Содержание
- 2. About these slides These slides give a comprehensive overview of the EASL clinical practice guidelines on
- 3. About these slides Definitions of all abbreviations shown in these slides are provided within the slide
- 4. Chair Julia Wendon Panel members Juan Cordoba, Anil Dhawan, Fin Stolze Larsen, Michael Manns, Frederik Nevens,
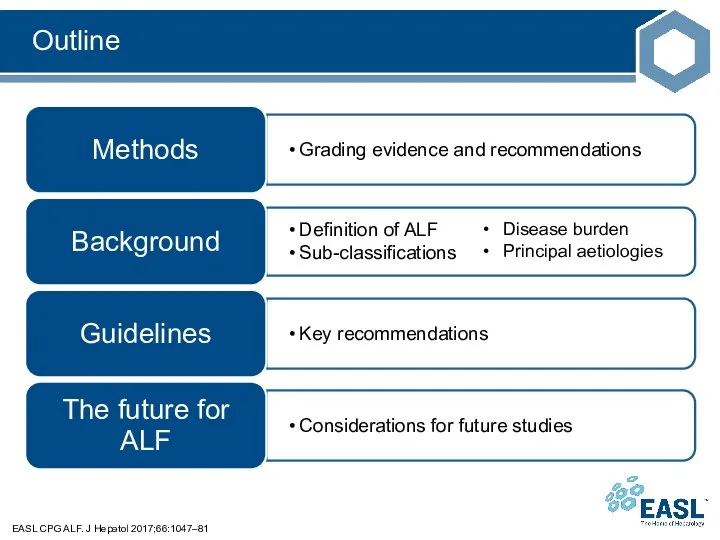
- 5. Outline EASL CPG ALF. J Hepatol 2017;66:1047–81 Disease burden Principal aetiologies
- 6. Methods Grading evidence and recommendations
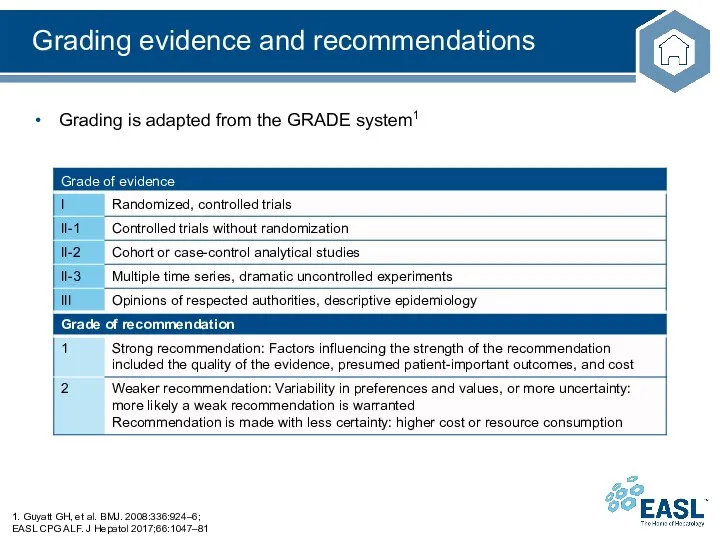
- 7. Grading evidence and recommendations Grading is adapted from the GRADE system1 1. Guyatt GH, et al.
- 8. Background Definition of ALF Sub-classifications Disease burden Principal aetiologies
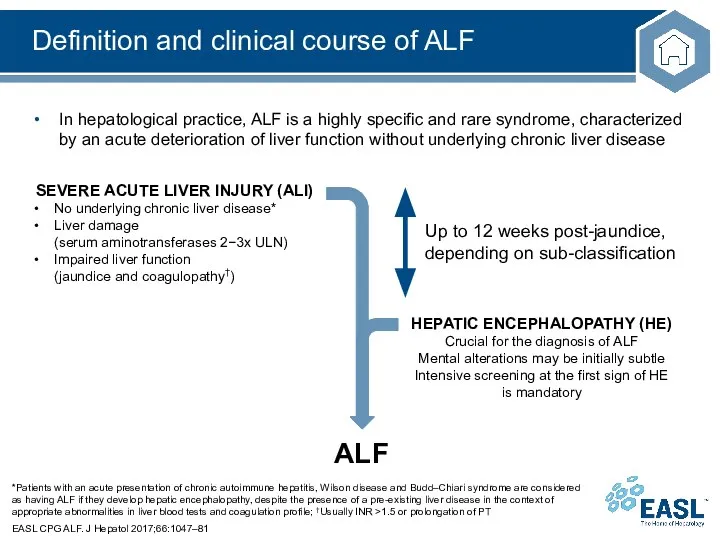
- 9. Definition and clinical course of ALF *Patients with an acute presentation of chronic autoimmune hepatitis, Wilson
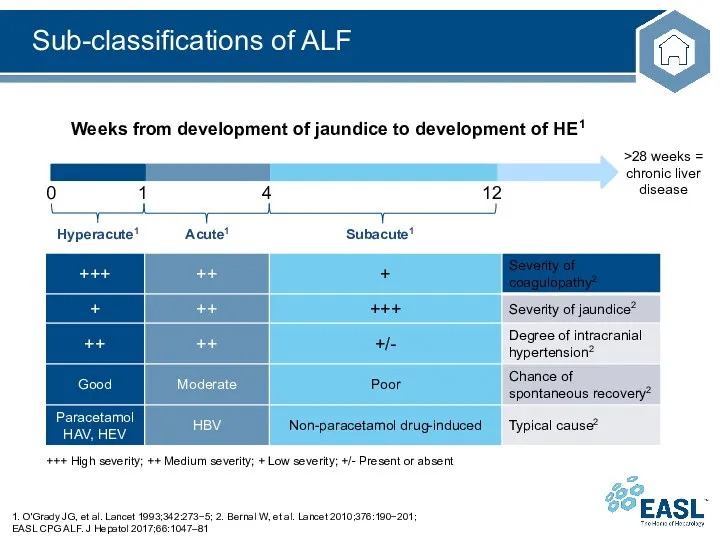
- 10. Sub-classifications of ALF 1. O'Grady JG, et al. Lancet 1993;342:273−5; 2. Bernal W, et al. Lancet
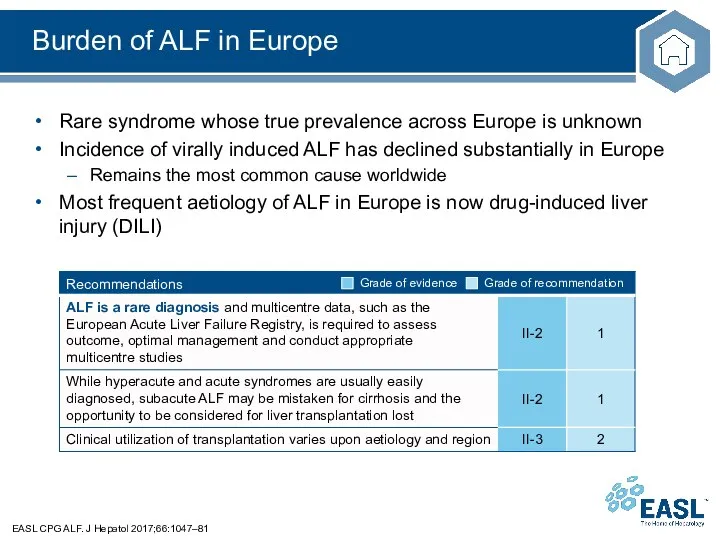
- 11. Burden of ALF in Europe EASL CPG ALF. J Hepatol 2017;66:1047–81 Rare syndrome whose true prevalence
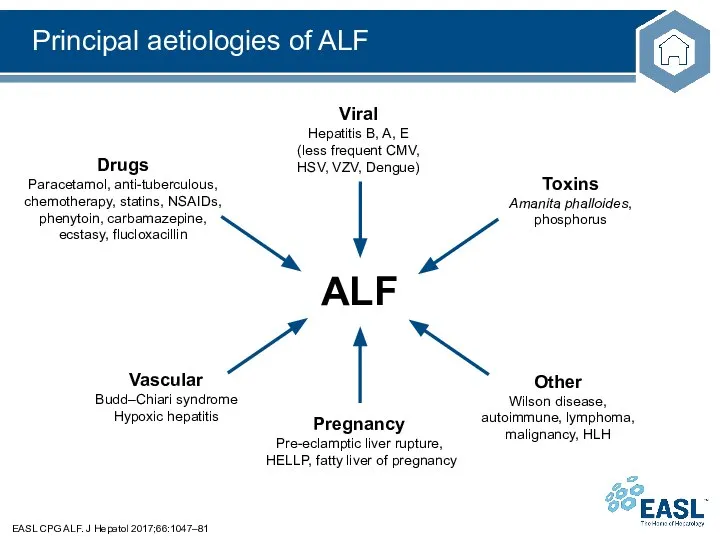
- 12. Principal aetiologies of ALF EASL CPG ALF. J Hepatol 2017;66:1047–81
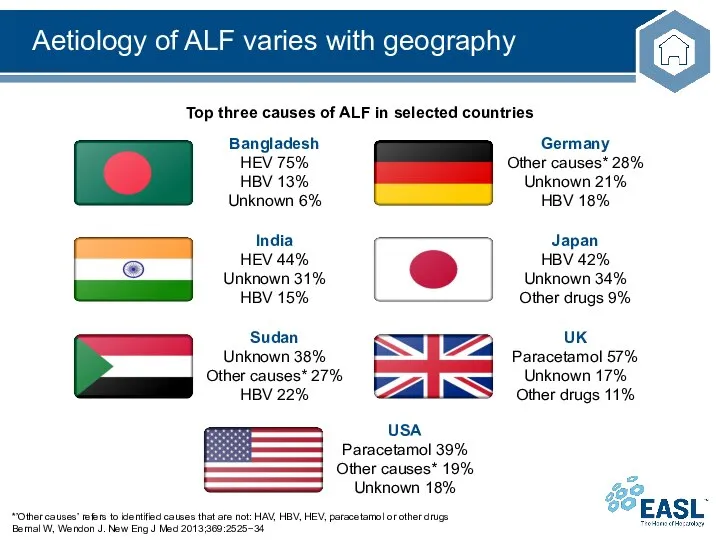
- 13. Aetiology of ALF varies with geography *’Other causes’ refers to identified causes that are not: HAV,
- 14. Guidelines Key recommendations
- 15. Topics EASL CPG ALF. J Hepatol 2017;66:1047–81 Assessment and management at presentation Organ-specific management Cardiovascular Respiratory
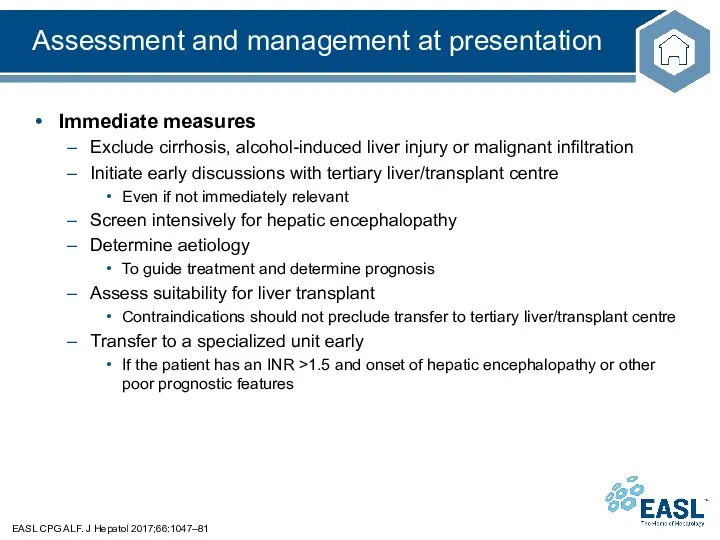
- 16. Assessment and management at presentation EASL CPG ALF. J Hepatol 2017;66:1047–81 Immediate measures Exclude cirrhosis, alcohol-induced
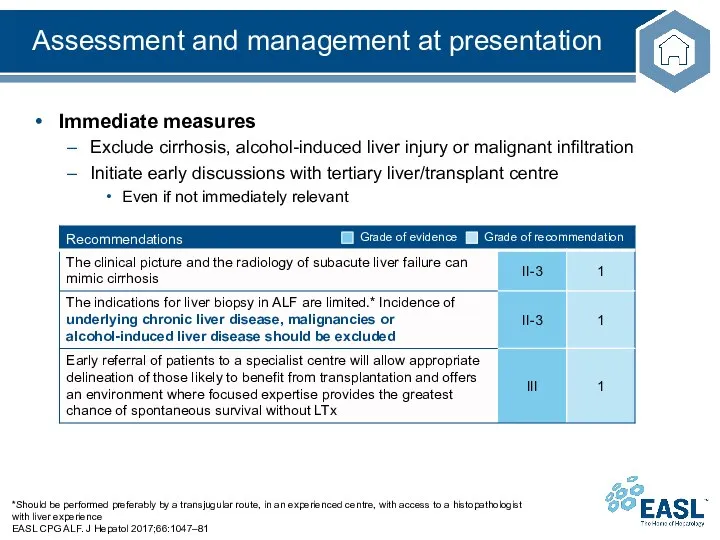
- 17. Assessment and management at presentation *Should be performed preferably by a transjugular route, in an experienced
- 18. Assessment and management at presentation EASL CPG ALF. J Hepatol 2017;66:1047–81 Immediate measures Determine aetiology to
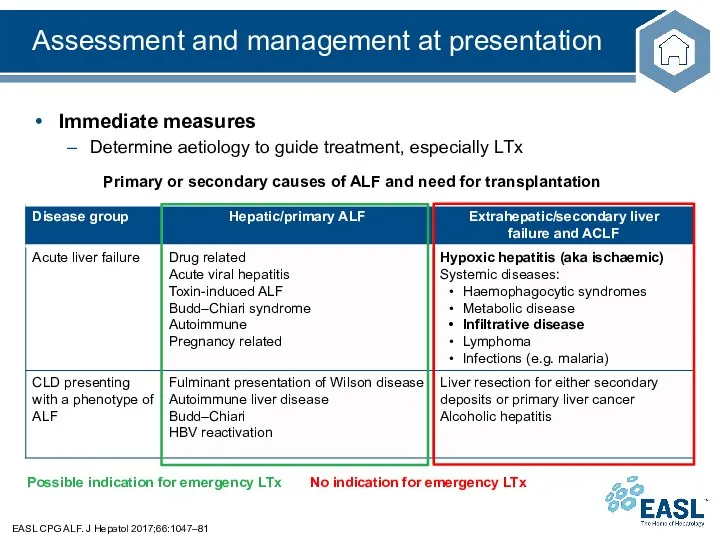
- 19. Differential diagnosis based on clinical features EASL CPG ALF. J Hepatol 2017;66:1047–81 No indication for emergency
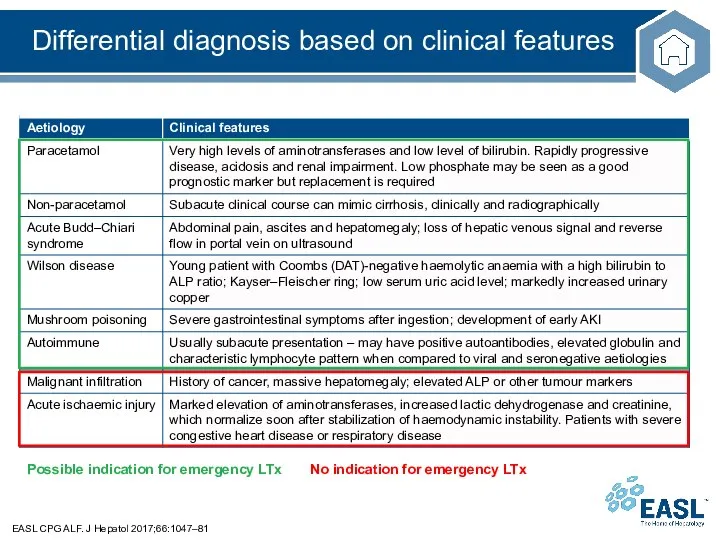
- 20. Aetiologies with no indication for LTx EASL CPG ALF. J Hepatol 2017;66:1047–81 Malignant infiltration of the
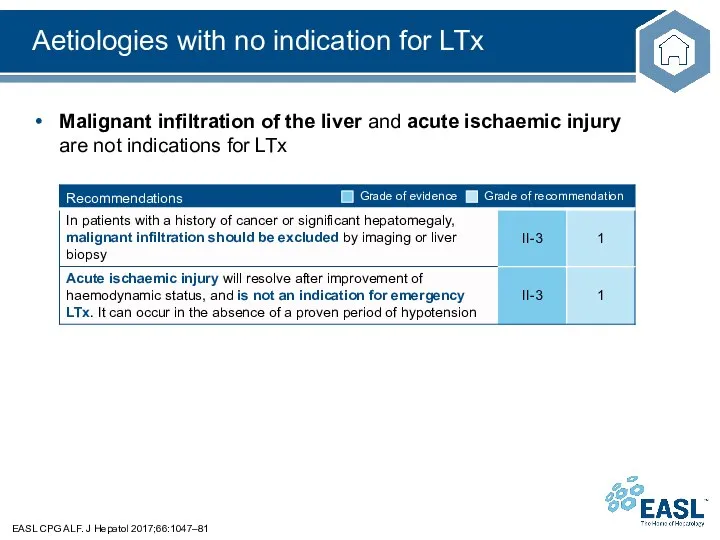
- 21. Aetiologies with possible indication for LTx EASL CPG ALF. J Hepatol 2017;66:1047–81 Drug-induced liver injury is
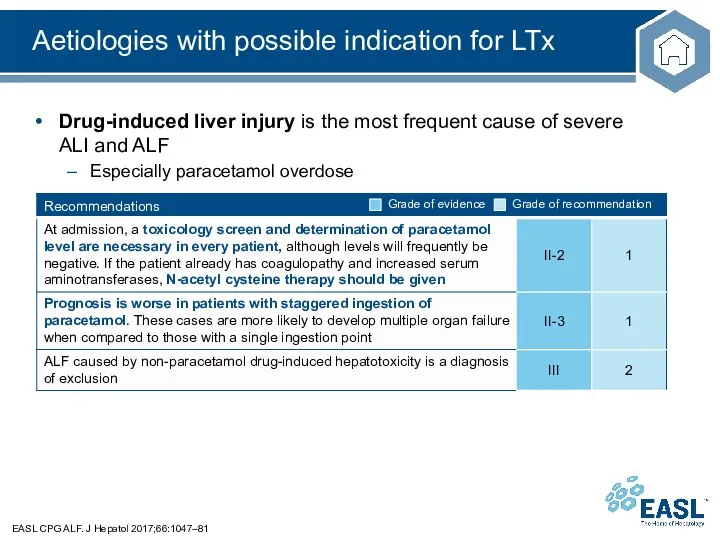
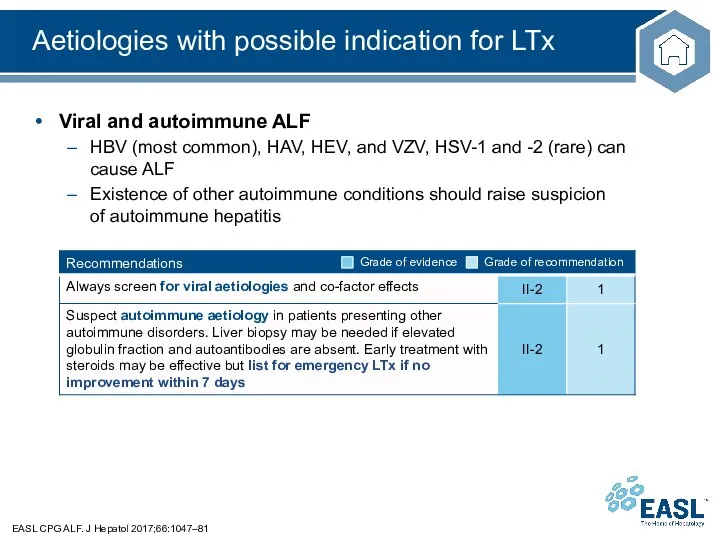
- 22. Aetiologies with possible indication for LTx EASL CPG ALF. J Hepatol 2017;66:1047–81 Viral and autoimmune ALF
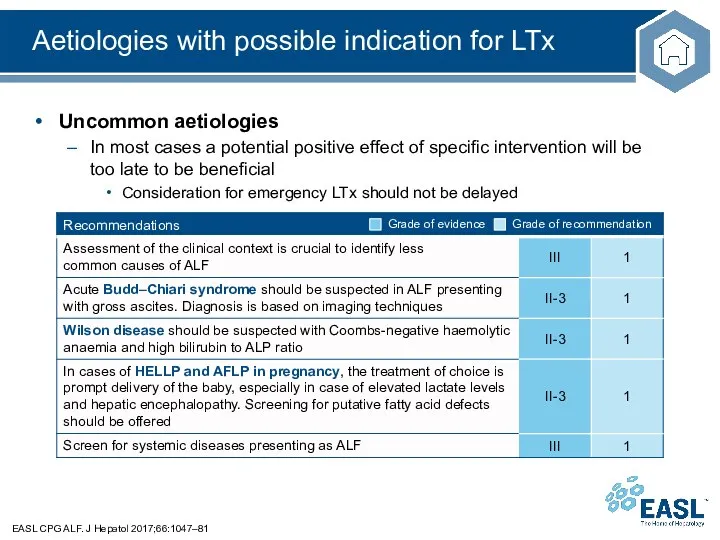
- 23. Aetiologies with possible indication for LTx EASL CPG ALF. J Hepatol 2017;66:1047–81 Uncommon aetiologies In most
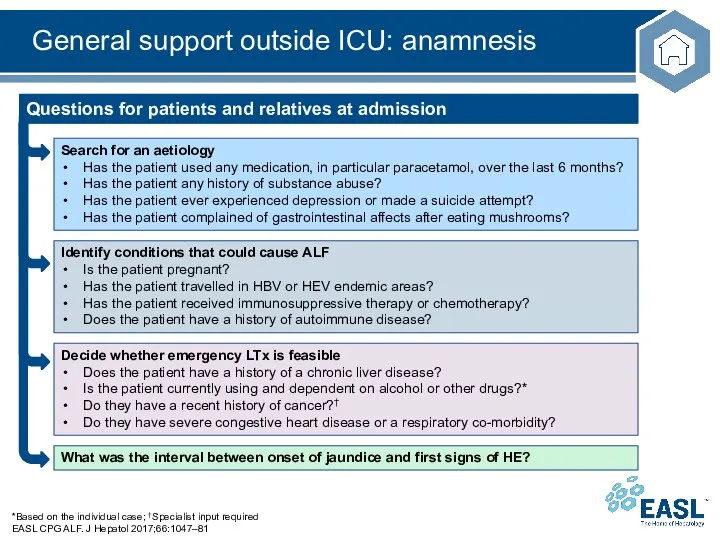
- 24. General support outside ICU: anamnesis *Based on the individual case; †Specialist input required EASL CPG ALF.
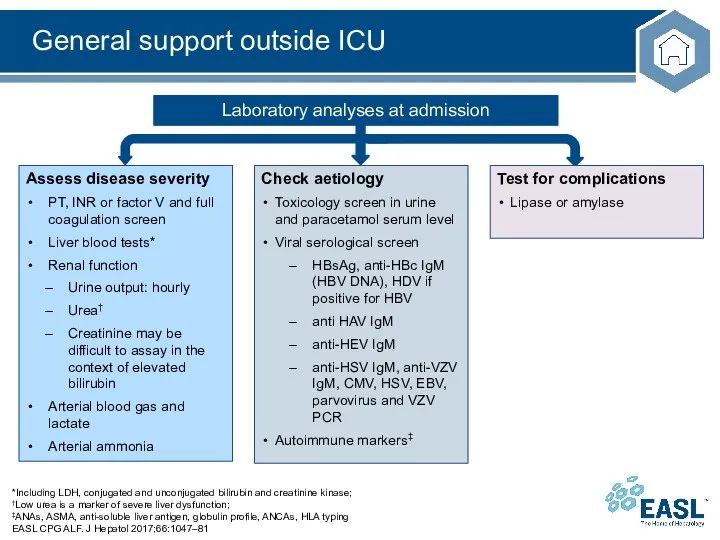
- 25. General support outside ICU *Including LDH, conjugated and unconjugated bilirubin and creatinine kinase; †Low urea is
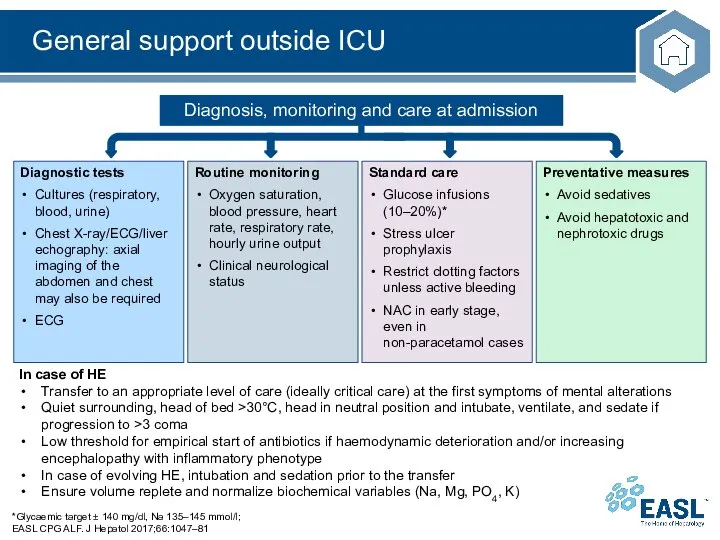
- 26. General support outside ICU *Glycaemic target ± 140 mg/dl, Na 135–145 mmol/l; EASL CPG ALF. J
- 27. Assessment and management at presentation EASL CPG ALF. J Hepatol 2017;66:1047–81 Immediate measures Assess suitability for
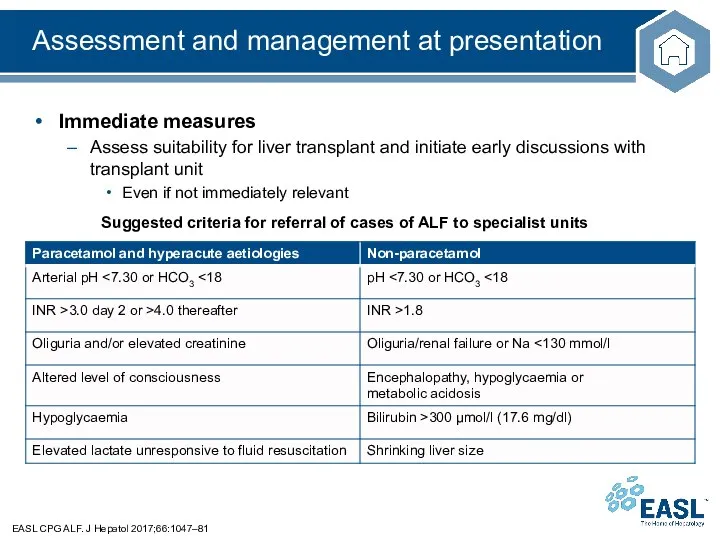
- 28. Assessment and management at presentation EASL CPG ALF. J Hepatol 2017;66:1047–81 Immediate measures Transfer to a
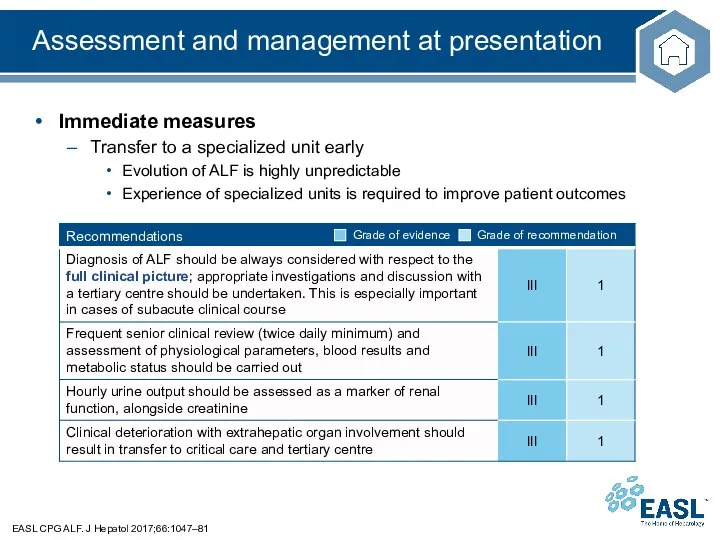
- 29. Organ-specific management EASL CPG ALF. J Hepatol 2017;66:1047–81 Main organ-specific complications in ALF Coagulation/haemostasis Unbalanced haemostasis
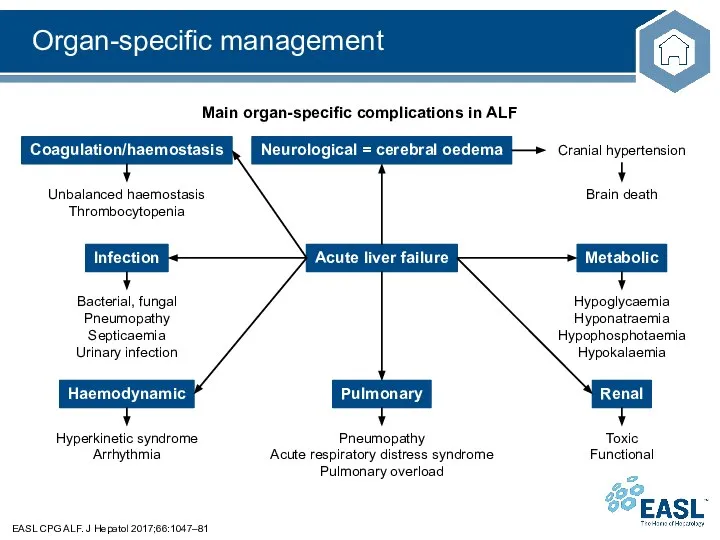
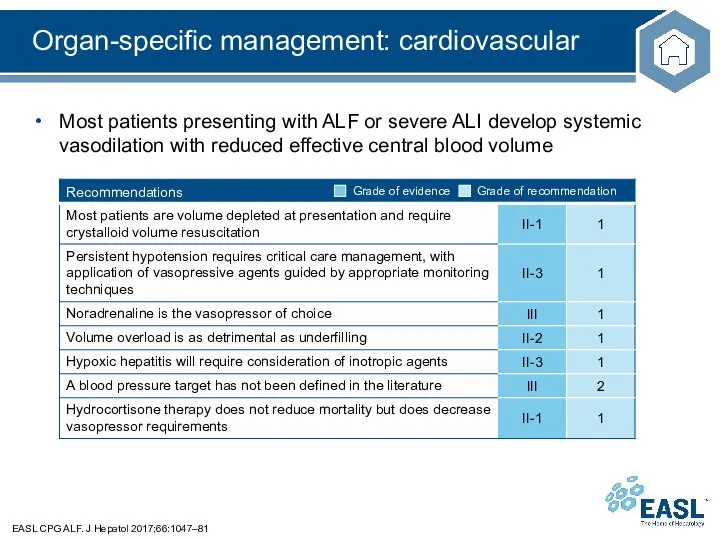
- 30. Organ-specific management: cardiovascular EASL CPG ALF. J Hepatol 2017;66:1047–81 Most patients presenting with ALF or severe
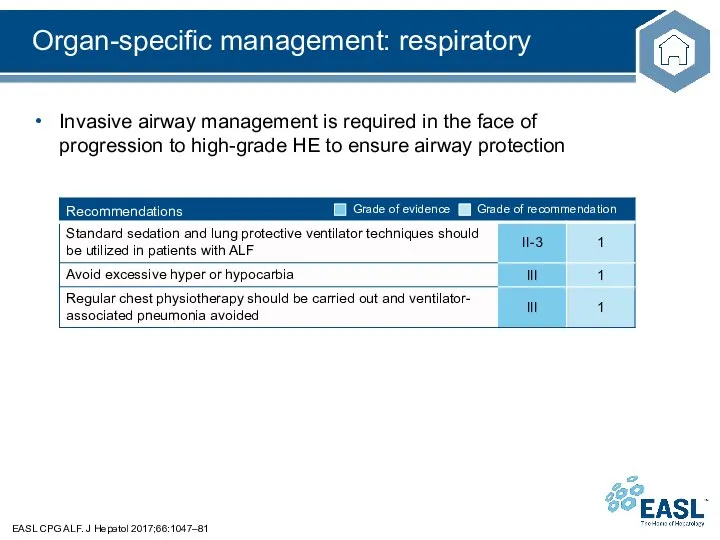
- 31. Organ-specific management: respiratory EASL CPG ALF. J Hepatol 2017;66:1047–81 Invasive airway management is required in the
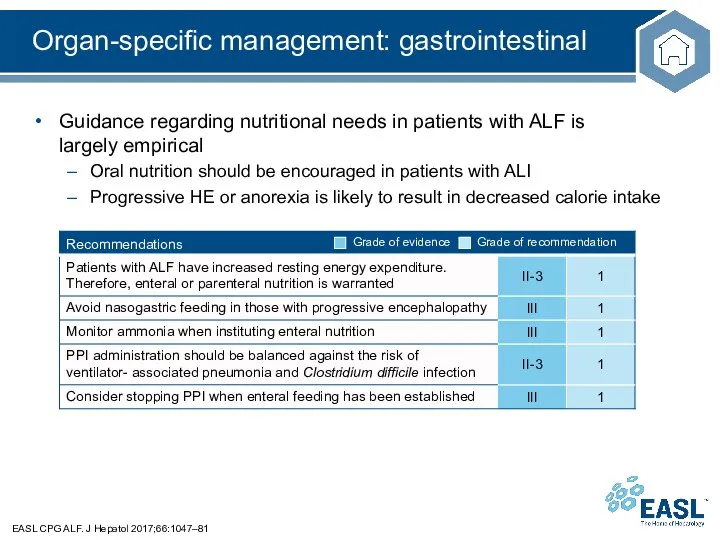
- 32. Organ-specific management: gastrointestinal EASL CPG ALF. J Hepatol 2017;66:1047–81 Guidance regarding nutritional needs in patients with
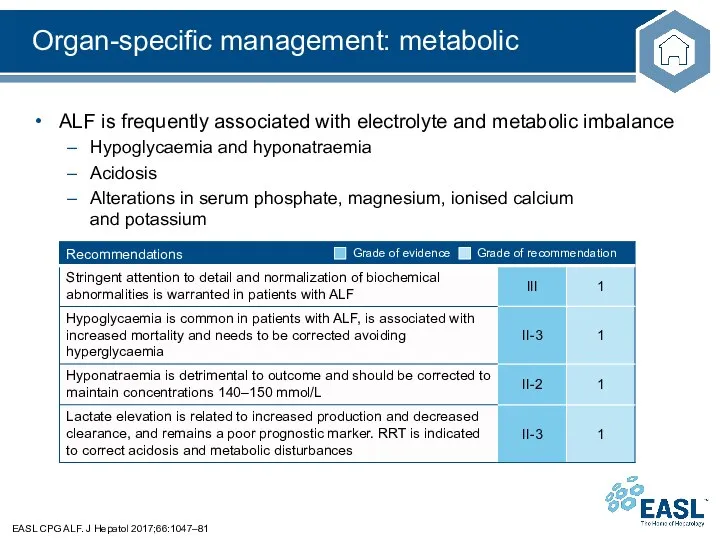
- 33. Organ-specific management: metabolic EASL CPG ALF. J Hepatol 2017;66:1047–81 ALF is frequently associated with electrolyte and
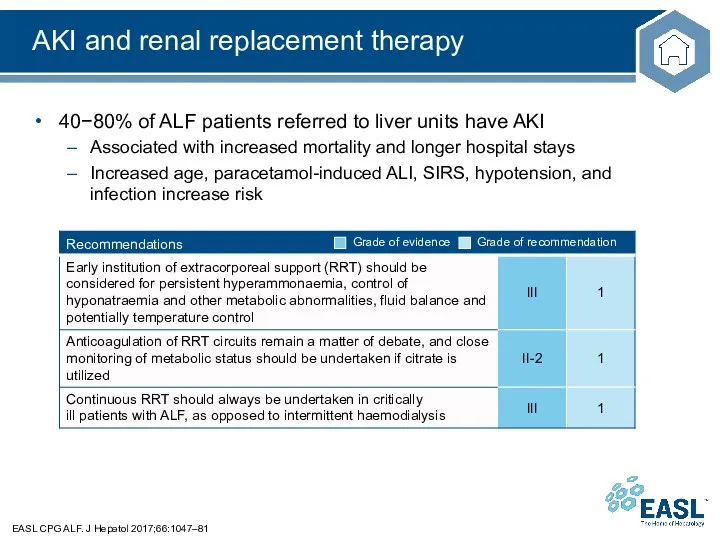
- 34. AKI and renal replacement therapy EASL CPG ALF. J Hepatol 2017;66:1047–81 40−80% of ALF patients referred
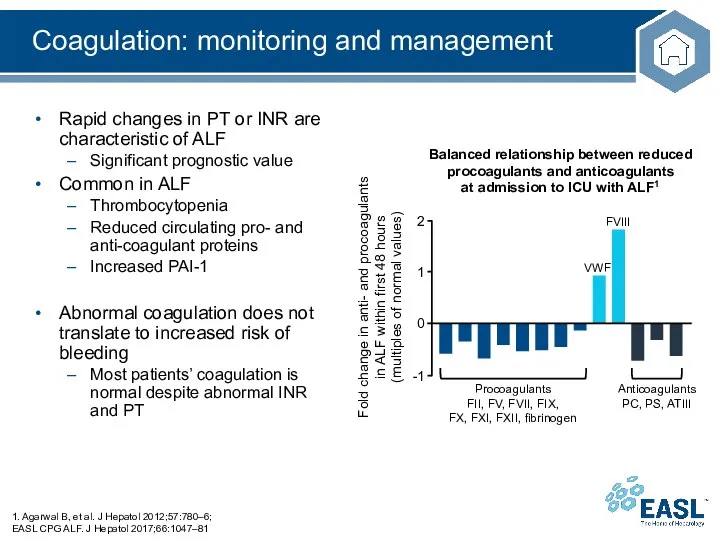
- 35. Rapid changes in PT or INR are characteristic of ALF Significant prognostic value Common in ALF
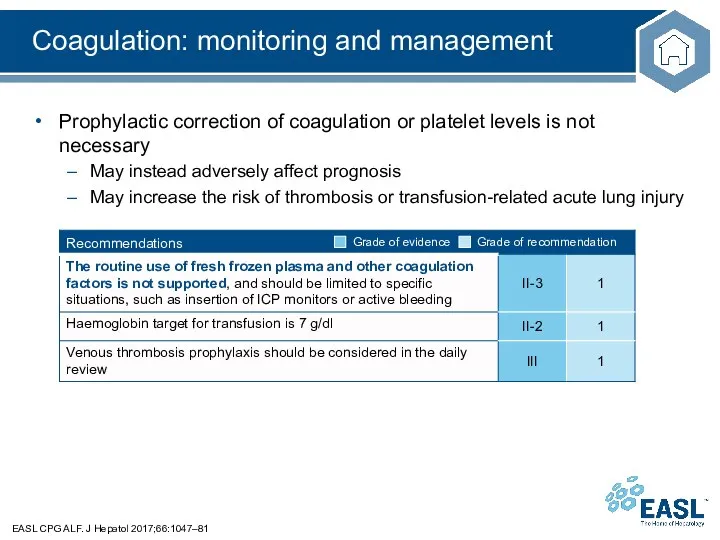
- 36. Coagulation: monitoring and management EASL CPG ALF. J Hepatol 2017;66:1047–81 Prophylactic correction of coagulation or platelet
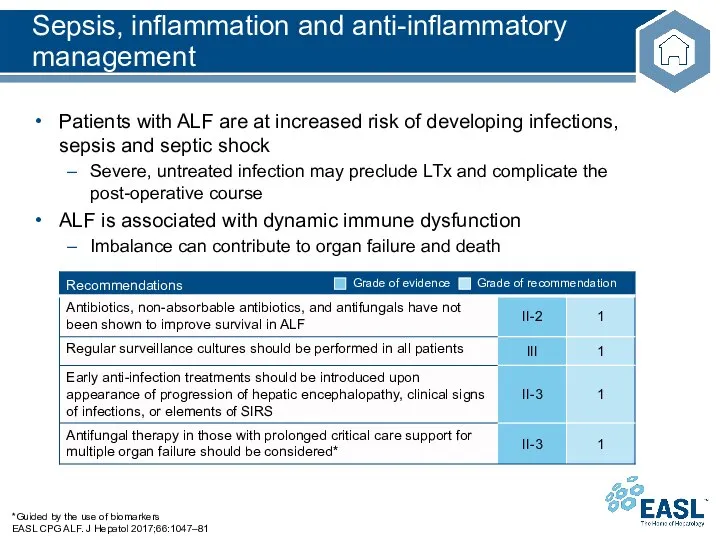
- 37. Sepsis, inflammation and anti-inflammatory management *Guided by the use of biomarkers EASL CPG ALF. J Hepatol
- 38. The brain in ALF: hepatic encephalopathy EASL CPG ALF. J Hepatol 2017;66:1047–81 HE tends to fluctuate
- 39. The brain in ALF: management of HE *Grade 3 coma in this context is not defined
- 40. Brain oedema-induced ICH is a classic complication of HE in ALF Incidence of ICH has decreased
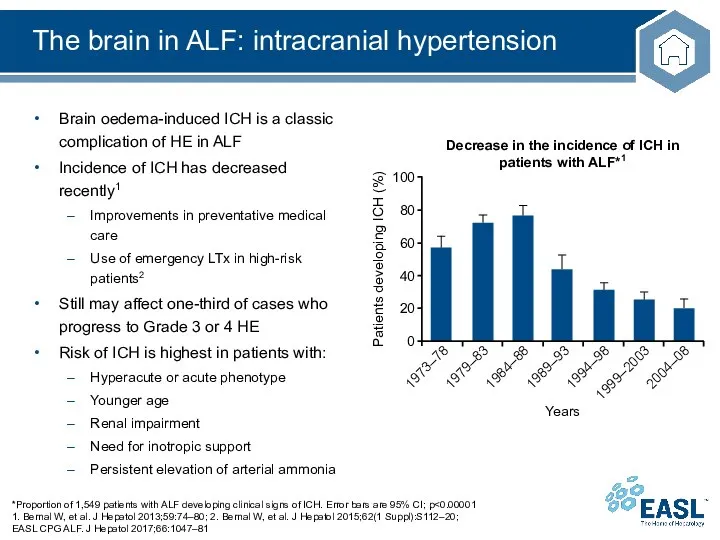
- 41. The brain in ALF EASL CPG ALF. J Hepatol 2017;66:1047–81 Regular clinical and neurological examination is
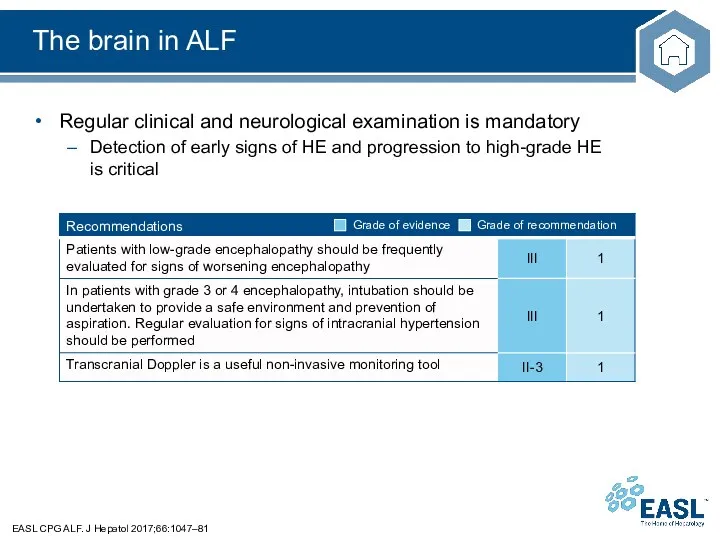
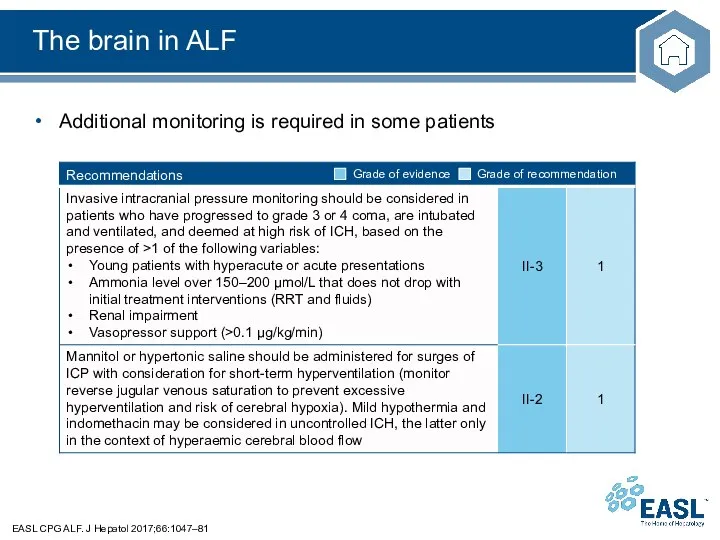
- 42. The brain in ALF EASL CPG ALF. J Hepatol 2017;66:1047–81 Additional monitoring is required in some
- 43. Artificial and bioartificial liver devices *HVP defined as exchange of 8–12 or 15% of ideal body
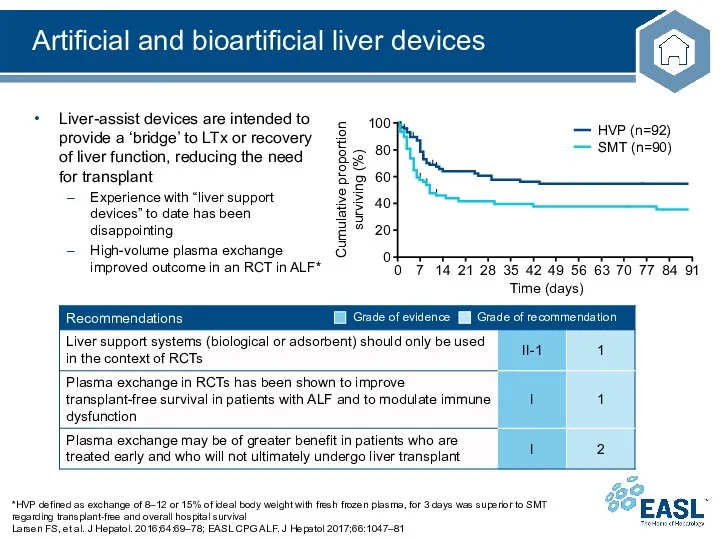
- 44. Impact of liver transplantation in ALF 1.Germani G, et al. J Hepatol 2012;57:288–96; EASL CPG ALF.
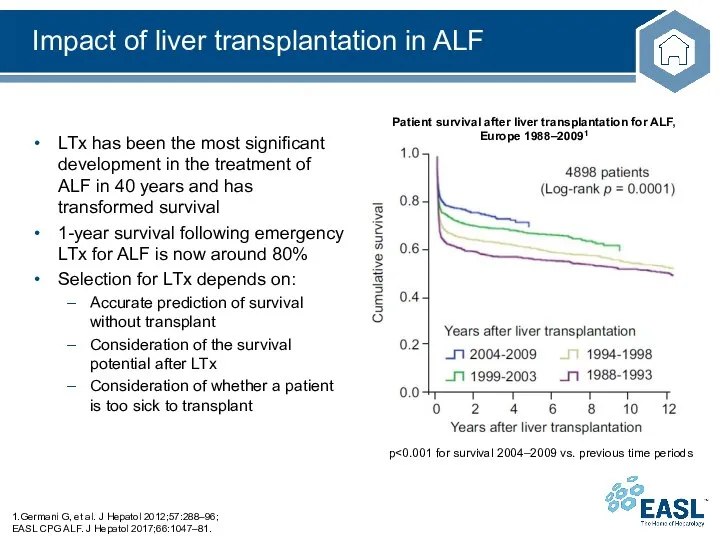
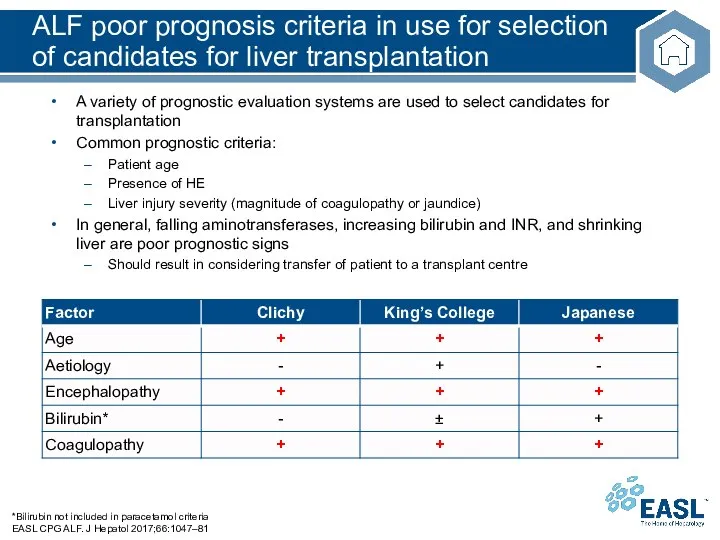
- 45. A variety of prognostic evaluation systems are used to select candidates for transplantation Common prognostic criteria:
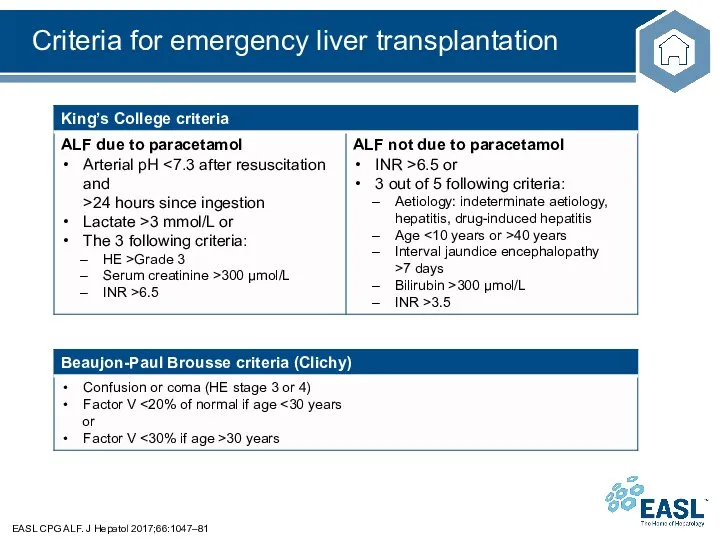
- 46. Criteria for emergency liver transplantation EASL CPG ALF. J Hepatol 2017;66:1047–81
- 47. Comparison of traditional criteria for emergency liver transplantation compared with new alternatives *Gc-globulin is a multifunctional
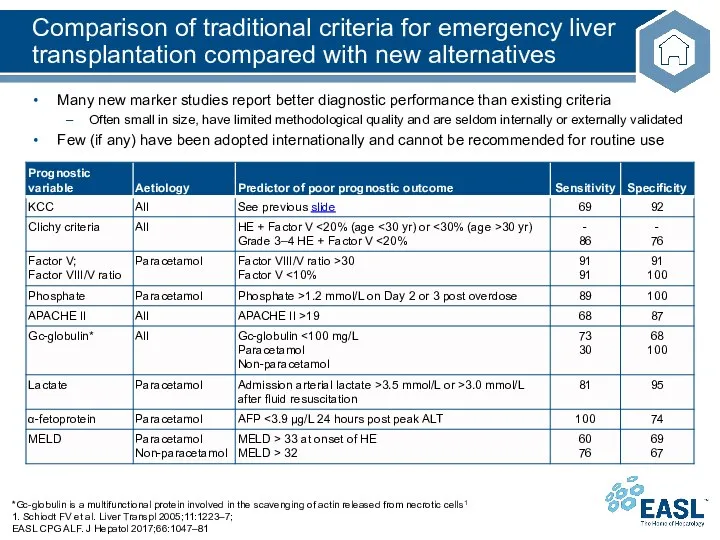
- 48. Liver transplantation EASL CPG ALF. J Hepatol 2017;66:1047–81 Evaluation of patient prognosis is key at the
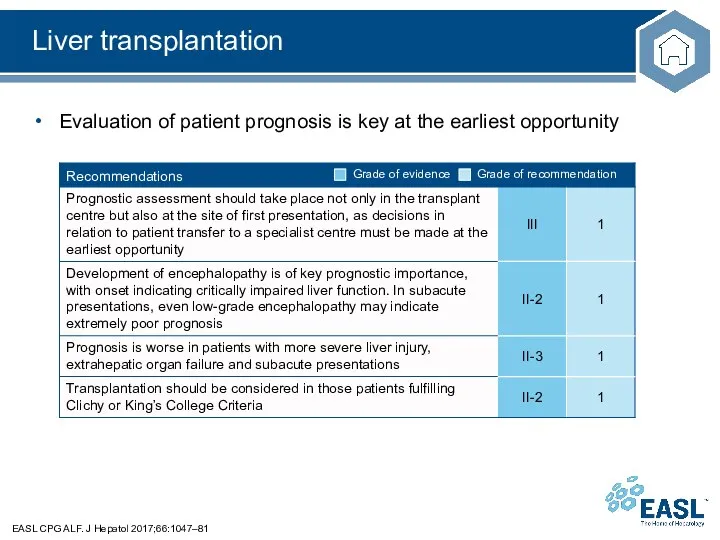
- 49. Liver transplantation EASL CPG ALF. J Hepatol 2017;66:1047–81 Evaluation of patient prognosis is key at the
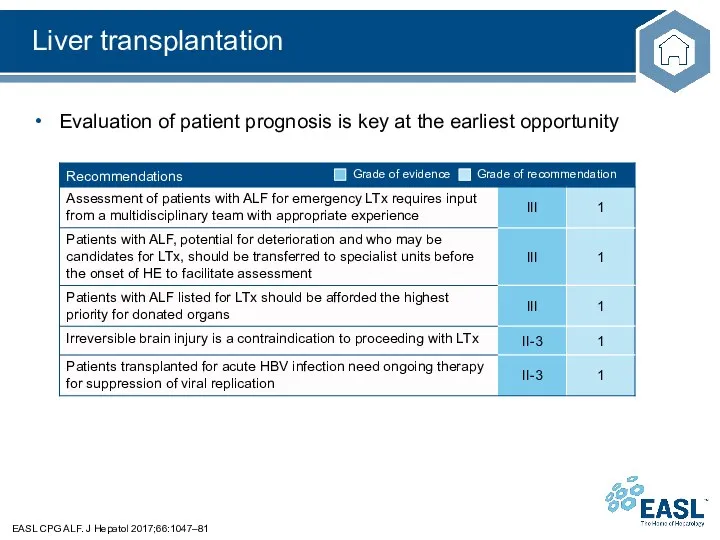
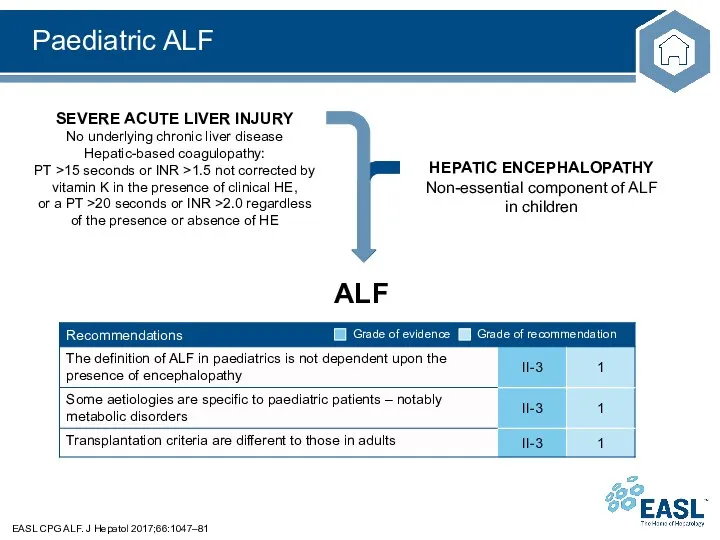
- 50. Paediatric ALF EASL CPG ALF. J Hepatol 2017;66:1047–81
- 51. Most common aetiologies of ALF in children
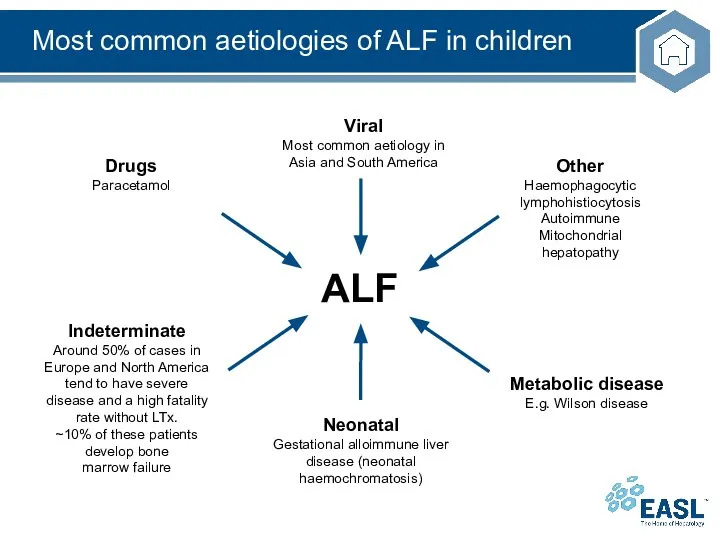
- 52. Most common aetiologies of ALF in children Dhawan A. Liver Transpl. 2008;14 Suppl 2:S80-4. 331 patients
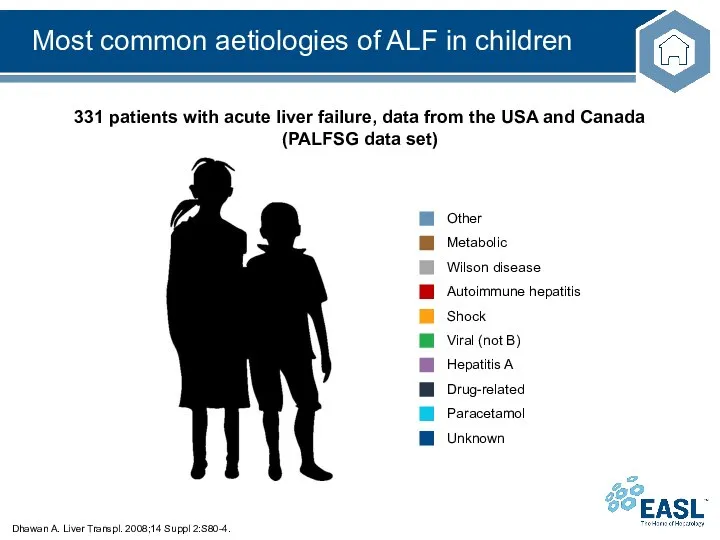
- 53. Liver transplantation in children with ALF EASL CPG ALF. J Hepatol 2017;66:1047–81 LTx is the only
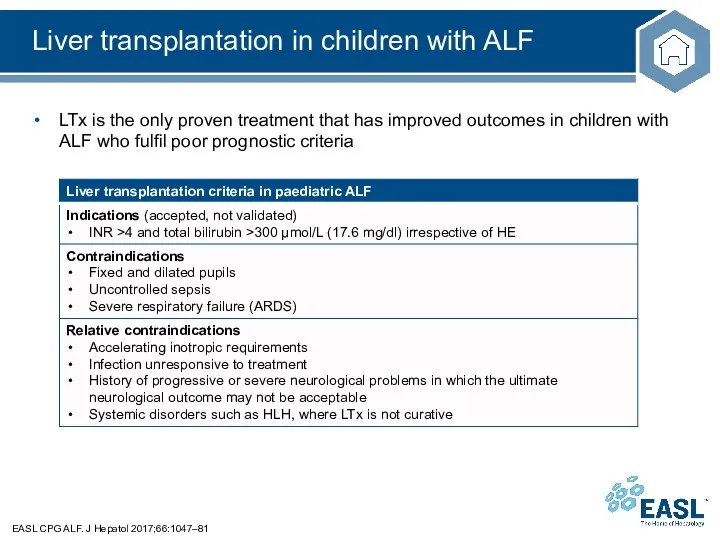
- 54. The future for ALF Considerations for future studies
- 55. Definitions and main clinical features Biomarkers to help predict progression from ALI to ALF Improved tests
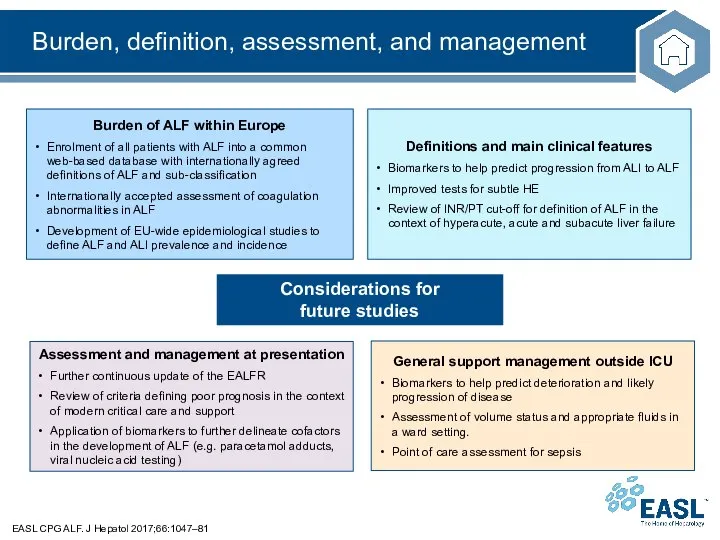
- 56. Organ-specific management EASL CPG ALF. J Hepatol 2017;66:1047–81 The brain in ALF Accurate non-invasive assessment of
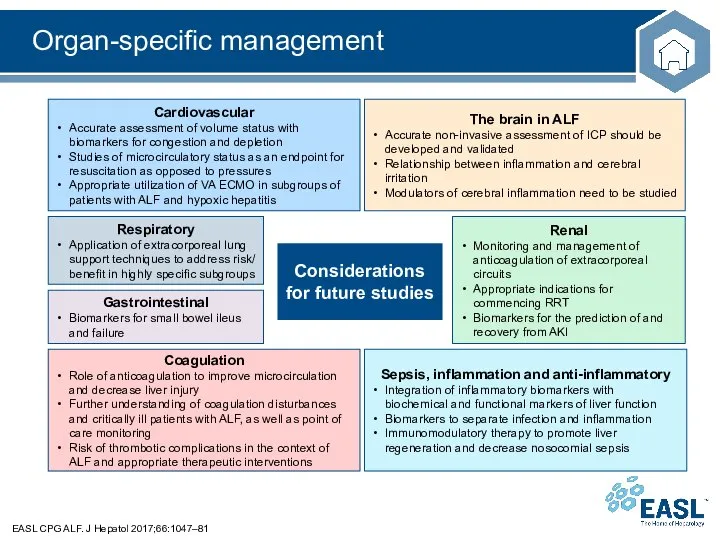
- 58. Скачать презентацию
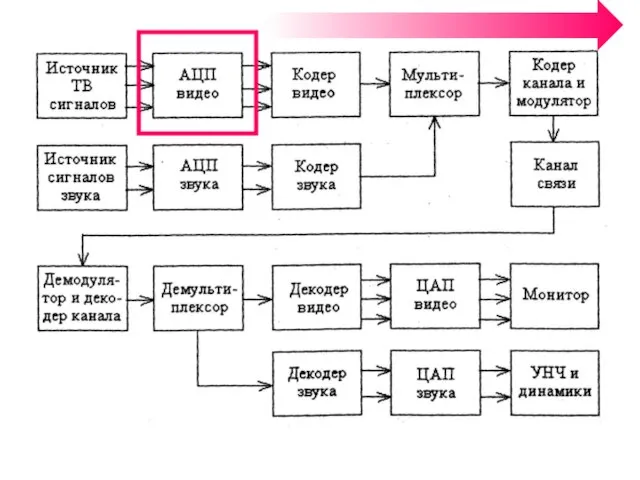 Аналого-цифровое преобразование ТВ-сигнала
Аналого-цифровое преобразование ТВ-сигнала ДОСТУПНАЯ СРЕДА В СИСТЕМЕ ОБРАЗОВАНИЯ (ГК ИСТОК-АУДИО)
ДОСТУПНАЯ СРЕДА В СИСТЕМЕ ОБРАЗОВАНИЯ (ГК ИСТОК-АУДИО) Вторичные преобразования минерального вещества пород, вмещающих углеводороды
Вторичные преобразования минерального вещества пород, вмещающих углеводороды Отток населения России в Москву
Отток населения России в Москву Постановка задач
Постановка задач Department of History of Medicine
Department of History of Medicine Получение нутриентов методами биотехнологии
Получение нутриентов методами биотехнологии Втормет-Волга
Втормет-Волга Техническое регулирование в строительстве: применение Еврокодов в Республике Казахстан
Техническое регулирование в строительстве: применение Еврокодов в Республике Казахстан Авилов О.В. Конф. в СПб
Авилов О.В. Конф. в СПб ИГ, семинар 1, вопрос 1е, Кузьмина
ИГ, семинар 1, вопрос 1е, Кузьмина Крещение Руси: от язычества к христианству
Крещение Руси: от язычества к христианству Технология газовой сварки чугуна
Технология газовой сварки чугуна Мазина Екатерина
Мазина Екатерина Пудель аппликация по мотивам стихотворения С.Я. Маршака
Пудель аппликация по мотивам стихотворения С.Я. Маршака Презентация 28 07 НАПРАВЛЕНИЕ ФРАНЧАЙЗИНГ (1)
Презентация 28 07 НАПРАВЛЕНИЕ ФРАНЧАЙЗИНГ (1) О ремонте подъездов МКД Московской области
О ремонте подъездов МКД Московской области 20130427_tolerantnost_0
20130427_tolerantnost_0 Введение. Оптимизация гидравлики
Введение. Оптимизация гидравлики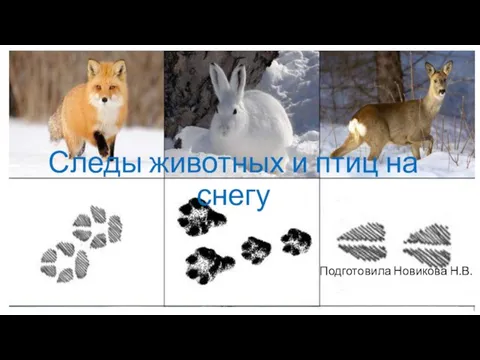 Следы животных и птиц на снегу
Следы животных и птиц на снегу Повышение клиентоориентированности многофункционального центра (МФЦ) Владимирской области
Повышение клиентоориентированности многофункционального центра (МФЦ) Владимирской области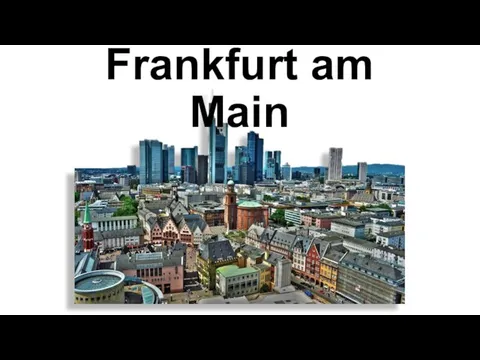 3 ФРАНКФУРТ
3 ФРАНКФУРТ Портфолио ученика начальной школы
Портфолио ученика начальной школы По страницам любимой книги
По страницам любимой книги Общество как форма жизнедеятельности людей
Общество как форма жизнедеятельности людей Повторение
Повторение Мотивация и её роль в жизни человека
Мотивация и её роль в жизни человека Измельчительно-режущее оборудование на предприятиях общественного питания
Измельчительно-режущее оборудование на предприятиях общественного питания