Содержание
- 2. The Respiratory System Respiration is gas exchange: O2 for CO2 Occurs between atmosphere and body cells
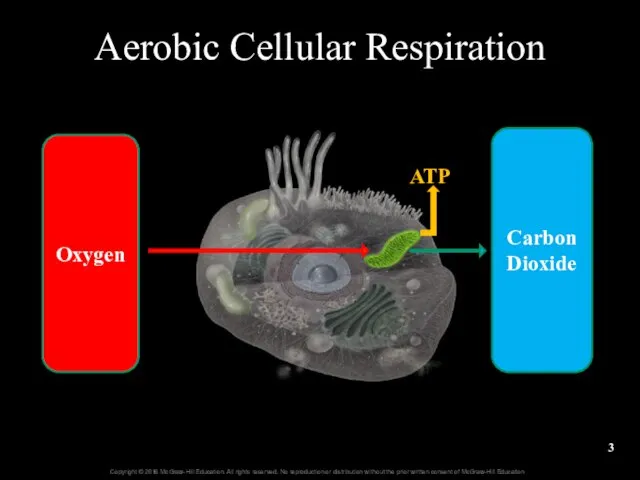
- 3. Aerobic Cellular Respiration Oxygen Carbon Dioxide ATP
- 4. 23.1 Introduction to the Respiratory System State the functions of the respiratory system. Distinguish between the
- 5. 23.1a General Functions of the Respiratory System Air passageway Air moves from atmosphere to alveoli as
- 6. 23.1a General Functions of the Respiratory System Sound production Air moves across vocal cords of the
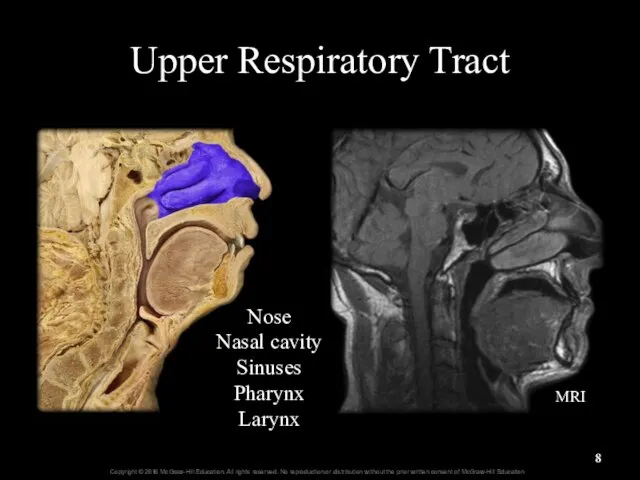
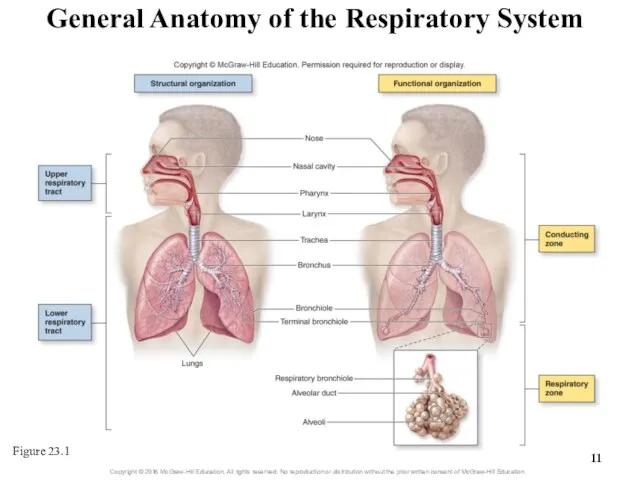
- 7. 23.1b General Organization of the Respiratory System Structural organization Upper respiratory tract Larynx and above Lower
- 8. Upper Respiratory Tract Nose Nasal cavity Sinuses Pharynx Larynx MRI
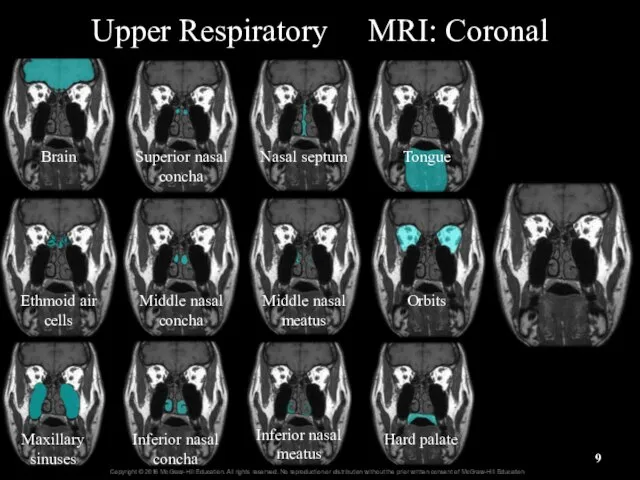
- 9. Upper Respiratory MRI: Coronal Brain Ethmoid air cells Maxillary sinuses Superior nasal concha Middle nasal concha
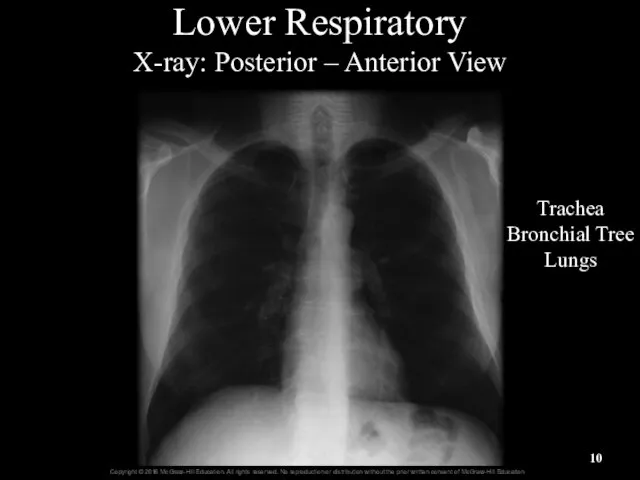
- 10. Lower Respiratory X-ray: Posterior – Anterior View Trachea Bronchial Tree Lungs
- 11. General Anatomy of the Respiratory System Figure 23.1
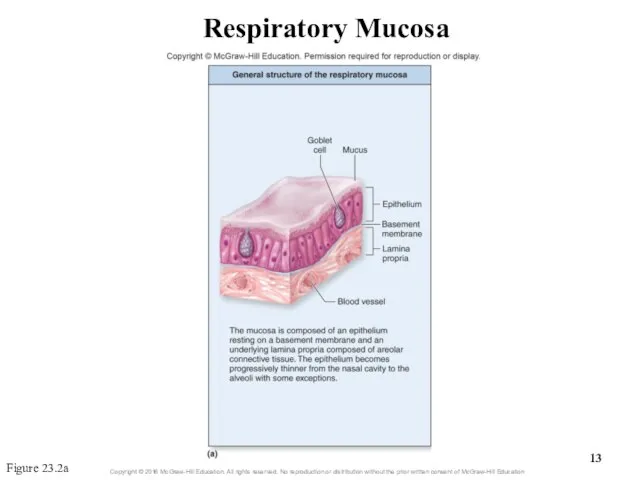
- 12. 23.1c Respiratory Mucosa Mucosa = mucous membrane: respiratory lining Epithelium resting on a basement membrane Underlying
- 13. Respiratory Mucosa Figure 23.2a
- 14. Respiratory Mucosa Figure 23.2b
- 15. Respiratory Epithelium High Magnification Respiratory epithelium Cilia Columnar epithelial cells Goblet cells Basal cells Basement membrane
- 16. 23.1c Respiratory Mucosa Mucous secretions Produced from secretions of Goblet cells of epithelial lining Mucous and
- 17. What did you learn? What is the difference between the conducting and respiratory zones? How does
- 18. 23.2 Upper Respiratory Tract Describe the structure and function of the nose. Provide a general description
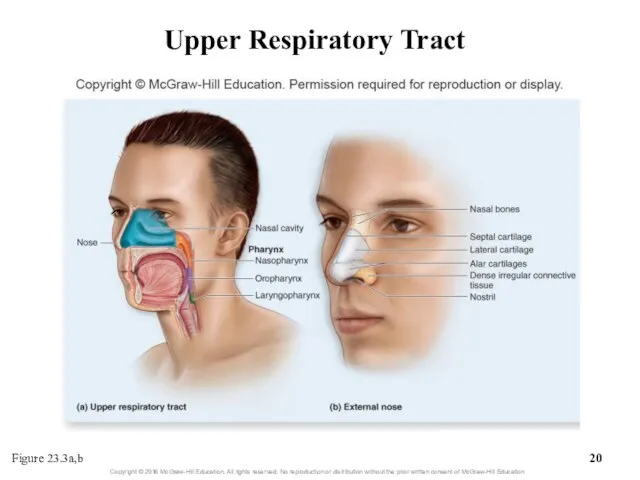
- 19. 23.2a Nose and Nasal Cavity Nose: first conducting structure for inhaled air Formed by bone, hyaline
- 20. Upper Respiratory Tract Figure 23.3a,b
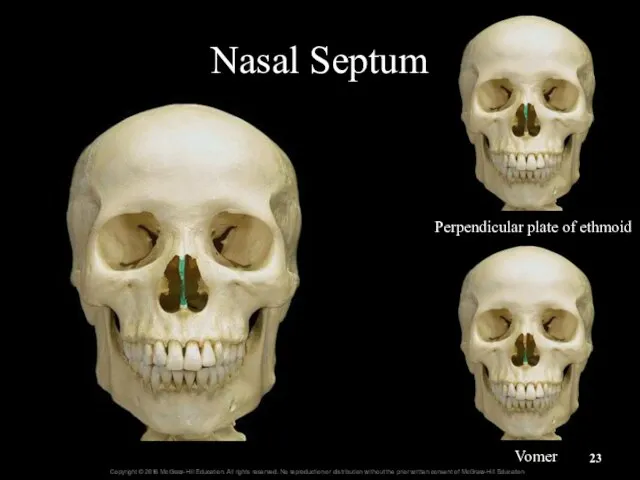
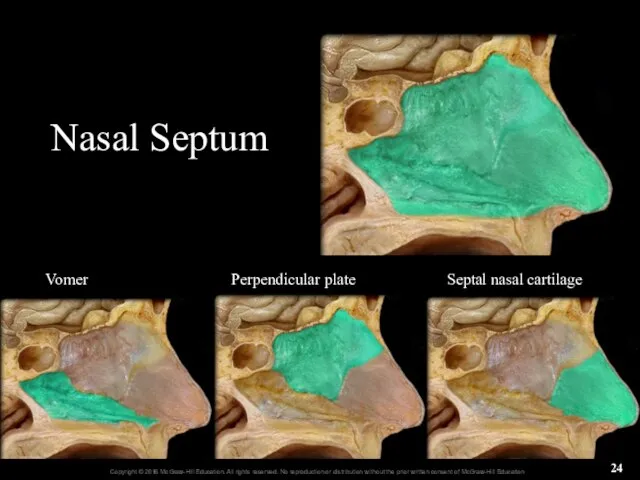
- 21. 23.2a Nose and Nasal Cavity Nasal cavity: from nostrils to choanae An oblong-shaped internal space Choanae
- 22. Nasal Cavity and Choanae Nares Nasal Cavity Nasal Septum Nasopharynx Soft Palate Uvula Choanae Hard Palate
- 23. Nasal Septum Perpendicular plate of ethmoid Vomer
- 24. Nasal Septum Vomer Perpendicular plate Septal nasal cartilage
- 25. 23.2a Nose and Nasal Cavity The nasal conchae Three paired, bony projections on lateral walls of
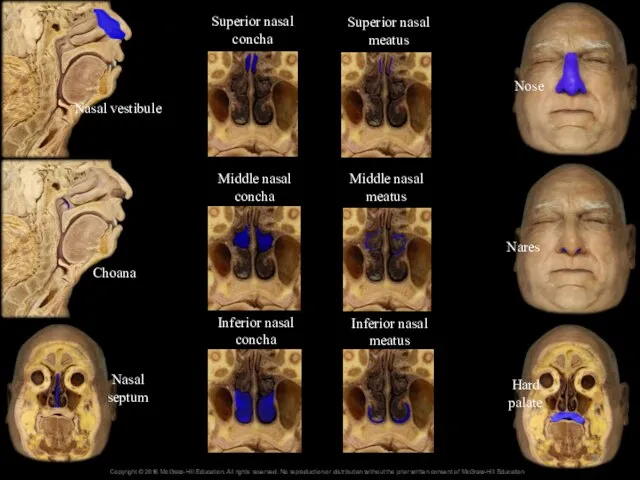
- 26. Nasal vestibule Choana Nasal septum Hard palate Nares Nose Superior nasal concha Middle nasal concha Inferior
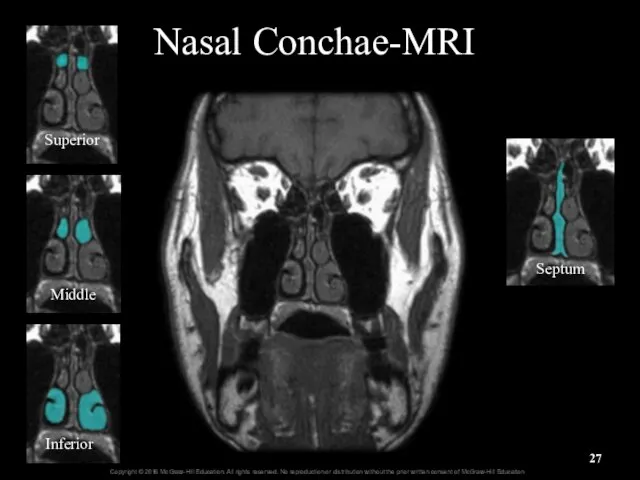
- 27. Nasal Conchae-MRI Superior Middle Inferior Septum
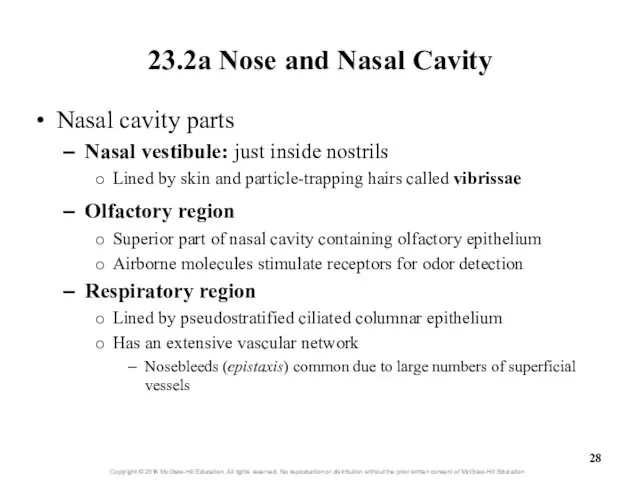
- 28. 23.2a Nose and Nasal Cavity Nasal cavity parts Nasal vestibule: just inside nostrils Lined by skin
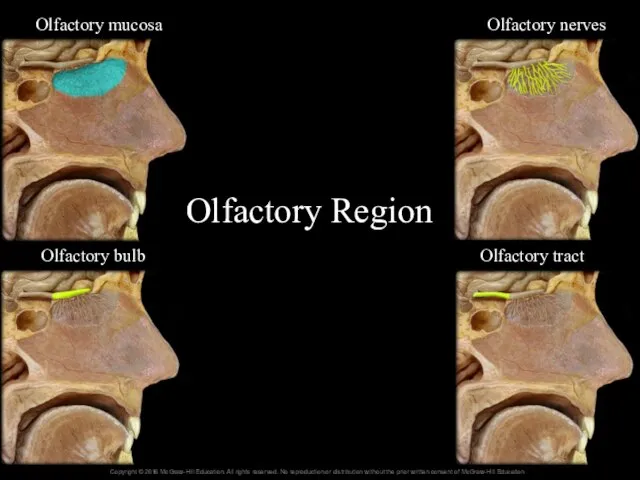
- 29. Olfactory Region 16- Olfactory tract Olfactory bulb Olfactory nerves Olfactory mucosa
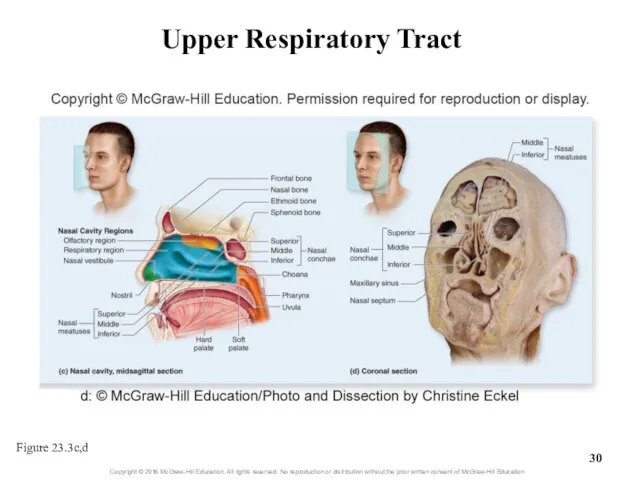
- 30. Upper Respiratory Tract Figure 23.3c,d
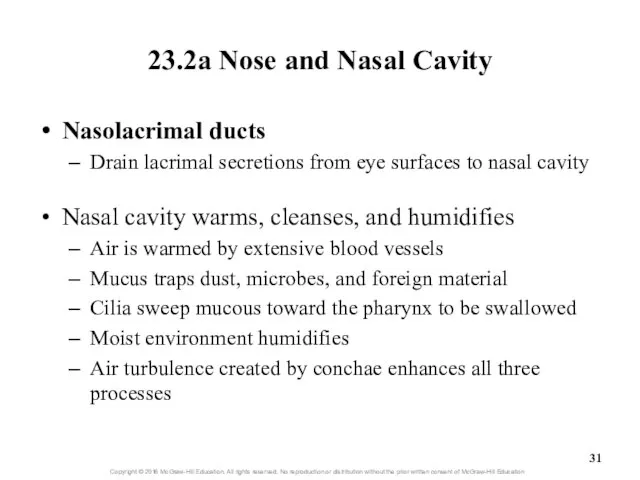
- 31. 23.2a Nose and Nasal Cavity Nasolacrimal ducts Drain lacrimal secretions from eye surfaces to nasal cavity
- 32. Clinical View: Runny Nose Rhinorrhea (runny nose) occurs as a result of Increased production of mucus
- 33. 23.2b Paranasal Sinuses Paranasal sinuses: spaces within skull bones Named for specific bone in which they
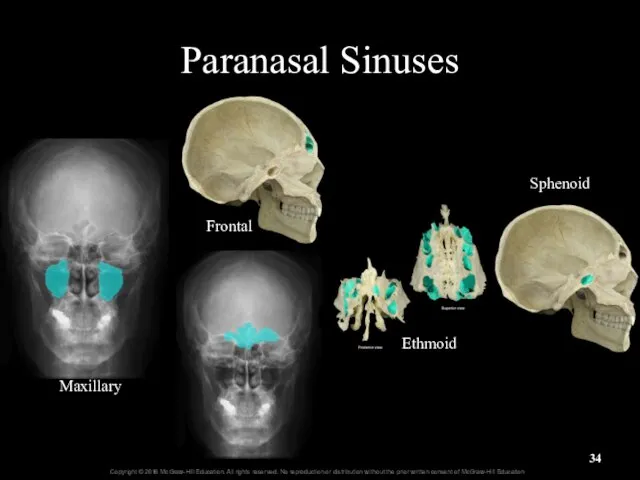
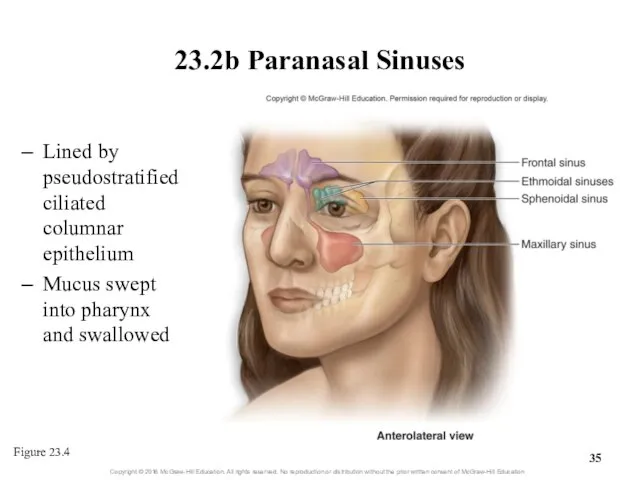
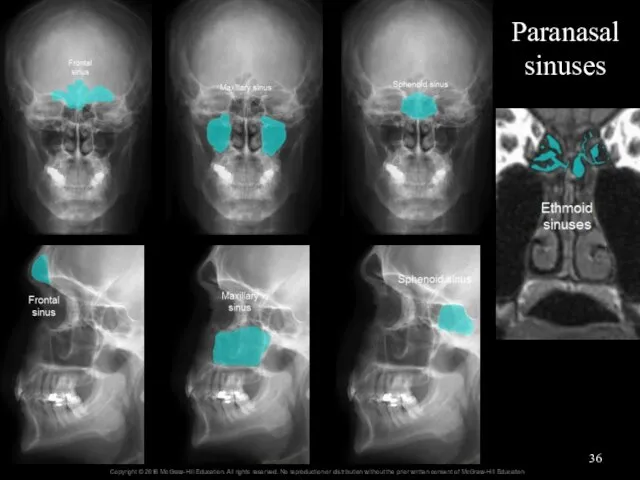
- 34. Maxillary Frontal Ethmoid Sphenoid Paranasal Sinuses
- 35. 23.2b Paranasal Sinuses Lined by pseudostratified ciliated columnar epithelium Mucus swept into pharynx and swallowed Figure
- 36. Paranasal sinuses
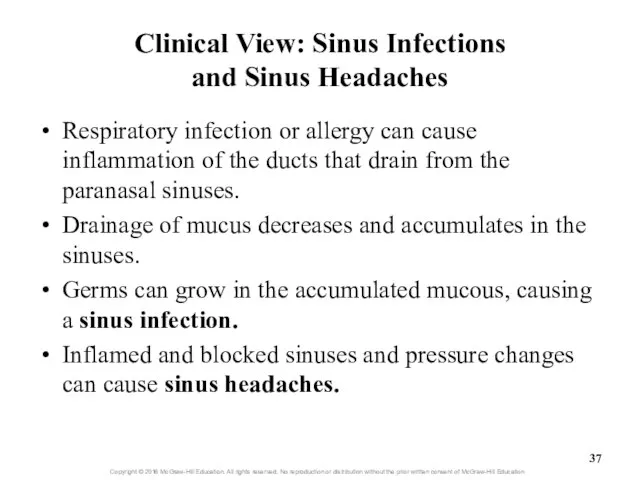
- 37. Clinical View: Sinus Infections and Sinus Headaches Respiratory infection or allergy can cause inflammation of the
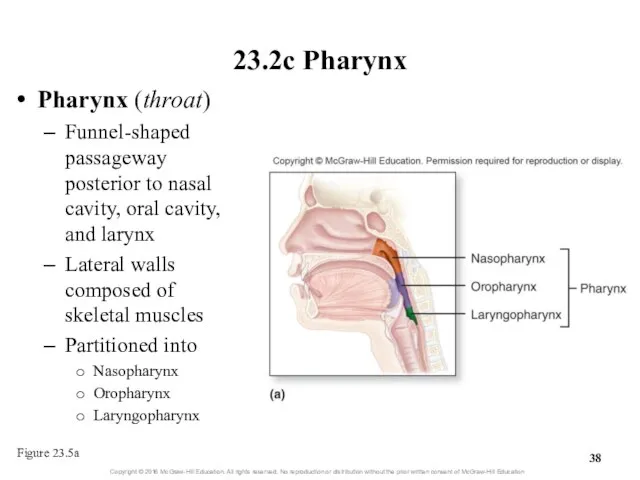
- 38. 23.2c Pharynx Pharynx (throat) Funnel-shaped passageway posterior to nasal cavity, oral cavity, and larynx Lateral walls
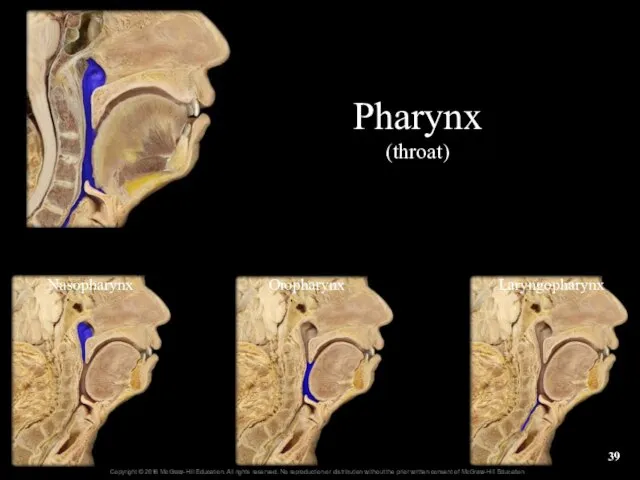
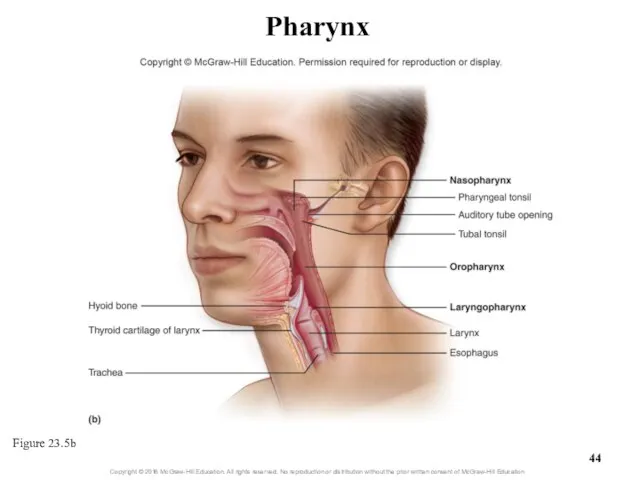
- 39. Nasopharynx Oropharynx Laryngopharynx Pharynx (throat)
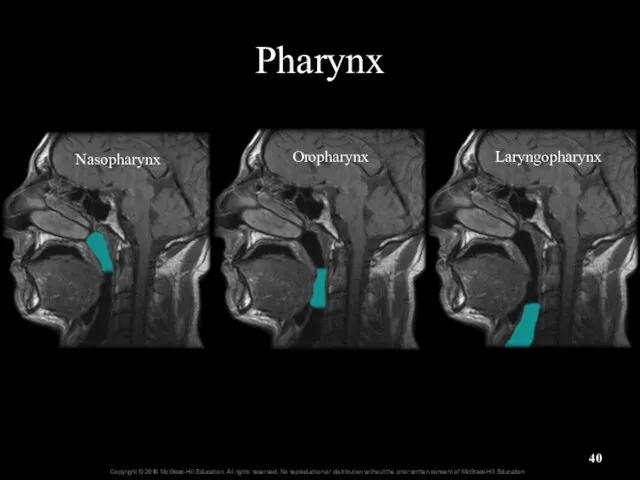
- 40. Pharynx Oropharynx Nasopharynx Laryngopharynx
- 41. 23.2c Pharynx Nasopharynx: most superior part of pharynx Posterior to nasal cavity, superior to soft palate
- 42. 23.2c Pharynx Oropharynx: middle pharyngeal region Posterior to oral cavity Extends from soft palate to hyoid
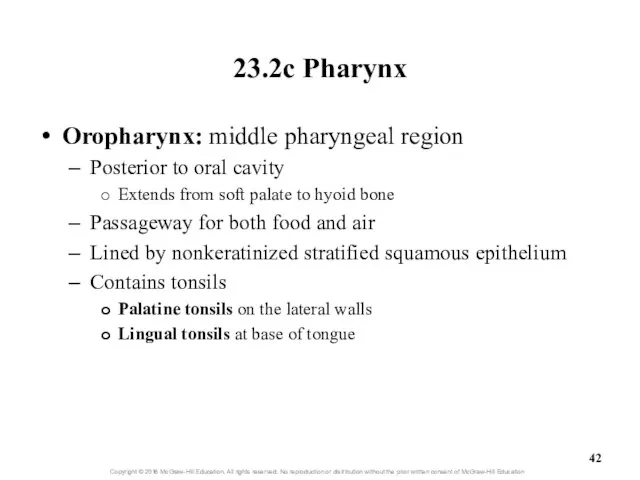
- 43. 23.2c Pharynx Laryngopharynx: inferior, narrow region of pharynx Posterior to the larynx From level of hyoid
- 44. Pharynx Figure 23.5b
- 45. What did you learn? What are vibrissae? Between which conchae is the middle nasal meatus located?
- 46. 23.3 Lower Respiratory Tract Describe the general functions and structure of the larynx. Explain how the
- 47. 23.3 Lower Respiratory Tract (continued) Explain the processes of bronchoconstriction and bronchodilation. Describe the structure and
- 48. 23.3 Lower Respiratory Tract Includes conducting pathways from larynx to terminal bronchioles Includes structures involved in
- 49. 23.3a Larynx Larynx (voice box) Cylindrical airway between laryngopharynx and trachea Several functions Air passageway (usually
- 50. 22.3a Larynx Several functions (continued) Participates in sneeze and cough reflexes Help remove irritants from nasal
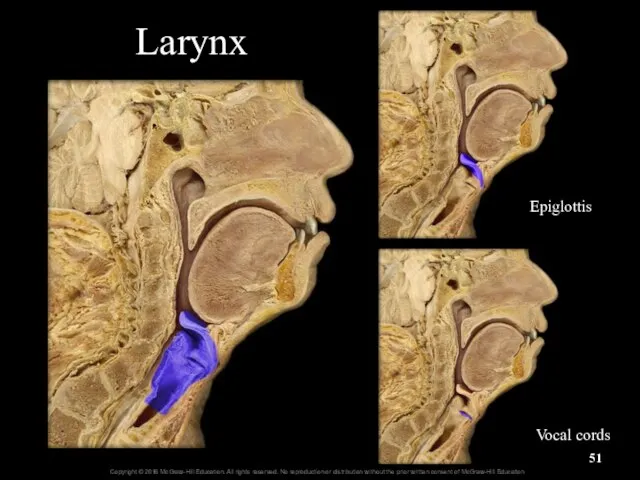
- 51. Larynx Epiglottis Vocal cords
- 52. Larynx
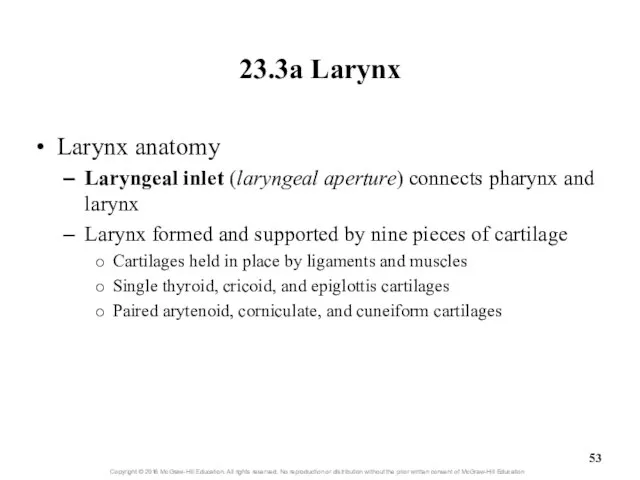
- 53. 23.3a Larynx Larynx anatomy Laryngeal inlet (laryngeal aperture) connects pharynx and larynx Larynx formed and supported
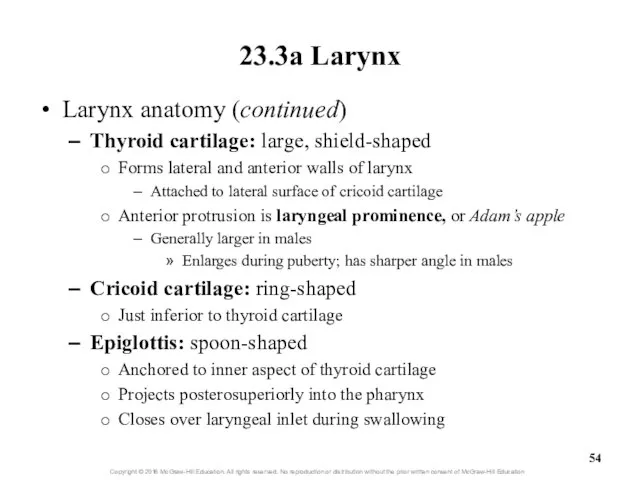
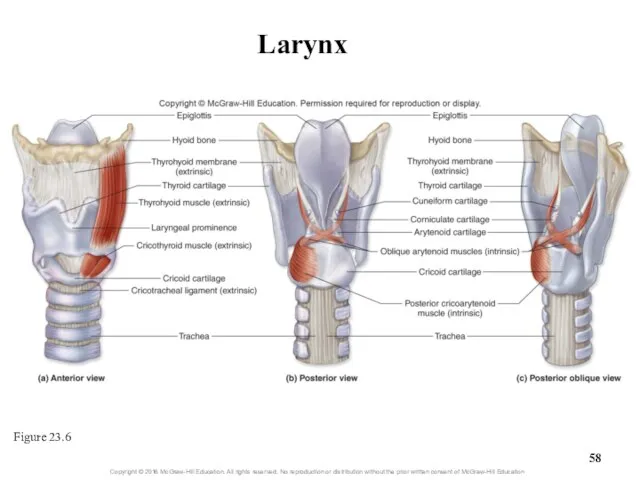
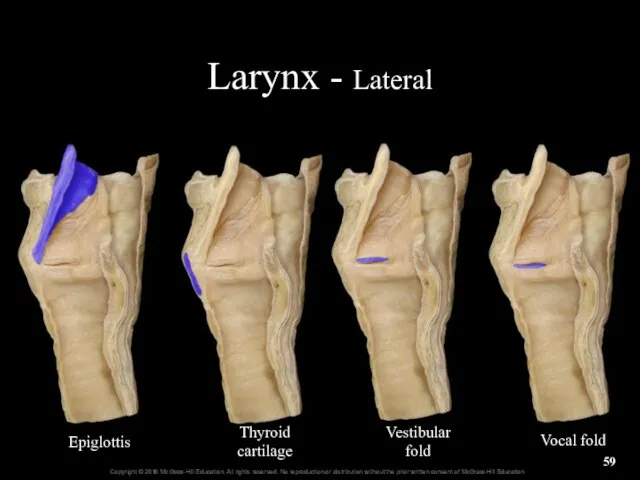
- 54. 23.3a Larynx Larynx anatomy (continued) Thyroid cartilage: large, shield-shaped Forms lateral and anterior walls of larynx
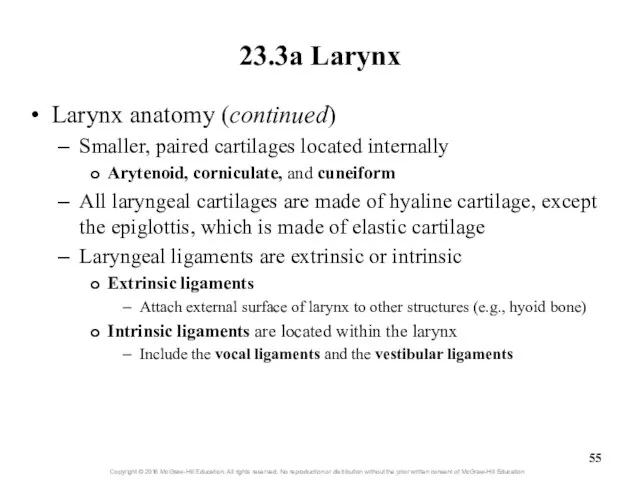
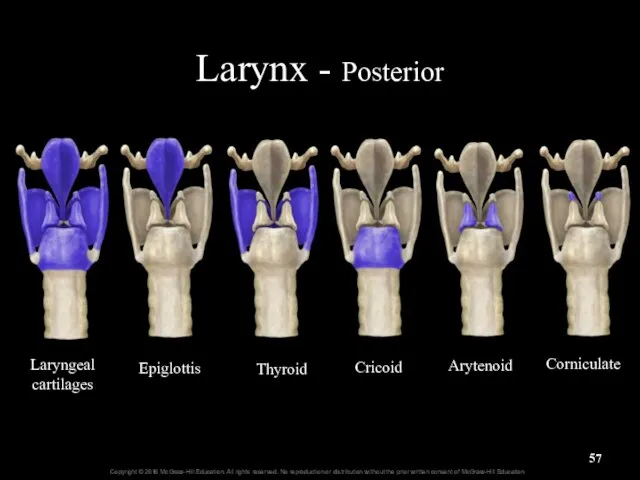
- 55. 23.3a Larynx Larynx anatomy (continued) Smaller, paired cartilages located internally Arytenoid, corniculate, and cuneiform All laryngeal
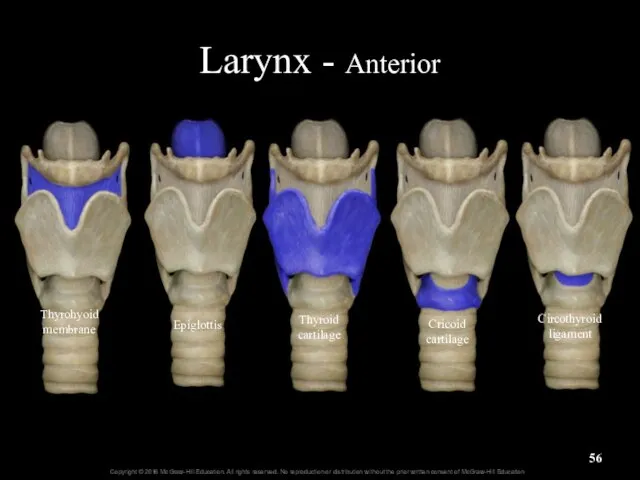
- 56. Larynx - Anterior Thyroid cartilage Cricoid cartilage Epiglottis Circothyroid ligament Thyrohyoid membrane
- 57. Larynx - Posterior Laryngeal cartilages Epiglottis Thyroid Cricoid Arytenoid Corniculate
- 58. Larynx Figure 23.6
- 59. Larynx - Lateral Epiglottis Thyroid cartilage Vestibular fold Vocal fold
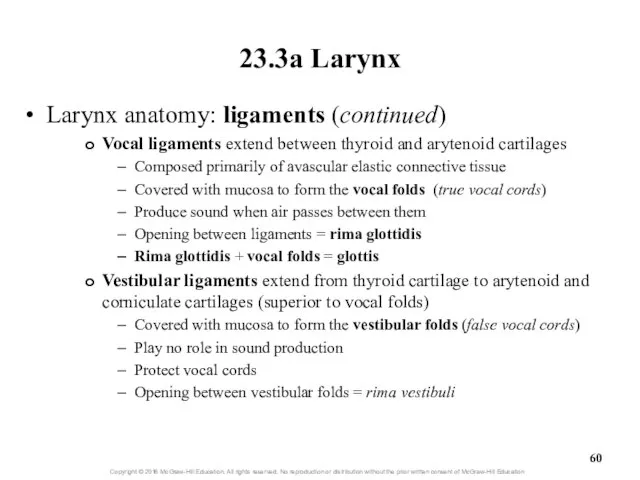
- 60. 23.3a Larynx Larynx anatomy: ligaments (continued) Vocal ligaments extend between thyroid and arytenoid cartilages Composed primarily
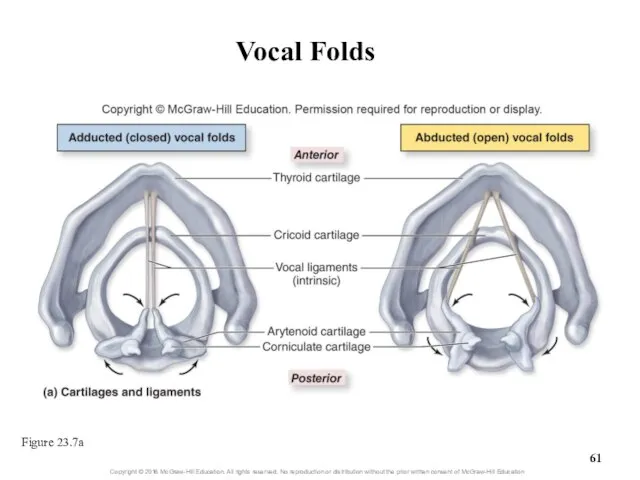
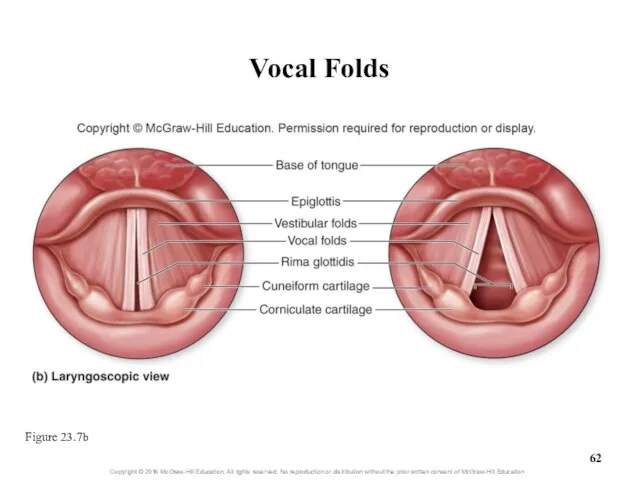
- 61. Vocal Folds Figure 23.7a
- 62. Vocal Folds Figure 23.7b
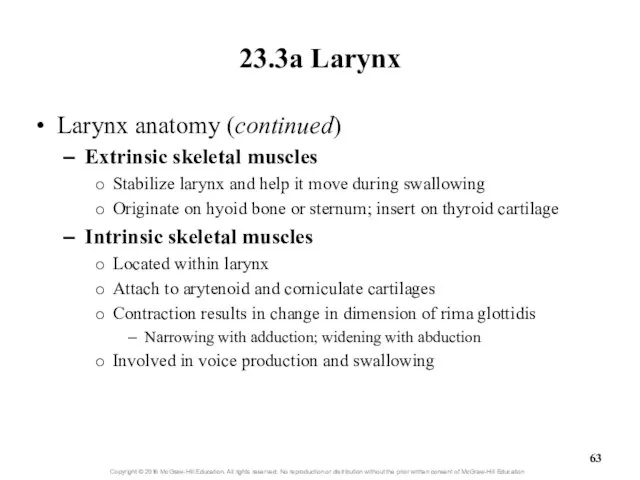
- 63. 23.3a Larynx Larynx anatomy (continued) Extrinsic skeletal muscles Stabilize larynx and help it move during swallowing
- 64. 23.3a Larynx Sound production: vocal cord vibration Intrinsic laryngeal muscles narrow opening of rima glottidis Air
- 65. 23.3a Larynx Sound production (continued) Other structures are also necessary for speech Pharynx, nasal and oral
- 66. Clinical View: Laryngitis Inflammation of the larynx Symptoms of hoarse voice, sore throat, sometimes fever Caused
- 67. 23.3b Trachea Gross anatomy of trachea (windpipe) Flexible, slightly rigid, tubular organ Goes from larynx to
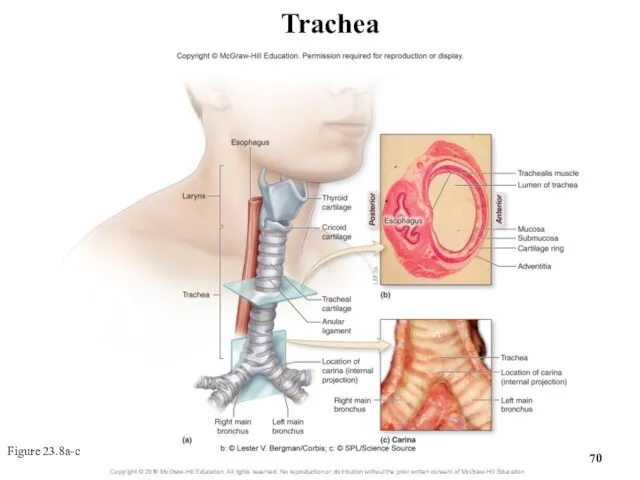
- 68. 23.3b Trachea Gross anatomy of the trachea (continued) Carina: internal ridge at inferior end of trachea
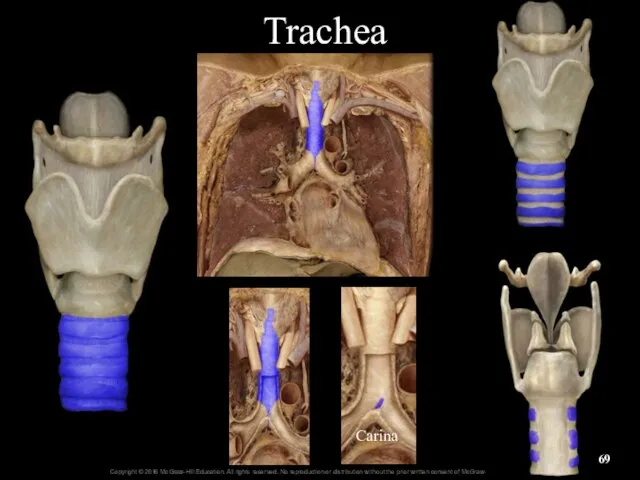
- 69. Trachea Carina
- 70. Trachea Figure 23.8a-c
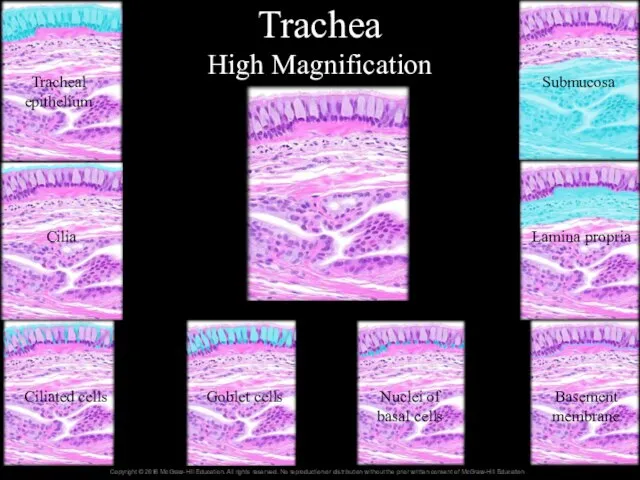
- 71. 23.3b Trachea Histology of the tracheal wall Layers, inner to outer Mucosa: pseudostratified ciliated columnar epithelium
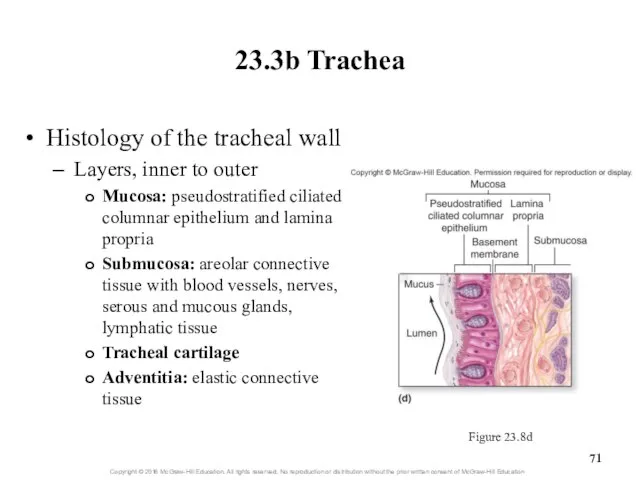
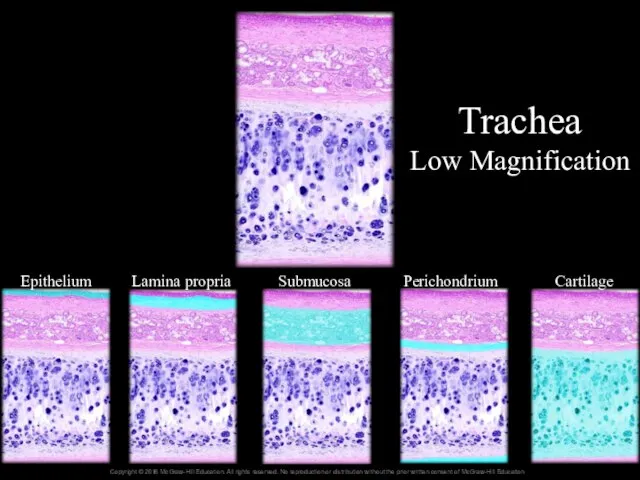
- 72. Trachea Low Magnification Epithelium Lamina propria Submucosa Perichondrium Cartilage
- 73. Trachea High Magnification Tracheal epithelium Cilia Ciliated cells Goblet cells Nuclei of basal cells Basement membrane
- 74. 23.3c Bronchial Tree Bronchial tree: system of highly branched air passages Originates at main bronchi, branches
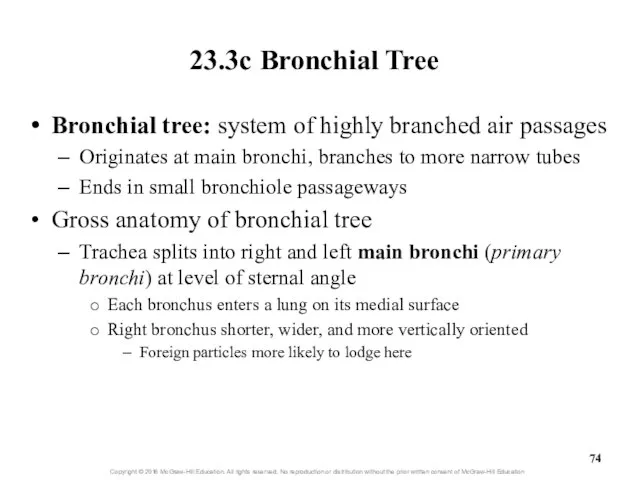
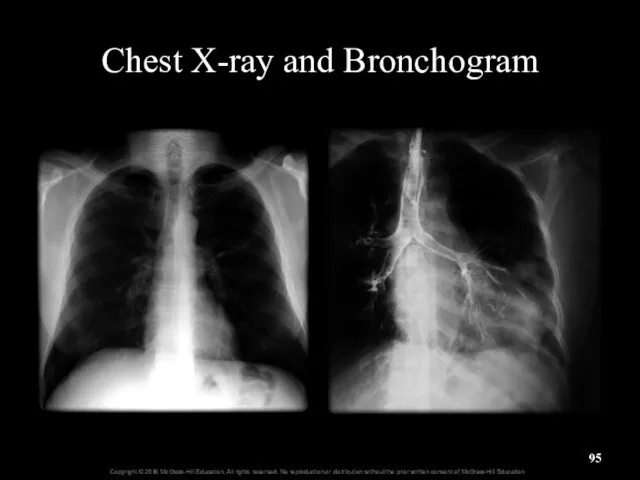
- 75. Chest X-ray and Bronchogram
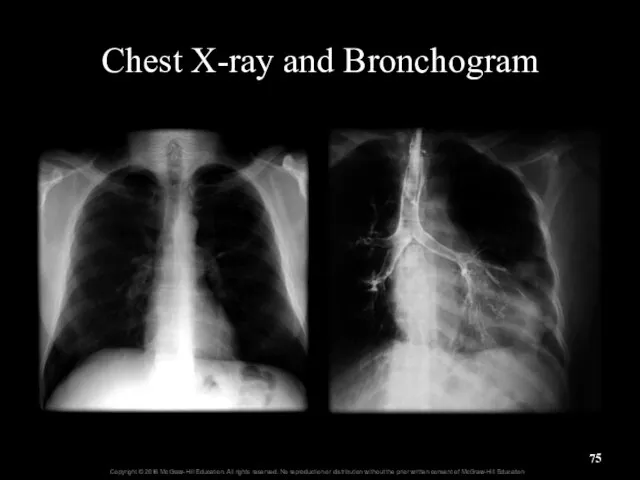
- 76. Trachea and Main (Primary) Bronchi
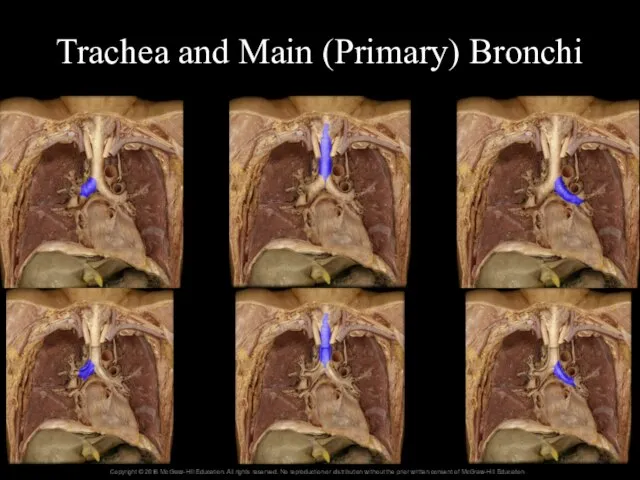
- 77. 23.3c Bronchial Tree Gross anatomy of the bronchial tree (continued) Each main bronchus branches into lobar
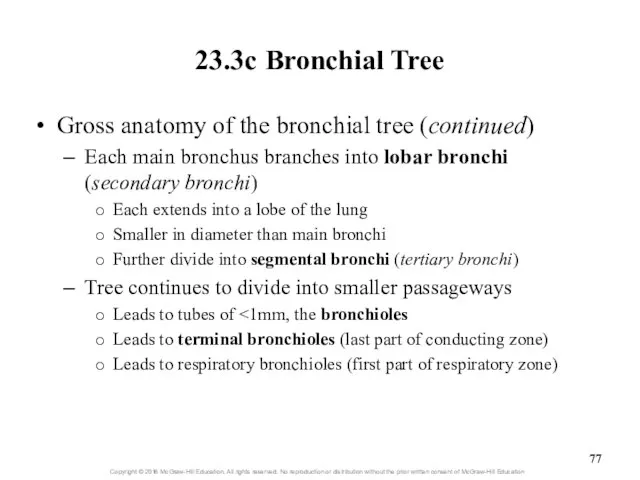
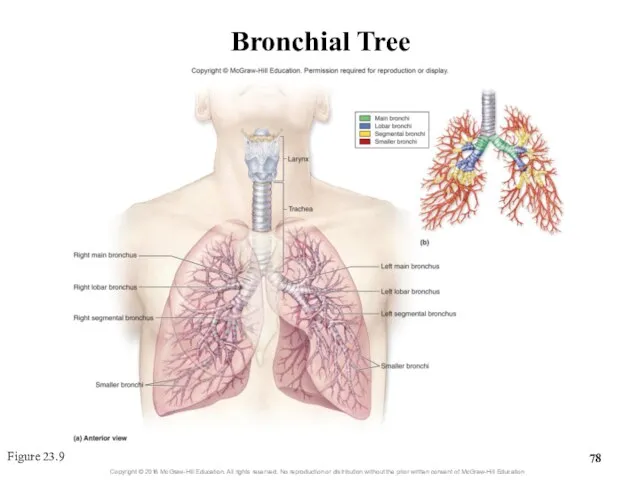
- 78. Bronchial Tree Figure 23.9
- 79. Clinical View: Bronchitis Inflammation of the bronchi caused by bacterial or viral infection or inhaled irritants
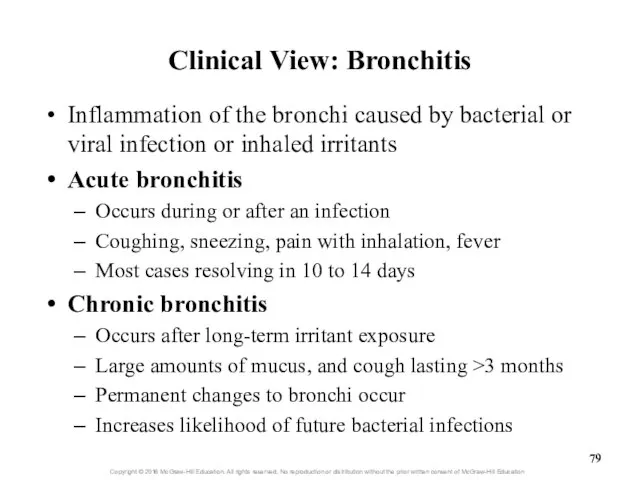
- 80. 23.3c Bronchial Tree Histology of the bronchial tree Main bronchi are supported by incomplete rings of
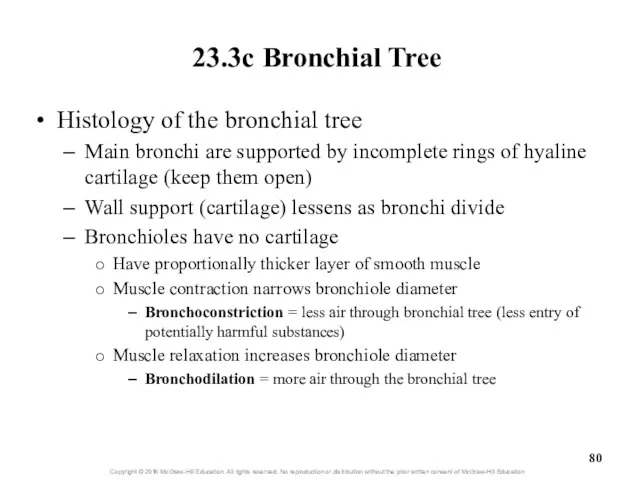
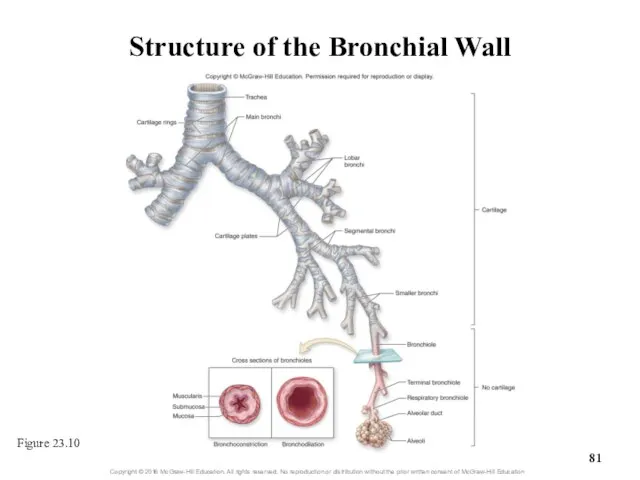
- 81. Structure of the Bronchial Wall Figure 23.10
- 82. Clinical View: Asthma Episodes of bronchoconstriction, wheezing, coughing, shortness of breath, and excess mucus Asthmatic with
- 83. 23.3d Respiratory Zone: Respiratory Bronchioles, Alveolar Ducts, and Alveoli Respiratory zone structures are microscopic Respiratory bronchioles
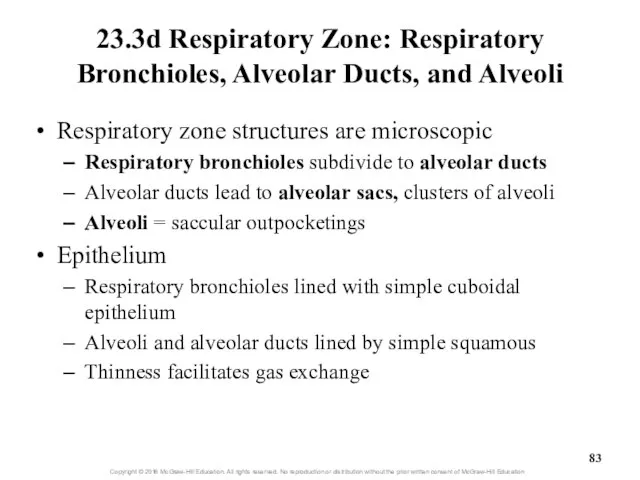
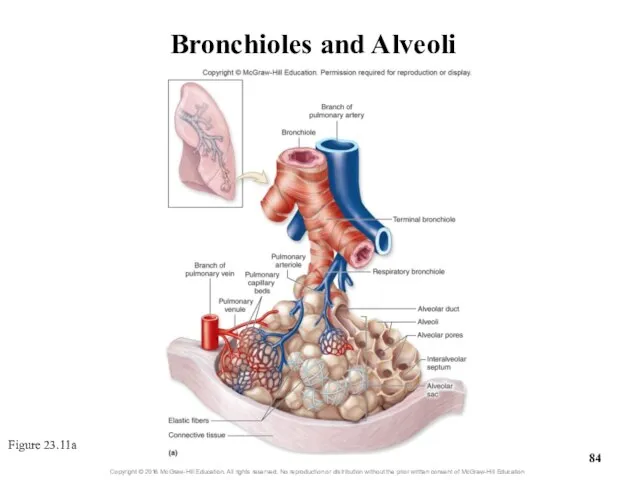
- 84. Bronchioles and Alveoli Figure 23.11a
- 85. 23.3d Respiratory Zone: Respiratory Bronchioles, Alveolar Ducts, and Alveoli Alveoli Each lung contains 300 to 400
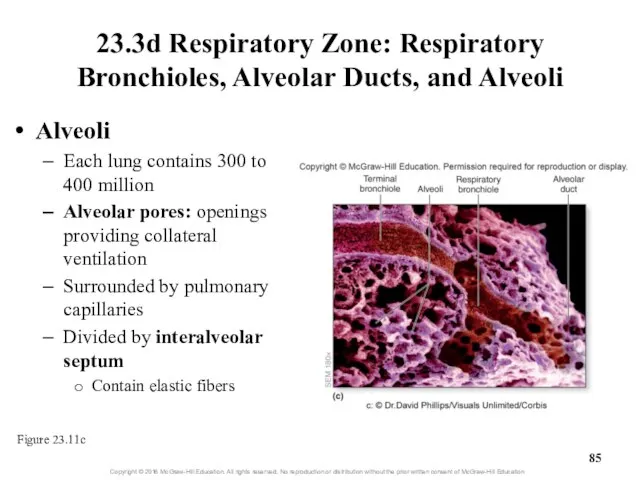
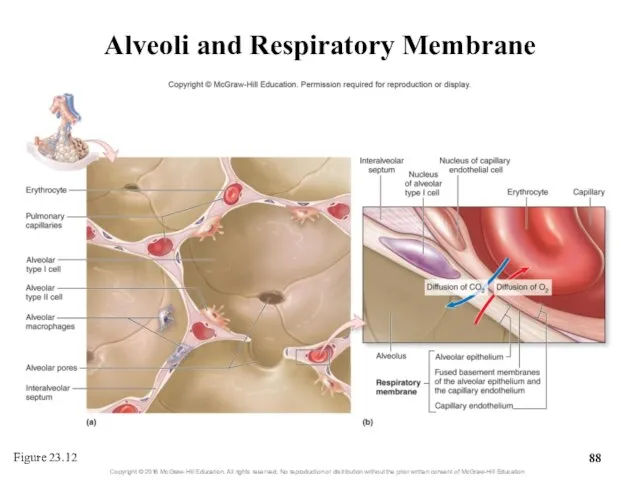
- 86. 23.3d Respiratory Zone: Respiratory Bronchioles, Alveolar Ducts, and Alveoli Cell types of alveolar wall Simple squamous
- 87. 23.3e Respiratory Membrane The respiratory membrane Thin barrier between alveoli and pulmonary capillaries Consists of Alveolar
- 88. Alveoli and Respiratory Membrane Figure 23.12
- 89. What did you learn? What makes one speech sound have a higher pitch than another? How
- 90. 23.4 Lungs Describe the location and general structure of the lungs. Compare and contrast the right
- 91. 23.4 Lungs (continued) Describe the pleural membranes and pleural cavity. Explain the function of serous fluid
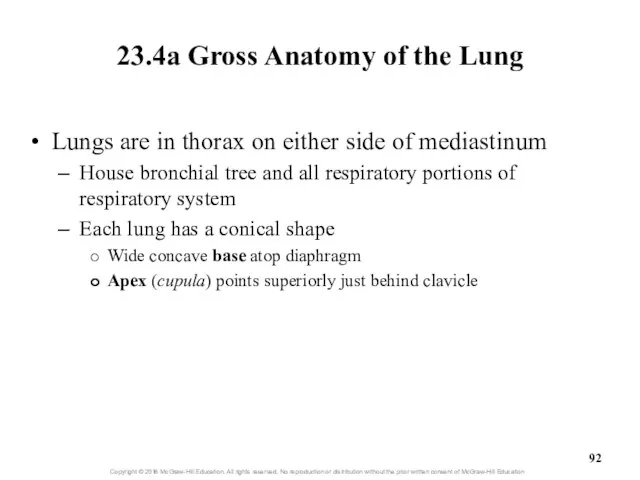
- 92. 23.4a Gross Anatomy of the Lung Lungs are in thorax on either side of mediastinum House
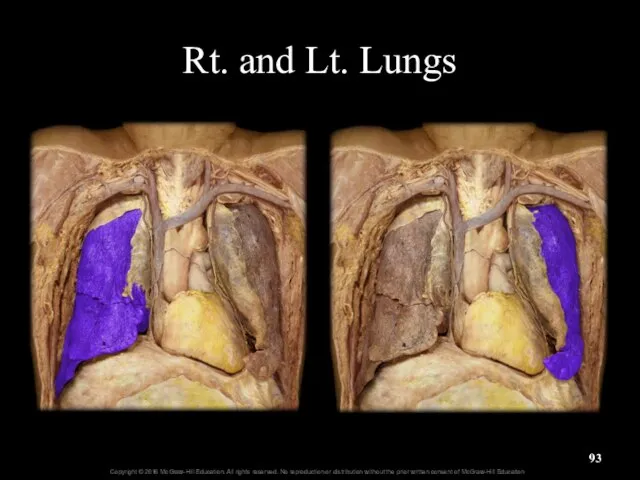
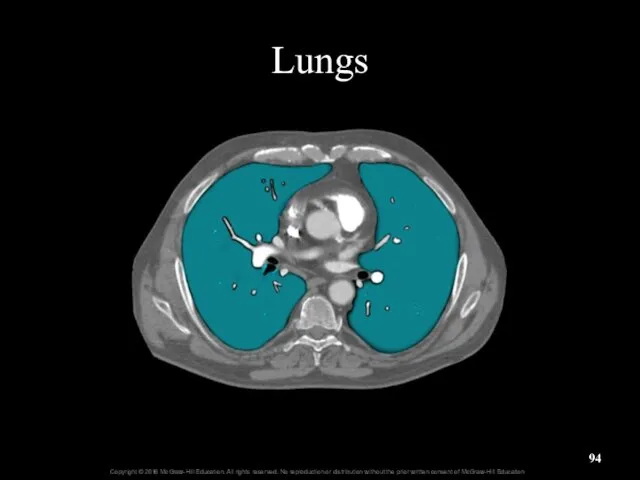
- 93. Rt. and Lt. Lungs
- 94. Lungs
- 95. Chest X-ray and Bronchogram
- 96. 23.4a Gross Anatomy of the Lung Lung surfaces Costal surface adjacent to ribs Mediastinal surface adjacent
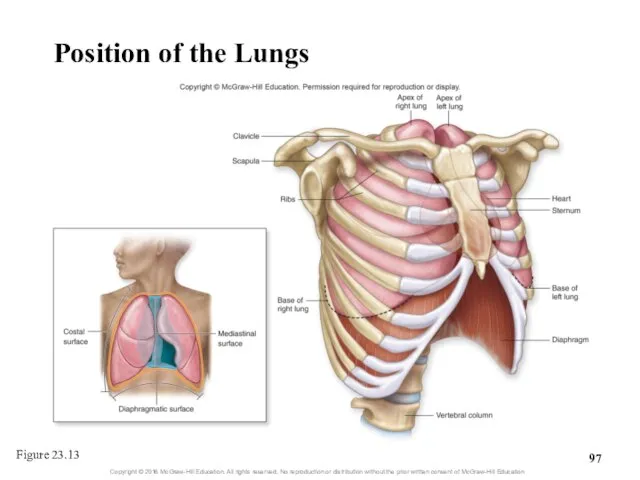
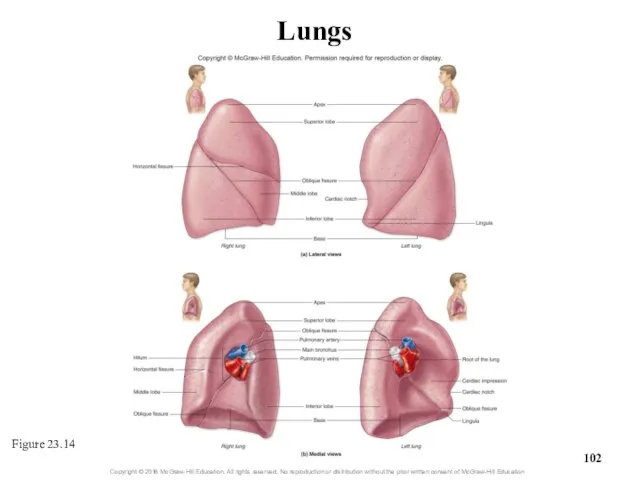
- 97. Position of the Lungs Figure 23.13
- 98. 23.4a Gross Anatomy of the Lung Right lung is larger and wider than left lung Has
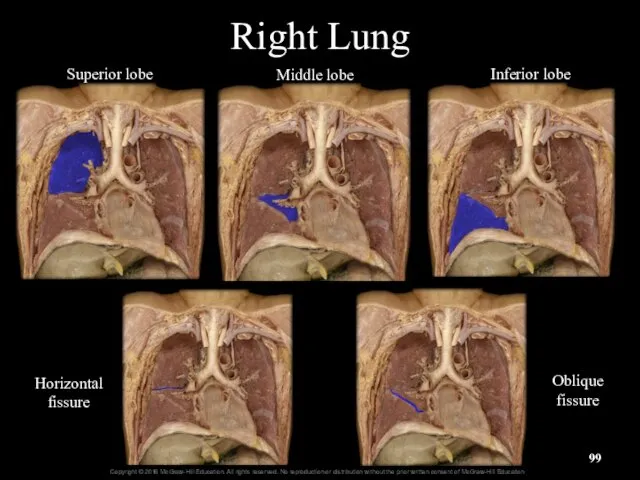
- 99. Right Lung Superior lobe Middle lobe Inferior lobe Horizontal fissure Oblique fissure
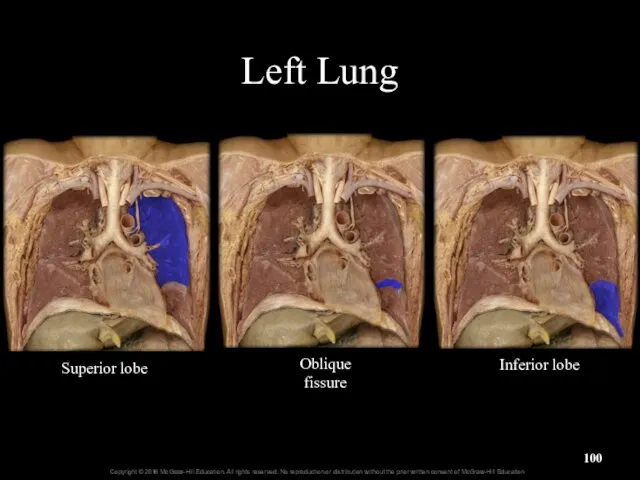
- 100. Left Lung Oblique fissure Superior lobe Inferior lobe
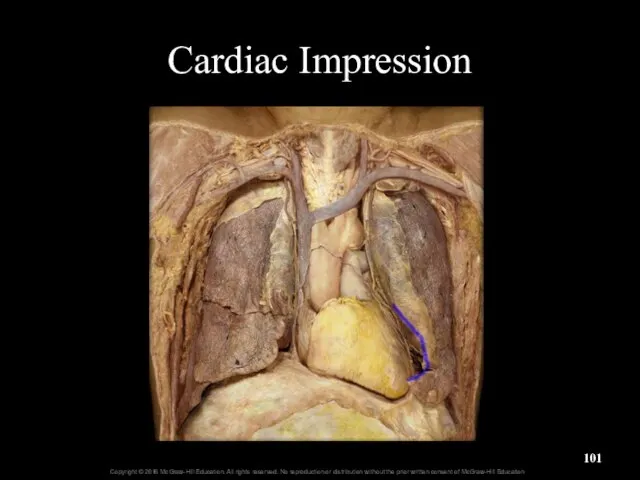
- 101. Cardiac Impression
- 102. Figure 23.14 Lungs
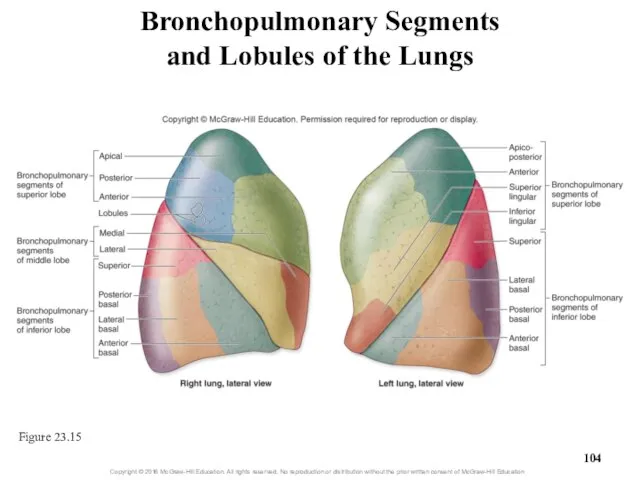
- 103. 23.4a Gross Anatomy of the Lung Each lung has multiple bronchopulmonary segments 10 segments in right
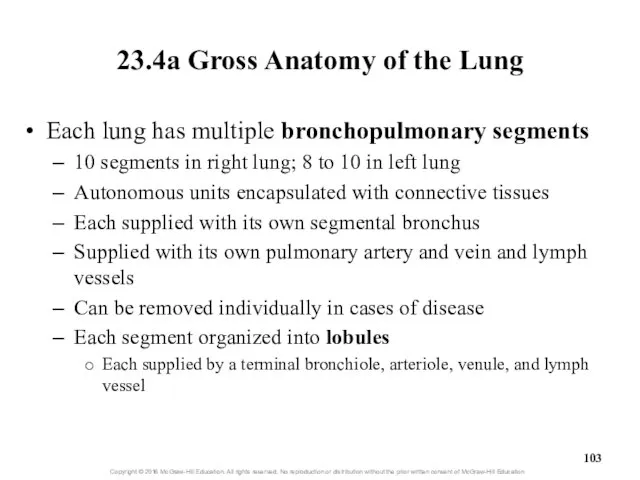
- 104. Bronchopulmonary Segments and Lobules of the Lungs Figure 23.15
- 105. Clinical View: Smoking Causes respiratory changes with increased chance of Respiratory infections Cellular or genetic changes
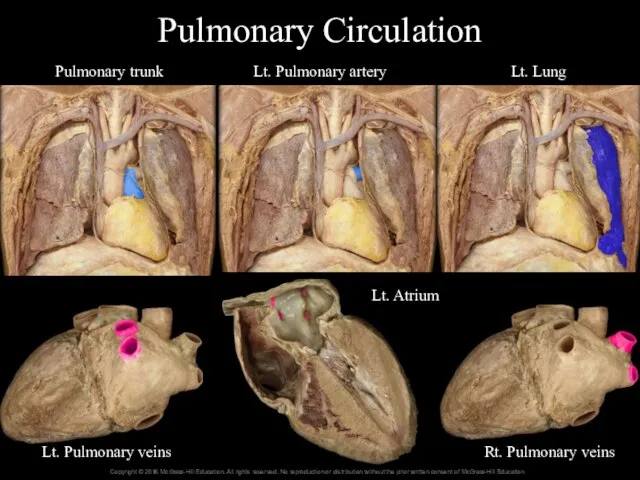
- 106. 23.4b Circulation to and Innervation of the Lungs Blood supply Two types of circulation in the
- 107. Pulmonary Circulation Pulmonary trunk Lt. Pulmonary artery Lt. Lung Lt. Pulmonary veins Rt. Pulmonary veins Lt.
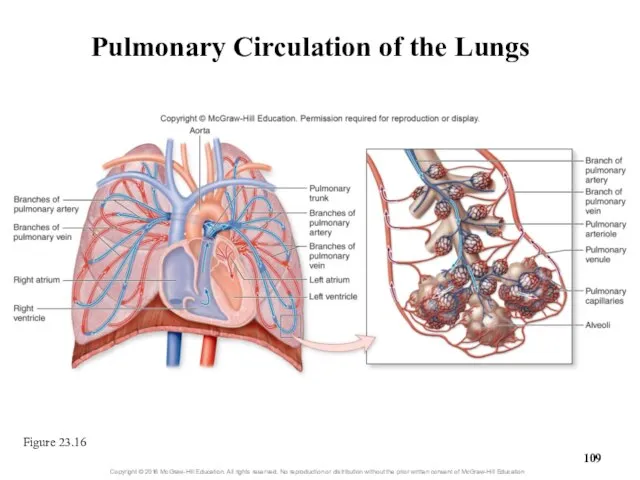
- 108. 23.4b Circulation to and Innervation of the Lungs Blood supply (continued) Bronchial circulation transports oxygenated blood
- 109. Pulmonary Circulation of the Lungs Figure 23.16
- 110. Clinical Views: Lung Cancer Highly aggressive malignancy with early metastasis Originates in respiratory epithelium Caused by
- 111. 23.4b Circulation to and Innervation of the Lungs Lymph drainage Lymph vessels and nodes located: Within
- 112. 23.4b Circulation to and Innervation of the Lungs Innervation of the respiratory system Autonomic nervous system
- 113. 23.4c Pleura Membranes and Pleural Cavity Pleura: serous membrane Outer lining of lung surfaces and adjacent
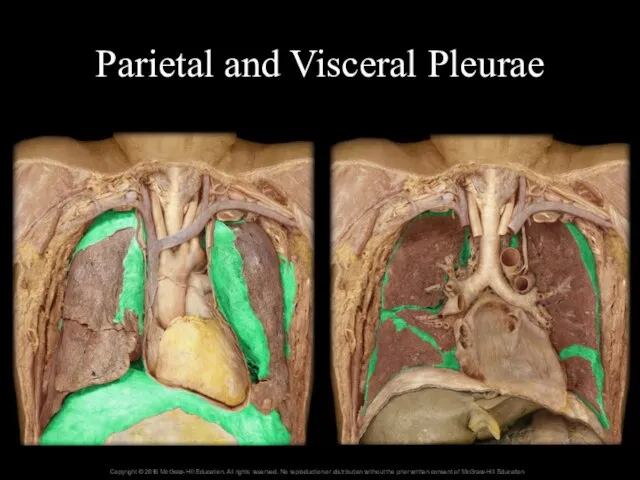
- 114. Pleura Membranes Visceral pleura Parietal pleura Pleural cavity
- 115. Parietal and Visceral Pleurae
- 116. 23.4c Pleura Membranes and Pleural Cavity Pleural cavity Located between visceral and parietal serous membranes When
- 117. Clinical View: Pleurisy and Pleural Effusion Pleurisy = inflammation of the pleural membranes Severe chest pain
- 118. 23.4d How Lungs Remain Inflated Intrapleural pressure (between membranes) is low Chest wall configured to expand
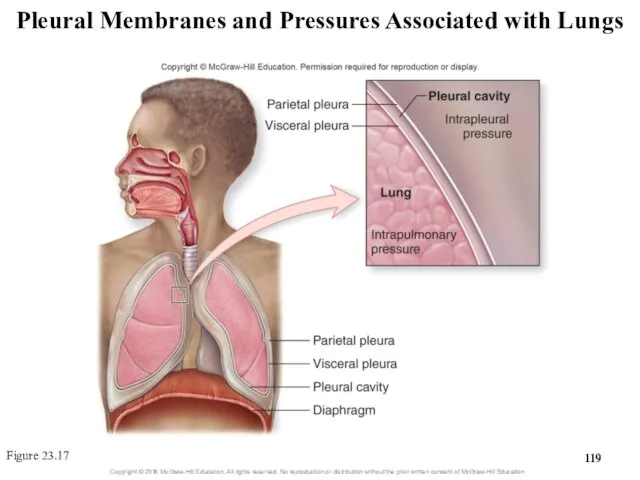
- 119. Pleural Membranes and Pressures Associated with Lungs Figure 23.17
- 120. Clinical Views: Pneumothorax and Atelectasis Pneumothorax = free air in the pleural cavity Air introduced externally—penetrating
- 122. Скачать презентацию







 Домашнее задание: Самостоятельно придумайте сюжет для анимации. Дайте ему название и подробно опишите планируемую последовател
Домашнее задание: Самостоятельно придумайте сюжет для анимации. Дайте ему название и подробно опишите планируемую последовател Язык SQL. Понятие базы данных
Язык SQL. Понятие базы данных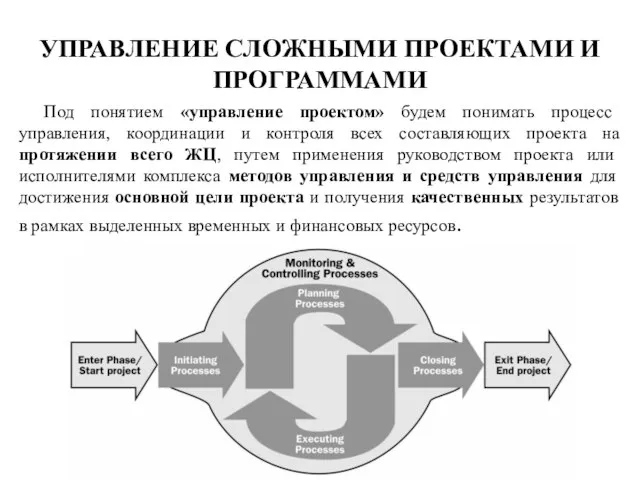 Управление сложными проектами и программами. (Лекция 3)
Управление сложными проектами и программами. (Лекция 3) Структура книги Excel
Структура книги Excel Тема урока: «Знакомство с клавиатурой» «Дорогу осилит идущий, а информатику – мыслящий» Гюстав Гийома
Тема урока: «Знакомство с клавиатурой» «Дорогу осилит идущий, а информатику – мыслящий» Гюстав Гийома Администрирование информационных систем Основы сетевого администрирования
Администрирование информационных систем Основы сетевого администрирования  Динамические структуры данных
Динамические структуры данных Существенные свойства и принятие решения.
Существенные свойства и принятие решения. «Списки» Составила: Смирнова Анна, обучающаяся 6 класса. Руководитель: Медведева Елена Валерьевна, учитель музыки и информатики.
«Списки» Составила: Смирнова Анна, обучающаяся 6 класса. Руководитель: Медведева Елена Валерьевна, учитель музыки и информатики. Информационная безопасность
Информационная безопасность Измерение и представление информации
Измерение и представление информации Пульт управления здоровьем в смартфоне
Пульт управления здоровьем в смартфоне Базовые понятия языка Си
Базовые понятия языка Си Домашнее задание по информатике
Домашнее задание по информатике Программное обеспечение
Программное обеспечение Сеть Internet
Сеть Internet Администрирование информационных систем Управление контентом веб-узла
Администрирование информационных систем Управление контентом веб-узла  Алгоритмы сжатия данных с потерями и без потерь
Алгоритмы сжатия данных с потерями и без потерь 5eb5a808-6762-48a9-a855-a31e57533794
5eb5a808-6762-48a9-a855-a31e57533794 Программа формирования УУД и ИКТ Программа формирования культуры ЗОЖ Учитель начальных классов Волкова Светлана Николаевна
Программа формирования УУД и ИКТ Программа формирования культуры ЗОЖ Учитель начальных классов Волкова Светлана Николаевна Информатика и ИКТ 10-11 класс Системы счисления
Информатика и ИКТ 10-11 класс Системы счисления  Урок-игра. «Умники и умницы»
Урок-игра. «Умники и умницы» Коллективное дело как инструмент приобретения социального и трудового опыта
Коллективное дело как инструмент приобретения социального и трудового опыта Коммуникационные операции «точка-точка» параллельное программирование
Коммуникационные операции «точка-точка» параллельное программирование  Основополагающие принципы информационного моделирования в строительстве. ISO 19650-1, 19650-2
Основополагающие принципы информационного моделирования в строительстве. ISO 19650-1, 19650-2 Текстовый процессор Word
Текстовый процессор Word Администрирование информационных систем Установка и начальная настройка SQL Server 2000
Администрирование информационных систем Установка и начальная настройка SQL Server 2000 Мультимедиа. Выходной контроль уровня овладения материалами курса (Online - тест)
Мультимедиа. Выходной контроль уровня овладения материалами курса (Online - тест)