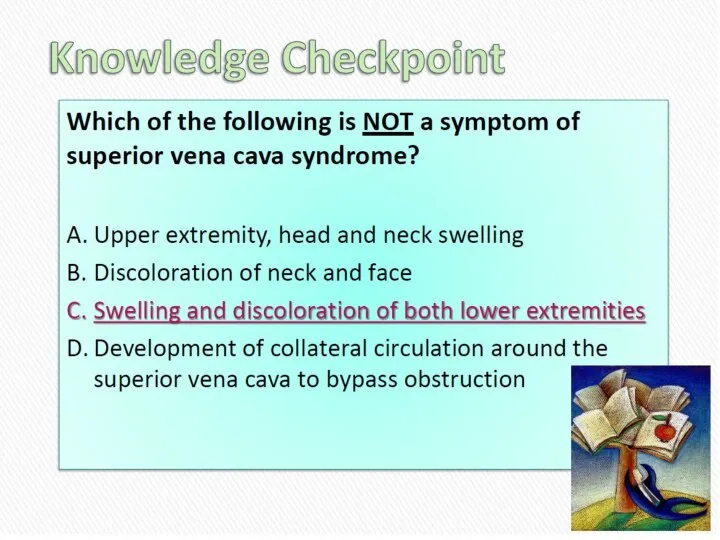
- 49. Superior Vena Cava Syndrome
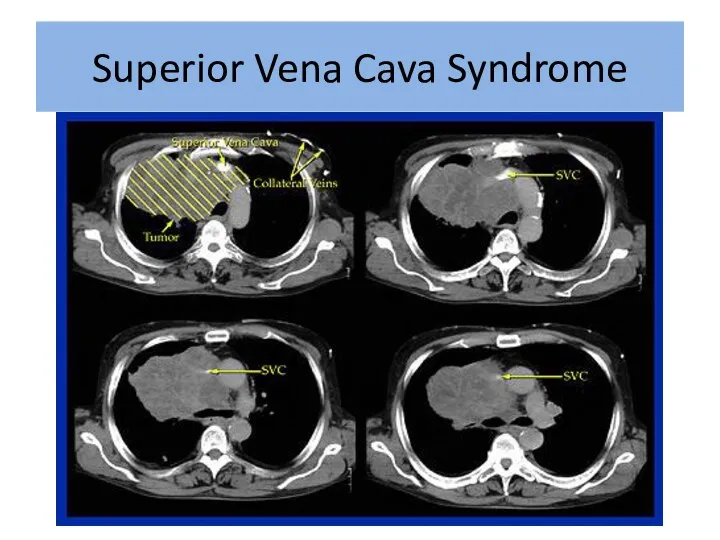
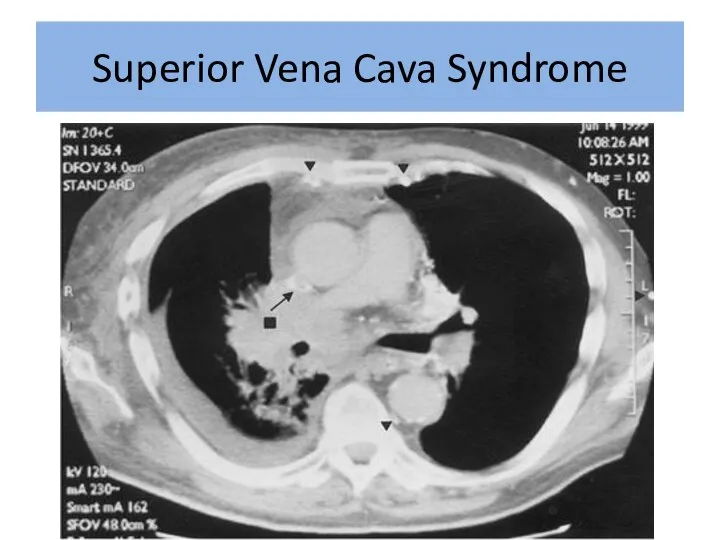
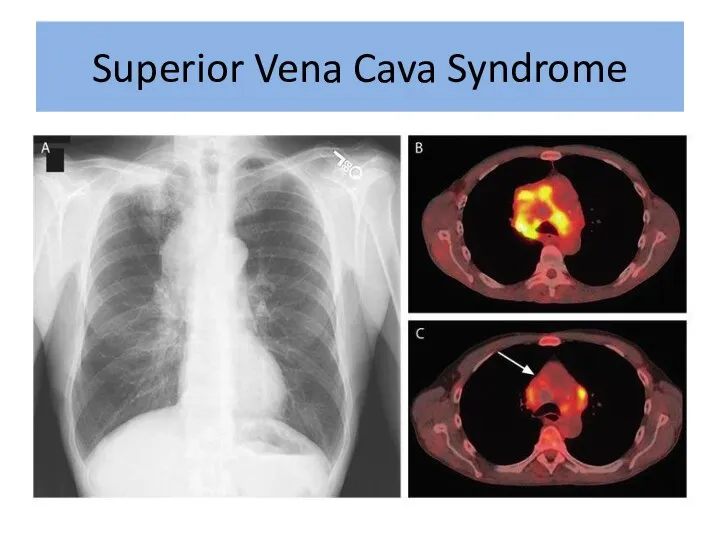
- 51. Superior Vena Cava Syndrome
- 52. Superior Vena Cava Syndrome
- 54. Superior Vena Cava Syndrome
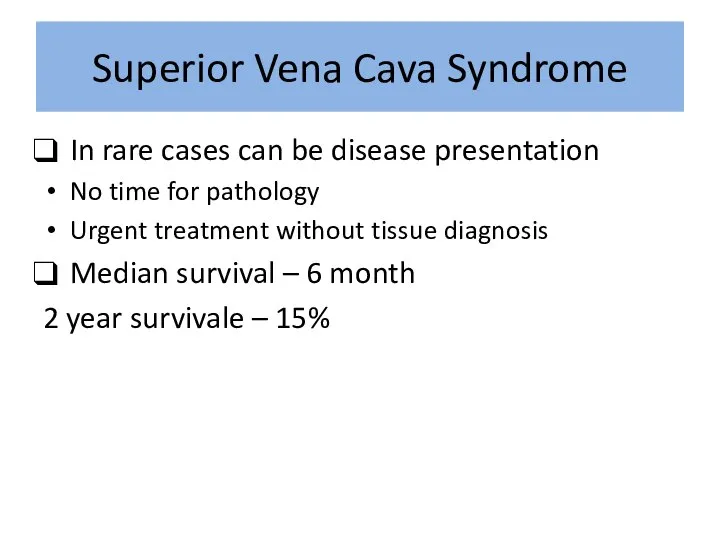
- 57. In rare cases can be disease presentation No time for pathology Urgent treatment without tissue diagnosis
- 58. Exeption: Treatment Sensitive Tumors NHLs, germ cells, and limited-stage small cell lung cancers usually respond to
- 59. Superior Vena Cava Syndrome
- 60. Superior Vena Cava Syndrome
- 61. Superior Vena Cava Syndrome
- 62. Treatment Options Radiation therapy Chemotherapy Intraluminal Stent +supportive care
- 63. Supportive Care: Rest Head elevation Oxygen Diuretics Anticoagulation Steroids Avoid high volume fluid infusion through upper
- 64. Intraluminal Stents Endovascular placement under fluoroscopy Patients who have recurrent disease in previously irradiated fields Tumors
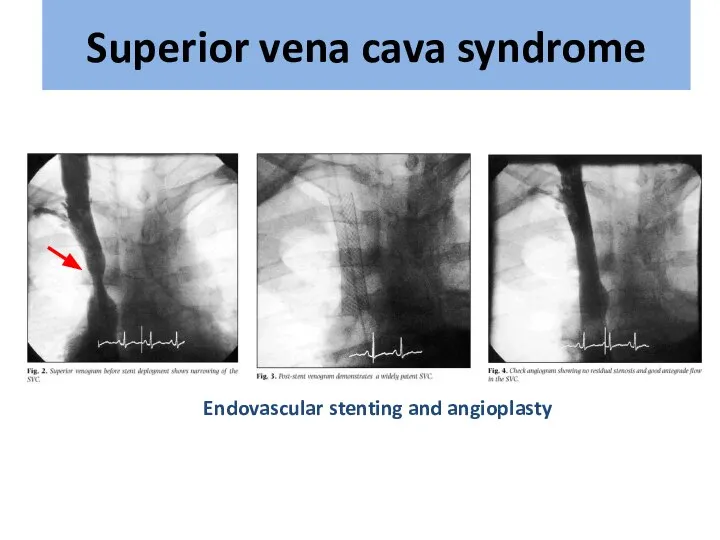
- 66. Endovascular stenting and angioplasty Superior vena cava syndrome
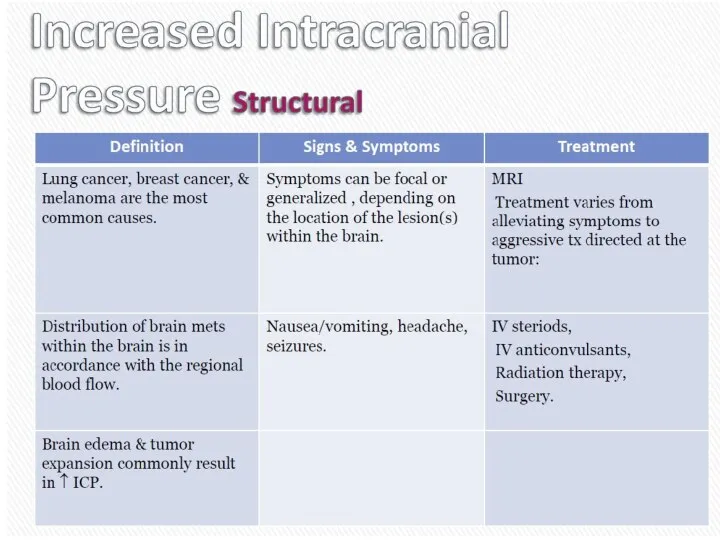
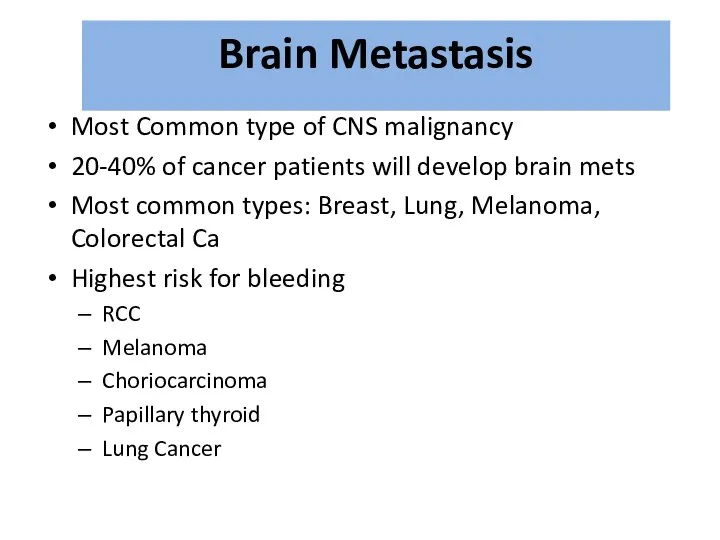
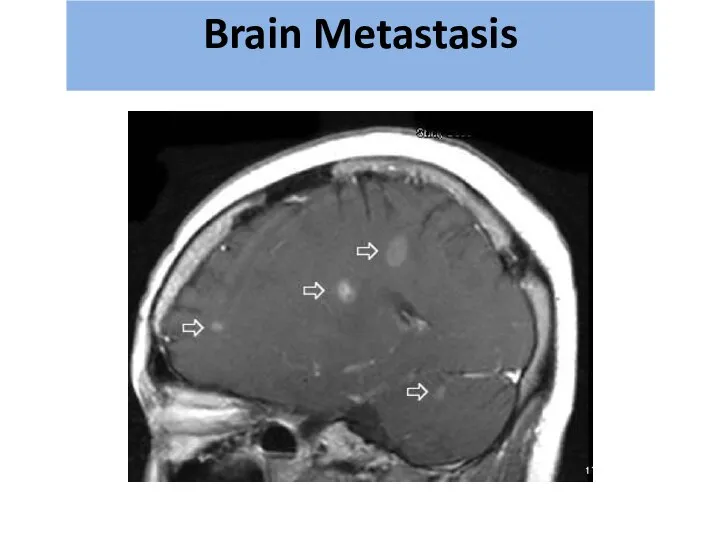
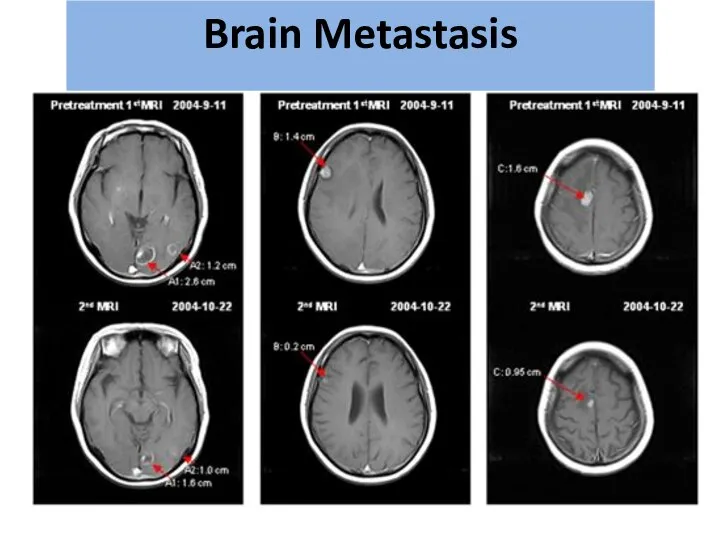
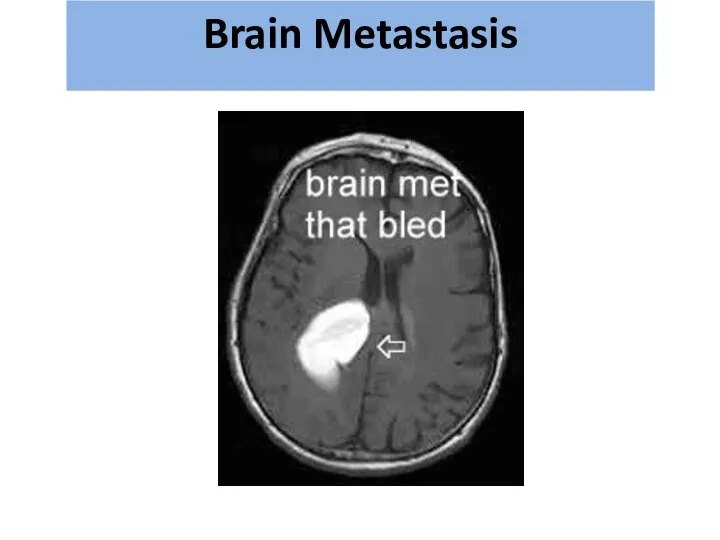
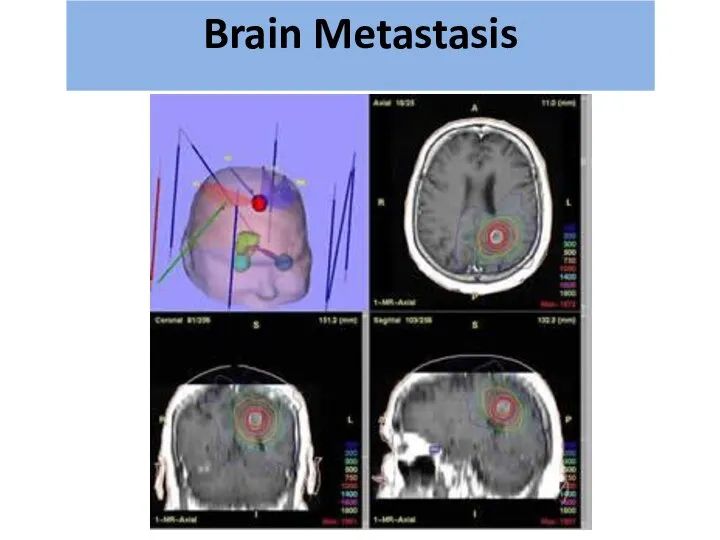
- 70. Most Common type of CNS malignancy 20-40% of cancer patients will develop brain mets Most common
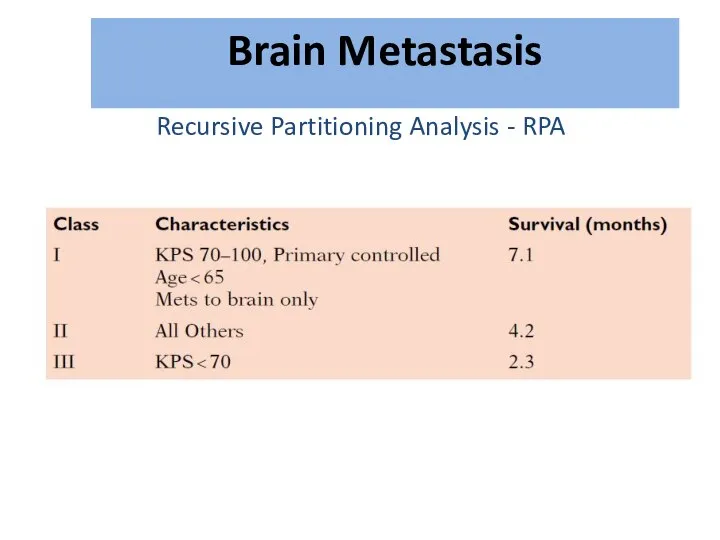
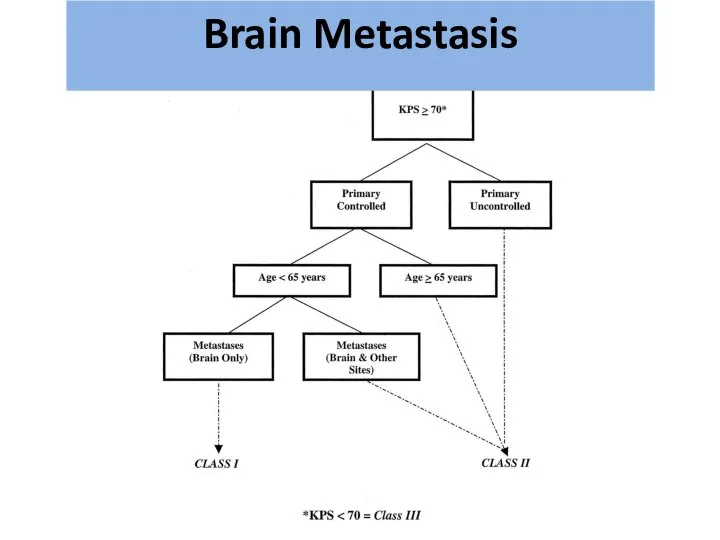
- 71. Recursive Partitioning Analysis - RPA גרורות מוחיות Brain Metastasis
- 72. גרורות מוחיות Brain Metastasis
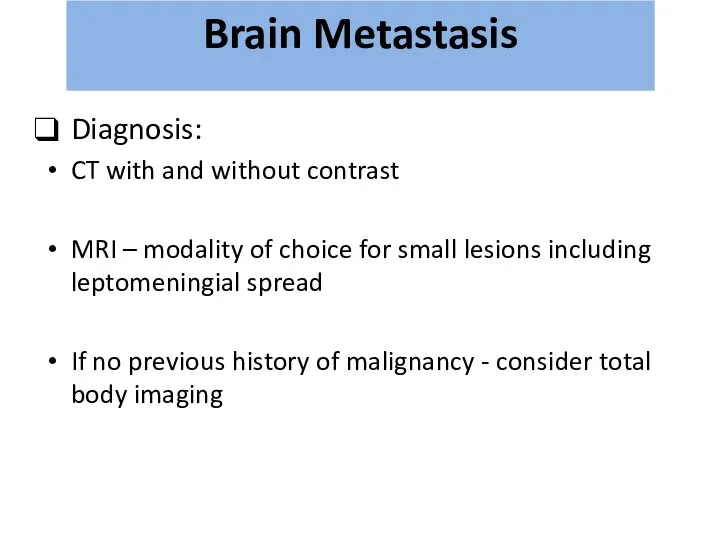
- 73. Diagnosis: CT with and without contrast MRI – modality of choice for small lesions including leptomeningial
- 74. גרורות מוחיות Brain Metastasis
- 75. גרורות מוחיות Brain Metastasis
- 76. גרורות מוחיות Brain Metastasis
- 77. Treatment: Steroids – Dexamethasone 16mg*2 Anticonvulsant Surgery? Radiation therapy גרורות מוחיות Brain Metastasis
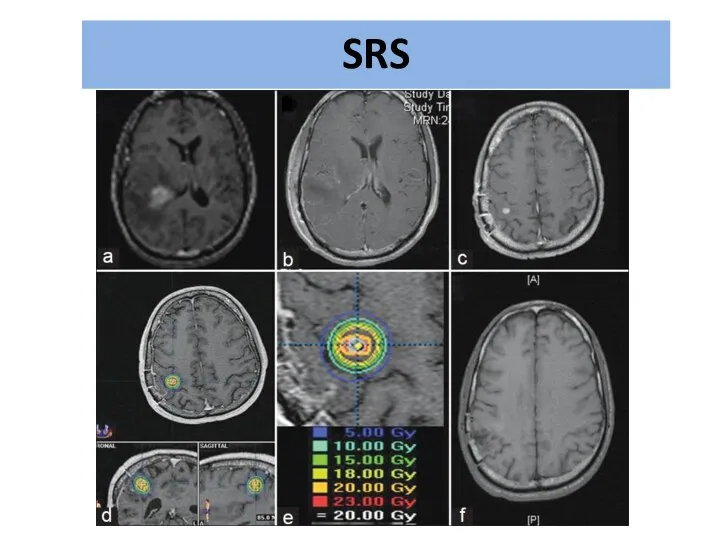
- 78. Radiation therapy WBRT=Whole Brain RT SRS=Stereotactic Radio Surgery גרורות מוחיות Brain Metastasis
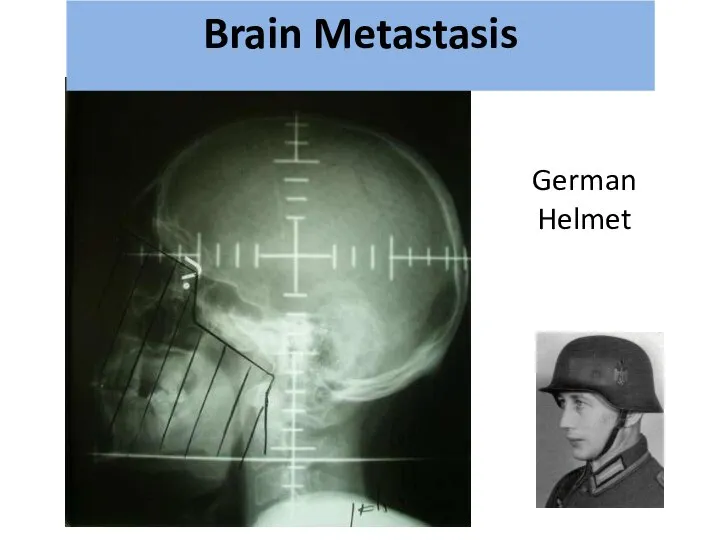
- 79. גרורות מוחיות German Helmet Brain Metastasis
- 80. גרורות מוחיות Brain Metastasis
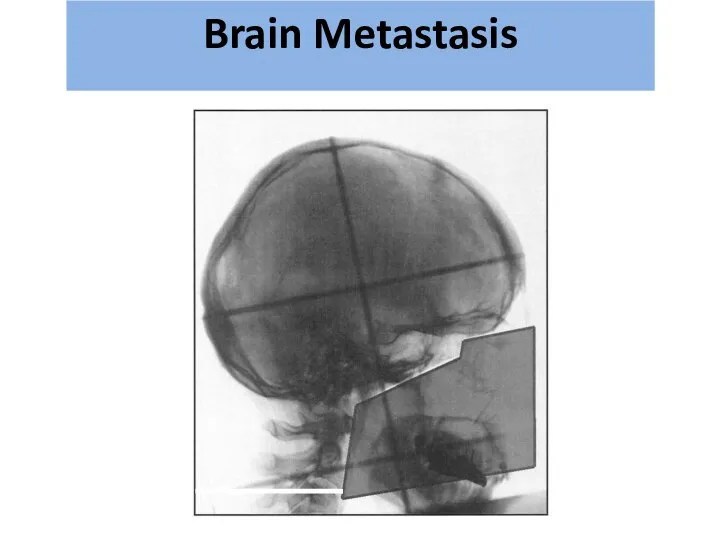
- 81. גרורות מוחיות Brain Metastasis
- 82. SRS
- 83. גרורות מוחיות Brain Metastasis
- 85. Скачать презентацию




 Христианская церковь в раннее Средневековья
Христианская церковь в раннее Средневековья Станок Нартова 1 часть
Станок Нартова 1 часть Машины для разметки покрытий, содержания обстановки, озеленения и благоустройства дорог
Машины для разметки покрытий, содержания обстановки, озеленения и благоустройства дорог Prezentatsiya_Metodi_v_filosofiyi_Talashov_Yegor_Volodimirovich
Prezentatsiya_Metodi_v_filosofiyi_Talashov_Yegor_Volodimirovich Инновационный подход к контрольно-оценочной деятельности в начальной школе. Портфолио
Инновационный подход к контрольно-оценочной деятельности в начальной школе. Портфолио 20170604_teatr_zadach
20170604_teatr_zadach Презентация Mой прадед Михайлов НГ
Презентация Mой прадед Михайлов НГ Три ступени, ведущие вниз
Три ступени, ведущие вниз Виды профилей. Прокатка. Прессование. Волочени
Виды профилей. Прокатка. Прессование. Волочени День самоуправления в школе
День самоуправления в школе Я здоровье сберегу, сам себе я помогу
Я здоровье сберегу, сам себе я помогу H480 Harvester Head Training Material
H480 Harvester Head Training Material Иконы, фрески, роспись церкви
Иконы, фрески, роспись церкви 20130304_35_ur_lit.5kl._obraz_rodiny_v_stihah_poetov_19v
20130304_35_ur_lit.5kl._obraz_rodiny_v_stihah_poetov_19v Работа над метроритмом размер 4/4
Работа над метроритмом размер 4/4 Досуговый центр
Досуговый центр Македония
Македония 0702А102_Тучкова М.Е
0702А102_Тучкова М.Е Оборудование отсеков и системы разгрузки танкера дедвейтом 3800т
Оборудование отсеков и системы разгрузки танкера дедвейтом 3800т Как читать молитву Отче наш
Как читать молитву Отче наш Подобие в жизни человека и немного юмора
Подобие в жизни человека и немного юмора Личная карточка инструктажа по безопасным методам работы, промсанитарии и противопожарной безопасности
Личная карточка инструктажа по безопасным методам работы, промсанитарии и противопожарной безопасности эрудит-викторина
эрудит-викторина Как зернышко на стол хлебом пришло
Как зернышко на стол хлебом пришло Моделирование
Моделирование ПромежуточнаяЗащита_2
ПромежуточнаяЗащита_2 Викторина. Где логика
Викторина. Где логика Система авто-полива сада
Система авто-полива сада