Содержание
- 2. CHEST PAIN 5% of all ED visits per year Differential diagnosis is difficult
- 3. CHEST PAIN ANATOMY DIFFERENTIAL DIAGNOSIS BRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAIN APPROACH TO CHEST
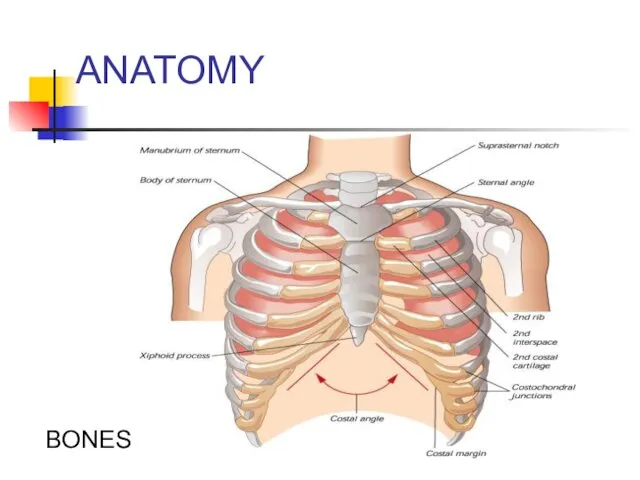
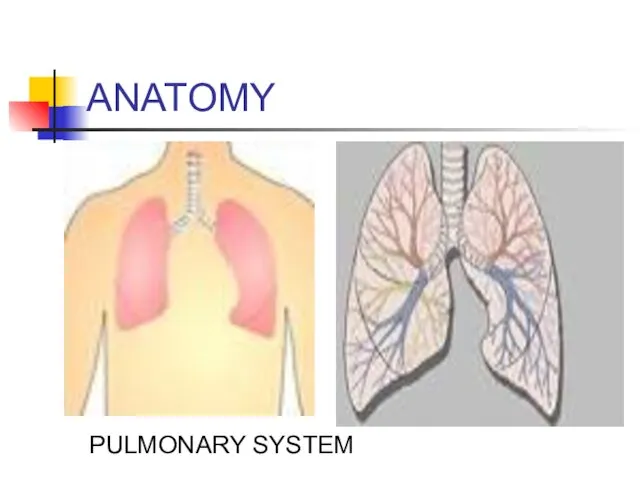
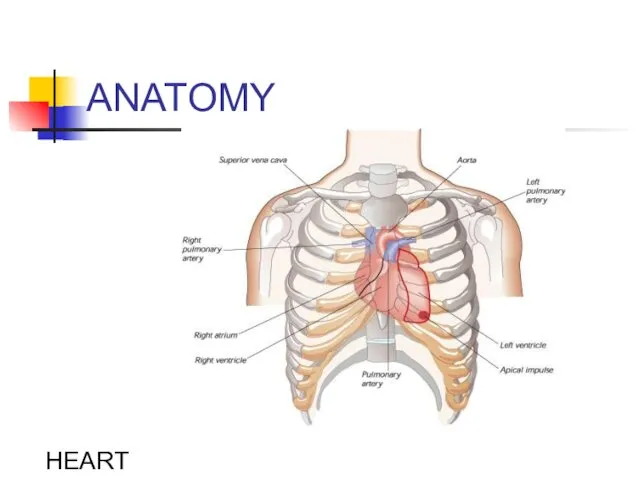
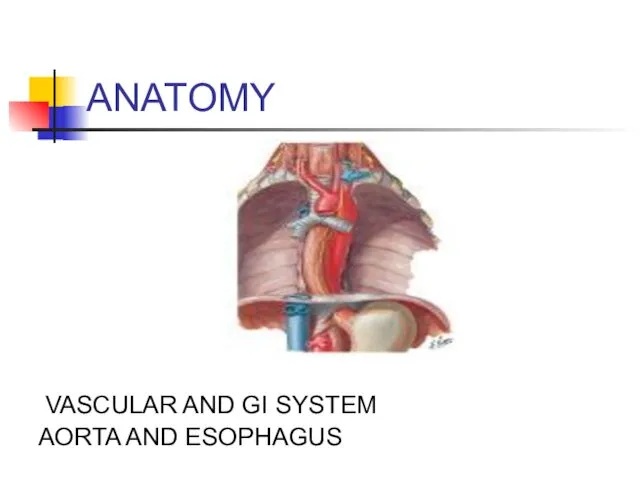
- 4. ANATOMY In devising a differential diagnosis for chest pain, it becomes essential to review the anatomy
- 5. ANATOMY SKIN MUSCLES
- 6. ANATOMY BONES
- 7. ANATOMY PULMONARY SYSTEM
- 8. ANATOMY HEART
- 9. ANATOMY VASCULAR AND GI SYSTEM AORTA AND ESOPHAGUS
- 10. DIFFERENTIAL DIAGNOSIS OF CHEST PAIN CHEST WALL PAIN PULMONARY CAUSES CARDIAC CAUSES VASCULAR CAUSES GI CAUSES
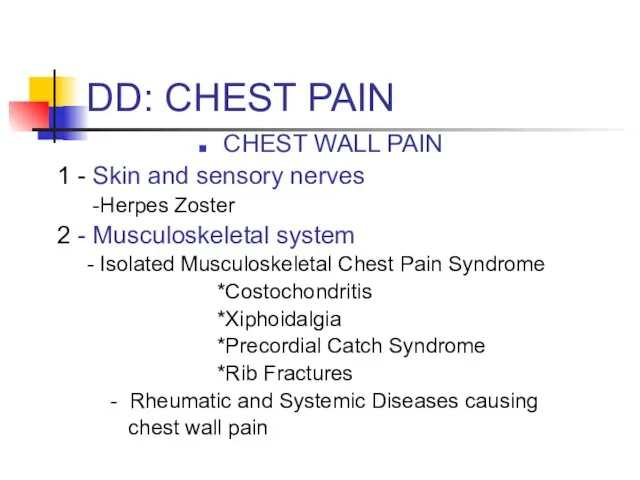
- 11. DD: CHEST PAIN CHEST WALL PAIN 1 - Skin and sensory nerves -Herpes Zoster 2 -
- 12. DD: CHEST PAIN PULMONARY CAUSES 1 - Pulmonary Embolism 2 – Pneumonia 3 - Pneumothorax/ Tension
- 13. DD: CHEST PAIN CARDIAC CAUSES - Coronary Heart Disease *Myocardial Ischemia *Unstable Angina *Angina - Valvular
- 14. DD: CHEST PAIN Vascular Causes: -Aortic Dissection
- 15. DD: CHEST PAIN GI CAUSES -ESOPHAGEAL *Reflux * Esophagitis * Rupture (Boerhaave Syndrome) * Spasm/Motility Disorder/Foreign
- 16. DD: CHEST PAIN PSYCHIATRIC - PANIC DISORDER - ANXIETY - DEPRESSION - SOMATOFORM DISORDERS
- 17. CHEST PAIN BRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAIN
- 18. CHEST WALL PAIN .
- 19. CHEST WALL PAIN HERPES ZOSTER -Reactivation of Herpes Varicellae - Immunocompromised patients often at risk for
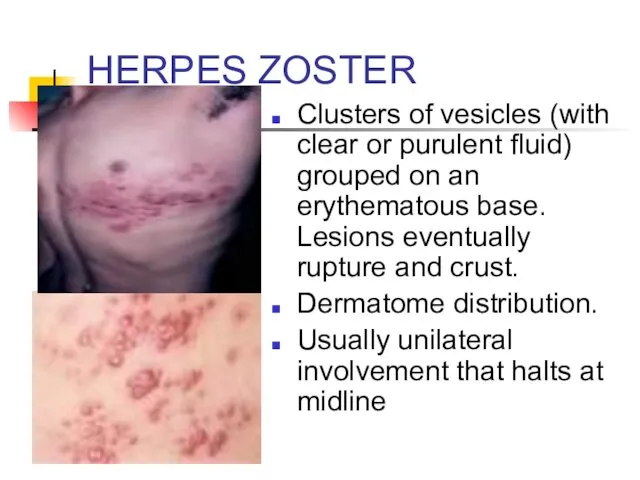
- 20. HERPES ZOSTER Clusters of vesicles (with clear or purulent fluid) grouped on an erythematous base. Lesions
- 21. HERPES ZOSTER TREATMENT: * Antivirals: reduce duration of symptoms; incidence of postherpatic neuralgia. * +/- corticosteroids:
- 22. CHEST WALL PAIN Musculoskeletal Pain - Usually localized, acute, positional; - Pain often reproducible by palpation,
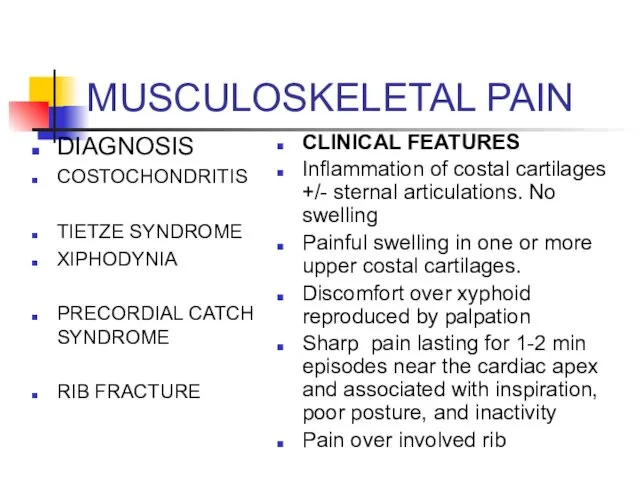
- 23. MUSCULOSKELETAL PAIN DIAGNOSIS COSTOCHONDRITIS TIETZE SYNDROME XIPHODYNIA PRECORDIAL CATCH SYNDROME RIB FRACTURE CLINICAL FEATURES Inflammation of
- 24. MUSCULOSKELETAL PAIN Treatment: Analgesia (NSAIDs)
- 25. PULMONARY CAUSES OF CHEST PAIN .
- 26. PULMONARY EMBOLISM RISK FACTORS: VIRCHOW’S TRIAD - Hypercoagulability *Malignancy *Pregnancy, Early Postpartum, OCPs, HRT *Genetic Mutations:
- 27. PULMONARY EMBOLISM (PE) CLINICAL FEATURES - Shortness of breath - Chest pain: often pleuritic - Tachycardia,
- 28. PE: DIAGNOSTIC TESTS ECG: -Sinus tachycardia most common - Often see nonspecific abnormalities - Look for
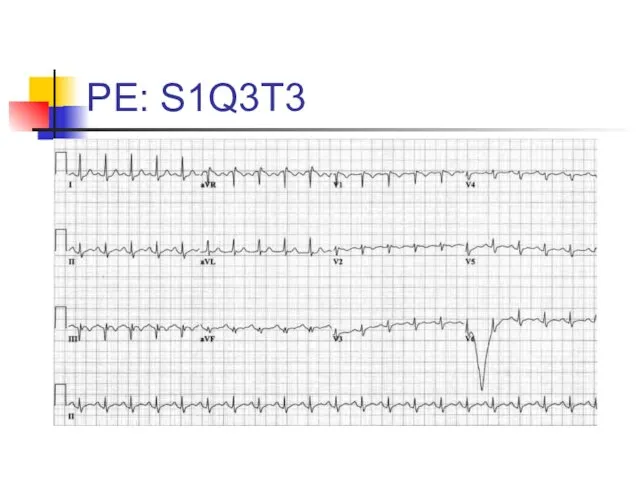
- 29. PE: S1Q3T3
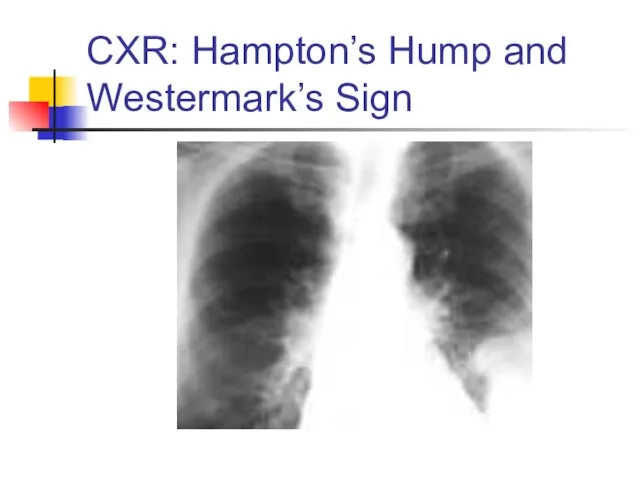
- 30. PE: DIAGNOSTIC TESTS CHEST X-RAY - Normal in 25% of cases - Often nonspecific findings -
- 31. CXR: Hampton’s Hump and Westermark’s Sign
- 32. PE: DIAGNOSTIC TESTS ABG: *Look for abnormal PaO2 or A-a gradient D-Dimer: *Often elevated in PE.
- 34. PE: DIAGNOSTIC TESTS VQ SCAN (Ventilation-Perfusion scan)- use in setting of renal insufficiency Helical CT scan
- 35. PE: TREATMENT Initiate Heparin * Unfractionated Heparin: 80 Units/Kg bolus IV, then 18units/kg/hr * Fractionated Heparin
- 36. PNEUMONIA CLINICAL FEATURES - Cough +/- sputum production - Fevers/chills - Pleuritic chest pain - Shortness
- 37. PNEUMONIA: DIAGNOSIS X-Ray If patient is to be hospitalized: Consider GBC (to look for leukocytosis) Consider
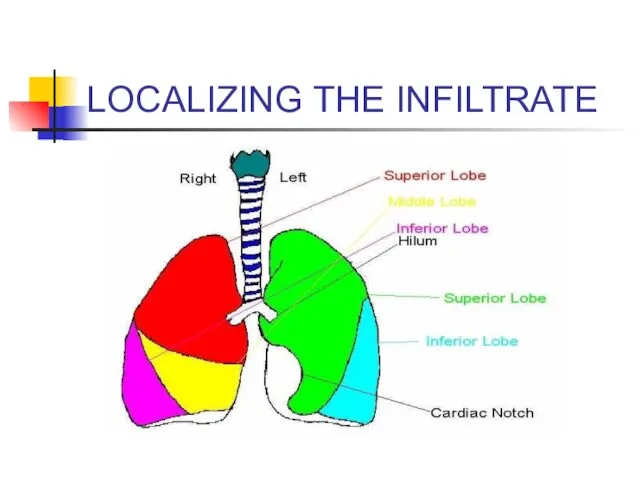
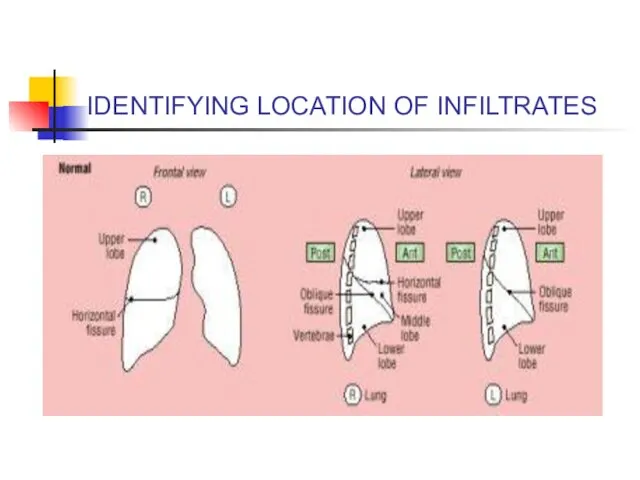
- 38. LOCALIZING THE INFILTRATE
- 39. IDENTIFYING LOCATION OF INFILTRATES
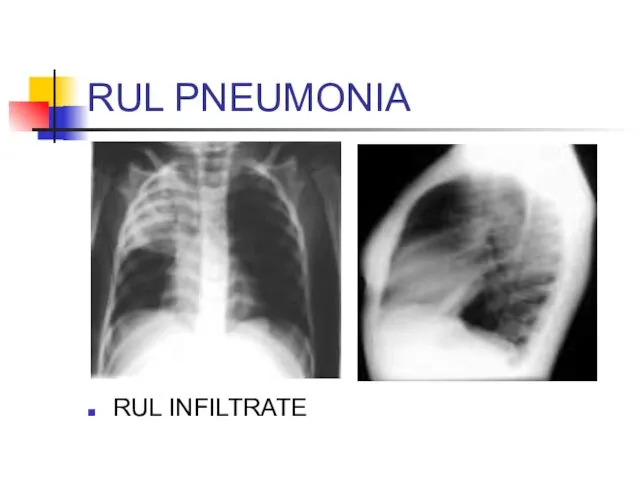
- 40. RUL PNEUMONIA RUL INFILTRATE
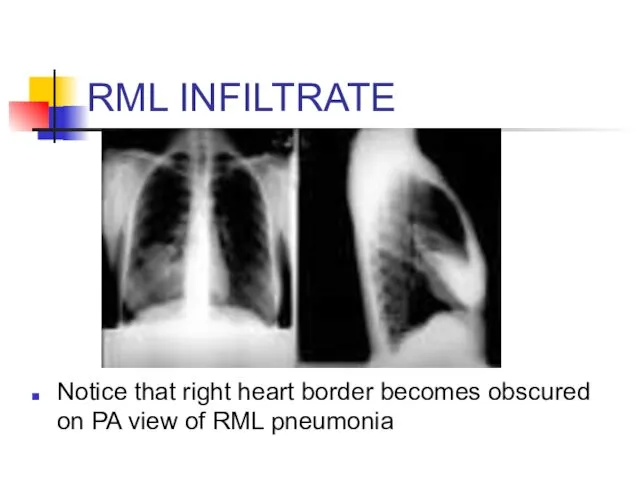
- 41. RML INFILTRATE Notice that right heart border becomes obscured on PA view of RML pneumonia
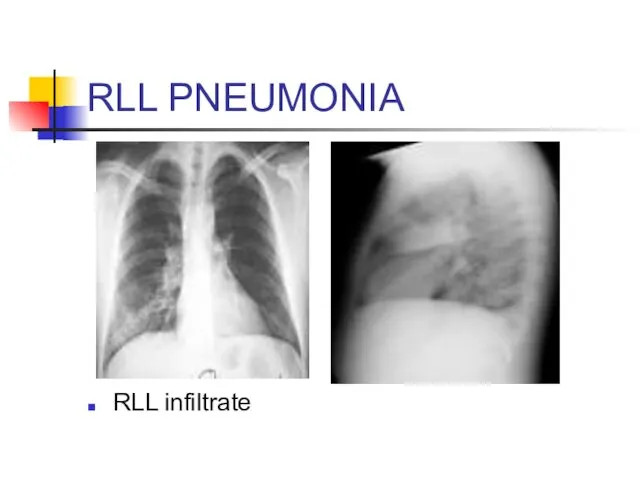
- 42. RLL PNEUMONIA RLL infiltrate
- 43. PNEUMONIA: TREATMENT Community- Acquired: - OUT-PATIENT *Doxycycline: Low cost option * Macrolide *Newer fluoroquinolone: Moxifloxacin, Levofloxacin,
- 44. SPONTANEOUS PNEUMOTHORAX RISK FACTORS: - Primary * No underlying lung disease * Young male with greater
- 45. PNEUMOTHORAX CLINICAL FEATURES - Acute pleuritic chest pain: 95% - Usually pain localized to side of
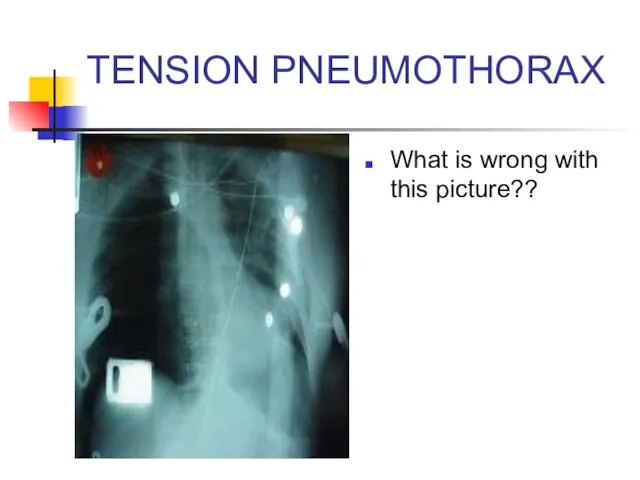
- 46. TENSION PNEUMOTHORAX What is wrong with this picture??
- 47. TENSION PNEUMOTHORAX Answer: Chest X-ray should have never been obtained Tension PTX is a clinical diagnosis
- 48. Tension Pneumothorax Trachea deviates to contralateral side Mediastinum shifts to contralateral side Decreased breath sounds and
- 49. NEEDLE DECOMPRESSION Insert large bore needle (14 or 16 Gauge) with catheter in the 2nd intercostal
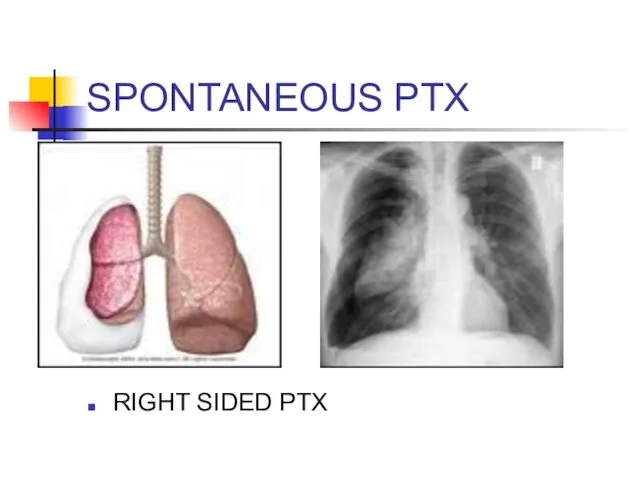
- 50. SPONTANEOUS PTX RIGHT SIDED PTX
- 51. SPONTANEOUS PTX TREATMENT: - If small ( - Give oxygen: Increases pleural air absorption - If
- 52. PLEURITIS/SEROSITIS Inflammation of pleura that covers lung Pleuritic chest pain Causes: - Viral etiology - SLE
- 53. COPD/ASTHMA EXACERBATIONS CLINICAL FEATURES: - Decrease in O2 saturations - Shortness of Breath - May see
- 54. COPD EXACERBATION: TREATMENT Oxygen: Must prevent hypoxemia. Watch for hypercapnia with O2 therapy B2 agonist (albuterol)
- 55. ASTHMA TREATMENT Oxygen Inhaled short acting B2 agonists: Albuterol Anticholinergics: Atrovent Corticosteroids Magnesium Systemic B2 agonists:
- 56. CARDIAC CAUSES OF CHEST PAIN .
- 57. RISK FACTORS FOR CAD Age Diabetes Hypertension Family History Tobacco Use Hypercholesterolemia Cocaine use
- 58. ISCHEMIC CHEST PAIN EXERTIONAL ANGINA * BRIEF EPISODES BROUGHT ON BY EXERTION AND RELIEVED BY REST
- 59. Angina pectoris Stable angina pectoris is a clinical syndrome characterized by precordial or anterior chest discomfort,
- 60. Angina pectoris The chest discomfort may be described by the patient either as a true pain
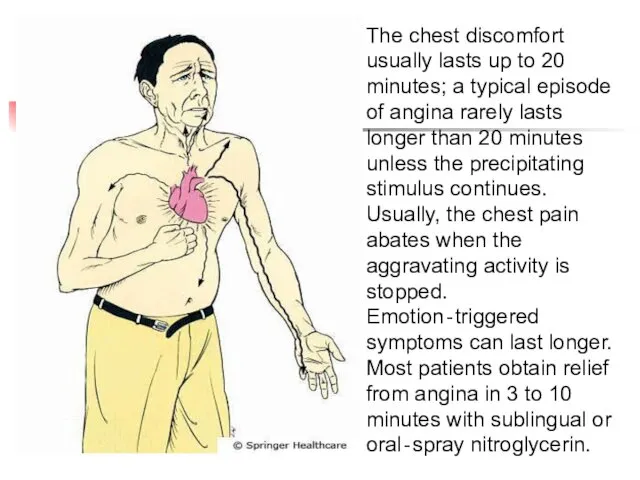
- 61. The chest discomfort usually lasts up to 20 minutes; a typical episode of angina rarely lasts
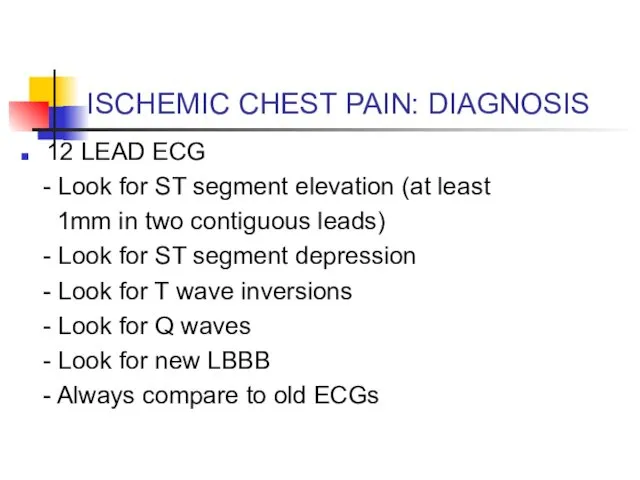
- 62. ISCHEMIC CHEST PAIN: DIAGNOSIS 12 LEAD EСG - Look for ST segment elevation (at least 1mm
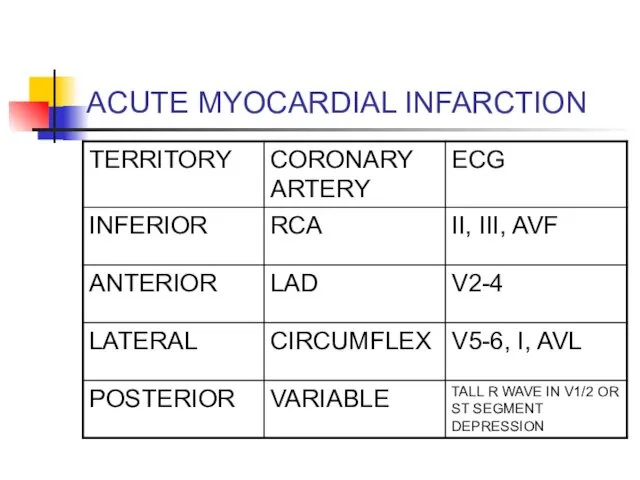
- 63. ACUTE MYOCARDIAL INFARCTION
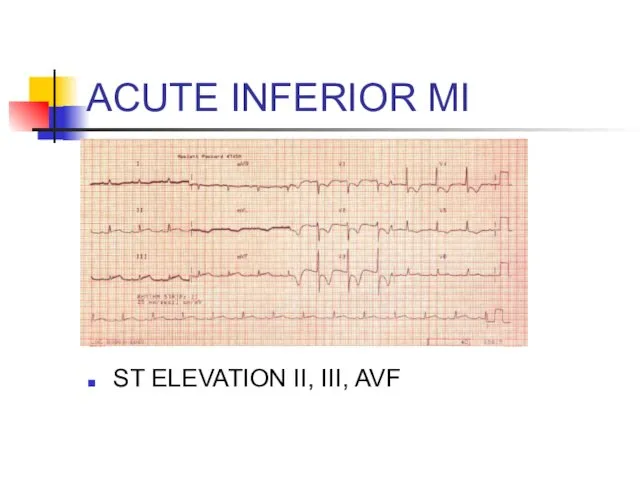
- 64. ACUTE INFERIOR MI ST ELEVATION II, III, AVF
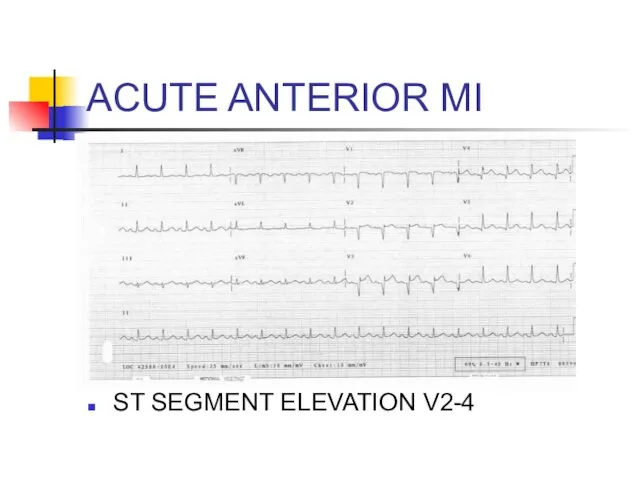
- 65. ACUTE ANTERIOR MI ST SEGMENT ELEVATION V2-4
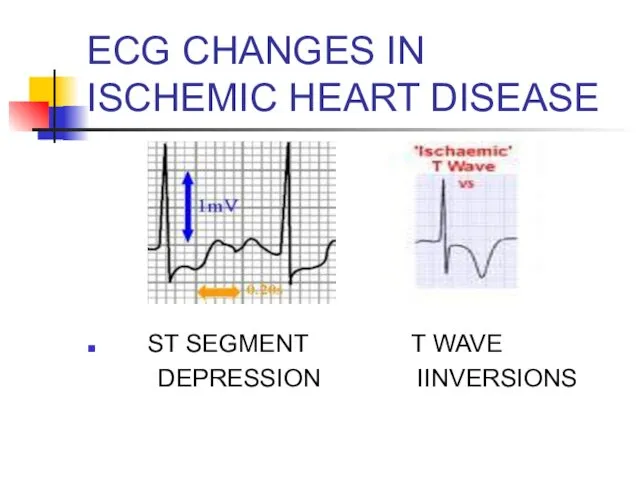
- 66. EСG CHANGES IN ISCHEMIC HEART DISEASE ST SEGMENT T WAVE DEPRESSION IINVERSIONS
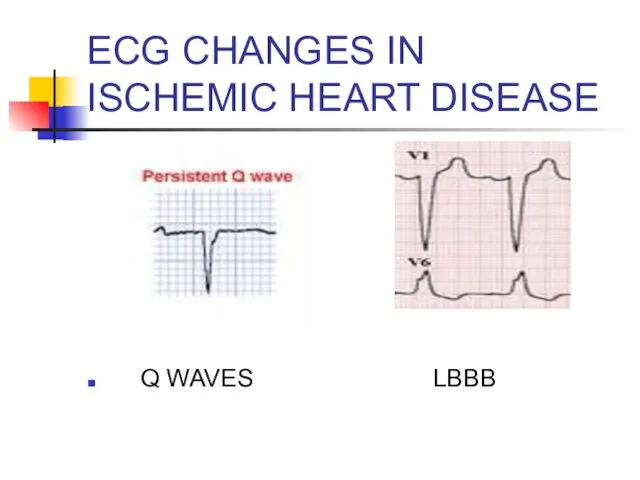
- 67. EСG CHANGES IN ISCHEMIC HEART DISEASE Q WAVES LBBB
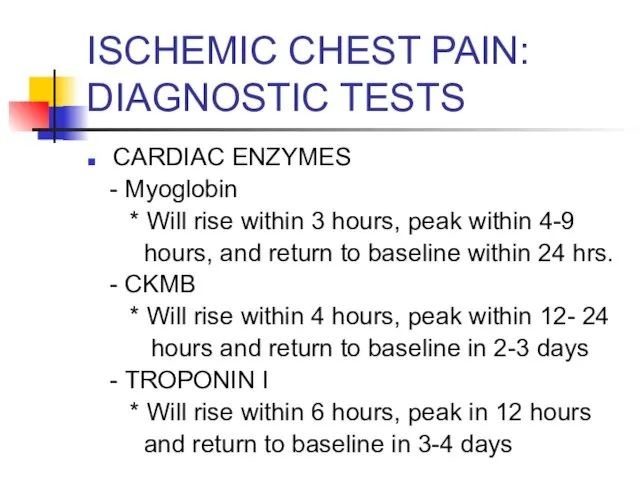
- 68. ISCHEMIC CHEST PAIN: DIAGNOSTIC TESTS CARDIAC ENZYMES - Myoglobin * Will rise within 3 hours, peak
- 69. ISCHEMIC HEART DISEASE TREATMENT: ACUTE ST SEGMENT ELEVATION MI - OXYGEN - ASPIRIN (4 BABY ASPIRIN)
- 70. ISCHEMIC HEART DISEASE TREATMENT: NONSTEMI AND UNSTABLE ANGINA - OXYGEN - ASPIRIN (4 BABY ASPIRIN) -
- 71. LOW RISK CARDIAC CHEST PAIN If low risk chest pain, can consider serial EСGs and enzymes.
- 72. VALVULAR HEART DISEASE AORTIC STENOSIS *Classic triad: dyspnea, chest pain, and syncope * Harsh systolic ejection
- 73. ACUTE PERICARDITIS CLINICAL FEATURES - Acute, stabbing chest pain - Pleuritic chest pain - Pain often
- 74. ACUTE PERICARDITIS COMMON CAUSES * IDIOPATHIC * INFECTIOUS * MALIGNANCY * UREMIA * RADIATION INDUCED *
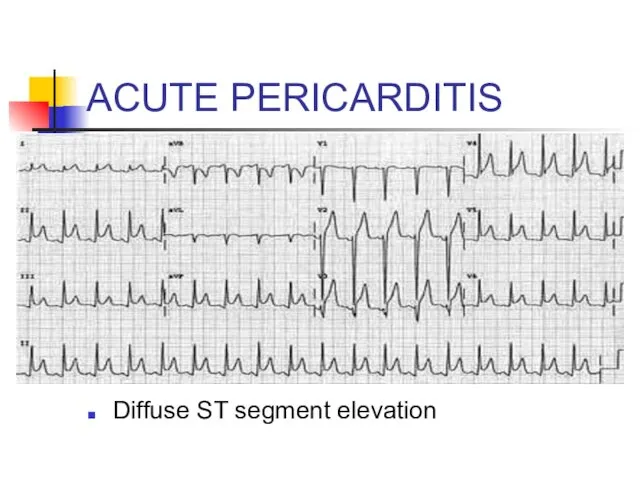
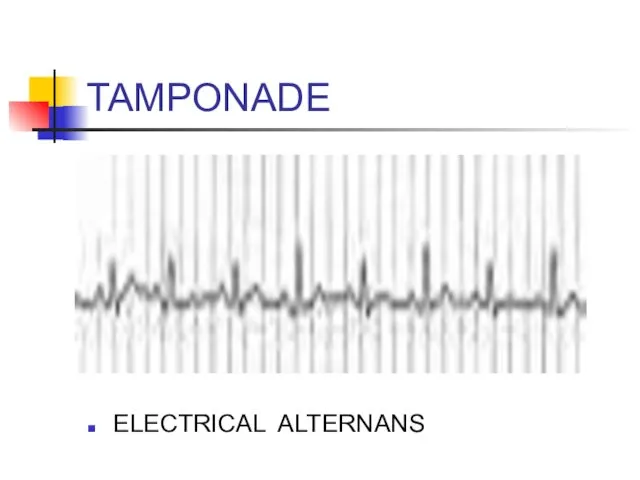
- 75. ACUTE PERICARDITIS: DIAGNOSTIC TESTS ECG *Look for diffuse ST segment elevation and PR depression. * If
- 76. ACUTE PERICARDITIS Diffuse ST segment elevation
- 77. TAMPONADE ELECTRICAL ALTERNANS
- 78. ACUTE PERICARDITIS TREATMENT: - If idiopathic or viral: NSAIDs - Otherwise treat underlying pathology
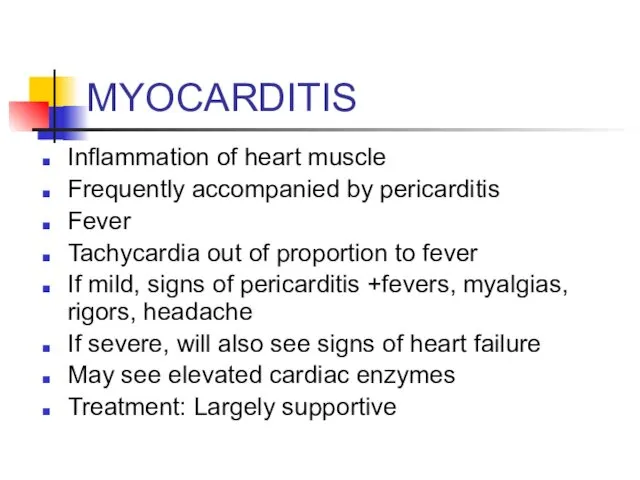
- 79. MYOCARDITIS Inflammation of heart muscle Frequently accompanied by pericarditis Fever Tachycardia out of proportion to fever
- 80. VASCULAR CAUSES OF CHEST PAIN .
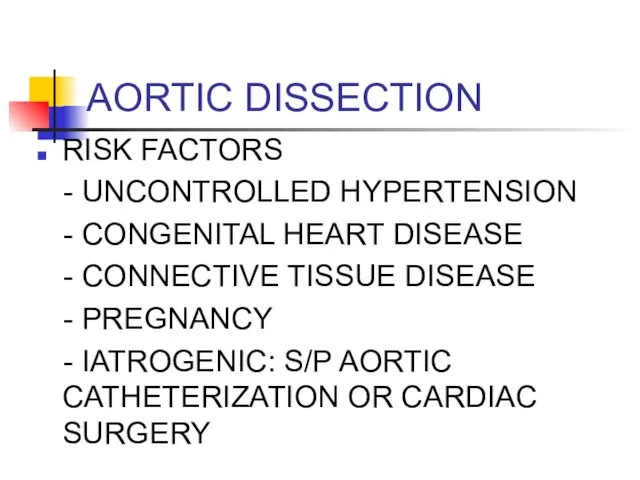
- 81. AORTIC DISSECTION RISK FACTORS - UNCONTROLLED HYPERTENSION - CONGENITAL HEART DISEASE - CONNECTIVE TISSUE DISEASE -
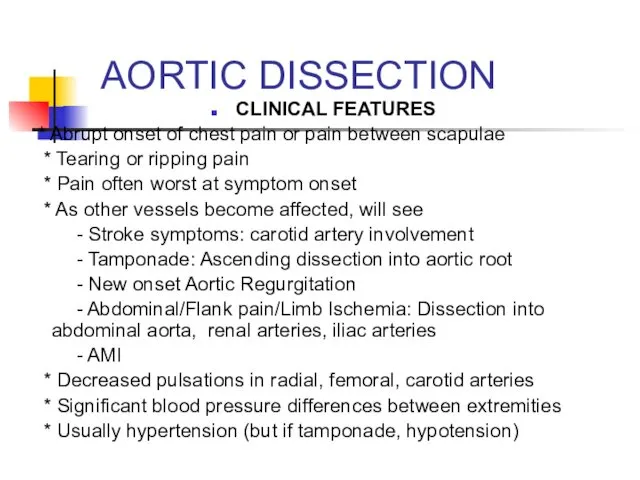
- 82. AORTIC DISSECTION CLINICAL FEATURES * Abrupt onset of chest pain or pain between scapulae * Tearing
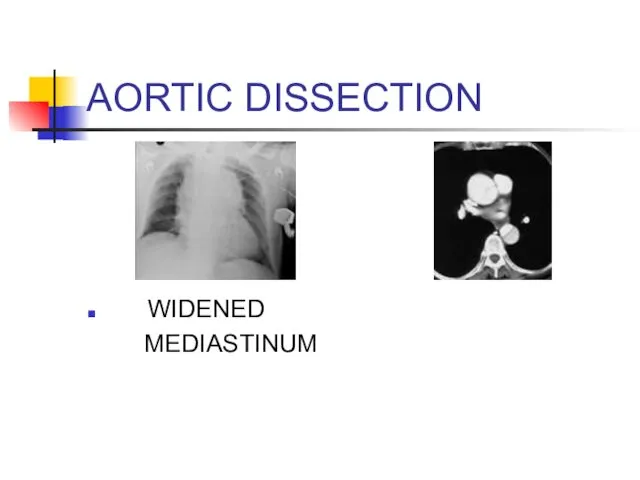
- 83. DIAGNOSIS: AORTIC DISSECTION CXR: Look for widened mediastinum CT SCAN: ANGIOGRAPHY TEE ** suspected dissectons must
- 84. AORTIC DISSECTION WIDENED MEDIASTINUM
- 85. AORTIC DISSECTION TREATMENT: - ANTIHYPERTENSIVE THERAPY *Start with beta blockers (smell, labetalol) * Can add vasodilators
- 86. GI CAUSES OF CHEST PAIN .
- 87. ESOPHAGEAL CAUSES REFLUX ESOPHAGITIS ESOPHAGEAL PERFORATION SPASM/MOTILITY DISORDER/
- 88. GERD RISK FACTORS * High food fat * Caffeine * Nicotine, alcohol * Medicines: CCB, nitrates,
- 89. GERD CLINICAL FEATURES * Burning pain * Association with sour taste in mouth, nausea/vomiting * May
- 90. ESOPHAGITIS CLINICAL FEATURES *Chest pain +Odynophagia (pain with swallowing) Causes *Inflammatory process: GERD or med related
- 91. ESOPHAGEAL PERFORATION CAUSES *Iatrogenic: Endoscopy * Boerhaave Syndrome: Spontaneous rupture secondary to increased intraesophageal pressure. -
- 92. ESOPHAGEAL PERFORATION CLINICAL FEATURES *Acute persistent chest pain that may radiate to back, shoulders, neck *
- 93. ESOPHAGEAL PERFORATION DIAGNOSIS *x-Ray: May see pleural effusion (usually on left). Also may see subQ emphysema,
- 94. ESOPHAGEAL MOTILITY DISORDERS CLINICAL FEATURES: * Chest pain often induced by ingestion of liquids at extremes
- 95. OTHER GI CAUSES In appropriate setting, consider PUD, Biliary Disease, and Pancreatitis in differential of chest
- 96. PSYCHOLOGIC CAUSES Diagnosis of exclusion
- 97. APPROACH TO THE PATIENT WITH CHEST PAIN PUTTING IT ALL TOGETHER
- 98. INITIAL APPROACH Like everything else: ABCs A: Airway B: Breathing C: Circulation IV, O2, cardiac monitor
- 99. CHEST PAIN: HISTORY Time and character of onset Quality Location Radiation Associated symptoms Aggravating symptoms Alleviating
- 100. CHEST PAIN: HISTORY TIME AND CHARACTER OF ONSET: * Abrupt onset with greatest intensity at start:
- 101. CHEST PAIN: HISTORY Quality: *Pleuritic Pain: PE, Pleurisy, Pneumonia, Pericarditis, PTX *Esophageal: Burning, etc *MI: squeezing,
- 102. CHEST PAIN: HISTORY RADIATION: * To neck, jaw, down either arm: consider Ischemia ASSOCIATED SYMPTOMS: *
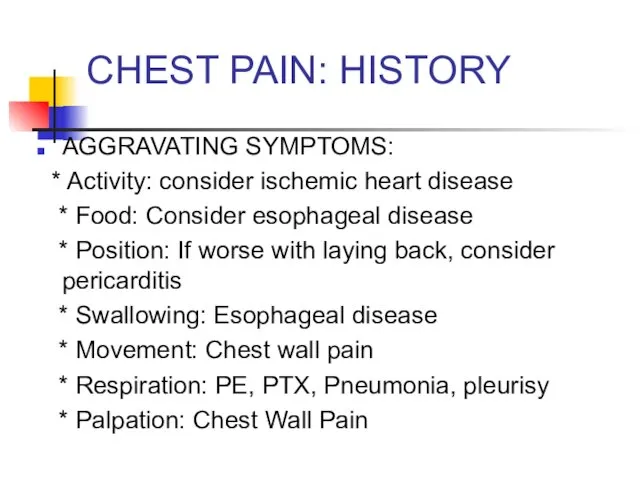
- 103. CHEST PAIN: HISTORY AGGRAVATING SYMPTOMS: * Activity: consider ischemic heart disease * Food: Consider esophageal disease
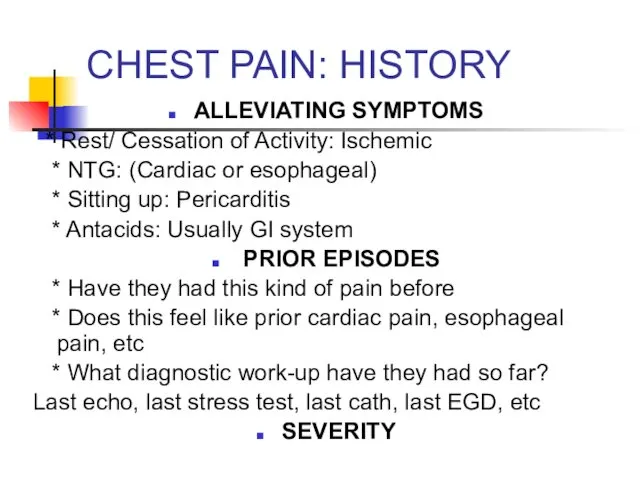
- 104. CHEST PAIN: HISTORY ALLEVIATING SYMPTOMS * Rest/ Cessation of Activity: Ischemic * NTG: (Cardiac or esophageal)
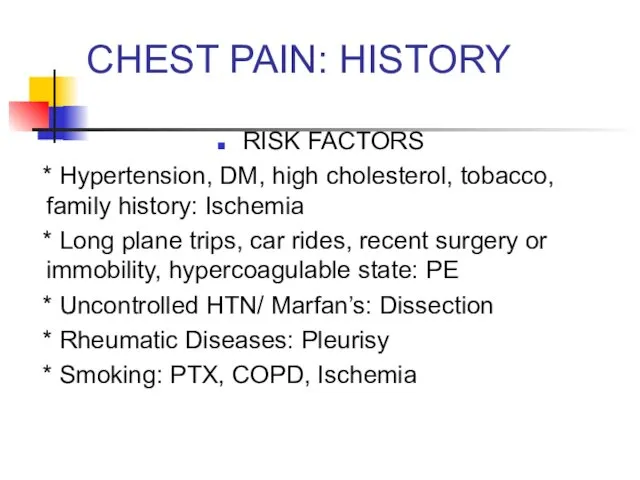
- 105. CHEST PAIN: HISTORY RISK FACTORS * Hypertension, DM, high cholesterol, tobacco, family history: Ischemia * Long
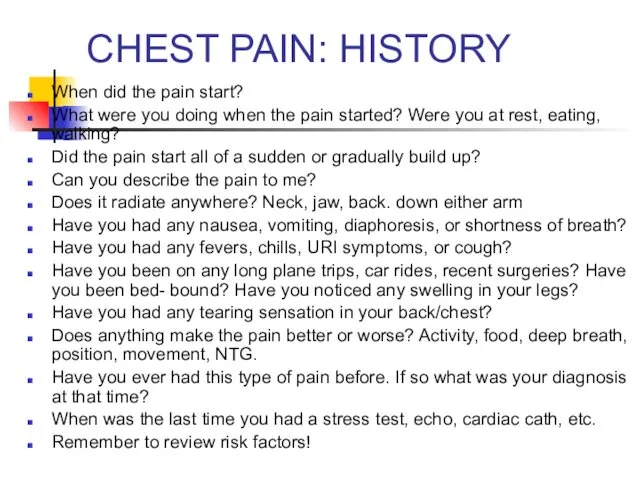
- 106. CHEST PAIN: HISTORY When did the pain start? What were you doing when the pain started?
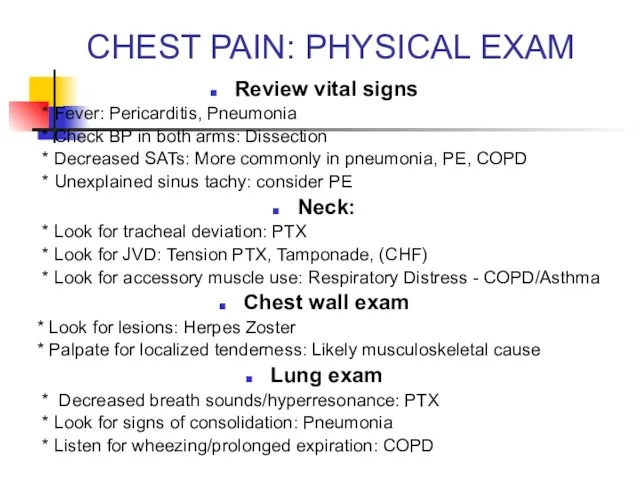
- 107. CHEST PAIN: PHYSICAL EXAM Review vital signs * Fever: Pericarditis, Pneumonia * Check BP in both
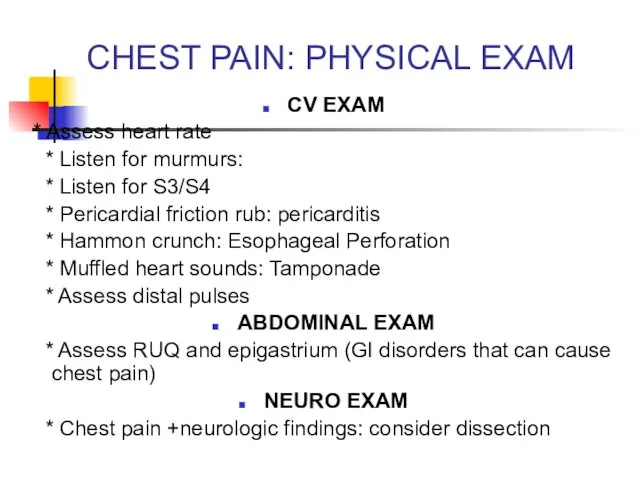
- 108. CHEST PAIN: PHYSICAL EXAM CV EXAM * Assess heart rate * Listen for murmurs: * Listen
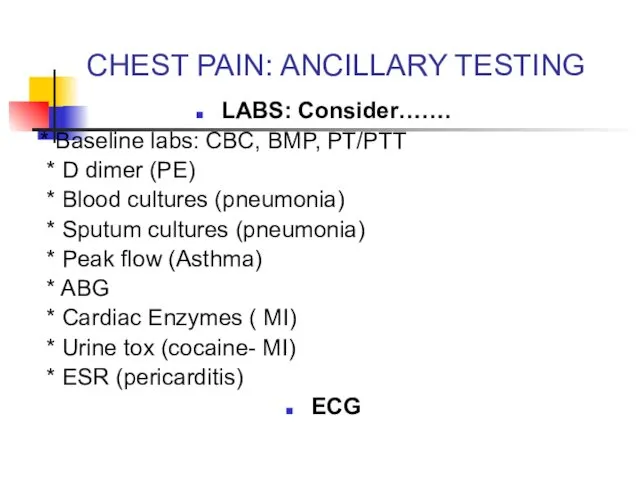
- 109. CHEST PAIN: ANCILLARY TESTING LABS: Consider……. * Baseline labs: CBC, BMP, PT/PTT * D dimer (PE)
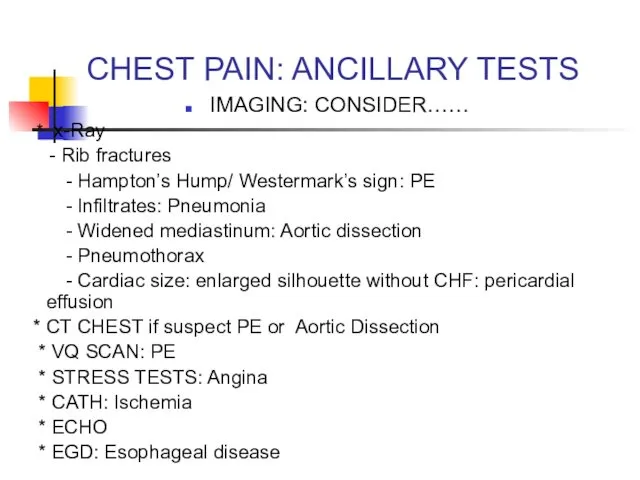
- 110. CHEST PAIN: ANCILLARY TESTS IMAGING: CONSIDER…… * x-Ray - Rib fractures - Hampton’s Hump/ Westermark’s sign:
- 112. Скачать презентацию

 Лекарственные растения Кузбасса
Лекарственные растения Кузбасса Дифференциальная диагностика при гепатомегалии
Дифференциальная диагностика при гепатомегалии Острый аппендицит или воспаление червеобразного отростка
Острый аппендицит или воспаление червеобразного отростка Ерте токсикоздардың сирек түрлері
Ерте токсикоздардың сирек түрлері Экзантема (сыпь)
Экзантема (сыпь) Холинолитические ЛС
Холинолитические ЛС Правила наложения повязок
Правила наложения повязок Целиакия (глютеновая энтеропатия)
Целиакия (глютеновая энтеропатия) Этика и деонтология в медицине
Этика и деонтология в медицине Анализ многолетней динамики заболеваемости в эпидемиологической диагностике
Анализ многолетней динамики заболеваемости в эпидемиологической диагностике Стоматологические проявления при ЖДА
Стоматологические проявления при ЖДА Қазақстан Республикасы аймағандағы туберкулез ауруының құрлымы мен деңгейін талдау
Қазақстан Республикасы аймағандағы туберкулез ауруының құрлымы мен деңгейін талдау Управление конфликтами
Управление конфликтами Паллиативная помощь онкологическим больным
Паллиативная помощь онкологическим больным Телесно-ориентированная психотерапия в массаже и детской абилитации
Телесно-ориентированная психотерапия в массаже и детской абилитации Патогенез себореи (акне). Механизм высыпаний
Патогенез себореи (акне). Механизм высыпаний Тотальная внутривенная анестезия
Тотальная внутривенная анестезия Болезнь Рейно
Болезнь Рейно Подстройка под собеседника. Вербальные и невербальные параметры
Подстройка под собеседника. Вербальные и невербальные параметры Электролечение постоянным и импульсным током низкой частоты
Электролечение постоянным и импульсным током низкой частоты Лекарственные препараты растительного происхождения
Лекарственные препараты растительного происхождения Воздушно-капельные инфекции
Воздушно-капельные инфекции Заболевания новорожденных
Заболевания новорожденных Геморрагические диатезы
Геморрагические диатезы Гипертоническая болезнь
Гипертоническая болезнь История развития сестринского дела
История развития сестринского дела Моя профессия - медицинская сестра
Моя профессия - медицинская сестра Эпикриз. Практика
Эпикриз. Практика