Содержание
- 2. ATOPIC DERMATITIS itch usually a family history of atopy trigger factors Dust mite (common) Sweating Sand
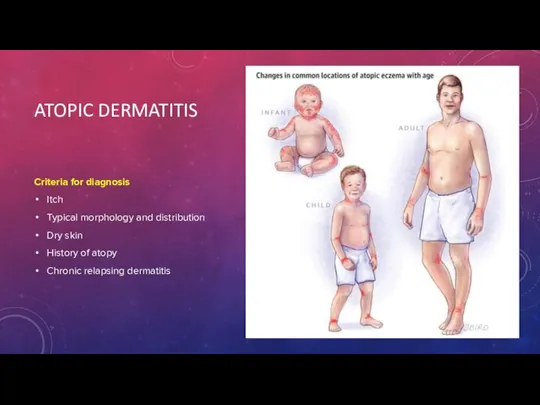
- 3. ATOPIC DERMATITIS Criteria for diagnosis Itch Typical morphology and distribution Dry skin History of atopy Chronic
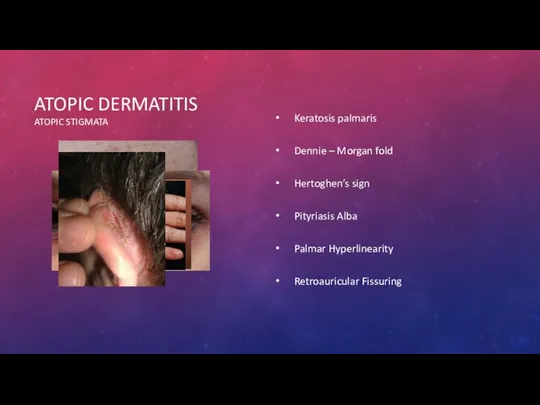
- 4. ATOPIC DERMATITIS ATOPIC STIGMATA Keratosis palmaris Dennie – Morgan fold Hertoghen’s sign Pityriasis Alba Palmar Hyperlinearity
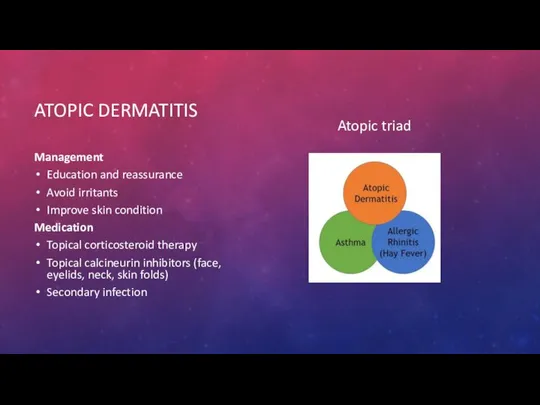
- 5. ATOPIC DERMATITIS Management Education and reassurance Avoid irritants Improve skin condition Medication Topical corticosteroid therapy Topical
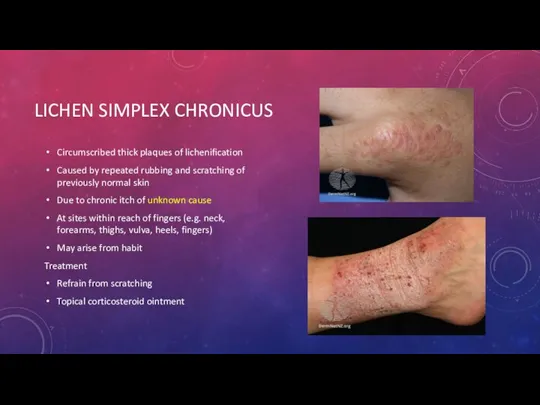
- 6. LICHEN SIMPLEX CHRONICUS Circumscribed thick plaques of lichenification Caused by repeated rubbing and scratching of previously
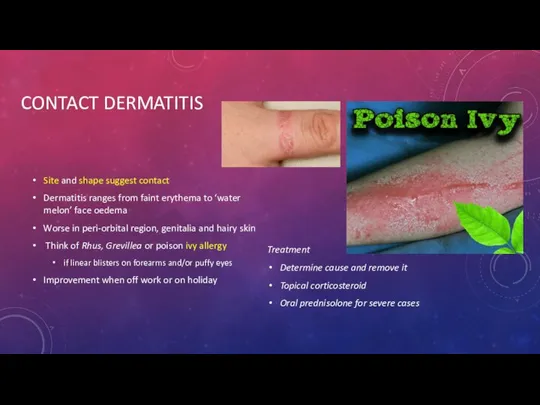
- 7. CONTACT DERMATITIS Site and shape suggest contact Dermatitis ranges from faint erythema to ‘water melon’ face
- 8. CONTACT DERMATITIS PATCH TEST
- 9. STASIS DERMATITIS risk factors: varicose veins high blood pressure obesity, vein surgeries multiple pregnancies a history
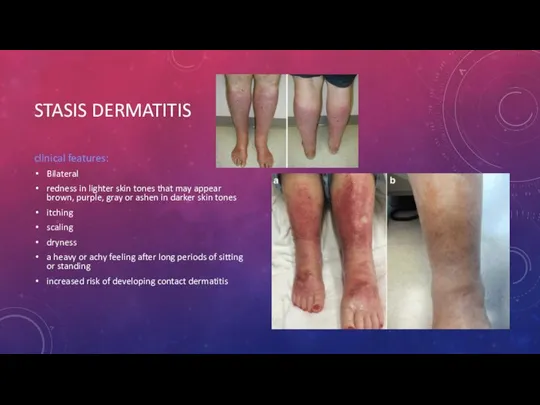
- 10. STASIS DERMATITIS clinical features: Bilateral redness in lighter skin tones that may appear brown, purple, gray
- 11. STASIS DERMATITIS Treatment compression stockings diuretics elevating legs above the heart for red or darker-colored, itchy
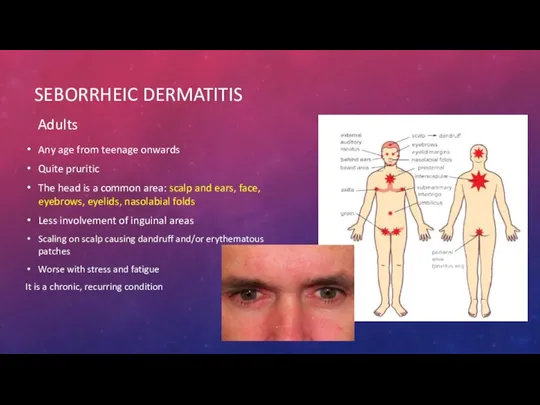
- 12. SEBORRHEIC DERMATITIS Adults Any age from teenage onwards Quite pruritic The head is a common area:
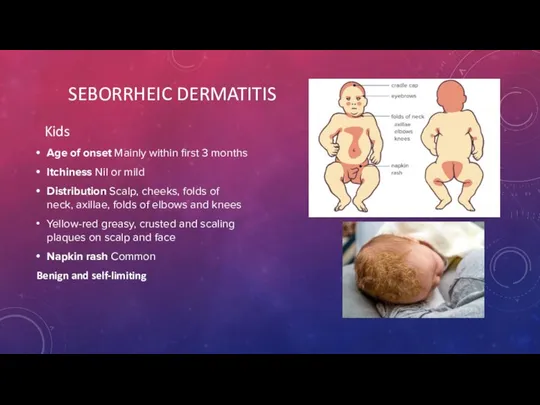
- 13. Kids Age of onset Mainly within first 3 months Itchiness Nil or mild Distribution Scalp, cheeks,
- 14. SEBORRHEIC DERMATITIS Management Likely to resolve on it’s own Soft baby brush and some baby oil
- 15. CELLULITIS Cellulitis is a common bacterial infection The most common bacteria causing cellulitis are Streptococcus pyogenes
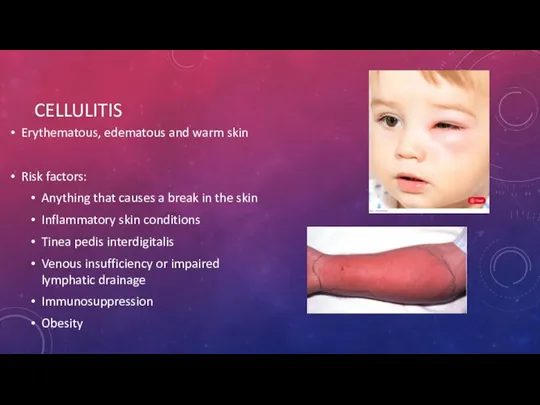
- 16. CELLULITIS Erythematous, edematous and warm skin Risk factors: Anything that causes a break in the skin
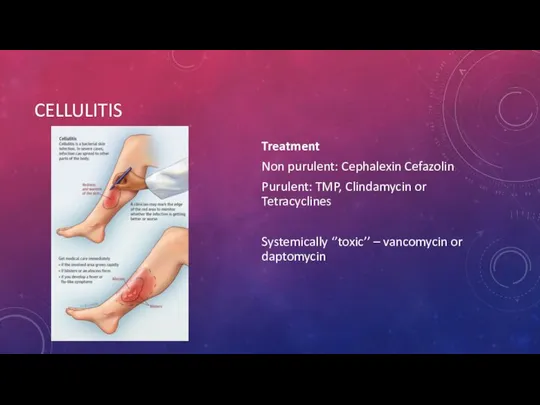
- 17. CELLULITIS Treatment Non purulent: Cephalexin Cefazolin Purulent: TMP, Clindamycin or Tetracyclines Systemically ‘’toxic’’ – vancomycin or
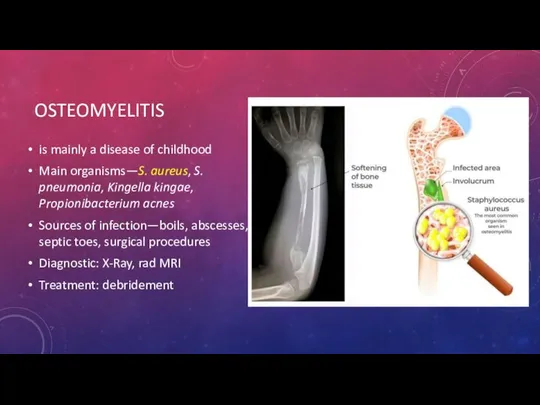
- 18. OSTEOMYELITIS is mainly a disease of childhood Main organisms—S. aureus, S. pneumonia, Kingella kingae, Propionibacterium acnes
- 19. GAS GANGRENE necrotising soft tissue infection can involve skin and subcutaneous fat, fascia and muscle caused
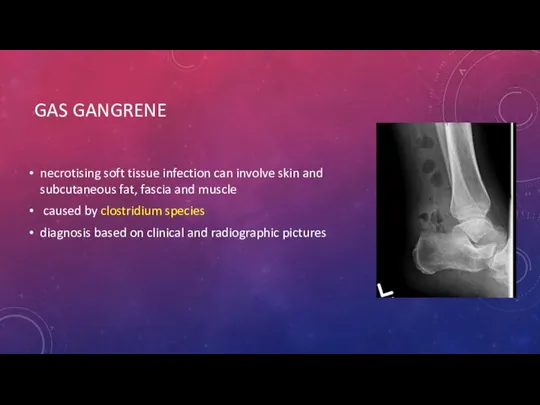
- 20. GAS GANGRENE Clinical features sweet smelling odor edema, discoloration, ecchymosis blebs and hemorrhagic bullae ''dishwater pus''
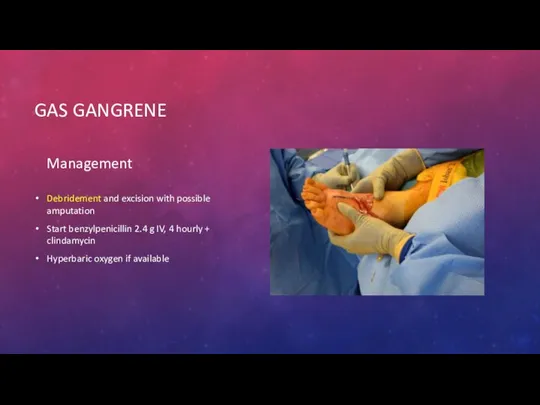
- 21. GAS GANGRENE Management Debridement and excision with possible amputation Start benzylpenicillin 2.4 g IV, 4 hourly
- 22. NECROTIZING FASCIITIS Necrotising fasciitis is a very serious bacterial infection of the soft tissue and fascia
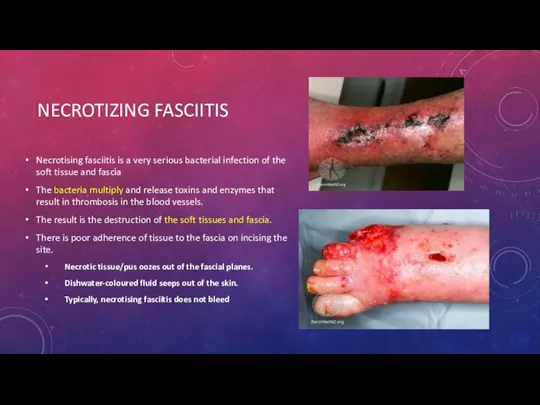
- 23. NECROTIZING FASCIITIS Treatment Immediate surgical debridement The third generation cephalosporins + Clinda
- 24. IMPETIGO caused by Streptococcus pyogenes or Staphylococcus aureus kids honey crusted lesions on the face Treatment
- 25. ERYSIPELAS is a superficial form of cellulitis involving the face – butterfly appearing rush an associated
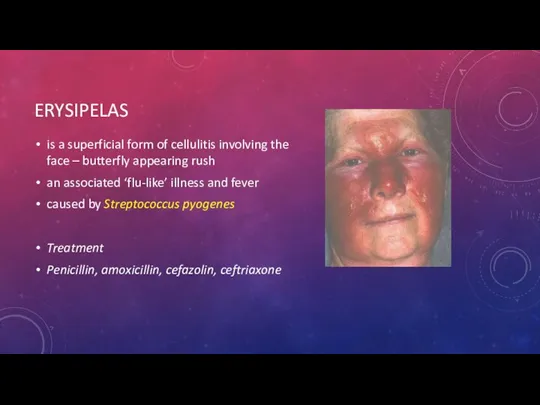
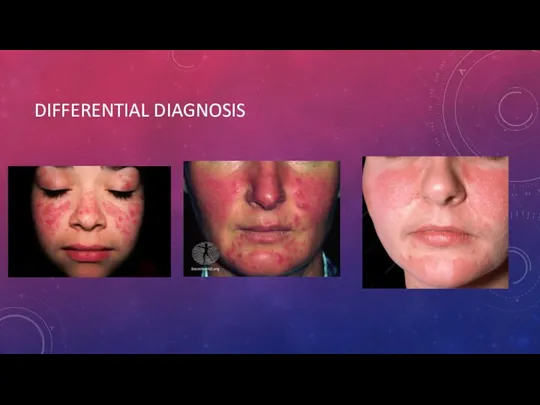
- 26. DIFFERENTIAL DIAGNOSIS
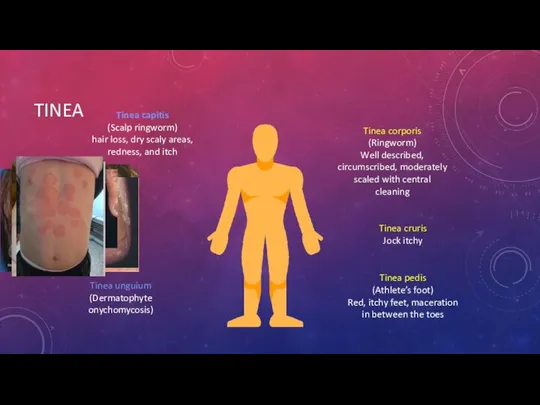
- 27. TINEA Tinea pedis (Athlete’s foot) Red, itchy feet, maceration in between the toes Tinea cruris Jock
- 28. CELLULITIS Deep dermis and subcutaneous adipose tissue Indolent onset Localised symptoms Non-purulent or purulent Non-purulent: Beta-hemolytic
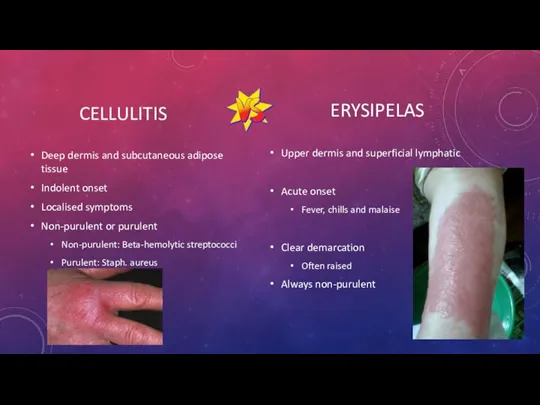
- 32. Скачать презентацию






 Патофизиология и диагностика вегетативных и коматозных состояний
Патофизиология и диагностика вегетативных и коматозных состояний Дентикюр. Забота о зубах и деснах
Дентикюр. Забота о зубах и деснах Коронaвирус Covid-19
Коронaвирус Covid-19 Врожденная краснуха
Врожденная краснуха Стерильные лекарственные формы, изготавливаемые в условиях аптеки и промышленного производства
Стерильные лекарственные формы, изготавливаемые в условиях аптеки и промышленного производства Periconception endogenous and exogenous maternal sex steroid hormones and risk of asthma and allergy in offspring
Periconception endogenous and exogenous maternal sex steroid hormones and risk of asthma and allergy in offspring История развития донорства
История развития донорства Алгоритм работы при отработке заболевших Сovid-19
Алгоритм работы при отработке заболевших Сovid-19 Психомоторное развитие на первом году жизни
Психомоторное развитие на первом году жизни Операции на сухожилиях, костях, суставах, мягких тканях
Операции на сухожилиях, костях, суставах, мягких тканях Мама-Судьба
Мама-Судьба Аспекты эндокринологии в практике кардиолога
Аспекты эндокринологии в практике кардиолога Халықтың табиғи қозғалысын бағалау
Халықтың табиғи қозғалысын бағалау Самоменеджмент пациентов и его роль в ПУЗ
Самоменеджмент пациентов и его роль в ПУЗ Новые методы в санитарно-гигиенических исследованиях
Новые методы в санитарно-гигиенических исследованиях Первая помощь и правила иммобилизации при переломах черепа, позвоночника и таза
Первая помощь и правила иммобилизации при переломах черепа, позвоночника и таза Точечный массаж
Точечный массаж Физиология психической деятельности. Лекция 12
Физиология психической деятельности. Лекция 12 Тромбофилия. Заболевания, связанные с генетическими дефектами
Тромбофилия. Заболевания, связанные с генетическими дефектами Курс по восстановлению и уходу за волосами
Курс по восстановлению и уходу за волосами Основы патологии
Основы патологии Общая артрология
Общая артрология Нейропсихологическая диагностика детей раннего возраста. Зачем нужна нейропсихологическая диагностика детям в 2 года?
Нейропсихологическая диагностика детей раннего возраста. Зачем нужна нейропсихологическая диагностика детям в 2 года? Психическое развитие в младенчестве
Психическое развитие в младенчестве Энурез у детей
Энурез у детей Caries (clinical application)
Caries (clinical application) Школьный возраст
Школьный возраст «Өзін-өзі тану» рухани-адамгершілік білім бағдарламасының психологиялық-педагогикалық негіздері
«Өзін-өзі тану» рухани-адамгершілік білім бағдарламасының психологиялық-педагогикалық негіздері