Содержание
- 2. DEFINITION Eclampsia is an acute and life-threatening complication of pregnancy, characterized by the appearance of tonic–clonic
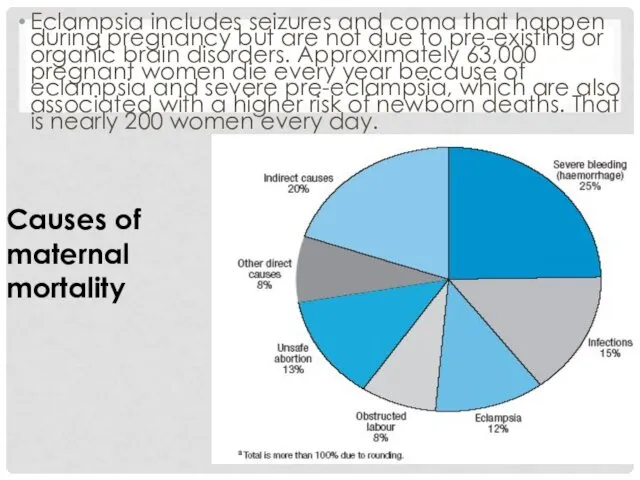
- 3. Eclampsia includes seizures and coma that happen during pregnancy but are not due to pre-existing or
- 4. SIGNS AND SYMPTOMS Typically patients show signs of pregnancy-induced hypertension and proteinuria before the onset of
- 5. In addition, with the advancement of the pathophysiological process, other organ symptoms may be present including
- 6. SEIZURES Chesley[2] distinguishes these four stages of an eclamptic event: 1. in the "stage of invasion"
- 7. 3. the next stage is the "stage of convulsion" when involuntary and forceful muscular movements occur,
- 8. In some rare cases there are no convulsions and the patient falls directly into a coma.
- 9. RISK FACTORS Eclampsia, like pre-eclampsia, tends to occur more commonly in first pregnancies and young mothers
- 10. Having a large placenta (multiple gestation, hydatidiform mole) also predisposes women to eclampsia. In addition, there
- 11. PATHOPHYSIOLOGY While multiple theories have been proposed to explain preeclampsia and eclampsia, it occurs only in
- 12. Placental hypoperfusion is linked to abnormal modelling of the fetal–maternal interface that may be immunologically mediated.
- 13. Eclampsia is seen as a form of hypertensive encephalopathy in the context of those pathological events
- 14. DIAGNOSIS Seizures during pregnancy that are unrelated to pre-eclampsia need to be distinguished from eclampsia. Such
- 15. PREVENTION Detection and management of pre-eclampsia is critical to reduce the risk of eclampsia. Appropriate management
- 16. CONVULSIONS Prevention of seizure convulsion is usually done using magnesium sulphate.[11] The idea to use Mg2+
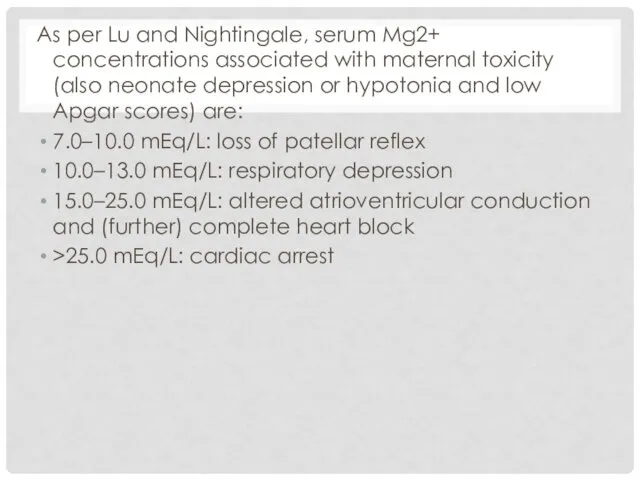
- 17. As per Lu and Nightingale, serum Mg2+ concentrations associated with maternal toxicity (also neonate depression or
- 18. Even with therapeutic serum Mg2+ concentrations, recurrent convulsions and seizures may occur—patients should receive additional MgSO4
- 19. TREATMENT The treatment of eclampsia requires prompt intervention and aims to prevent further convulsions, control the
- 20. DELIVERY If the baby has not yet been delivered, steps need to be taken to stabilize
- 21. Management(carried out by a team) 1.Turn the patient on her side 2.Ensure clear airway(suction,mouth gag) 3.Maintain
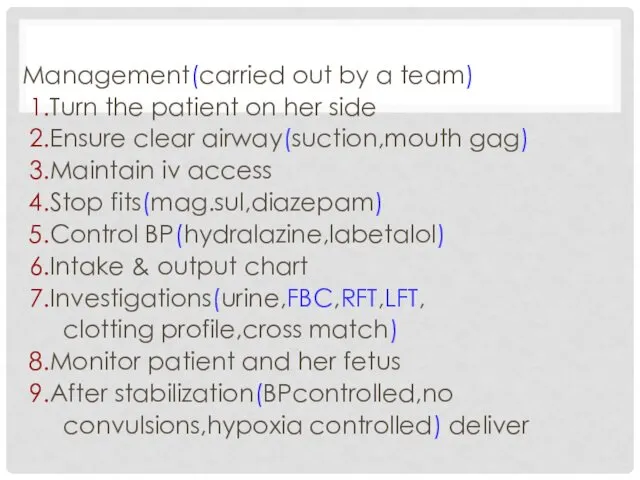
- 23. Скачать презентацию
![SEIZURES Chesley[2] distinguishes these four stages of an eclamptic event: 1.](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/462163/slide-5.jpg)


![CONVULSIONS Prevention of seizure convulsion is usually done using magnesium sulphate.[11]](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/462163/slide-15.jpg)
 Роль диких животных в развитии эпизоотии рабической инфекции
Роль диких животных в развитии эпизоотии рабической инфекции Безинтерфероновая терапия гепатита С
Безинтерфероновая терапия гепатита С Шаттыққа толы жүрекпен
Шаттыққа толы жүрекпен Індивідуальні зміни. Лекція 2
Індивідуальні зміни. Лекція 2 Паспортизация канцерогеноопасных производств в Воронежской области
Паспортизация канцерогеноопасных производств в Воронежской области Этапы обработки инструментария. Предстерилизационная очистка и стерилизация. Упаковка, контроль, качество стерилизации
Этапы обработки инструментария. Предстерилизационная очистка и стерилизация. Упаковка, контроль, качество стерилизации Неврологиядағы науқастарды қайта қалпына келтіру негіздері
Неврологиядағы науқастарды қайта қалпына келтіру негіздері Эмпирическое исследование познавательных процессов. Общепсихологический практикум часть 2
Эмпирическое исследование познавательных процессов. Общепсихологический практикум часть 2 Теория и метод поэтапного формирования умственных действий П.Я. Гальперина
Теория и метод поэтапного формирования умственных действий П.Я. Гальперина Строение, соединения скелета верхней конечности
Строение, соединения скелета верхней конечности Предпатологические состояния и заболевания при нерациональных занятиях физической культурой и спортом
Предпатологические состояния и заболевания при нерациональных занятиях физической культурой и спортом Гормоны в лечении гинекологических заболеваний
Гормоны в лечении гинекологических заболеваний Назначение брекет-системы
Назначение брекет-системы История сестринского дела
История сестринского дела Тістердің тіс жегі емес зақымдануларының рентгендік диагностикасы (флюороздың жаралы түрі, тістің қатты тінінің гипоплазиясы)
Тістердің тіс жегі емес зақымдануларының рентгендік диагностикасы (флюороздың жаралы түрі, тістің қатты тінінің гипоплазиясы) Флоатинг. Что такое флоатинг?
Флоатинг. Что такое флоатинг? Стоматологическая помощь, её виды
Стоматологическая помощь, её виды Гельминтоздар. Этиологиясы
Гельминтоздар. Этиологиясы Коллоиды (альбумин, ГЭК) и гипертонический раствор NaCl
Коллоиды (альбумин, ГЭК) и гипертонический раствор NaCl Оздоровительные услуги в структуре гостиничного сервиса. (Лекция 1)
Оздоровительные услуги в структуре гостиничного сервиса. (Лекция 1) Внутренняя среда организма. Кровь
Внутренняя среда организма. Кровь Психологическое консультирование
Психологическое консультирование Online education in COVID19
Online education in COVID19 Биохимия почек и мочи
Биохимия почек и мочи Первая помощь при ожогах и обморожениях. Тема 11
Первая помощь при ожогах и обморожениях. Тема 11 Клиническая фармакология глюкокортикостероидов
Клиническая фармакология глюкокортикостероидов Окклюзия
Окклюзия Крипторхизм. Этиология
Крипторхизм. Этиология