Содержание
- 2. Definition of BO BO - condition develops due to the presence of obstacles to the outgoing
- 3. Types of BO By prevalence: 1. Local: tumor foreign body diseases with intrathoracic LAP 2. Diffuse:
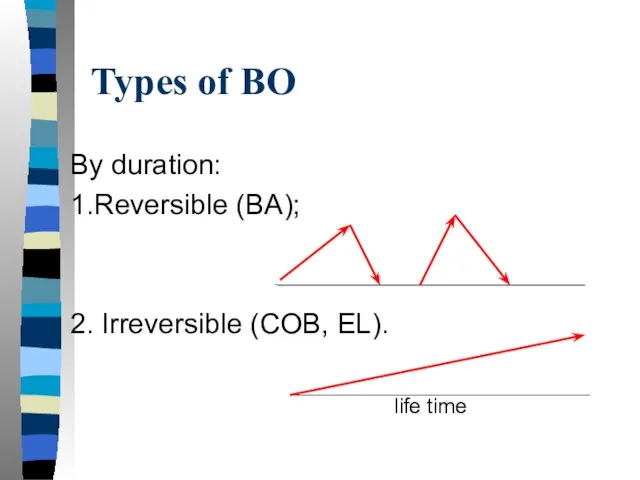
- 4. Types of BO By duration: 1.Reversible (BA); 2. Irreversible (COB, EL). life time
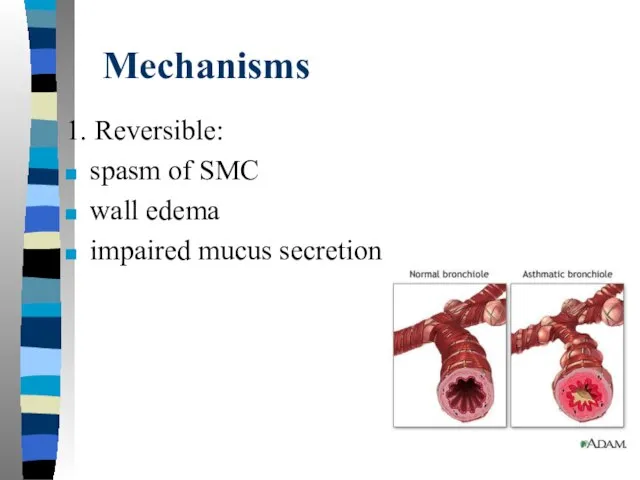
- 5. Mechanisms 1. Reversible: spasm of SMC wall edema impaired mucus secretion
- 6. 2. Irreversible: fibrosis of the wall pathological expiratory collapse of bronchioles (due to the lost of
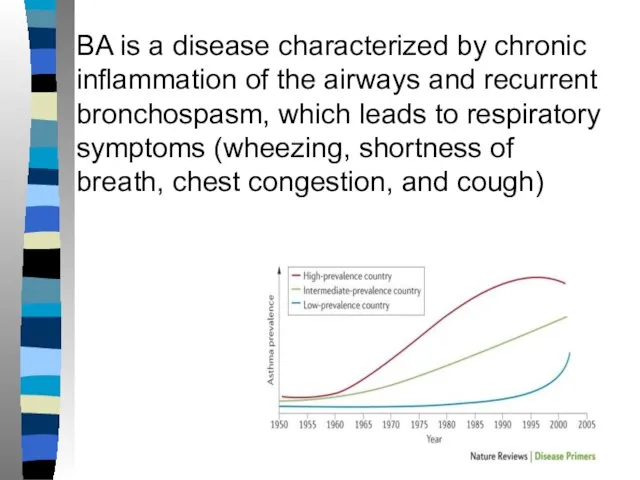
- 7. BA is a disease characterized by chronic inflammation of the airways and recurrent bronchospasm, which leads
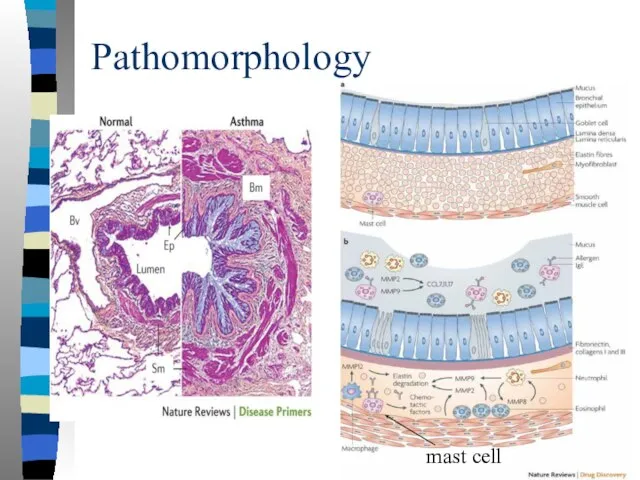
- 8. Pathomorphology mast cell
- 9. Inflammation in BA (AD) The development of AD is based on chronic inflammation in the airways.
- 10. Bronchial hyperreactivity BHR - the possibility of developing bronchospasm under the action of a stimulus that
- 11. Provoking factors of the bronchospasm Allergen triggers (have a protein structure) - cause sensitization (the appearance
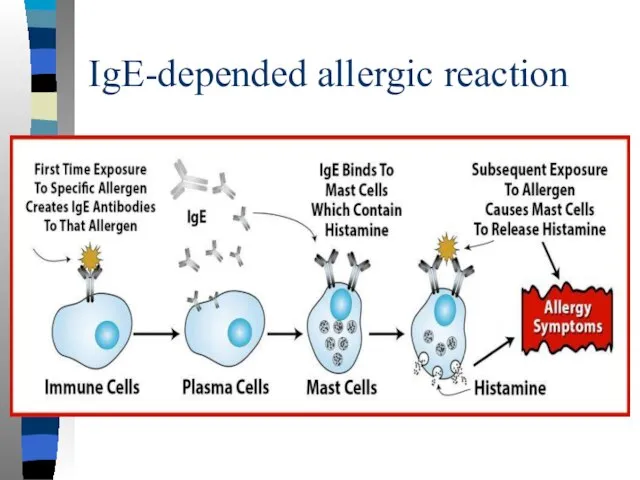
- 12. IgE-depended allergic reaction
- 13. Provoking factors of the bronchospasm Nonspecific triggers (non-allergenic) - provoke bronchospasm in the presence of bronchial
- 14. Symptoms Wheezing rales Feeling of chest congestion Dyspnea Unproductive cough (may be the dominant symptom !)
- 15. Choking appears with non-stopping severe attack of asthma, which is regarded as a severe exacerbation of
- 16. About asthma symptoms (it may help in diagnosis) Provocation (exercise, exposure to an allergen, cold air,
- 17. Patient examination Important ! signs of bronchial obstruction appear only at the time of an attack
- 18. History of life Childhood (early beginning) Occupational hazards (risk of occupational BA) Living conditions (mold, house
- 19. Tests Confirmation of variability of bronchial obstruction Peak expiratory flow (PEF) monitoring - peak flowmetry Spirometry
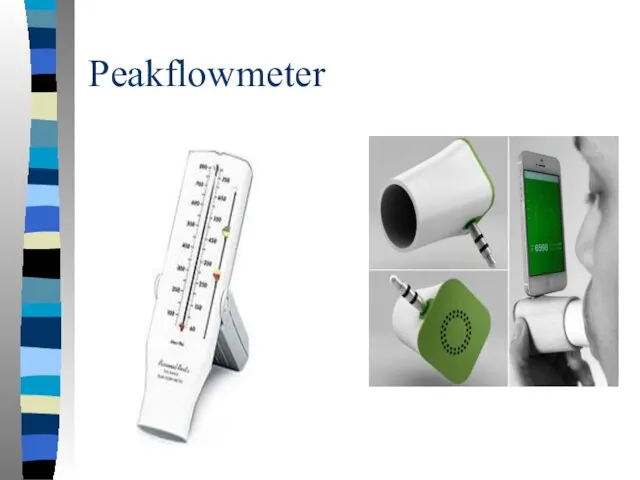
- 20. Peakflowmeter
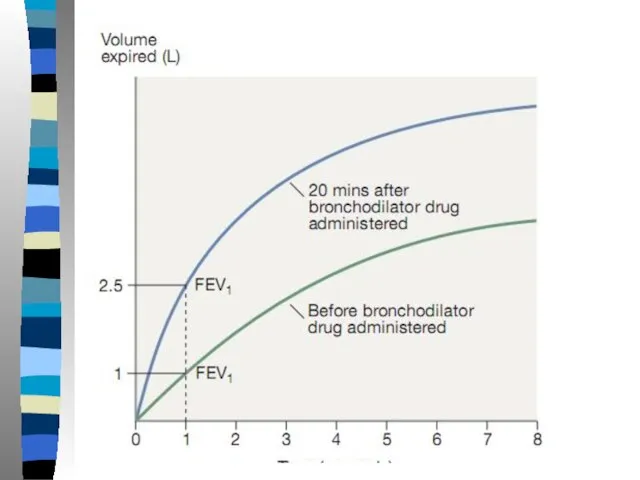
- 22. Criteria of bronchial obstruction variability Positive test with bronchodilator (assessed 15 min after 400 mcg salbutamol)
- 23. Положительный тест с бронхолитиком
- 24. Can a patient with asthma have normal spirometry and peak flow results?
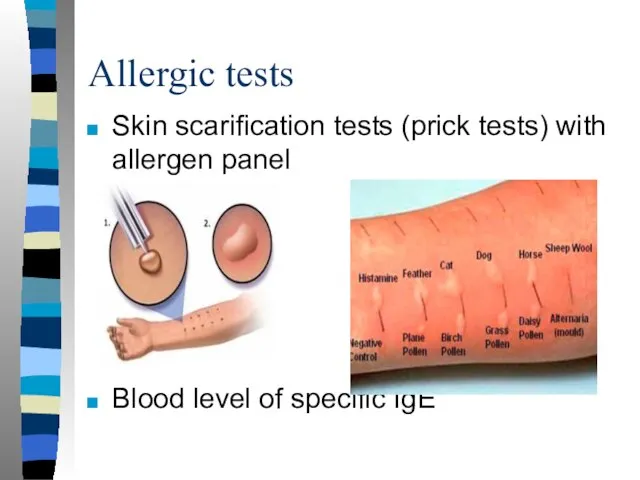
- 25. Allergic tests Skin scarification tests (prick tests) with allergen panel Blood level of specific IgE
- 26. Others Eosinophilia is detected in a small number of patients with AD In the analysis of
- 27. Treatment Long-term (in many patients lifelong) basic anti-inflammatory therapy with inhaled glucocorticoids (ICS) Use of short-acting
- 28. Chronic bronchitis CB - “smoker's cough” when other causes of cough are excluded (such as asthma,
- 29. Smokers usually do not seek medical help at the stage of CB, since the cough in
- 30. CB = Chronic productive cough + Long-term exposure to tobacco smoking + Other causes of chronic
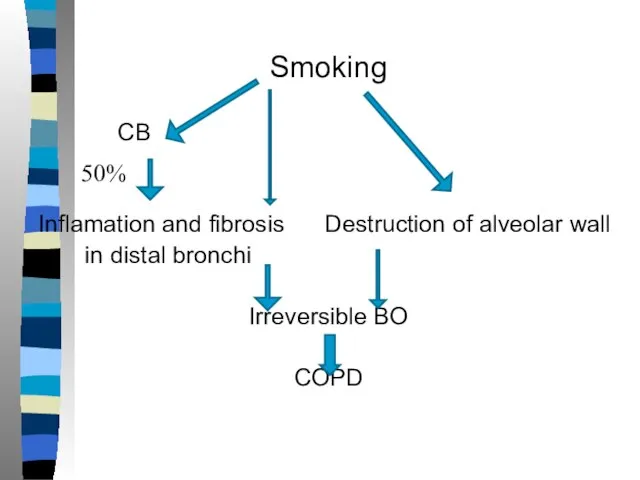
- 31. Smoking CB Inflamation and fibrosis Destruction of alveolar wall in distal bronchi Irreversible BO COPD 50%
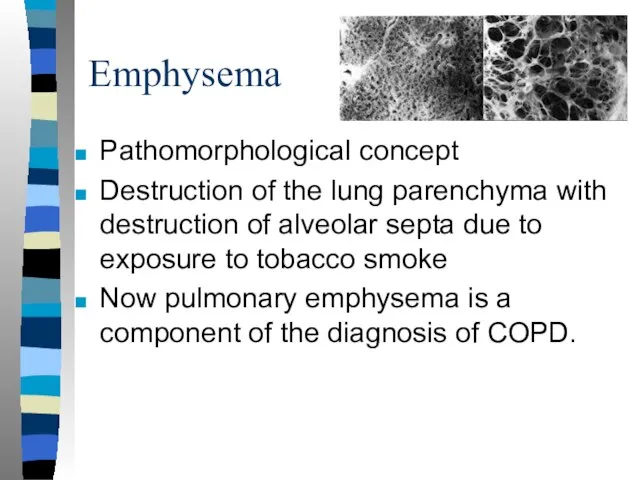
- 32. Emphysema Pathomorphological concept Destruction of the lung parenchyma with destruction of alveolar septa due to exposure
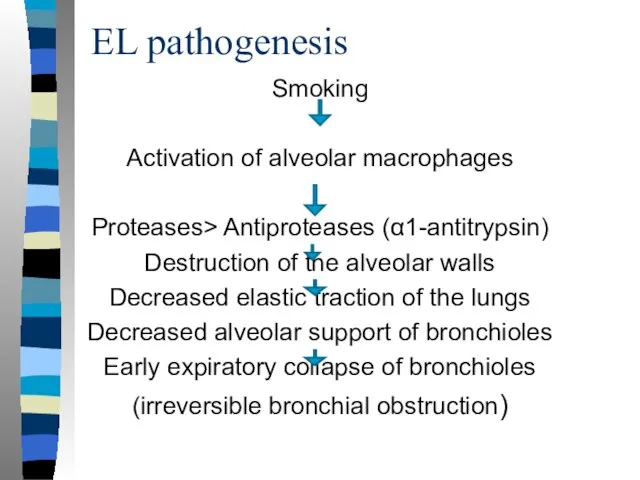
- 33. EL pathogenesis Smoking Activation of alveolar macrophages Proteases> Antiproteases (α1-antitrypsin) Destruction of the alveolar walls Decreased
- 34. COPD Chronic obstructive pulmonary disease is a disease with progressive irreversible bronchial obstruction that develops due
- 35. C(O)B EL COPD / ХОБЛ
- 36. Pathogenesis - Long-term smoking (smoking experience 20 packs / years or more, women may have less
- 37. With the development of bronchial obstruction (narrowing of the distal AW), the volumetric velocity of the
- 38. Air traps (dynamic hyperinflation) With bronchial obstruction, it is impossible to quickly breathe out a required
- 39. "Air traps" lead to an increase in the residual volume and a decrease in VC, disrupt
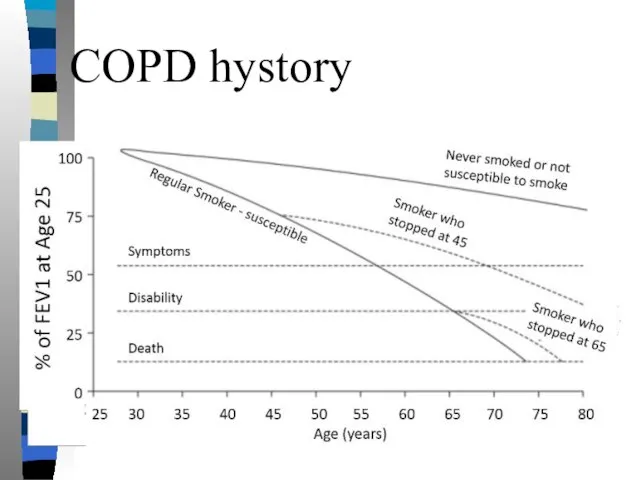
- 40. COPD hystory
- 41. Symptoms: complaints Shortness of breath on exertion, in the terminal stage - at minimal exertion and
- 42. Cough Most patients with COPD have a productive cough with little sputum. During periods of exacerbation,
- 43. Examination Central cyanosis in severe COPD due to arterial hypoxemia. Flushing of the neck and upper
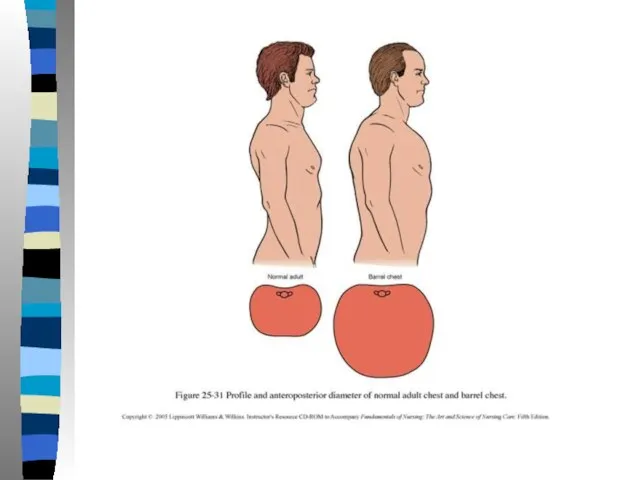
- 45. Chest examination Barrel chest in emphysematous COPD In severe patients with COPD, the involvement of additional
- 48. Palpation and percussion With emphysema and pulmonary hyperinflation, a boxed (hyperresonant) percussion sound is determined. Auscultation
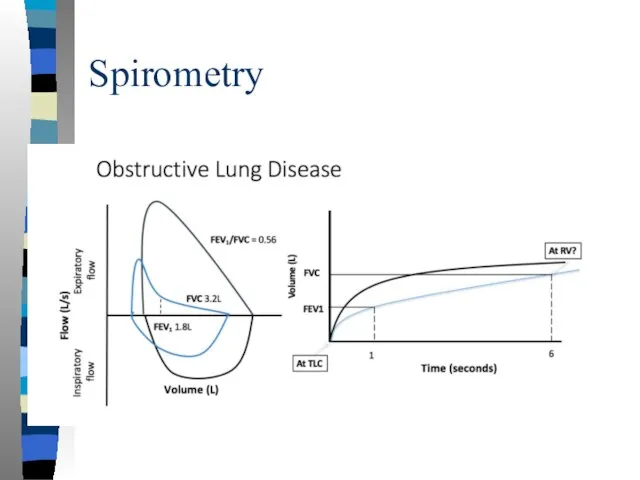
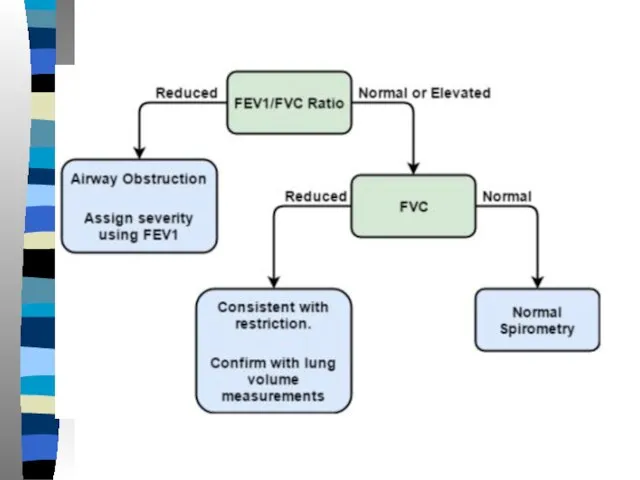
- 49. Spirometry
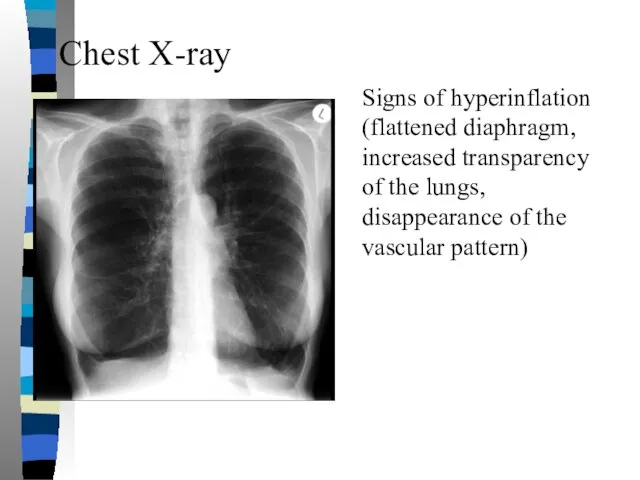
- 51. Chest X-ray Signs of hyperinflation (flattened diaphragm, increased transparency of the lungs, disappearance of the vascular
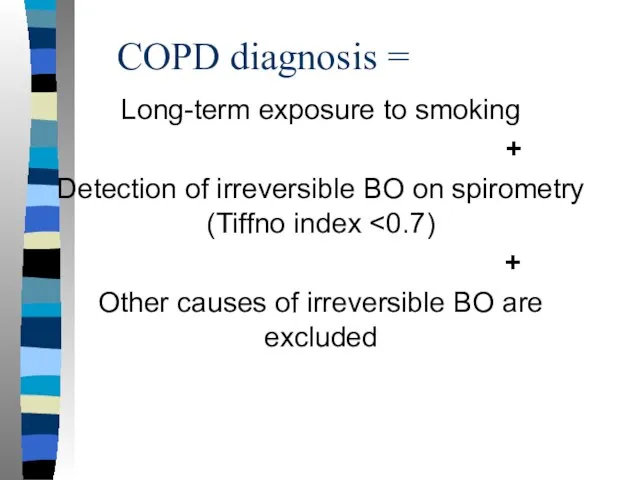
- 52. COPD diagnosis = Long-term exposure to smoking + Detection of irreversible BO on spirometry (Tiffno index
- 53. Treatment principles QUITING SMOKING is the only treatment that can slow the progression of COPD Bronchodilators
- 56. Скачать презентацию




 Срединные и боковые кисты и свищи шеи
Срединные и боковые кисты и свищи шеи Жеке тұлға
Жеке тұлға Вирус герпеса
Вирус герпеса Осложнение ГЭРБ, профилактика и лечение
Осложнение ГЭРБ, профилактика и лечение Характеристика некоторых форм первичных иммунодефицитов
Характеристика некоторых форм первичных иммунодефицитов Современные аспекты первичной профилактики сахарного диабета. Оказание доврачебной помощи при неотложных состояниях
Современные аспекты первичной профилактики сахарного диабета. Оказание доврачебной помощи при неотложных состояниях Рудометова
Рудометова ВИЧ-инфекция
ВИЧ-инфекция Forensic medicine
Forensic medicine Набор эффективных техник для работы с подсознанием - НЛП
Набор эффективных техник для работы с подсознанием - НЛП Технология разрешения внутрисемейных конфликтов
Технология разрешения внутрисемейных конфликтов Мифы и легенды о лошадином здоровье
Мифы и легенды о лошадином здоровье Аллергия. Типы гиперчувствительности
Аллергия. Типы гиперчувствительности Талдаудың дайындық кезеңі. Зиянды ағзалардың фитосанитарлық қауіп-қатерлерін талдау
Талдаудың дайындық кезеңі. Зиянды ағзалардың фитосанитарлық қауіп-қатерлерін талдау Нейросифилис. Клинические формы
Нейросифилис. Клинические формы Алкогольдің ұрыққа әсері
Алкогольдің ұрыққа әсері Вредные ингридиенты
Вредные ингридиенты Коронавирусная инфекция COVID-19
Коронавирусная инфекция COVID-19 Etiologiya. Аллергендер сырттан енетін экзогендік және ағзаның өзінде болатын эндогендік болып ажыратылады
Etiologiya. Аллергендер сырттан енетін экзогендік және ағзаның өзінде болатын эндогендік болып ажыратылады Слюна
Слюна Современные клинико-фармакологические подходы к лечению аллергических заболеваний
Современные клинико-фармакологические подходы к лечению аллергических заболеваний Формирование правильной осанки
Формирование правильной осанки Волшебное молоко
Волшебное молоко Балалардағы жіті аппендицит
Балалардағы жіті аппендицит Лечение аппендицита
Лечение аппендицита Основы фармакологии. Тематический план
Основы фармакологии. Тематический план Врожденная кишечная непроходимость
Врожденная кишечная непроходимость Правильное питание
Правильное питание