Содержание
- 2. Background: Diabetes has long been associated with maternal and perinatal morbidity and mortality. Before the discovery
- 3. Pathophysiology: It is necessary to understand the physiology of fetal glucose control to appreciate the causes
- 4. Glucose and amino acids traverse the placental membrane. On the other hand, insulin is unable to
- 5. Fetal congenital malformations are most common when maternal glucose control has been poor during the first
- 6. Fetal macrosomia Quality of fetal growth is determined by plotting birthweight against gestational age on standard
- 7. Pulmonary disease These infants are at an increased risk of respiratory distress syndrome and may present
- 8. Metabolic and electrolyte abnormalities Hypoglycemia may present within the first few hours of life, with such
- 9. Cardiovascular anomalies Cardiomyopathy with intraventricular hypertrophy and outflow tract obstruction may occur in as many as
- 10. Congenital malformations Central nervous malformations are 16 times more likely in these infants. In particular, the
- 11. Causes: HbA1C levels Complications caused by maternal hyperglycemia during pregnancy are reflected by elevated HbA1C levels,
- 12. Lab Studies: Complete blood cell count Polycythemia, commonly defined as a central hematocrit higher than 65%
- 13. Glucose concentration (serum or whole-blood) Seizures, coma, and long-term brain damage may occur if neonatal hypoglycemia
- 14. Procedures: Nasal or endotracheal continuous positive airway pressure, endotracheal intubation, and mechanical ventilation Nasal continuous positive
- 15. Medical Care: Communication between members of the perinatal team is of crucial importance to identify infants
- 16. Guidelines based on glucose level Level less than 36 mg/dL (2 mmol/L): Close surveillance of glucose
- 17. Immediate intravenous therapy with 2-mL/kg infusion of dextrose 10% (D10 provides 100 mg/mL of dextrose, starting
- 18. Electrolyte management Hypocalcemia and hypomagnesemia may complicate the clinical course. Because low serum calcium levels cannot
- 19. Respiratory management Pulmonary management is tailored to the individual infant's signs and symptoms. Increased ambient oxygen
- 20. Complications: All risks are directly proportional to the degree of maternal hyperglycemia in utero. Thompson and
- 21. Complications: All risks are directly proportional to the degree of maternal hyperglycemia in utero. Thompson and
- 23. Скачать презентацию
Background: Diabetes has long been associated with maternal and perinatal morbidity
Background: Diabetes has long been associated with maternal and perinatal morbidity
Fetal and neonatal mortality rates were as high as 65% before the development of specialized maternal, fetal, and neonatal care. Since then, infants of diabetic mothers (IDMs) have experienced a nearly 30-fold decrease in morbidity and mortality rates. Today, 3-10% of pregnancies are affected by abnormal glucose regulation and control. Of these, 80% are related to abnormal glucose control of pregnancy or gestational diabetes mellitus.
Infants born to mothers with glucose intolerance are at an increased risk of morbidity and mortality related to the following:
Respiratory distress
Growth abnormalities (large for gestational age [LGA], small for gestational age [SGA])
Hyperviscosity secondary to polycythemia
Hypoglycemia
Congenital malformations
Hypocalcemia, hypomagnesemia, and iron abnormalities
These infants are likely to be born by cesarean section for many reasons, among which are such complications as shoulder dystocia with potential brachial plexus injury related to the infant's large size. It is important for these mothers to be monitored closely throughout pregnancy. If optimal care is provided, the perinatal mortality rate, excluding congenital malformations, is nearly equivalent to that observed in normal pregnancies.
Pathophysiology: It is necessary to understand the physiology of fetal glucose
Pathophysiology: It is necessary to understand the physiology of fetal glucose
Increased insulin levels stimulate glycogen deposition and decrease hepatic glucose production. It is not uncommon to recognize a decreased need for insulin in the diabetic patient in early pregnancy. Furthermore, amino acids decrease and fatty acid triglycerides and ketones both increase with increased fatty acid deposition. As a result, increased protein catabolism and accelerated renal gluconeogenesis occurs.
As pregnancy progresses, human placental lactogen is released by the syncytiotrophoblast, leading to lipolysis in the mother. The subsequent release of glycerol and fatty acids reduces maternal use of glucose and amino acid, thus preserving these substrates for the fetus.
The release of increasing amounts of contrainsulin factors as placental growth continues causes up to a 30% increase in maternal insulin needs as pregnancy progresses. Mothers with previous borderline glucose control, obesity, or frank diabetes may require initiation of or increase in their insulin requirements to maintain glucose homeostasis.
Glucose and amino acids traverse the placental membrane. On the other
Glucose and amino acids traverse the placental membrane. On the other
The fetus is subjected to high levels of glucose during times of maternal hyperglycemia. Before 20 weeks' gestation, fetal islet cells are incapable of responding, subjecting the fetus to unchecked hyperglycemia and decreased fetal growth. Poor growth is especially noted in mothers with diabetic vascular disease. After 20 weeks' gestation, the fetus responds to hyperglycemia with pancreatic beta-cell hyperplasia and increased insulin levels.
Proinsulin (insulinlike growth factor-1 [IGF-1], insulinlike growth factor–binding protein-3 [IGFBP-3]) also acts as a growth factor that, in the presence of increased fetal amino acids, results in fetal macrosomia. Fetal growth acceleration can be noted on ultrasound by 24 weeks' gestation, especially with fluctuating maternal glucose levels. The combination of hyperglycemia and insulin increases fat and glycogen stores, resulting in weight increases marked by hepatosplenomegaly and cardiomegaly without an increase in head circumference.
Chronic fetal hyperglycemia and hyperinsulinemia increase the fetal basal metabolic rate and oxygen consumption, leading to a relative hypoxic state. The fetus responds by increasing oxygen-carrying capacity through increased erythropoieten production, possibly leading to polycythemia. The fetus redistributes iron from developing organs, including the heart and brain, to support this expanded blood mass, leaving these organs iron deficient and with possible long-term functional consequences.
Prior to birth, elevated insulin levels may inhibit the maturational effect of cortisol on the lung, including the production of surfactant from type 2 pneumocytes. This puts the fetus at risk for developing respiratory distress syndrome after birth
Fetal congenital malformations are most common when maternal glucose control has
Fetal congenital malformations are most common when maternal glucose control has
Fetal macrosomia
Quality of fetal growth is determined by plotting birthweight against
Fetal macrosomia
Quality of fetal growth is determined by plotting birthweight against
LGA infants should be routinely screened for potential hypoglycemia. This is particularly important if the mother has received large amounts of glucose-containing fluids during her labor.
Fetal macrosomia is observed in 26% of IDMs and in 10% (by definition) of infants of nondiabetic women. While most common as a consequence of maternal hyperglycemia and hyperinsulinemia, fetal macrosomia may occur despite maternal euglycemia.
Pulmonary disease
These infants are at an increased risk of respiratory distress
Pulmonary disease
These infants are at an increased risk of respiratory distress
Initially, the differential diagnosis might include transient tachypnea of the newborn, respiratory distress syndrome, pneumonia, or persistent pulmonary hypertension.
Metabolic and electrolyte abnormalities
Hypoglycemia may present within the first few
Metabolic and electrolyte abnormalities
Hypoglycemia may present within the first few
Hypoglycemia is caused by hyperinsulinemia due to hyperplasia of fetal pancreatic beta cells consequent to maternal-fetal hyperglycemia. Because the continuous supply of glucose is stopped after birth, the neonate develops hypoglycemia because of insufficient substrate. Stimulation of fetal insulin release by maternal hyperglycemia during labor significantly increases the risk of early hypoglycemia in these infants. Perinatal stress may have an additive effect on hypoglycemia due to catecholamine release and glycogen depletion.
The overall risk of hypoglycemia is anywhere from 25-40%, with LGA and preterm infants at highest risk.
Hypocalcemia or hypomagnesemia also may be apparent in the first few hours after birth; symptoms may include jitteriness or seizure activity. Hypocalcemia (levels <7 mg/dL) is believed to be associated with a delay in parathyroid hormone synthesis after birth.
Sixty-five percent of all IDMs demonstrate abnormalities of iron metabolism at birth. Iron deficiency increases an infant's risk for neurodevelopmental abnormalities. Iron is redistributed to the iron-deficient tissues after birth, as the RBC mass is postnatally broken down.
Cardiovascular anomalies
Cardiomyopathy with intraventricular hypertrophy and outflow tract obstruction may occur
Cardiovascular anomalies
Cardiomyopathy with intraventricular hypertrophy and outflow tract obstruction may occur
These infants also are at an increased risk of congenital heart defects, including (most commonly) ventricular septal defect (VSD) and transposition of the great arteries (TGA).
Congenital malformations
Central nervous malformations are 16 times more likely in these
Congenital malformations
Central nervous malformations are 16 times more likely in these
Renal (eg, hydronephrosis, renal agenesis, ureteral duplication), ear, cardiovascular (eg, single umbilical artery, VSDs, atrial septal defects, TGA, coarctation of the aorta, cardiomegaly), and gastrointestinal (eg, duodenal or anorectal atresia, small left colon syndrome) anomalies are more frequent in these infants
Causes:
HbA1C levels
Complications caused by maternal hyperglycemia during pregnancy are reflected
Causes:
HbA1C levels
Complications caused by maternal hyperglycemia during pregnancy are reflected
Because HbA1C is a direct measure of glucose control in the mother, higher levels are predictive of increased risks for congenital complications. Thus, the incidence of complications has been reported as 3.4% with HbA1C levels lower than 8.5% and 22.4% with levels higher than 8.5%.
There is speculation that birth defects in IDMs may be related to reduced arachidonic acid and myoinositol levels and elevated sorbitol and trace metal levels in the fetus.
Others speculate about the role of excess oxygen radicals and hydroperoxides in the mitochondria of susceptible fetal tissues because these prostacyclin inhibitors may cause disruption in the vascularization of developing tissues.
A past history of LGA infants, diabetes, stillbirth, hypertension, gestational diabetes, obesity, or glycosuria, or a current history of excessive weight gain in the present pregnancy or low socioeconomic class place the mother at an increased risk of poor glucose control during pregnancy and increase her risk of delivering an infant with subsequent complications.
Lab Studies:
Complete blood cell count
Polycythemia, commonly defined as a central
Lab Studies:
Complete blood cell count
Polycythemia, commonly defined as a central
Maternal-fetal hyperglycemia is a strong stimulus for fetal erythropoietin production and subsequent increase in fetal hemoglobin concentration secondary to chronic in utero hypoxia, which can be associated with the infant of a diabetic mother. Fetal hyperviscosity, intravascular sludging, regional ischemia, and hypoxemia are all potential complications. Thrombocytopenia may occur because of impaired thrombopoiesis due to "crowding-out" of thrombocytes by the excess of erythroid precursors in the bone marrow.
Glucose concentration (serum or whole-blood)
Seizures, coma, and long-term brain damage may
Glucose concentration (serum or whole-blood)
Seizures, coma, and long-term brain damage may
Most centers recognize levels lower than 20-40 mg/dL within the first 24 hours after birth as abnormal, but the precise level remains controversial. A policy to screen IDMs for hypoglycemia should be in place in every hospital. A recent suggestion of operational thresholds was proposed by Cornblath et al. Their suggestion in an infant with compromised metabolic adaptation (ie, IDMs) should include blood glucose measurements (1) as soon as possible after birth, (2) within 2-3 hours after birth and before feeding, and (3) at any time abnormal clinical signs are observed.
Magnesium concentration (serum)
Hypomagnesemia is related to younger maternal age, severity of maternal diabetes, and prematurity. Neonatal magnesium levels are also related to maternal serum magnesium, neonatal calcium and phosphorus levels, and neonatal parathyroid function.
The clinical significance of low magnesium levels in these infants remains controversial and uncertain.
Calcium concentration (serum, ionized or total levels): Low serum calcium levels in IDMs are common. They are speculated to be caused by a functional hypoparathyroidism; however, their clinical relevance remains uncertain and controversial.
Bilirubin level (serum, total and unconjugated): Hyperbilirubinemia is notably more common than in the general population of neonates. Causative factors include prematurity, hepatic enzyme immaturity, polycythemia with hyperviscosity and "sludging," and reduced red blood cell half-life.
Arterial blood gas: Assessing oxygenation and ventilation is essential in infants with clinical evidence of respiratory distress. Although noninvasive methods (eg, transcutaneous oxygen and carbon dioxide electrodes, oximeters) have gained wide acceptance at many centers, comparison of results with those from arterial blood is intermittently required
Procedures:
Nasal or endotracheal continuous positive airway pressure, endotracheal intubation, and
Procedures:
Nasal or endotracheal continuous positive airway pressure, endotracheal intubation, and
Nasal continuous positive airway pressure (NCPAP) or endotracheal intubation with CPAP and/or intermittent mandatory or synchronized positive pressure ventilation (IMV, SIMV) may be employed for management of severe respiratory distress.
Common criteria for such interventions include inspired oxygen requirements (FiO2) of 60-100% to maintain arterial PO2 of 50-80 mm Hg, arterial PCO2 levels higher than 60-80 mm Hg or rising 10 or more mm Hg/h, and apnea. The specific criteria for using these modes of assisted ventilation may vary considerably among neonatologists or across institutions.
Indwelling vascular lines (peripheral, umbilical, or central)
Noninvasive blood gas monitoring using transcutaneous electrodes (PaO2 and PaCO2) and oximeters (O2% saturation) has greatly reduced the need for invasive indwelling catheters. However, indwelling lines often are needed early in the course of cardiorespiratory disease. In some instances, the need for continuous arterial blood pressure monitoring may warrant placement of a peripheral or umbilical arterial line. Once again, use of these invasive methods varies.
Placement of an umbilical venous or a central venous catheter often is employed when the infant requires hyperosmolar intravenous fluids or when peripheral access is limited or exhausted.
Medical Care:
Communication between members of the perinatal team is of
Medical Care:
Communication between members of the perinatal team is of
Hypoglycemic management
It is generally agreed that serum or whole blood glucose levels less than 20-40 mg/dL within the first 24 hours after birth are significantly low. Cornblath et al's recent suggestions for approach at treatment suggest that measurement of the blood glucose level should be determined, as follows:
As soon as possible after birth
Within 2-3 hours after birth and before feeding
At any time abnormal clinical signs are observed
Guidelines based on glucose level
Level less than 36 mg/dL (2
Guidelines based on glucose level
Level less than 36 mg/dL (2
Level less than 20-25 mg/dL (1.1-1.4 mmol/L): Intravenous glucose should be administered, with the target glucose level of more than 45 mg/dL (2.5 mmol/L). This goal of 45 mg/dL is accentuated as a margin of safety. Should the infant be significantly symptomatic with profound, recurrent, or persistent hyperinsulinemic hypoglycemia, then a goal of more than 60 mg/dL (3.3 mmol/L) may be more appropriate.
It is difficult to determine which infants require the highest dextrose administration to maintain euglycemia. The following suggestions represent a guideline for glucose administration to a hypoglycemic, clinically symptomatic, infant.
Immediate intravenous therapy with 2-mL/kg infusion of dextrose 10% (D10 provides
Immediate intravenous therapy with 2-mL/kg infusion of dextrose 10% (D10 provides
Maintenance of a continuous infusion of dextrose at an infusion rate of 6-8 mg/kg/min of dextrose is necessary once bolus therapy is complete. Failure to do so may result in rebound hypoglycemia as a result of heightened pancreatic insulin release triggered by the glucose infusion.
Frequent serum or whole blood glucose analyses are important to properly titrate the dextrose infusion. Should follow-up glucose levels remain less than 40 mg/dL, the dextrose infusion may be increased by 2 mg/kg/min until euglycemia is achieved.
If the infant requires a dextrose concentration more than D12.5 through a peripheral vein at 80-100 mL/kg/d, placement of a central venous catheter may be considered to avoid venous sclerosis. Continued enteral feedings hasten improvement in glucose control because of the presence of protein and fat in the formula.
Once the infant's glucose levels have been stable for 12 hours, intravenous glucose may be tapered by 1-2 mg/kg/min, depending on maintenance of preprandial glucose levels higher than 40 mg/dL.
Electrolyte management
Hypocalcemia and hypomagnesemia may complicate the clinical course.
Because
Electrolyte management
Hypocalcemia and hypomagnesemia may complicate the clinical course.
Because
In IDMs, calcium and magnesium levels are commonly measured within the first hours after birth. Ideally, ionized levels of these electrolytes should be obtained and employed to properly manage these electrolyte disturbances.
True symptomatic hypocalcemia is extremely rare in these infants. In most cases, symptoms interpreted to be caused by low calcium or magnesium levels are due to low glucose levels associated with perinatal asphyxia or associated with a variety of central nervous system problems.
When these low levels are treated, an infusion of 10% calcium gluconate at 2 mL/kg often is administered over 5 minutes (18 mg/kg of elemental calcium). This treatment has particular hazards because the hyperosmolal mixture may cause serious tissue necrosis and sclerosis; also, serious cardiac arrhythmias may occur during the infusion. It is routine in many centers to monitor the infant's ECG during infusion.
Respiratory management
Pulmonary management is tailored to the individual infant's signs
Respiratory management
Pulmonary management is tailored to the individual infant's signs
Increased ambient oxygen concentrations may be required to maintain oxygen saturations higher than 90%, transcutaneous oxygen tensions at 40-70 mm Hg, or arterial oxygen tensions at 50-90 mm Hg.
When an inspired oxygen concentration (FiO2) higher than 40% is required, the most important task is to determine a precise diagnosis of the cause for the hypoxemia. Principals of management, which are generally agreed on, are based on monitoring of blood levels of oxygen and carbon dioxide, as well as their maintenance within physiologic ranges using the least invasive techniques that are successful.
Complications:
All risks are directly proportional to the degree of maternal
Complications:
All risks are directly proportional to the degree of maternal
Thompson and associates found that tight control of euglycemia in the patient with gestational diabetes led to normal perinatal outcomes. When comparing good glucose control (mean plasma glucose level <120 mg/dL) with poor glucose control (mean plasma glucose level >140 mg/dL), the hyperglycemic group was found to have more preeclampsia, maternal urinary tract infections, premature deliveries, cesarean deliveries, macrosomia, respiratory distress, neonatal hypoglycemia, congenital malformations, and perinatal mortality.
Congenital anomalies: The overall risk is 8-15%, with 30-50% of perinatal fatalities related to major congenital malformations. Poor glycemic control early in pregnancy directly correlates with a higher incidence of congenital malformations.
Perinatal mortality
In the past, 10-30% of pregnancies terminated with sudden and unexplained stillbirth. This is believed to have been secondary to chronic fetal hypoxia with subsequent polycythemia and vascular sludging. A higher incidence was noted in pregnancies further complicated by maternal vascular disease.
A considerable proportion of perinatal problems are a consequence of fetal macrosomia. Macrosomia is associated with protracted labor, perinatal asphyxia, shoulder dystocia and brachial plexus injury, other skeletal and nerve injuries, and an elevated rate of operative deliveries.
Complications:
All risks are directly proportional to the degree of maternal
Complications:
All risks are directly proportional to the degree of maternal
Thompson and associates found that tight control of euglycemia in the patient with gestational diabetes led to normal perinatal outcomes. When comparing good glucose control (mean plasma glucose level <120 mg/dL) with poor glucose control (mean plasma glucose level >140 mg/dL), the hyperglycemic group was found to have more preeclampsia, maternal urinary tract infections, premature deliveries, cesarean deliveries, macrosomia, respiratory distress, neonatal hypoglycemia, congenital malformations, and perinatal mortality.
Congenital anomalies: The overall risk is 8-15%, with 30-50% of perinatal fatalities related to major congenital malformations. Poor glycemic control early in pregnancy directly correlates with a higher incidence of congenital malformations.
Perinatal mortality
In the past, 10-30% of pregnancies terminated with sudden and unexplained stillbirth. This is believed to have been secondary to chronic fetal hypoxia with subsequent polycythemia and vascular sludging. A higher incidence was noted in pregnancies further complicated by maternal vascular disease.
A considerable proportion of perinatal problems are a consequence of fetal macrosomia. Macrosomia is associated with protracted labor, perinatal asphyxia, shoulder dystocia and brachial plexus injury, other skeletal and nerve injuries, and an elevated rate of operative deliveries.

 Эндокринологическая аллея. Остановка Исторический музей
Эндокринологическая аллея. Остановка Исторический музей Репродуктивное здоровье – составляющая здоровья человека и общества
Репродуктивное здоровье – составляющая здоровья человека и общества Здоровый образ жизни – залог успешности специалиста
Здоровый образ жизни – залог успешности специалиста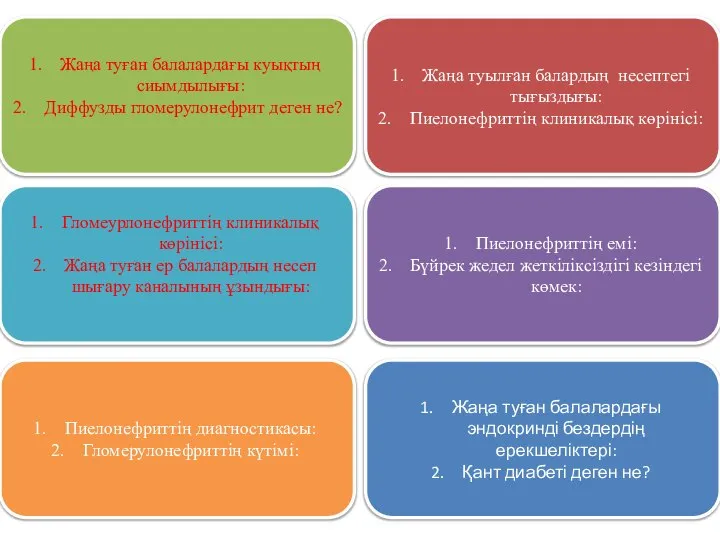 Педиатрия. Карточкалары
Педиатрия. Карточкалары Запальні захворювання органів малого тазу
Запальні захворювання органів малого тазу Туберкулез. Сепсис. Мерез
Туберкулез. Сепсис. Мерез Здоровая земля, здоровые растения и люди
Здоровая земля, здоровые растения и люди Ұрықтың туа біткен патологиясының алдын алу және ерте диагностикасы
Ұрықтың туа біткен патологиясының алдын алу және ерте диагностикасы Hendlings un zīdaiņa prasmes
Hendlings un zīdaiņa prasmes Усадка в стоматології
Усадка в стоматології Туа біткен жүрек ақаулары
Туа біткен жүрек ақаулары Организация ухода за больными кардиологического профиля
Организация ухода за больными кардиологического профиля Патофизиология нервной системы
Патофизиология нервной системы Солнце, воздух и вода. Закаливание
Солнце, воздух и вода. Закаливание Роль общения в развитии личности
Роль общения в развитии личности Геморрагические лихорадки
Геморрагические лихорадки Болезнь Фабри-Андерсона: клиническая картина, диагностика, клинические наблюдения
Болезнь Фабри-Андерсона: клиническая картина, диагностика, клинические наблюдения Угрожающие тромбозы у детей
Угрожающие тромбозы у детей Влияние эмоционального стресса на здоровье полости рта
Влияние эмоционального стресса на здоровье полости рта Криза 3-х років
Криза 3-х років Ұршық буынының және санның зақымдалуы
Ұршық буынының және санның зақымдалуы Антибиотики. Классификация антибиотиков
Антибиотики. Классификация антибиотиков 3 период родов
3 период родов Передача возбуждения в холинергических синапсах
Передача возбуждения в холинергических синапсах Клинический случай острого респираторного заболевания у ребенка с некетотической гиперглицинемией
Клинический случай острого респираторного заболевания у ребенка с некетотической гиперглицинемией Клинические рекомендации по диагностике, профилактике и лечению тромбоза у детей и подростков
Клинические рекомендации по диагностике, профилактике и лечению тромбоза у детей и подростков Причины травматизма в школьном возрасте и пути их предотвращения
Причины травматизма в школьном возрасте и пути их предотвращения Понятие, признаки и виды вспомогательных репродуктивных технологий. Нормативно-правовое регулирование
Понятие, признаки и виды вспомогательных репродуктивных технологий. Нормативно-правовое регулирование