Содержание
- 2. Anti-anxiety drugs Prof. Anatoly Kreinin MD, PhD Director of Psychiatric Department, Maale Carmel Mental Health Center,
- 3. תרופות נוגדות חרדה.. Benzodiazepines (BZDs) Buspirone Antihistamines Antidepressants Anti-epileptic drugs (AEDs) Atypical antipsychotics
- 4. תרופות שלא משומשות יותר לחרדה Typical antipsychotics (e.g., thioridazineמלריל -) Barbiturates
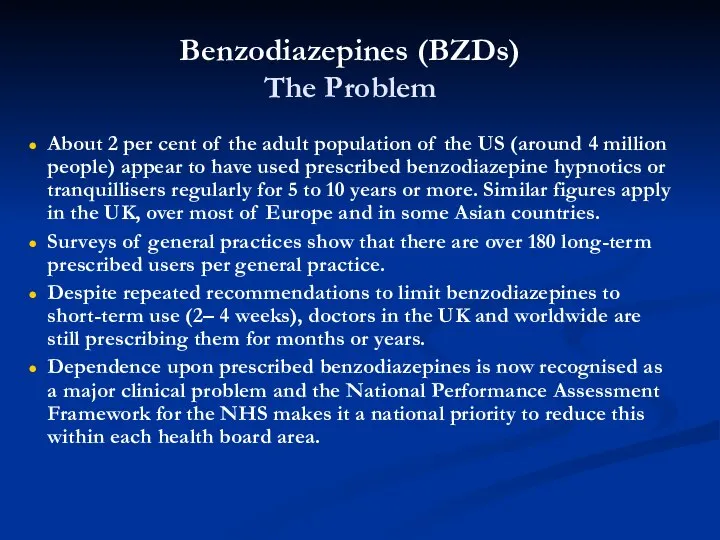
- 5. Benzodiazepines (BZDs) The Problem About 2 per cent of the adult population of the US (around
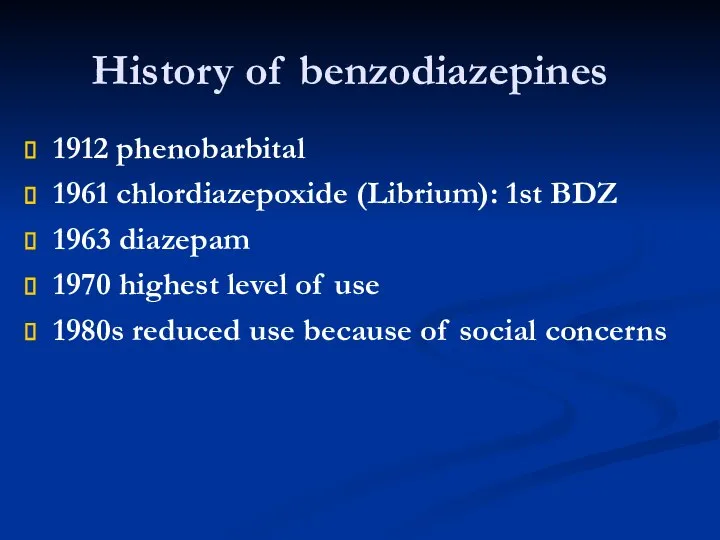
- 6. History of benzodiazepines 1912 phenobarbital 1961 chlordiazepoxide (Librium): 1st BDZ 1963 diazepam 1970 highest level of
- 7. BZD Alprazolam (Xanax) Clonazepam (clonex) Diazepam (Valium,Assival) Lorazepam (Lorivan) Oxazepam (Vaben) Clorazepate (Tranxal) Chlordiazepoxide (Librium)
- 8. History The first benzodiazepine (benzo) was synthesized by an Austrian scientist - Dr. Leo Sternbach in
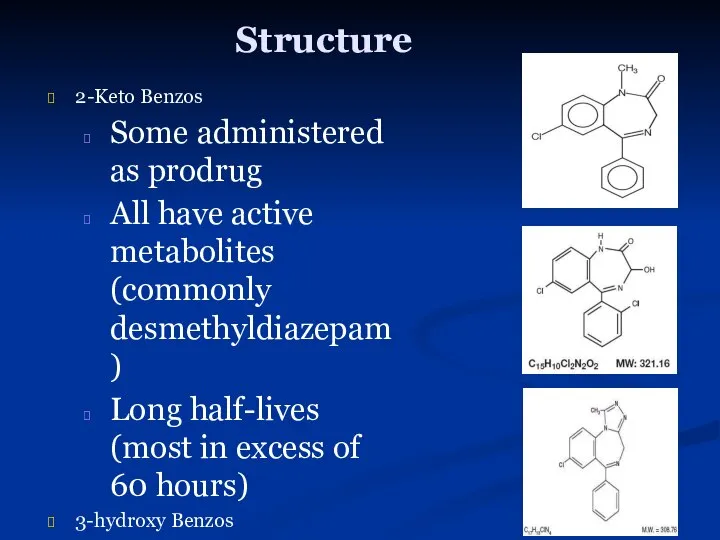
- 9. Structure 2-Keto Benzos Some administered as prodrug All have active metabolites (commonly desmethyldiazepam) Long half-lives (most
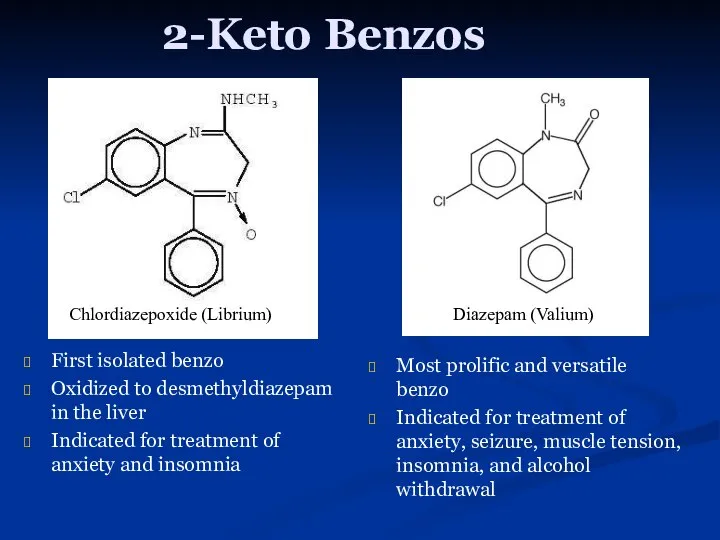
- 10. 2-Keto Benzos First isolated benzo Oxidized to desmethyldiazepam in the liver Indicated for treatment of anxiety
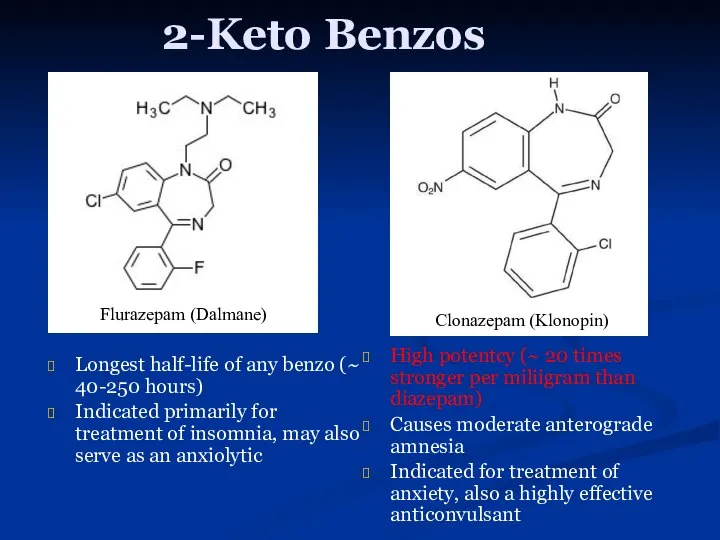
- 11. 2-Keto Benzos Longest half-life of any benzo (~ 40-250 hours) Indicated primarily for treatment of insomnia,
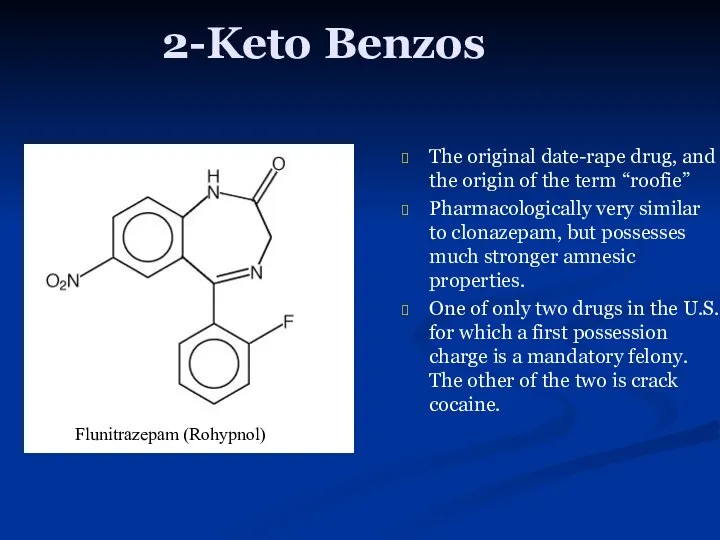
- 12. 2-Keto Benzos The original date-rape drug, and the origin of the term “roofie” Pharmacologically very similar
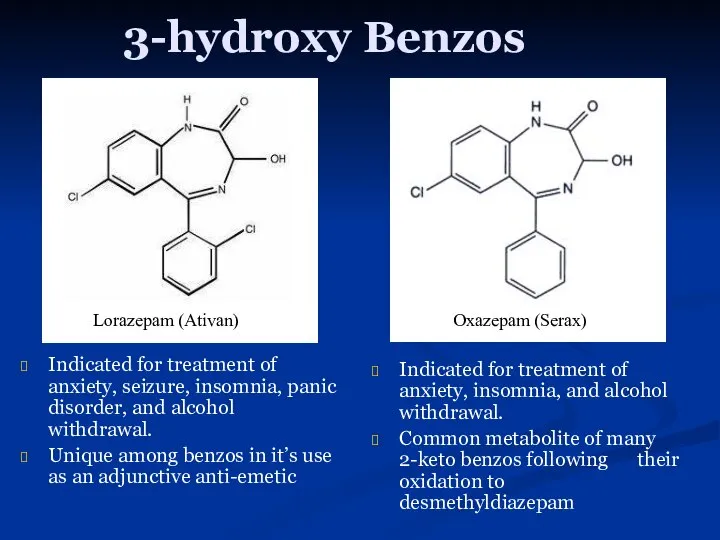
- 13. 3-hydroxy Benzos Indicated for treatment of anxiety, seizure, insomnia, panic disorder, and alcohol withdrawal. Unique among
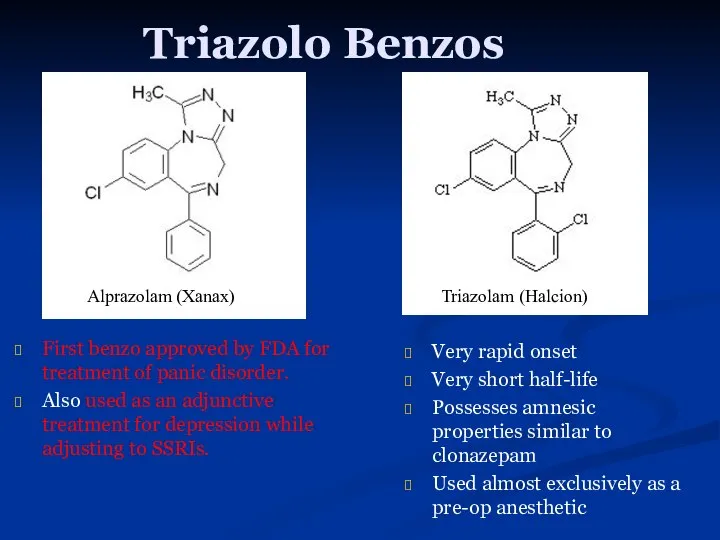
- 14. Triazolo Benzos First benzo approved by FDA for treatment of panic disorder. Also used as an
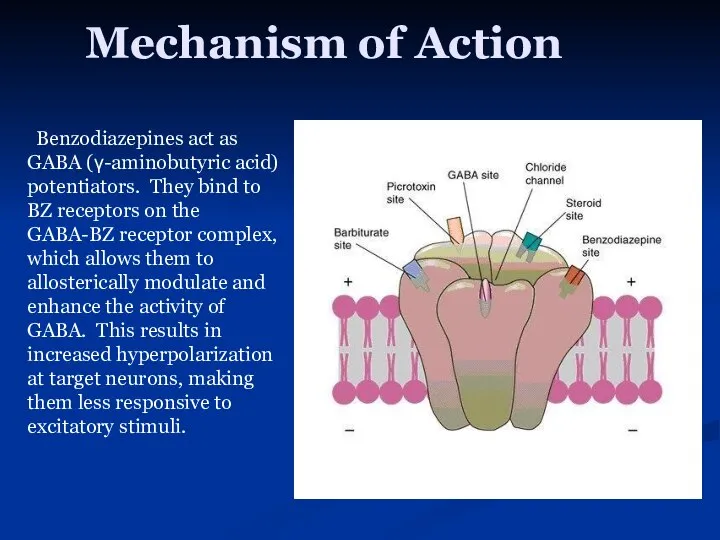
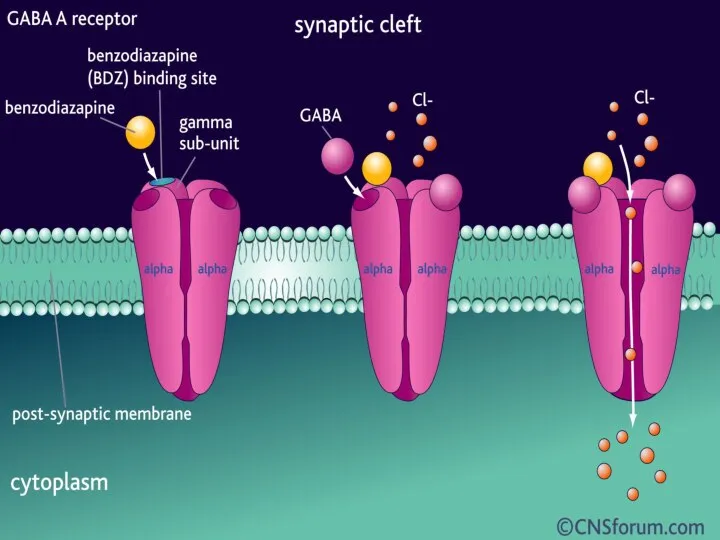
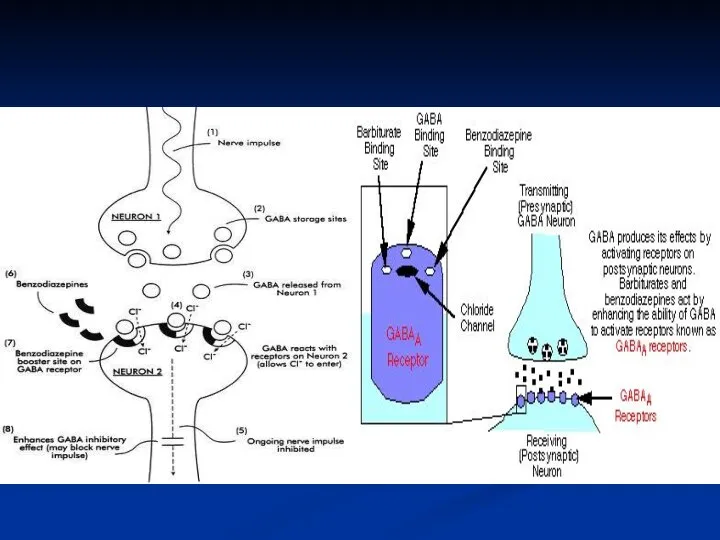
- 15. Mechanism of Action Benzodiazepines act as GABA (γ-aminobutyric acid) potentiators. They bind to BZ receptors on
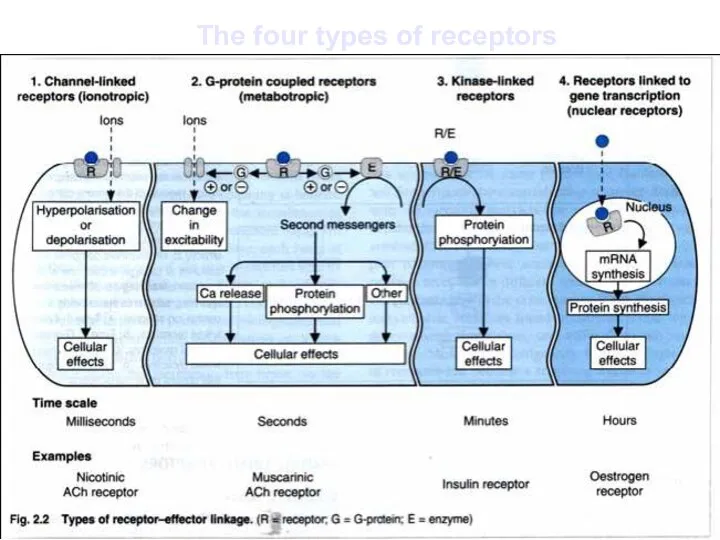
- 18. The four types of receptors
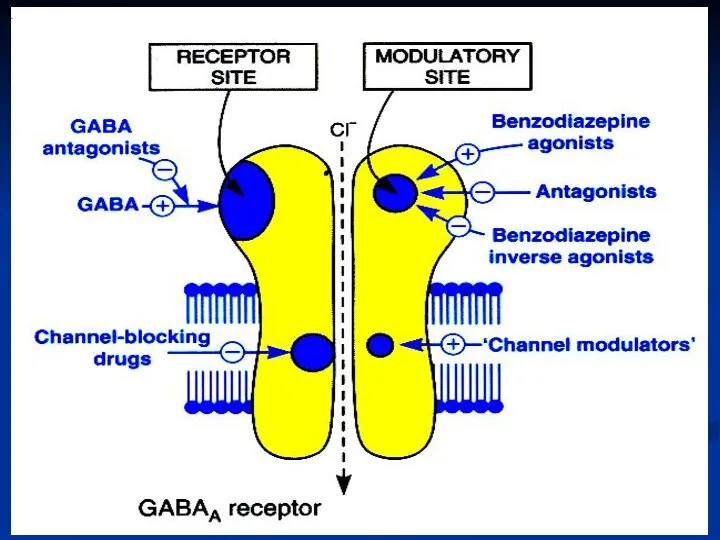
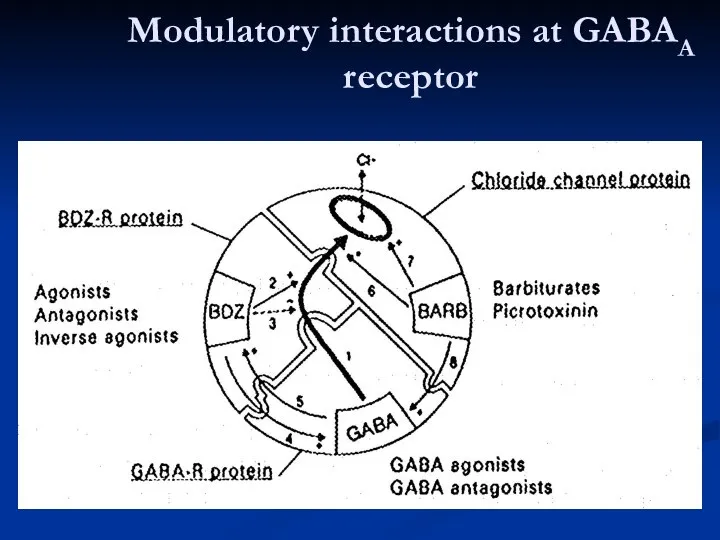
- 20. Modulatory interactions at GABAA receptor
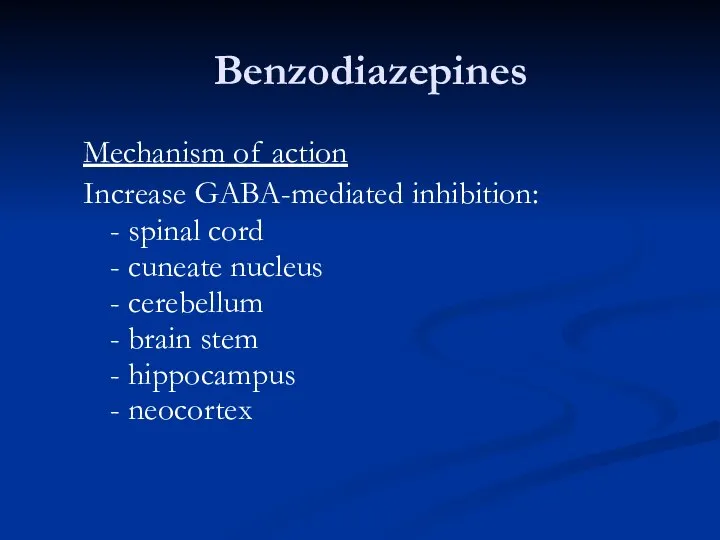
- 21. Benzodiazepines Mechanism of action Increase GABA-mediated inhibition: - spinal cord - cuneate nucleus - cerebellum -
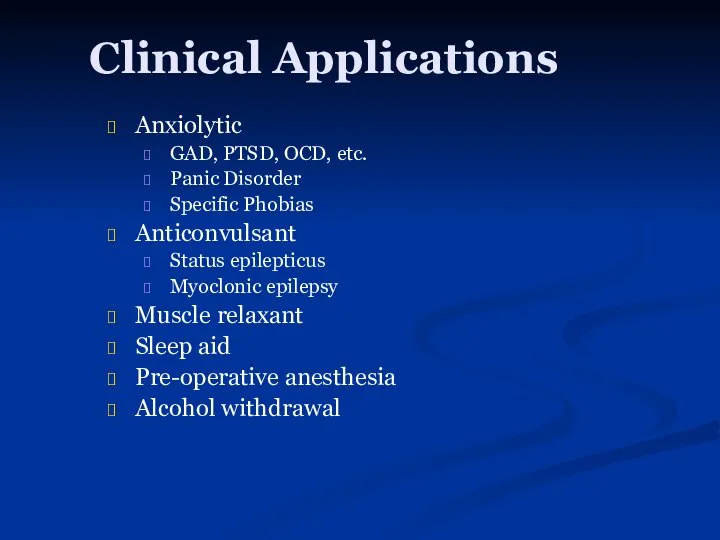
- 22. Clinical Applications Anxiolytic GAD, PTSD, OCD, etc. Panic Disorder Specific Phobias Anticonvulsant Status epilepticus Myoclonic epilepsy
- 23. Benzodiazepines CNS - Antianxiety, sedative - Hypnotic - Amnesic - Anticonvulsant - Muscle relaxant
- 24. Benzodiazepines Antianxiety - sedative effects - relief of anxiety and tension - emotional calming - drowsiness
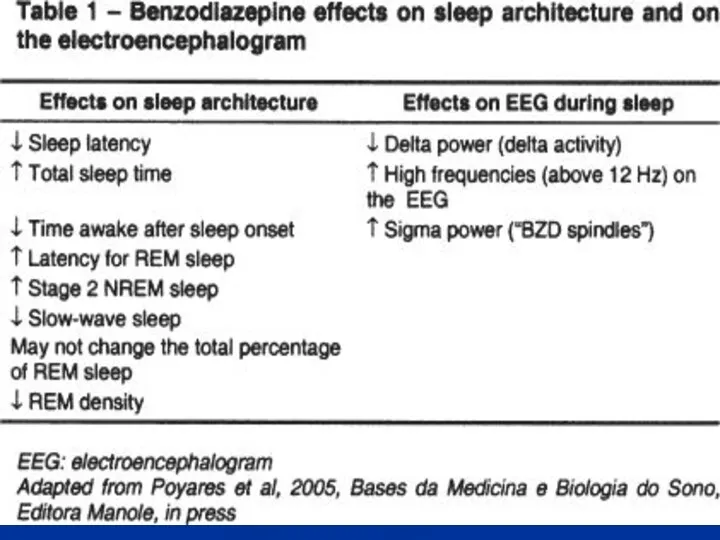
- 25. Benzodiazepines Hypnotic effects - ↓ latency of sleep onset - ↓ awakenings - ↑ stage 2
- 27. Benzodiazepines Anticonvulsant effects - interrupt status epilepticus or any existing seizures – diazepam (i.v.) - prevent
- 28. Benzodiazepines Muscle relaxant effects ! No effect on NMJ (neuromuscular junction); a CNS effect! Diazepam: i.v.
- 29. Benzodiazepines Effects on respiration and cardiovascular system -usually insignificant Preexisting respiratory failure can be aggravated by
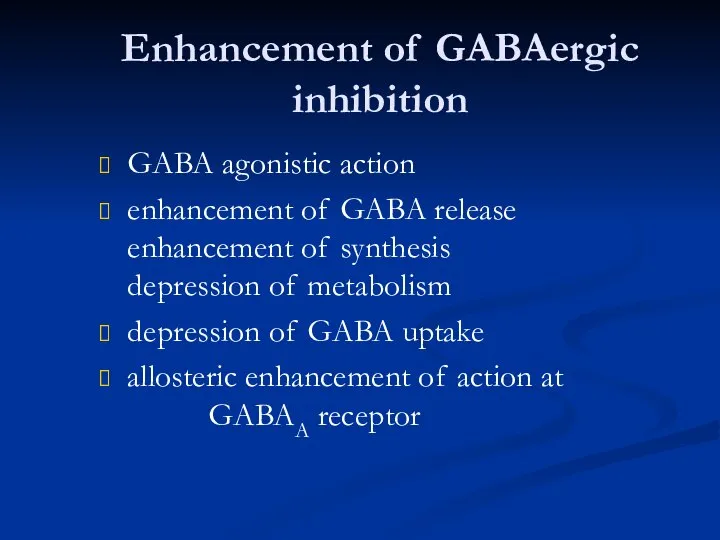
- 30. Enhancement of GABAergic inhibition GABA agonistic action enhancement of GABA release enhancement of synthesis depression of
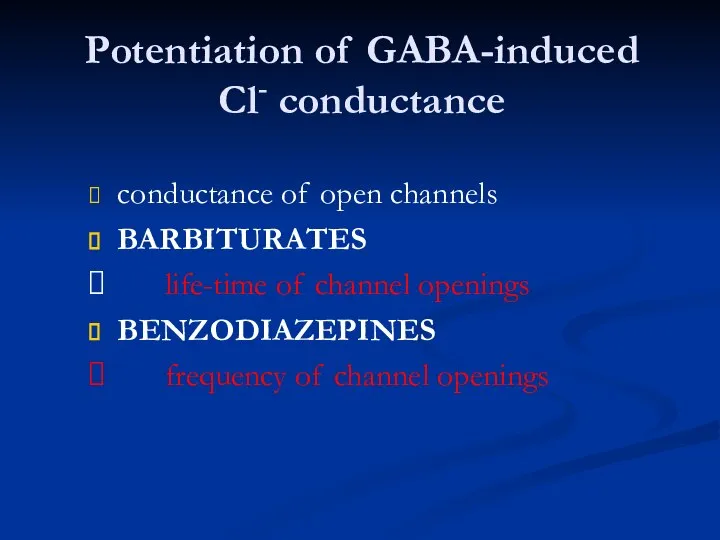
- 31. Potentiation of GABA-induced Cl- conductance conductance of open channels BARBITURATES life-time of channel openings BENZODIAZEPINES frequency
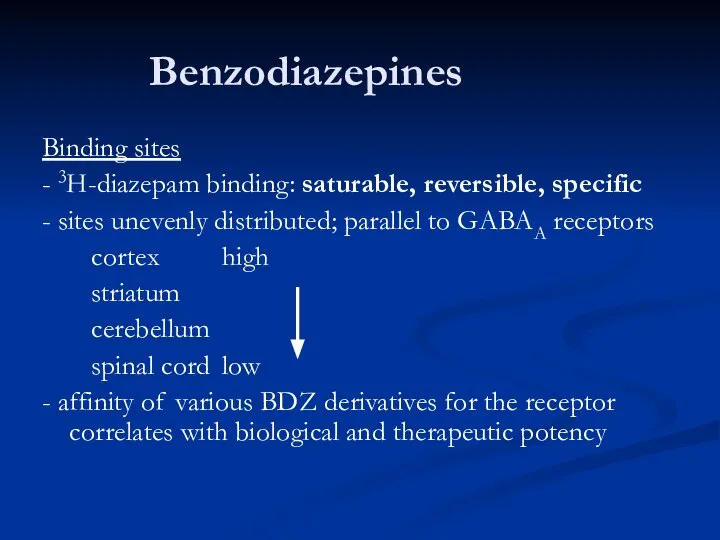
- 32. Benzodiazepines Binding sites - 3H-diazepam binding: saturable, reversible, specific - sites unevenly distributed; parallel to GABAA
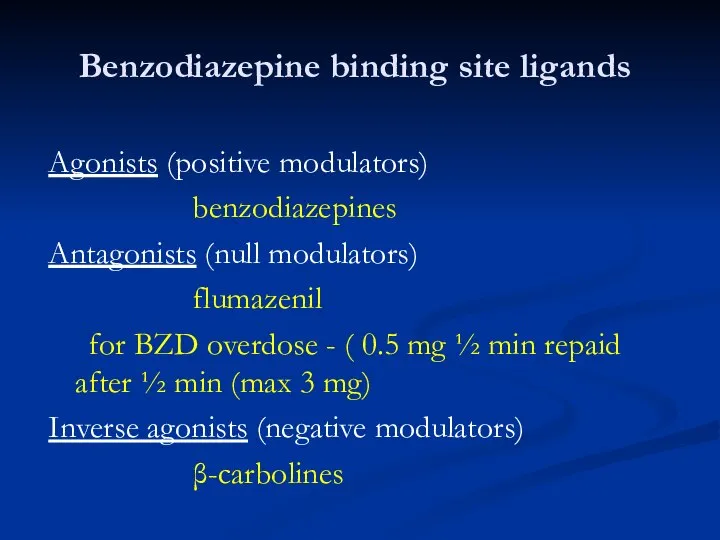
- 33. Benzodiazepine binding site ligands Agonists (positive modulators) benzodiazepines Antagonists (null modulators) flumazenil for BZD overdose -
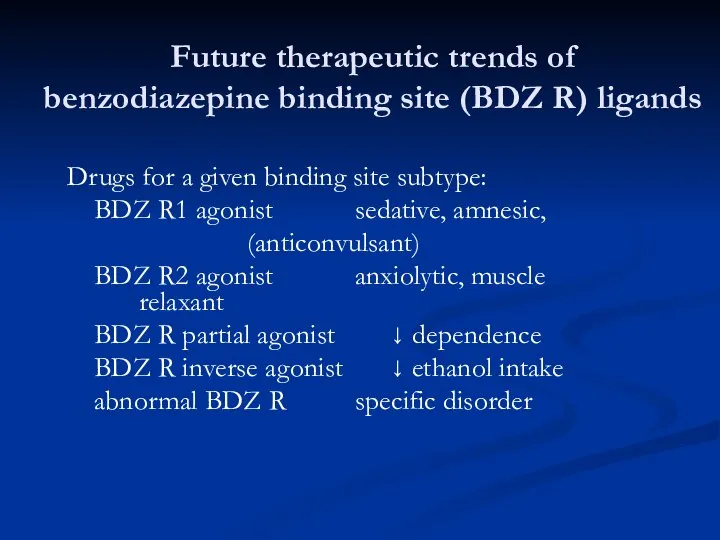
- 34. Future therapeutic trends of benzodiazepine binding site (BDZ R) ligands Drugs for a given binding site
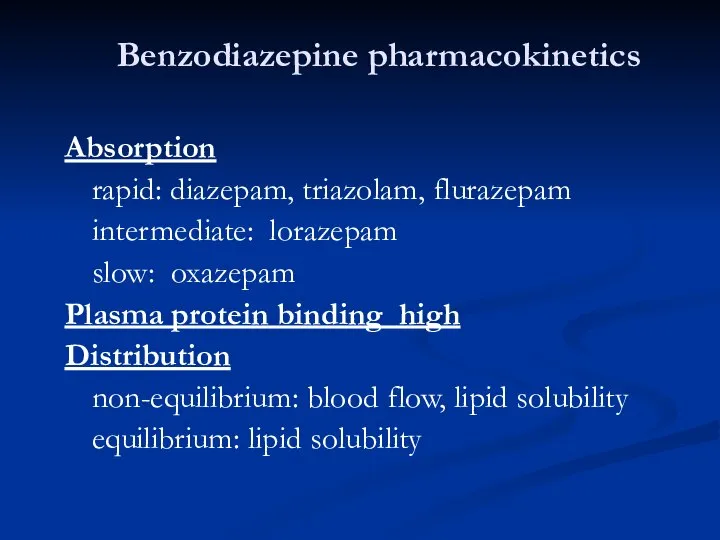
- 35. Benzodiazepine pharmacokinetics Absorption rapid: diazepam, triazolam, flurazepam intermediate: lorazepam slow: oxazepam Plasma protein binding high Distribution
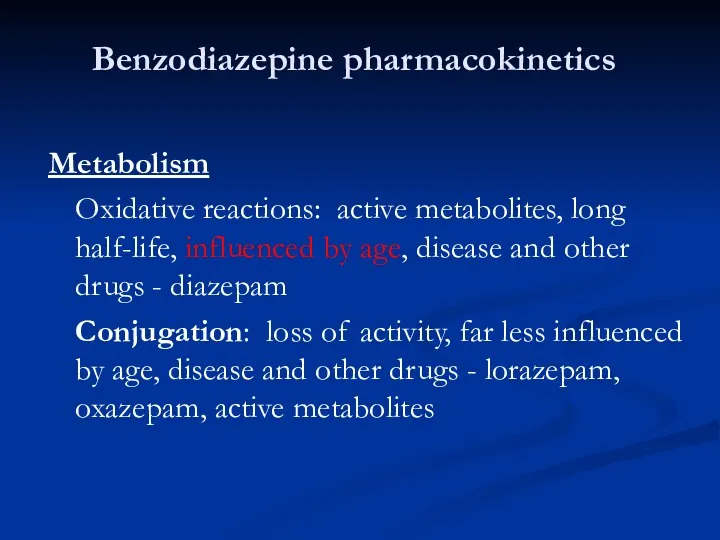
- 36. Benzodiazepine pharmacokinetics Metabolism Oxidative reactions: active metabolites, long half-life, influenced by age, disease and other drugs
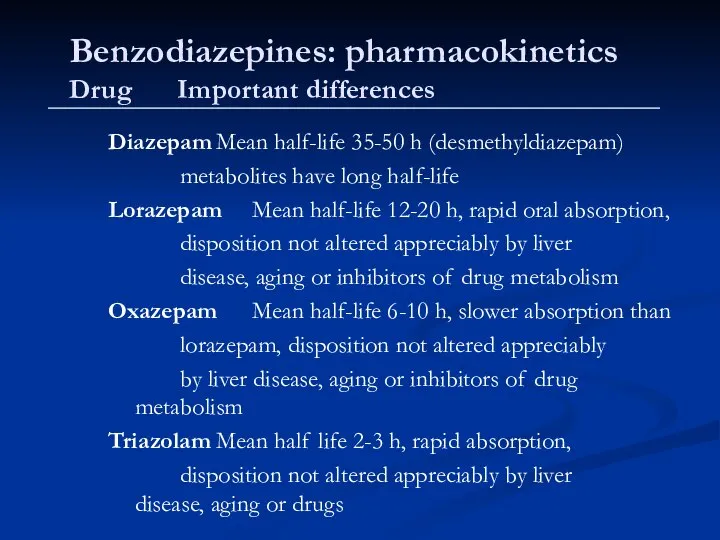
- 37. Benzodiazepines: pharmacokinetics Drug Important differences Diazepam Mean half-life 35-50 h (desmethyldiazepam) metabolites have long half-life Lorazepam
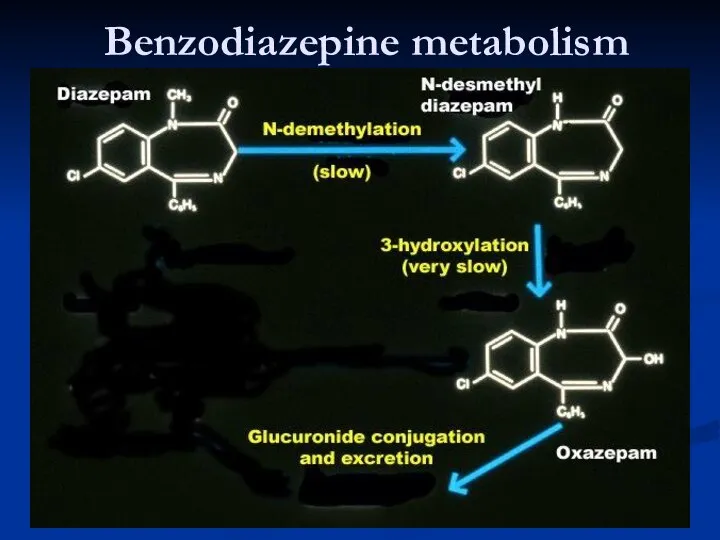
- 38. Benzodiazepine metabolism
- 40. Скачать презентацию



 Физические и физико-химические свойства и характеристики грунтов. (Лекция 2)
Физические и физико-химические свойства и характеристики грунтов. (Лекция 2) Мұнай, құрамыөңдеу әдістері
Мұнай, құрамыөңдеу әдістері Типы химических реакций в органической химии
Типы химических реакций в органической химии Методы исследования гидрохимического режима водоемов
Методы исследования гидрохимического режима водоемов В гостях у Хозяйки Медной горы. Покровская сельская библиотека
В гостях у Хозяйки Медной горы. Покровская сельская библиотека Железо в сплавах и природе. Состав железа
Железо в сплавах и природе. Состав железа Метод комплексонометрического титрования (лекция 8)
Метод комплексонометрического титрования (лекция 8) Биохимия витаминов. Классификация витаминов. Жирорастворимые витамины. (Лекция 20)
Биохимия витаминов. Классификация витаминов. Жирорастворимые витамины. (Лекция 20) Electrochemical properties of arylsilanes
Electrochemical properties of arylsilanes Кинетика
Кинетика Презентация Применение электролиза
Презентация Применение электролиза  Химик-эколог
Химик-эколог Второе начало термодинамики. Направленность химических процессов
Второе начало термодинамики. Направленность химических процессов Наука о веществе - химия
Наука о веществе - химия Основні класи неорганічних сполук
Основні класи неорганічних сполук Анализ консервантов в пищевых продуктах
Анализ консервантов в пищевых продуктах Аллотропия - явление образования нескольких простых веществ атомами одного и того же химического элемента
Аллотропия - явление образования нескольких простых веществ атомами одного и того же химического элемента Химическая промышленность
Химическая промышленность Оксид серы(VI). Серная кислота
Оксид серы(VI). Серная кислота Презентация Нефть и способы ее переработки
Презентация Нефть и способы ее переработки Органические вещества спирты
Органические вещества спирты Презентация по Химии "Нуклеиновые кислоты(НК)." - скачать смотреть бесплатно
Презентация по Химии "Нуклеиновые кислоты(НК)." - скачать смотреть бесплатно Превращения веществ. Роль химии в жизни человека
Превращения веществ. Роль химии в жизни человека ГИА. А1: Строение атомов первых 20 химических элементов ПСХЭ
ГИА. А1: Строение атомов первых 20 химических элементов ПСХЭ Вода. Классы неорганических соединений. 8 класс
Вода. Классы неорганических соединений. 8 класс Химикаты для сельского хозяйства
Химикаты для сельского хозяйства Стійкість до важких металів
Стійкість до важких металів Соединения алюминия
Соединения алюминия