Содержание
- 2. План: Поиск информации в русскоязычных сайтах Использование англоязычных поисковых систем Pubmed AJP
- 4. Вялотекущая шизофрения в общемедицинской практике А.Б.Смулевич НЦПЗ РАМН, Москва На первом этапе комбинированной психофармакотерапии используются антидепрессанты
- 5. Кардиологические аспекты проблемы переносимости и безопасности нейролептика М.Ю.Дробижев Клиника кардиологии ММА им. И.М. Сеченова, НЦПЗ РАМН,
- 6. Комбинированное использование антидепрессантов и нейролептиков при аффективных расстройствах и шизофрении: показания к назначению, побочные эффекты и
- 8. Drug interactions of psychotropic drugs Sawada Y, Satoh H. Laboratory of Drug Informatics, Graduate School of
- 9. Benzodiazepines alone or in combination with antipsychotic drugs for acute psychosis Gillies D, Beck A, McCloud
- 10. Clozapine combined with different antipsychotic drugs for treatment resistant schizophrenia Cipriani A, Boso M, Barbui C
- 11. Trifluoperazine, an Antipsychotic Agent, Inhibits Cancer Stem Cell Growth and Overcomes Drug Resistance of Lung Cancer
- 12. Double-blind placebo-controlled randomized efficacy and safety trial of add-on treatment of dimebon plus risperidone in schizophrenic
- 13. Combination treatment of depression Høiseth G, Solberg DK, Refsum H. Senter for psykofarmakologi, Diakonhjemmet Sykehus, Norway.
- 15. Multiple Versus Single Antipsychotic Agents for Hospitalized Psychiatric Patients: Case-Control Study of Risks Versus Benefits Franca
- 16. Combined use of risperidone and olanzapine in the treatment of patients with resistant schizophrenia: a preliminary
- 17. Metformin Addition Attenuates Olanzapine-Induced Weight Gain in Drug-Naive First-Episode Schizophrenia Patients: A Double-Blind, Placebo-Controlled Study Ren-Rong
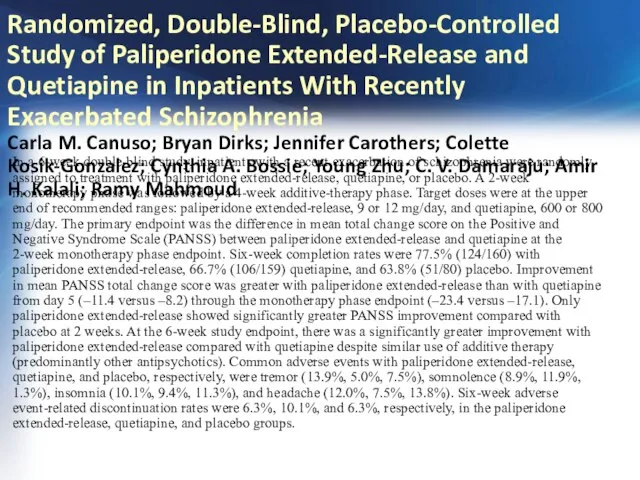
- 18. Randomized, Double-Blind, Placebo-Controlled Study of Paliperidone Extended-Release and Quetiapine in Inpatients With Recently Exacerbated Schizophrenia Carla
- 20. Скачать презентацию
План:
Поиск информации в русскоязычных сайтах
Использование англоязычных поисковых систем
Pubmed
AJP
План:
Поиск информации в русскоязычных сайтах
Использование англоязычных поисковых систем
Pubmed
AJP
Вялотекущая шизофрения в общемедицинской практике
А.Б.Смулевич
НЦПЗ РАМН, Москва
На первом этапе комбинированной
Вялотекущая шизофрения в общемедицинской практике
А.Б.Смулевич
НЦПЗ РАМН, Москва
На первом этапе комбинированной
Кардиологические аспекты проблемы переносимости и безопасности нейролептика
М.Ю.Дробижев
Клиника кардиологии ММА им. И.М.
Кардиологические аспекты проблемы переносимости и безопасности нейролептика М.Ю.Дробижев Клиника кардиологии ММА им. И.М.
Опасность развития желудочковых нарушений ритма резко возрастает при одновременном применении двух нейролептиков (в частности, тиоридазина и других фенотиазинов, тиоридазина и пимозида, пимозида и других фенотиазинов, а также прометазина и других антипсихотиков). Сочетание прометазина с сульпиридом или левомепромазином может приводить к желудочковой тахикардии и пируэтной тахикардии.
Некоторые нейролептики, в частности трифлуоперазин, могут усиливать позднюю кардиотоксичность цитостатика доксорубицина. При этом возможно развитие токсического миокардита.
Наконец, некоторые результаты интеракции нейролептиков с другими препаратами отличаются по своим проявлениям от описанных побочных эффектов антипсихотиков в отношении сердечно-сосудистой системы. В частности, галоперидол и хлорпромазин, особенно при их назначении в высоких дозах, могут противодействовать гипотензивному эффекту b-адреноблокаторов. Сочетание производных фенотиазина с симпатомиметиками сопровождается противодействием вазопрессорному действию этих кардиотропных препаратов. Совместное назначение кветиапина и варфарина может усиливать антигоагулянтное действие последнего.
Комбинированная терапия нейролептиками и вступающими с ними во взаимодействие медикаментозными средствами требует (если вообще допустима) тщательного наблюдения за концентрациями препаратов в плазме крови и побочными эффектами. Очевидно, что выполнение этого требования сопряжено со значительными временными и материальными затратами. Соответственно в обычной лечебной практике следует избегать перечисленных сочетаний.
Комбинированное использование антидепрессантов и нейролептиков при аффективных расстройствах и шизофрении: показания
Комбинированное использование антидепрессантов и нейролептиков при аффективных расстройствах и шизофрении: показания
М.П.Андрусенко, М.А.Морозова
Лаборатория психофармакологии НЦПЗ РАМН, Москва
Назначение комбинированной терапии АД и НЛ в большинстве случаев отражает симптоматический подход: наличие в клинической картине депрессивных и психотических симптомов рассматривается как достаточное показание к ее использованию. Этот подход, как правило, является наиболее характерным в повседневной врачебной практике. Однако результаты целенаправленных иссследований с контрольными группами показывают чрезмерную упрощенность такого подхода. Судя по данным исследований, наиболее важную роль играет не собственно наличие депрессивных и психотических симптомов в клинической картине, а характер их взаимоотношений внутри синдрома. Так, при развитии депрессивно-бредовых состояний в рамках аффективного расстройства комбинированное лечение АД и НЛ является высокоэффективным. Напротив, при лечении острых состояний, определяющихся психотическими расстройствами с элементами депрессивных нарушений, развивающихся в рамках шизофрении и шизоаффективного расстройства, эффективной является монотерапия НЛ, а добавление АД может вести к ухудшению состояния больных. Тем не менее и в рамках шизофрении, возможно, существуют состояния, при которых АД показаны. На это указывают некоторые данные об эффективности добавления АД к НЛ при постпсихотических депрессиях. Уточнение показаний к комбинированному назначению АД и НЛ требует дальнейших клинических и клинико-фармакологических исследований.
Drug interactions of psychotropic drugs
Sawada Y, Satoh H.
Laboratory of Drug Informatics, Graduate School of Pharmaceutical Sciences,
Drug interactions of psychotropic drugs Sawada Y, Satoh H. Laboratory of Drug Informatics, Graduate School of Pharmaceutical Sciences,
For the appropriate use of psychotropic drugs, such as hypnotics, antidepressants and antipsychotics, knowledge of the pharmacokinetic characteristics and the interactions of these drugs are required. The mechanisms of drug interaction can be subdivided into pharmacokinetic interactions and pharmacodynamic interactions. Among the former, interactions involving inhibition or induction of cytochrome P450 (CYP) enzymes are clinically very important. If such interactions cause an increase of systemic exposure to psychotropic drugs, adverse effects are likely, while a decrease exposure may lead to treatment failure. In this article, we review drug interactions of psychotropic drugs from the viewpoints of clinical evidence, mechanism, and management.
Benzodiazepines alone or in combination with antipsychotic drugs for acute psychosis
Gillies
Benzodiazepines alone or in combination with antipsychotic drugs for acute psychosis Gillies
In this review we estimated the effects of benzodiazepines (e.g. diazepam, lorazapam, midazolam, clonazepam), for controlling acutely disturbed behaviour and psychotic symptoms when compared with placebo, antipsychotic drugs such as haloperidol, or a combination of both antipsychotics and benzodiazepines. We concluded from this review that there is little difference between benzodiazepines and antipsychotics for the management of acute psychotic behaviour, and that the few small trials we found were often poorly reported. The lower incidence of distressing acute movement disorder in people receiving benzodiazepines may encourage use of benzodiazepines in preference to the older antipsychotics (administered without additional anti-movement-disorder medication), but these adverse effects can be prevented with the use of alternative drugs such as procyclidine and promethazine. However, all the studies included in this review were underpowered and failed to identify potentially serious adverse effects of benzodiazepines such as respiratory depression. This review highlights the need for further more comprehensive studies in this area.
Clozapine combined with different antipsychotic drugs for treatment resistant schizophrenia
Cipriani A,
Clozapine combined with different antipsychotic drugs for treatment resistant schizophrenia Cipriani A,
When people on clozapine plus risperidone were compared to those on clozapine plus sulpiride, more people taking risperidone showed an improvement generally. However, when specific symptoms of schizophrenia were studied, there was change for the better in all groups but no second antipsychotic was significantly better than the one it was compared to. When looking at adverse effects, people taking sulpiride were slightly more likely to suffer from hypersalivation and weight gain than those taking risperidone.
Trifluoperazine, an Antipsychotic Agent, Inhibits Cancer Stem Cell Growth and Overcomes Drug Resistance
Trifluoperazine, an Antipsychotic Agent, Inhibits Cancer Stem Cell Growth and Overcomes Drug Resistance
Using in silico drug screening via Connectivity Map followed by empirical validations, we repurposed an existing phenothiazine-like anti-psychotic drug, trifluoperazine, as a potential anti-CSC agent that could overcome EGFR-TKI and chemotherapy resistance.
Double-blind placebo-controlled randomized efficacy and safety trial of add-on treatment of
Double-blind placebo-controlled randomized efficacy and safety trial of add-on treatment of
56 male subjects with paranoid schizophrenia were included in the study. All the patients demonstrated therapeutic response to risperidone as treatment of the acute psychotic episode. After 4 weeks of stability patients were randomized into two groups with placebo or dimebon add-on treatment in a 1 to 1 ratio for 8 weeks. PANSS, CGI-S, CSDS and NSA-16 were used as clinical measures of symptom severity. Different aspects of memory, psycho-motor coordination and executive functioning were assessed with a battery of cognitive tests. Clinical and cognitive assessment was performed twice: after a patient was randomized and 2 months later.
Combination treatment of depression
Høiseth G, Solberg DK, Refsum H.
Senter for psykofarmakologi, Diakonhjemmet Sykehus, Norway.
Combination treatment of depression Høiseth G, Solberg DK, Refsum H. Senter for psykofarmakologi, Diakonhjemmet Sykehus, Norway.
Severe depression is a common diagnosis and a number of studies have demonstrated the superiority of antidepressants to placebos. More than half of the patients remain depressed despite initial treatment. If reasons like incorrect diagnosis and non-optimal choice of drug or doses are excluded,combination therapy may be considered. Augmentation of antidepressants with lithium or the thyroid hormone T3 has documented effectiveness, mainly with tricyclic antidepressants, but is not frequently used. Less documentation exists for a combination of two antidepressant drugs, but their use is relatively common.
Multiple Versus Single Antipsychotic Agents for Hospitalized Psychiatric Patients: Case-Control Study
Multiple Versus Single Antipsychotic Agents for Hospitalized Psychiatric Patients: Case-Control Study
Inpatient treatment groups receiving either antipsychotic monotherapy or polytherapy were matched in terms of age, sex, diagnostic category, and admission clinical ratings (Global Assessment of Functioning [GAF] and Clinical Global Impression [CGI]), which yielded 70 subject pairs. They were compared in terms of total chlorpromazine-equivalent daily dose, changes in total daily dose, length of hospitalization, incidence of adverse effects, and changes in clinical ratings (CGI, GAF, Positive and Negative Syndrome Scale score) between admission and discharge.Initial doses were closely similar at admission for both treatment groups, but the median total final antipsychotic dose was 78% higher for those receiving antipsychotic polytherapy versus monotherapy. Also, median length of stay in the hospital was 55% (8.5 days) longer, and risk of adverse effects was 56% higher with polytherapy, whereas clinical improvement scores were similar (within 11%) for both treatments.
Combined use of risperidone and olanzapine in the treatment of patients with resistant
Combined use of risperidone and olanzapine in the treatment of patients with resistant
Polypharmacy, or the use of multiple drugs in the therapy of psychiatric disorders, is not recommended. However, appropriate combinations of pharmacologic mechanisms may enhance the efficacy of antipsychotic drugs and alter the course of schizophrenia. In recent years, some articles have been published about the successful use of clozapine and risperidone in combination for the treatment of patients with resistant schizophrenic and schizoaffective disorders. However, safety of this drug combination is open to discussion. This report presents the results of a preliminary study of five patients with resistant schizophrenia successfully treated with risperidone-olanzapine combination. The results suggest that this combinationmay be useful. In the future, the efficacy of risperidone-olanzapine combination should be confirmed in larger study populations before its clinical application is considered.
Metformin Addition Attenuates Olanzapine-Induced Weight Gain in Drug-Naive First-Episode Schizophrenia Patients:
Metformin Addition Attenuates Olanzapine-Induced Weight Gain in Drug-Naive First-Episode Schizophrenia Patients:
Forty patients with schizophrenia were randomly assigned to treatment for 12 weeks with olanzapine, 15 mg/day, plus metformin, 750 mg/day (N=20), or olanzapine, 15 mg/day, plus placebo (N=20). This investigation was conducted in a double-blind fashion. Planned assessments included body weight, body mass index, proportion of patients who gained more than 7% of their baseline weight at the end of the 12-week treatment, waist circumference, waist-to-hip ratio, fasting glucose and insulin, insulin resistance index, and scores on the Scale for the Assessment of Positive Symptoms (SAPS) and Scale for the Assessment of Negative Symptoms (SANS). Results: Of the 40 patients who were randomly assigned, 37 (92.5%) completed treatments. The weight, body mass index, waist circumference, and waist-to-hip ratio levels increased less in the olanzapine plus metformin group relative to the olanzapine plus placebo group during the 12-week follow-up period. The insulin and insulin resistance index values of the olanzapine plus placebo group increased significantly at weeks 8 and 12. In contrast, the insulin and insulin resistance index levels of the olanzapine plus metformin group remained unchanged. Significantly fewer patients in the olanzapine plus metformin group relative to patients in the olanzapine plus placebo group increased their baseline weight by more than 7%, which was the cutoff for clinically meaningful weight gain. There was a significant decrease in SAPS and SANS scores within each group from baseline to week 12, with no between-group differences. Metformin was tolerated well by all patients.
Randomized, Double-Blind, Placebo-Controlled Study of Paliperidone Extended-Release and Quetiapine in Inpatients
Randomized, Double-Blind, Placebo-Controlled Study of Paliperidone Extended-Release and Quetiapine in Inpatients
In a 6-week double-blind study, inpatients with a recent exacerbation of schizophrenia were randomly assigned to treatment with paliperidone extended-release, quetiapine, or placebo. A 2-week monotherapy phase was followed by a 4-week additive-therapy phase. Target doses were at the upper end of recommended ranges: paliperidone extended-release, 9 or 12 mg/day, and quetiapine, 600 or 800 mg/day. The primary endpoint was the difference in mean total change score on the Positive and Negative Syndrome Scale (PANSS) between paliperidone extended-release and quetiapine at the 2-week monotherapy phase endpoint. Six-week completion rates were 77.5% (124/160) with paliperidone extended-release, 66.7% (106/159) quetiapine, and 63.8% (51/80) placebo. Improvement in mean PANSS total change score was greater with paliperidone extended-release than with quetiapine from day 5 (–11.4 versus –8.2) through the monotherapy phase endpoint (–23.4 versus –17.1). Only paliperidone extended-release showed significantly greater PANSS improvement compared with placebo at 2 weeks. At the 6-week study endpoint, there was a significantly greater improvement with paliperidone extended-release compared with quetiapine despite similar use of additive therapy (predominantly other antipsychotics). Common adverse events with paliperidone extended-release, quetiapine, and placebo, respectively, were tremor (13.9%, 5.0%, 7.5%), somnolence (8.9%, 11.9%, 1.3%), insomnia (10.1%, 9.4%, 11.3%), and headache (12.0%, 7.5%, 13.8%). Six-week adverse event-related discontinuation rates were 6.3%, 10.1%, and 6.3%, respectively, in the paliperidone extended-release, quetiapine, and placebo groups.




 Реабилитация заболеваний дыхательной системы у детей
Реабилитация заболеваний дыхательной системы у детей Аллергия - проблема XXI века
Аллергия - проблема XXI века Обструктивный синдром у детей
Обструктивный синдром у детей Физическое развитие детей раннего возраста
Физическое развитие детей раннего возраста Лечебная физкультура (ЛФК) для восстановления позвоночника
Лечебная физкультура (ЛФК) для восстановления позвоночника Остеомиелит салдары
Остеомиелит салдары Пандемии прошлого в сравнении с пандемией COVID-19
Пандемии прошлого в сравнении с пандемией COVID-19 Грипп: профилактика и лечение
Грипп: профилактика и лечение Удивительная жидкость - кровь
Удивительная жидкость - кровь Сосудистые средства
Сосудистые средства Диагностика психологической готовности ребенка к школе
Диагностика психологической готовности ребенка к школе Основные характеристики ВИЧ - инфекции
Основные характеристики ВИЧ - инфекции Синдром анемии в обще-врачебной практике
Синдром анемии в обще-врачебной практике Всемирный день борьбы против рака
Всемирный день борьбы против рака Преодоление конфликтов. Виды конфликтов
Преодоление конфликтов. Виды конфликтов Обучение альтернативной коммуникации детей с ОПФР
Обучение альтернативной коммуникации детей с ОПФР Дифференцированный логопедический массаж
Дифференцированный логопедический массаж Организация питания пациентов терапевтического и хирургического профиля
Организация питания пациентов терапевтического и хирургического профиля Жатыр мойны обыры
Жатыр мойны обыры Психология малой группы
Психология малой группы Алгоритмы диагностики и лечения злокачественных новообразований
Алгоритмы диагностики и лечения злокачественных новообразований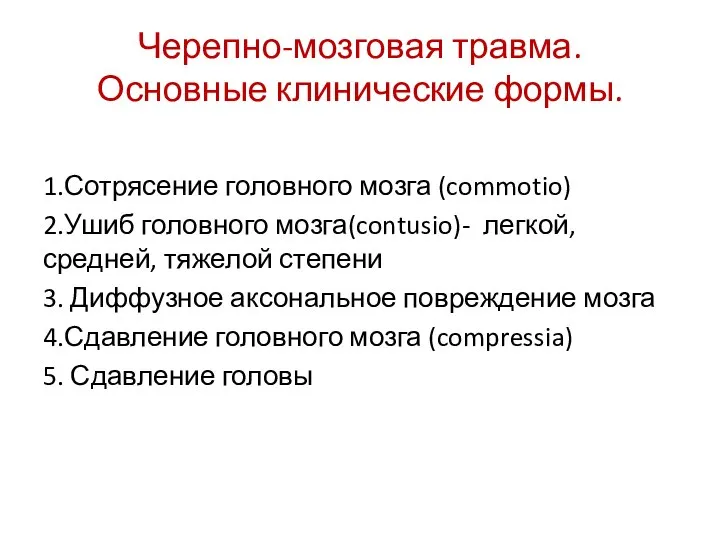 Черепно-мозговая травма. Основные клинические формы
Черепно-мозговая травма. Основные клинические формы Conflict
Conflict Переломы костей
Переломы костей Как понять, что нужно клиенту
Как понять, что нужно клиенту Гиршпрунг ауруының визуалды диагностикасы
Гиршпрунг ауруының визуалды диагностикасы Новая линия косметических средств MEZOcomplex
Новая линия косметических средств MEZOcomplex Диэнай. Зачем нужна фрагментированная ДНК
Диэнай. Зачем нужна фрагментированная ДНК