Содержание
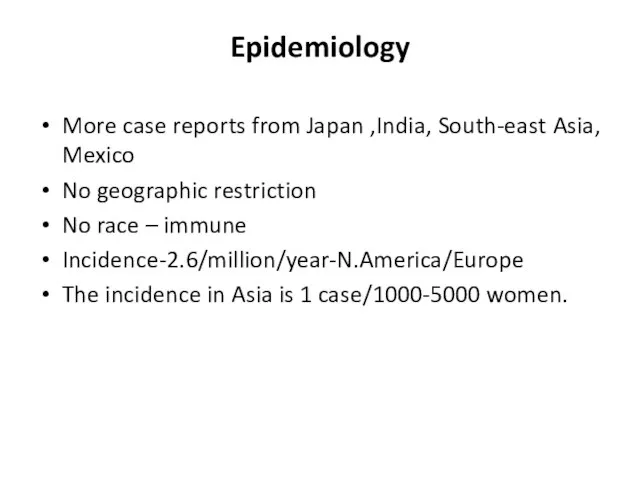
- 7. Epidemiology More case reports from Japan ,India, South-east Asia, Mexico No geographic restriction No race –
- 8. Age Mc-2nd & 3rd decade May range from infancy to middle age Indian studies-age 3- 50
- 9. Genetics Japan - HLA-B52 and B39 Mexican and Colombian patients - HLA-DRB1*1301 and HLA-DRB1*1602 India- HLA-
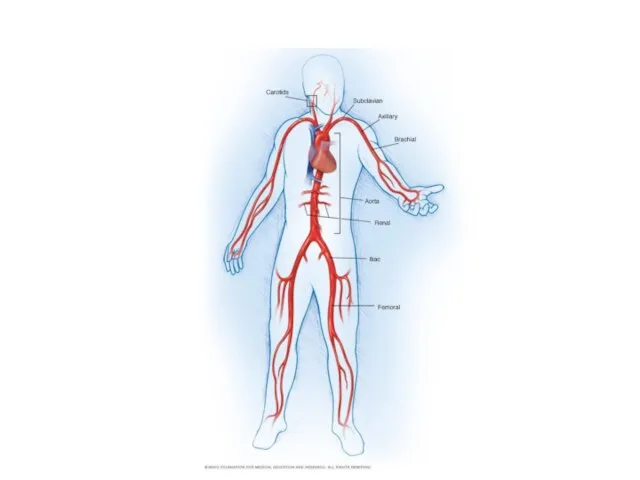
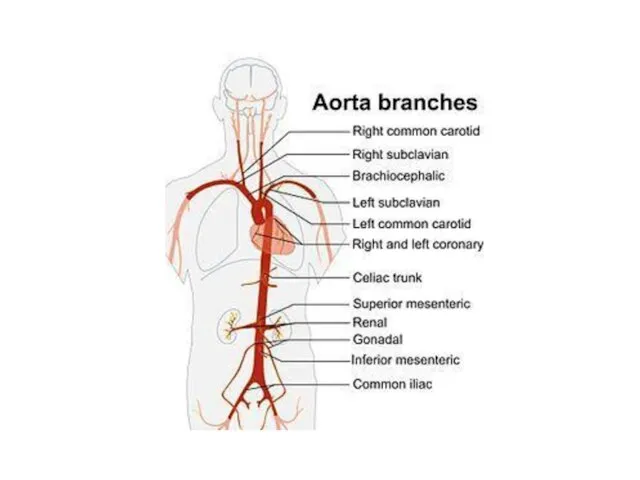
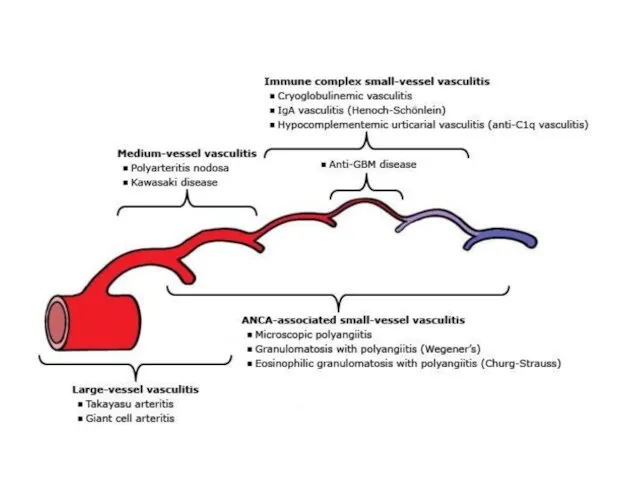
- 10. Histopathology Idiopathic inflammatory arteritis of elastic arteries resulting in occlusive/ ectatic changes Large vessels – Aorta
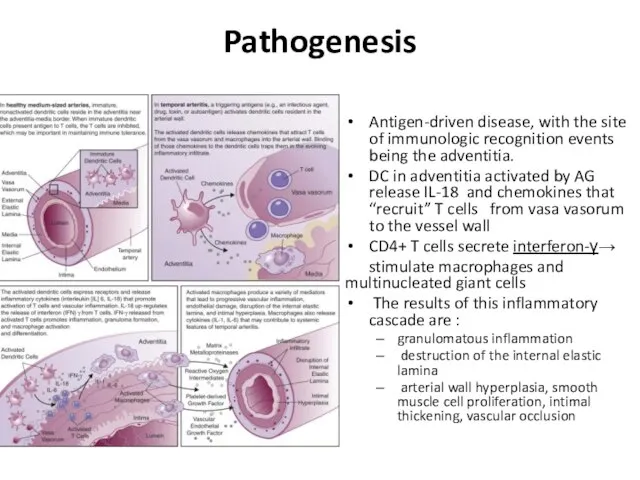
- 11. Pathogenesis Antigen-driven disease, with the site of immunologic recognition events being the adventitia. DC in adventitia
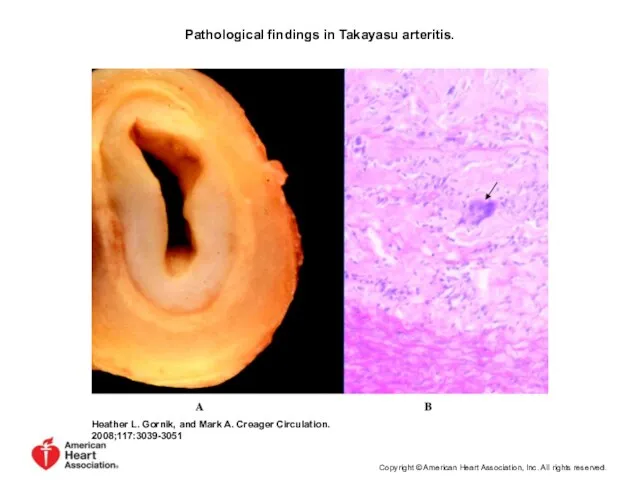
- 12. Pathological findings in Takayasu arteritis. Heather L. Gornik, and Mark A. Creager Circulation. 2008;117:3039-3051 Copyright ©
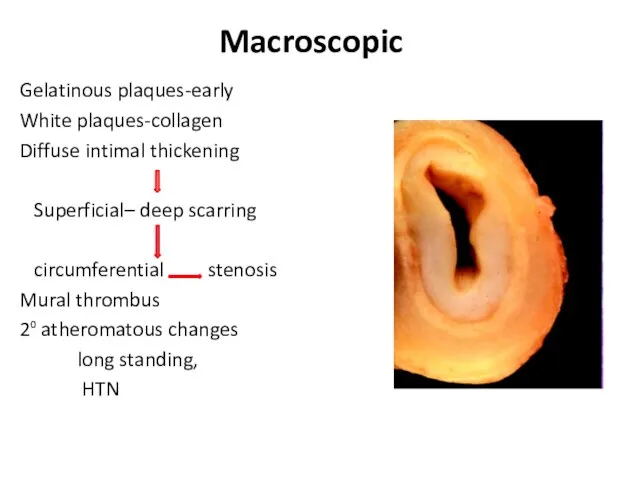
- 13. Macroscopic Gelatinous plaques-early White plaques-collagen Diffuse intimal thickening Superficial– deep scarring circumferential stenosis Mural thrombus 2⁰
- 14. Macroscopic Wall thickening, fibrosis, stenosis, thrombus formation →end organ ischemia More inflammation → destroys arterial media
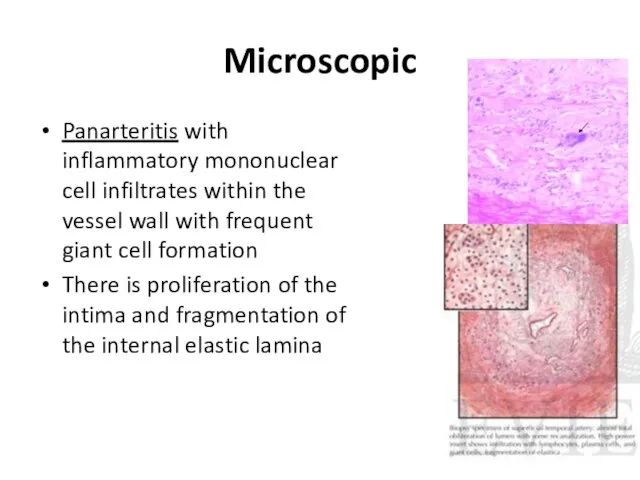
- 15. Microscopic Panarteritis with inflammatory mononuclear cell infiltrates within the vessel wall with frequent giant cell formation
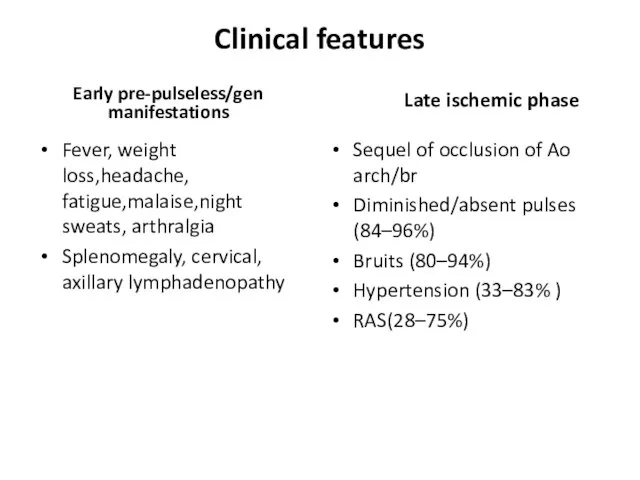
- 17. Clinical features Early pre-pulseless/gen manifestations Fever, weight loss,headache, fatigue,malaise,night sweats, arthralgia Splenomegaly, cervical, axillary lymphadenopathy Late
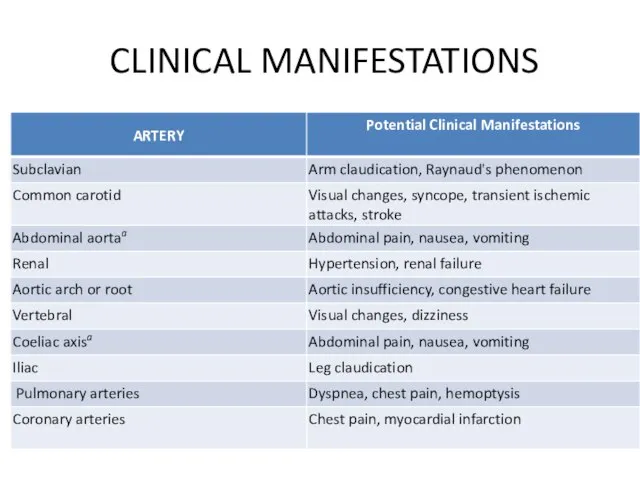
- 18. CLINICAL MANIFESTATIONS
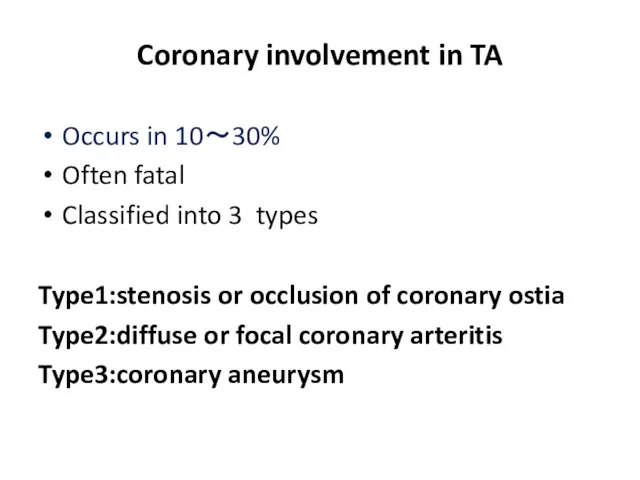
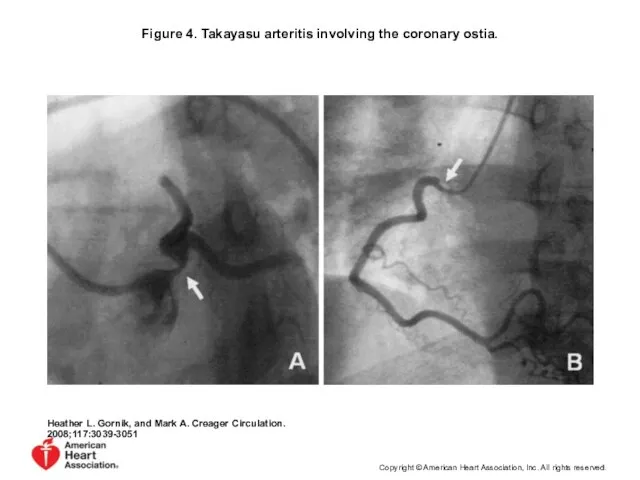
- 20. Coronary involvement in TA Occurs in 10~30% Often fatal Classified into 3 types Type1:stenosis or occlusion
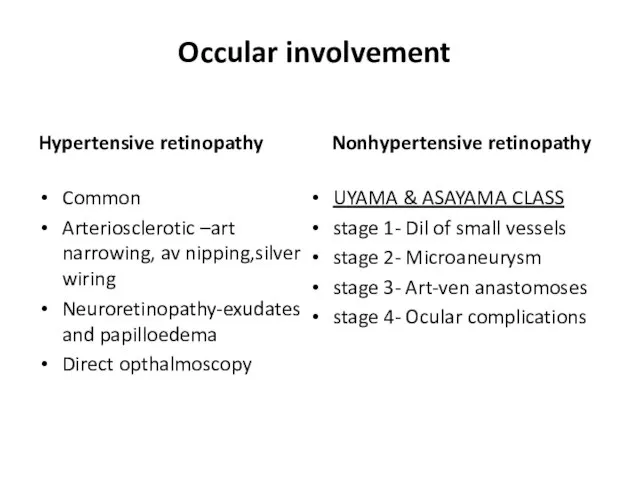
- 21. Occular involvement Hypertensive retinopathy Common Arteriosclerotic –art narrowing, av nipping,silver wiring Neuroretinopathy-exudates and papilloedema Direct opthalmoscopy
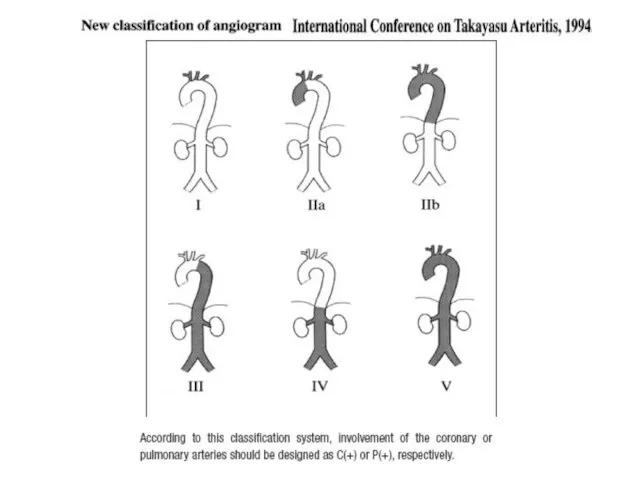
- 23. nee
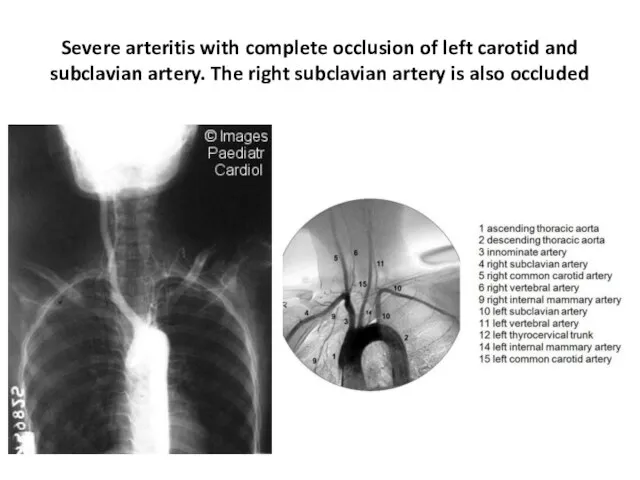
- 24. Severe arteritis with complete occlusion of left carotid and subclavian artery. The right subclavian artery is
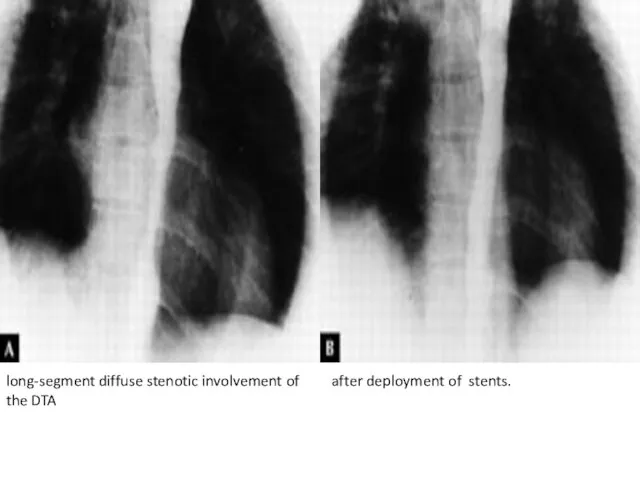
- 25. long-segment diffuse stenotic involvement of the DTA after deployment of stents.
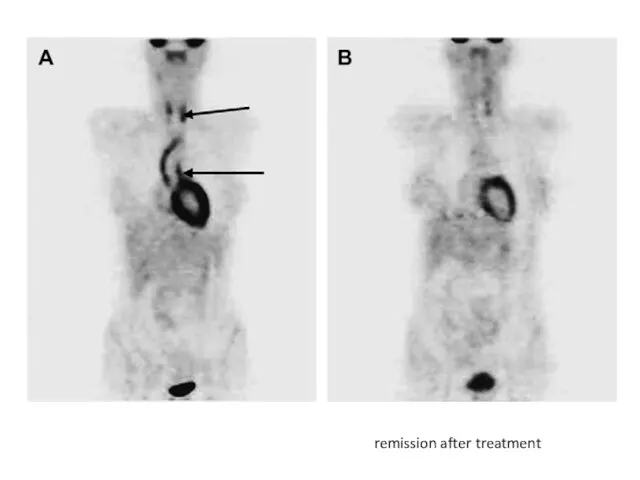
- 26. remission after treatment
- 27. Figure 4. Takayasu arteritis involving the coronary ostia. Heather L. Gornik, and Mark A. Creager Circulation.
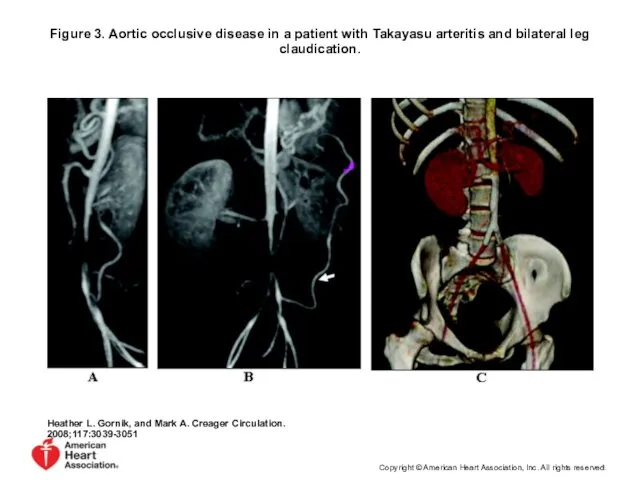
- 28. Figure 3. Aortic occlusive disease in a patient with Takayasu arteritis and bilateral leg claudication. Heather
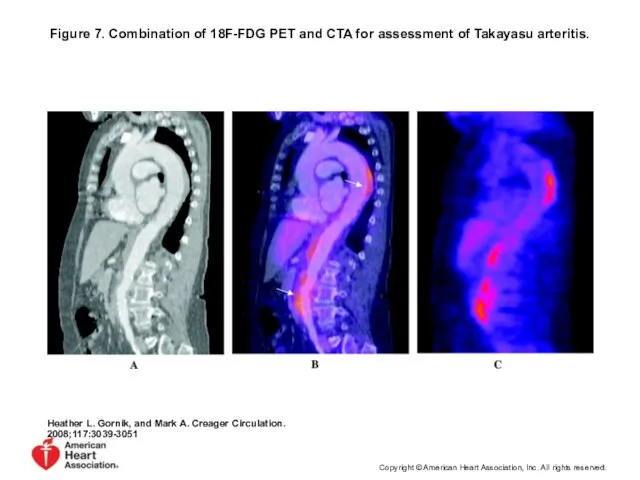
- 29. Figure 7. Combination of 18F-FDG PET and CTA for assessment of Takayasu arteritis. Heather L. Gornik,
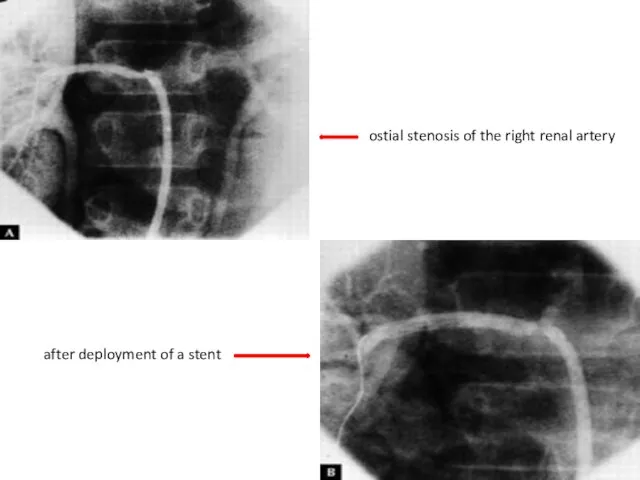
- 30. ostial stenosis of the right renal artery after deployment of a stent
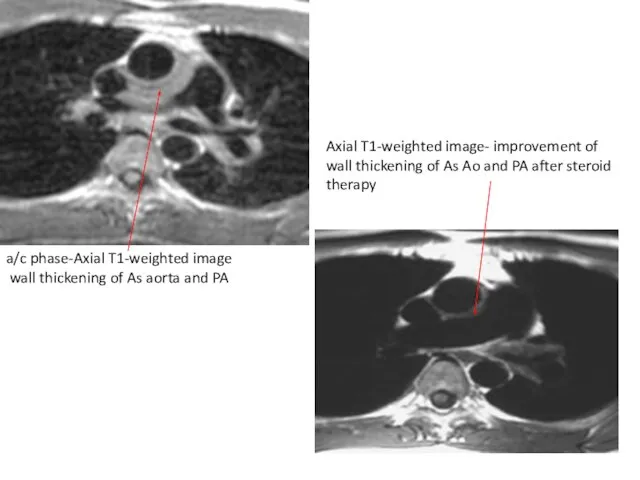
- 31. a/c phase-Axial T1-weighted image wall thickening of As aorta and PA Axial T1-weighted image- improvement of
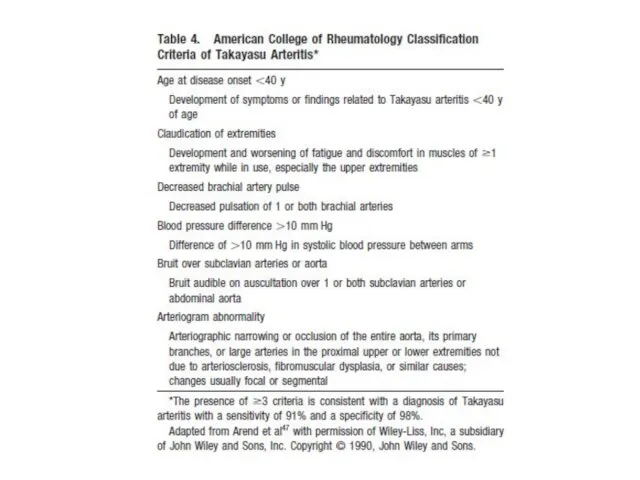
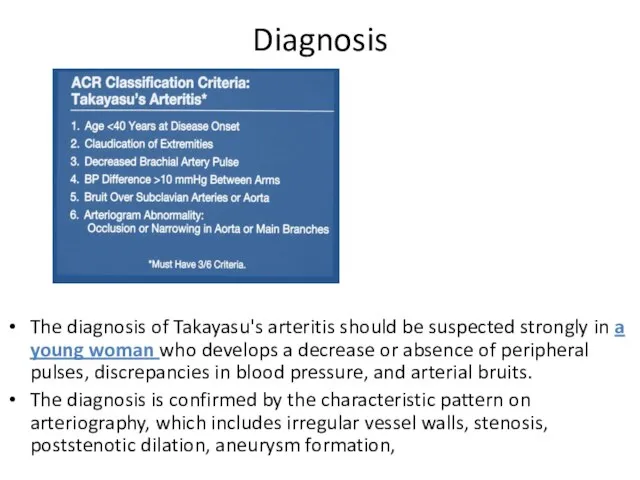
- 33. Diagnosis The diagnosis of Takayasu's arteritis should be suspected strongly in a young woman who develops
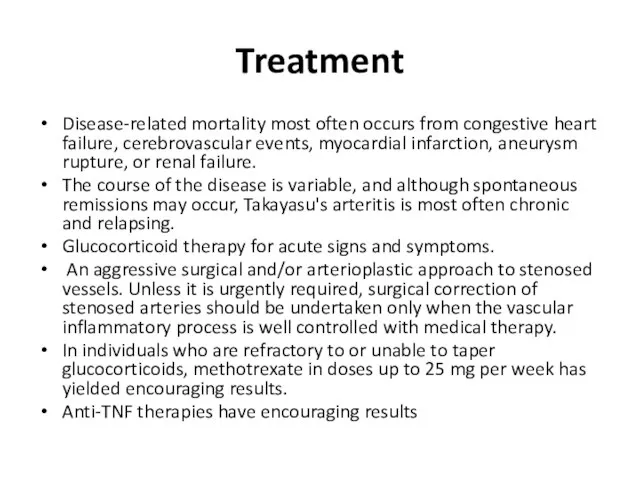
- 34. Treatment Disease-related mortality most often occurs from congestive heart failure, cerebrovascular events, myocardial infarction, aneurysm rupture,
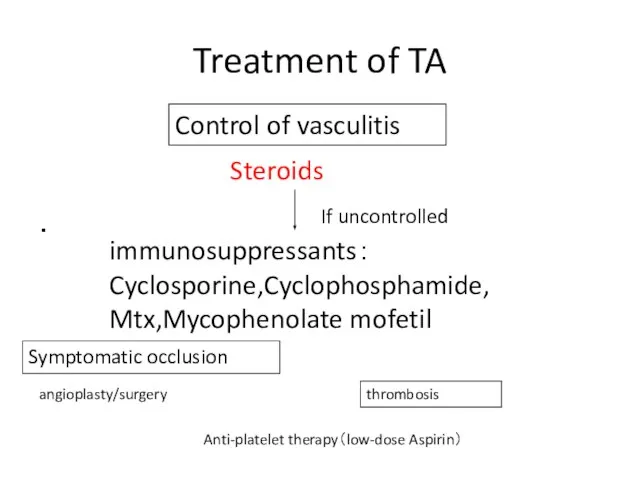
- 35. Treatment of TA ・ Steroids immunosuppressants: Cyclosporine,Cyclophosphamide, Mtx,Mycophenolate mofetil Anti-platelet therapy(low-dose Aspirin) angioplasty/surgery If uncontrolled Control
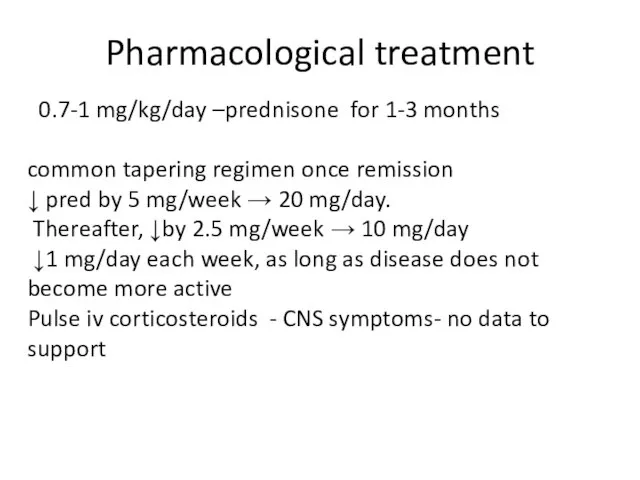
- 36. Pharmacological treatment 0.7-1 mg/kg/day –prednisone for 1-3 months common tapering regimen once remission ↓ pred by
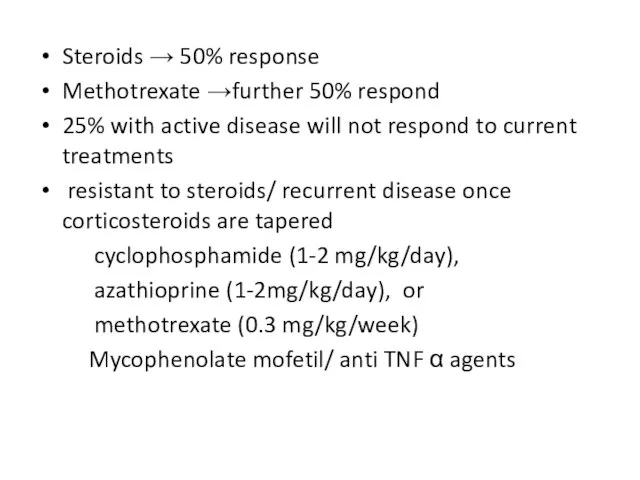
- 37. Steroids → 50% response Methotrexate →further 50% respond 25% with active disease will not respond to
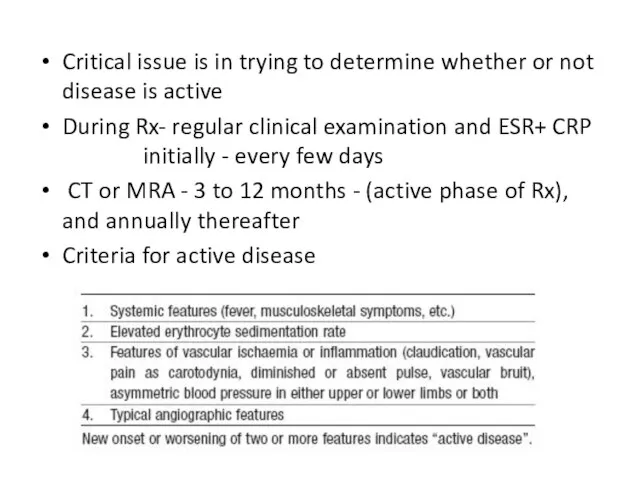
- 38. Critical issue is in trying to determine whether or not disease is active During Rx- regular
- 40. Скачать презентацию





 Сравнительное исследование депрессивных состояний у мужчин и женщин при помощи методики «Шкалы депрессии» А. Бека
Сравнительное исследование депрессивных состояний у мужчин и женщин при помощи методики «Шкалы депрессии» А. Бека Реабилитация хирургических больных. Врачебно-трудовая экспертиза. Функции ВКК, МСЭК
Реабилитация хирургических больных. Врачебно-трудовая экспертиза. Функции ВКК, МСЭК Острый и хронический синусит
Острый и хронический синусит Острая дыхательная недостаточность
Острая дыхательная недостаточность Аттестационная работа. Методическая разработка по выполнению проекта Берегите зрение
Аттестационная работа. Методическая разработка по выполнению проекта Берегите зрение Лечение диареи у детей
Лечение диареи у детей Лимфатическая система. Иммунная система
Лимфатическая система. Иммунная система Effective communication for vaccinations
Effective communication for vaccinations Радиобиологиялық эффекттер
Радиобиологиялық эффекттер Анатомия и физиология речевой системы
Анатомия и физиология речевой системы Эфферентные нервные волокна. Средства, влияющие на передачу возбуждения в адренергических синапсах
Эфферентные нервные волокна. Средства, влияющие на передачу возбуждения в адренергических синапсах Старший школьный возраст
Старший школьный возраст КТ. Признаки отека головного мозга
КТ. Признаки отека головного мозга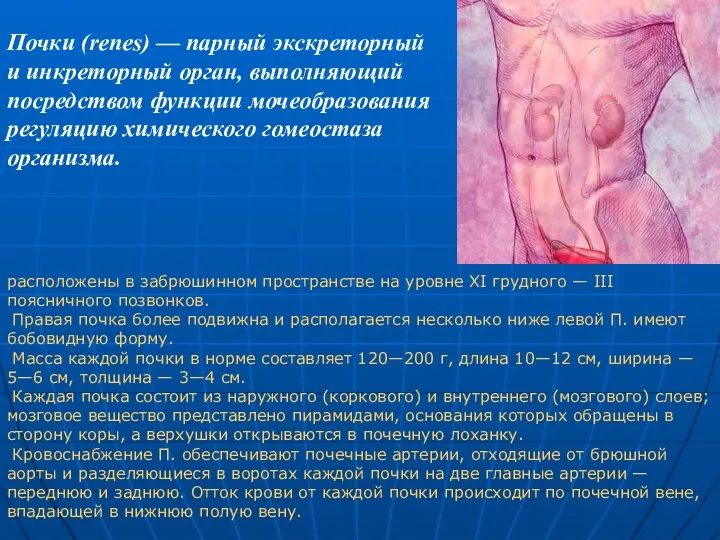 Почки. Важнейшая физиологическая роль почек
Почки. Важнейшая физиологическая роль почек Рак желудка
Рак желудка Тірек тістерді егеу ерекшелігі. Дайындаудың клиникалық кезеңдері
Тірек тістерді егеу ерекшелігі. Дайындаудың клиникалық кезеңдері Гипоксия (кислородное голодание)
Гипоксия (кислородное голодание) Құрсақішілік даму кезеңдері
Құрсақішілік даму кезеңдері Определение показаний к хирургическому лечению при септическом шоке
Определение показаний к хирургическому лечению при септическом шоке Клинические методы обследования в стоматологии
Клинические методы обследования в стоматологии Жүктіліктің үзілу қаупі терапиясы
Жүктіліктің үзілу қаупі терапиясы Сам себе косметолог. Уход за кожей лица
Сам себе косметолог. Уход за кожей лица Особенности хирургии
Особенности хирургии Установка для терагерцевой и длиноволновой ИК-терапии Инфратератрон
Установка для терагерцевой и длиноволновой ИК-терапии Инфратератрон Голос не рождённого ребёнка
Голос не рождённого ребёнка Методы исследования слуха
Методы исследования слуха Медицинская приборно-компьютерная система. Разновидности МПКС. Классификация по функциональным возможностям
Медицинская приборно-компьютерная система. Разновидности МПКС. Классификация по функциональным возможностям ВИЧ - инфекция
ВИЧ - инфекция