Содержание
- 2. PLAN Introduction Pathogenesis Classification Types Conclusion
- 3. INTRODUCTION Acute myeloid leukemia (AML), also known as acute myelogenous leukemia or acute nonlymphocytic leukemia (ANLL),
- 4. Pathogenesis
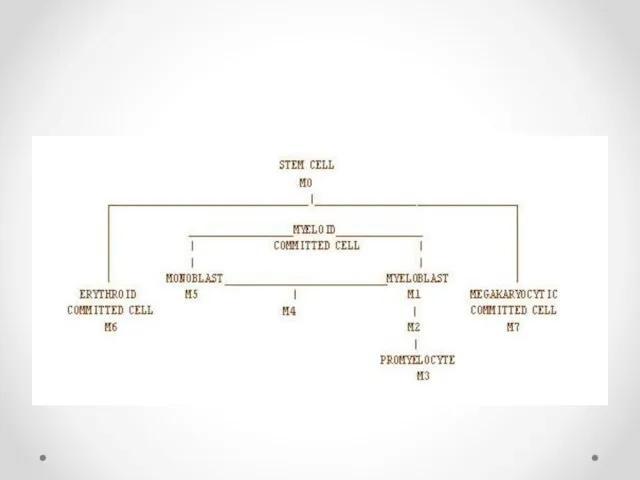
- 6. Modern classification schemes for AML recognize the characteristics and behavior of the leukemic cell (and the
- 7. Classification
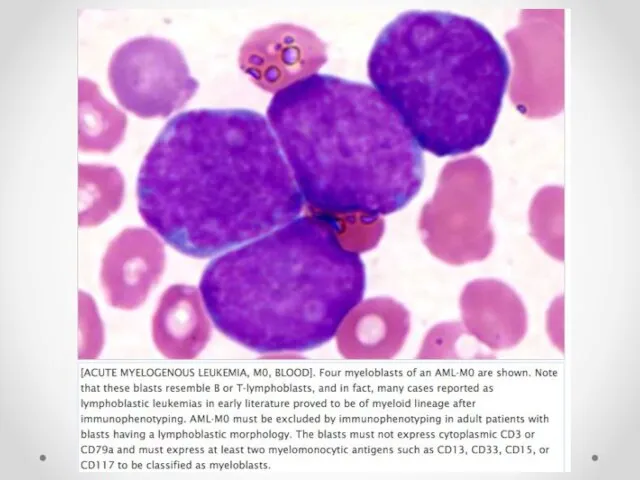
- 10. M0-M3 This scheme takes into account the degree of maturation M0 acute myeloblastic leukemia, minimally differentiated
- 11. Minimally differentiated acute myeloblastic leukemia(M0)
- 15. Acute myeloblastic leukemia without maturation(M1)
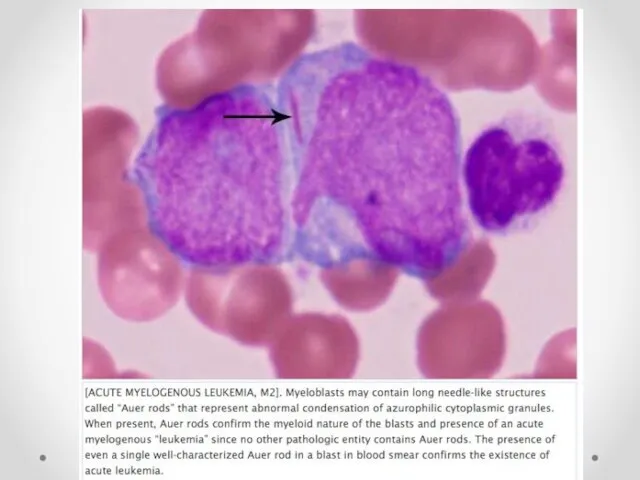
- 16. [ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. AML-M1 is defined by presence of more than 90% myeloblasts in
- 17. [ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. The defining feature of a myeloblast is fine nuclear chromatin and
- 18. [ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. Multiple myeloblasts are shown with one myeloblast containing several fine rods-like
- 19. Acute Myeloid Leukemia with Maturation (AML-M2)
- 23. Acute promyelocytic leukemia M3
- 24. [AML-M3]. Acute myelogenous leukemia, M3 type, also known as acute promyelocytic.This case illustrates hypergranular morphology with
- 25. [AML-M3].This photomicrograph shows another important morphologic feature of hypergranular type; specifically, not only intact cells with
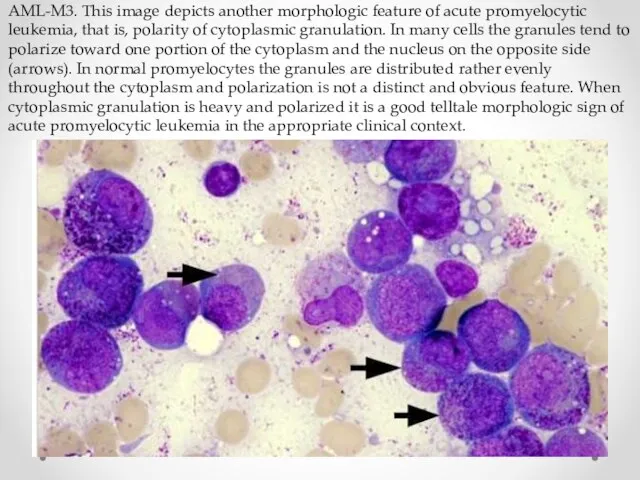
- 26. AML-M3. This image depicts another morphologic feature of acute promyelocytic leukemia, that is, polarity of cytoplasmic
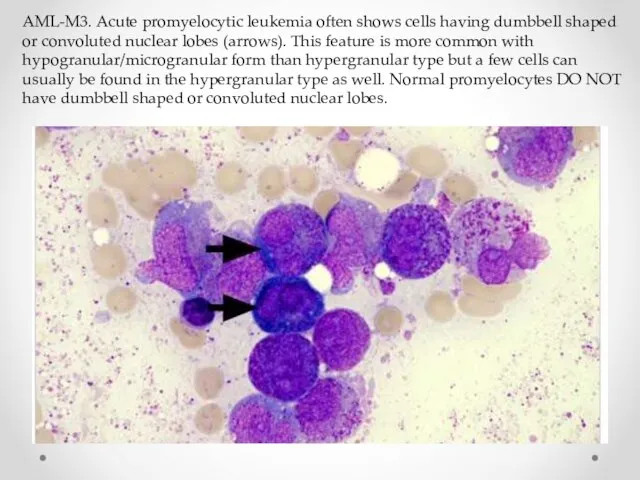
- 27. AML-M3. Acute promyelocytic leukemia often shows cells having dumbbell shaped or convoluted nuclear lobes (arrows). This
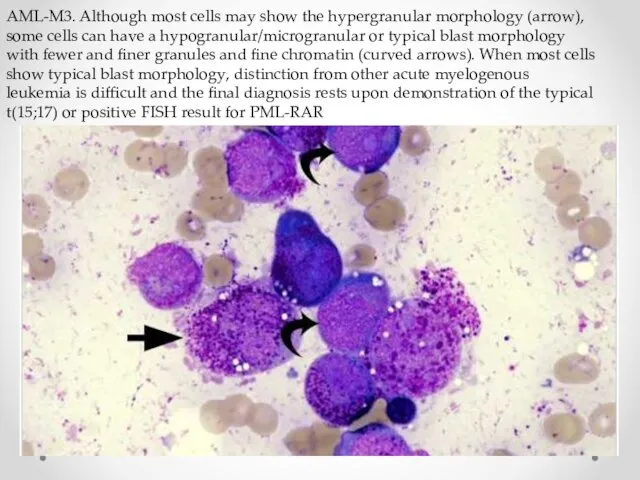
- 28. AML-M3. Although most cells may show the hypergranular morphology (arrow), some cells can have a hypogranular/microgranular
- 29. M4-M7 Lineage of the leukemic blasts: M4 acute myelomonocytic leukemia inv(16)(p13q22), del(16q) 20% M4eo myelomonocytic together
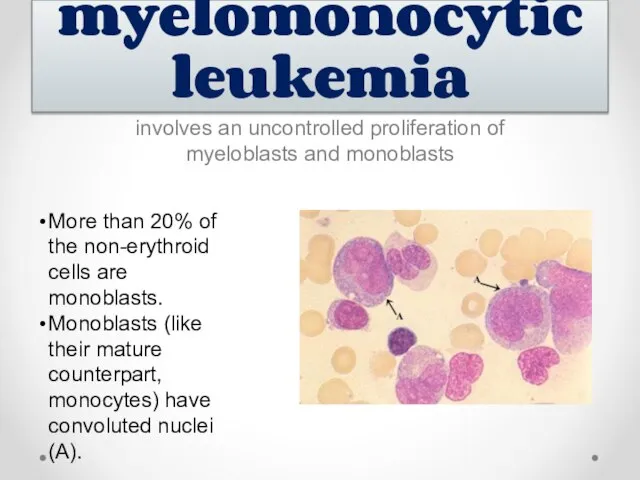
- 30. involves an uncontrolled proliferation of myeloblasts and monoblasts Acute myelomonocytic leukemia More than 20% of the
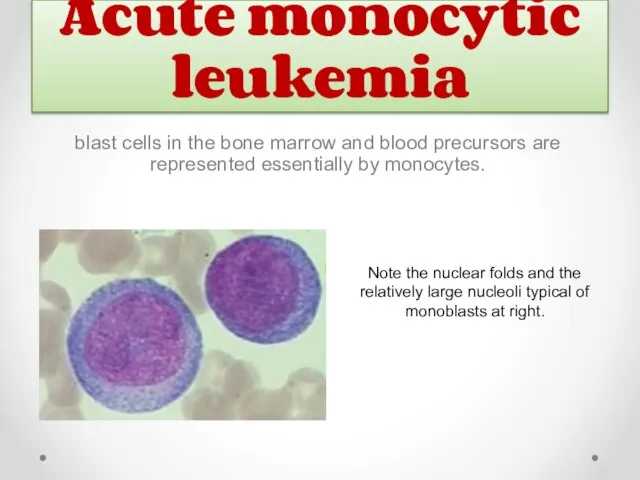
- 31. Acute monocytic leukemia Note the nuclear folds and the relatively large nucleoli typical of monoblasts at
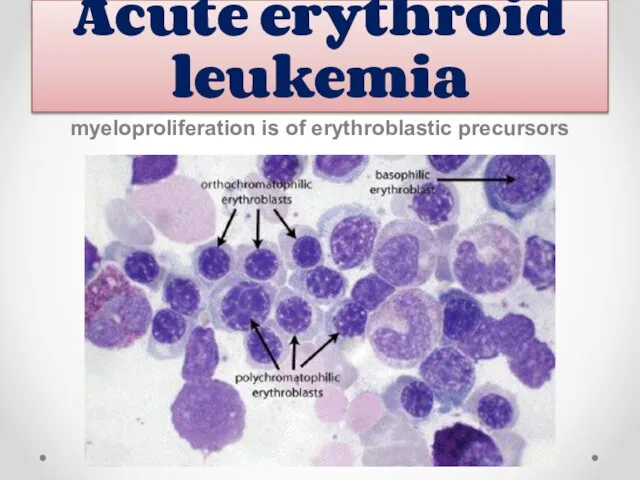
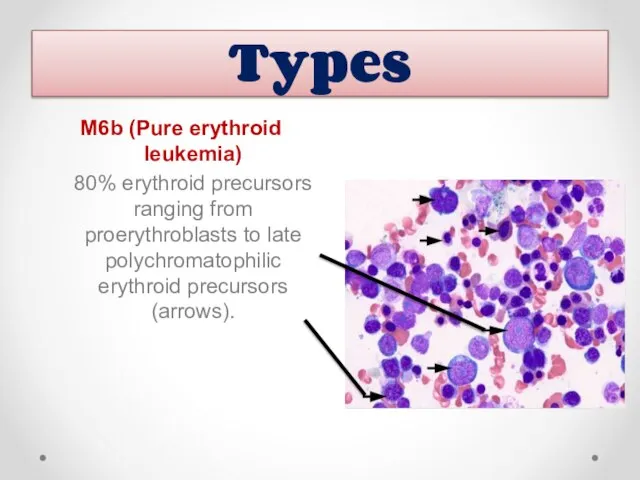
- 32. Acute erythroid leukemia myeloproliferation is of erythroblastic precursors
- 33. M6b (Pure erythroid leukemia) 80% erythroid precursors ranging from proerythroblasts to late polychromatophilic erythroid precursors (arrows).
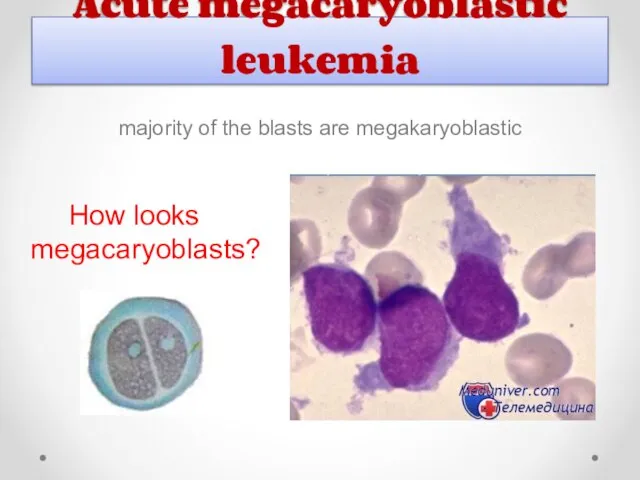
- 34. Acute megacaryoblastic leukemia majority of the blasts are megakaryoblastic How looks megacaryoblasts?
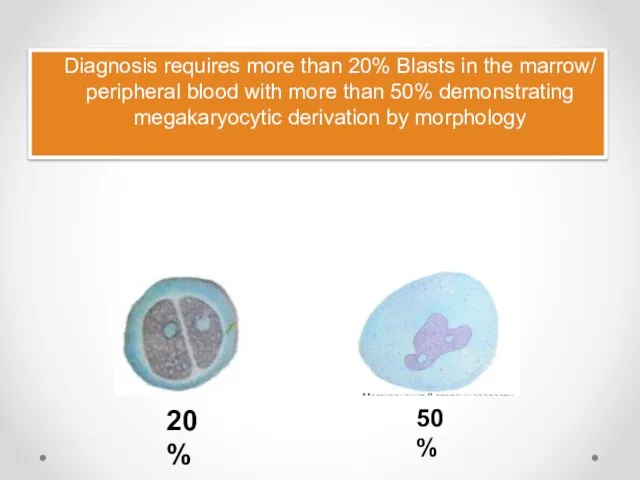
- 35. Diagnosis requires more than 20% Blasts in the marrow/ peripheral blood with more than 50% demonstrating
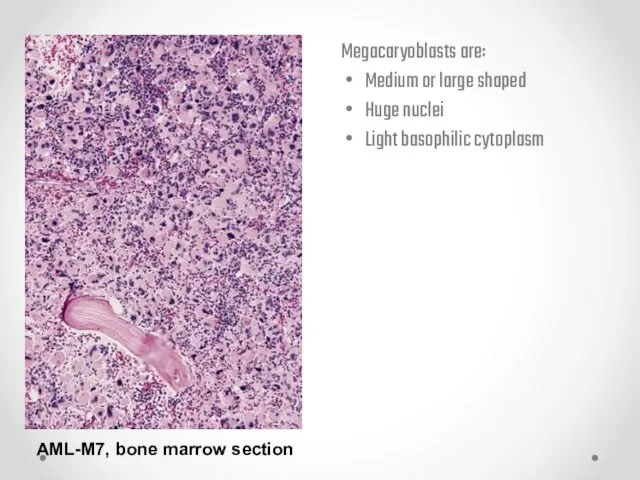
- 36. AML-M7, bone marrow section Megacaryoblasts are: Medium or large shaped Huge nuclei Light basophilic cytoplasm
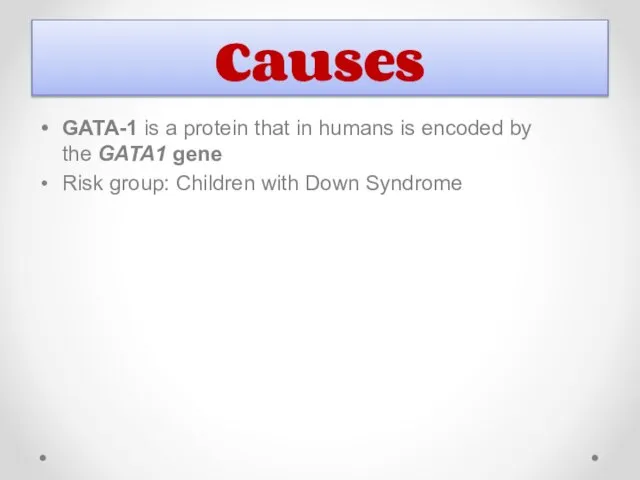
- 37. Causes GATA-1 is a protein that in humans is encoded by the GATA1 gene Risk group:
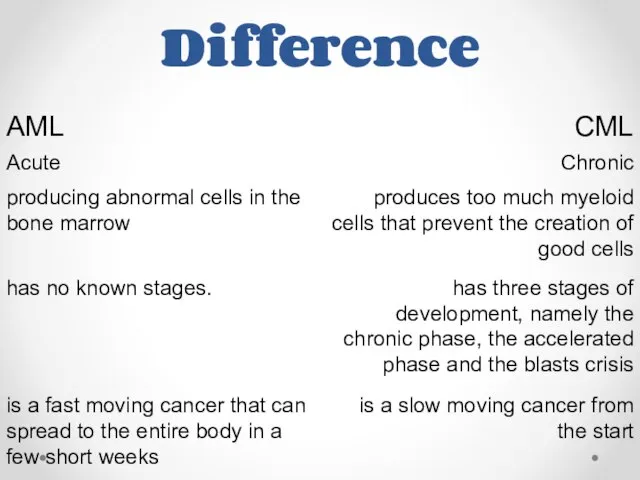
- 38. Difference
- 39. Classification is based on the type of cell from which the leukemia developed and its degree
- 41. Скачать презентацию




![[ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. AML-M1 is defined by presence of](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/532573/slide-15.jpg)
![[ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. The defining feature of a myeloblast](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/532573/slide-16.jpg)
![[ACUTE MYELOGENOUS LEUKEMIA, M1, BLOOD]. Multiple myeloblasts are shown with one](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/532573/slide-17.jpg)


![[AML-M3]. Acute myelogenous leukemia, M3 type, also known as acute promyelocytic.This](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/532573/slide-23.jpg)
![[AML-M3].This photomicrograph shows another important morphologic feature of hypergranular type; specifically,](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/532573/slide-24.jpg)
 Внутренние повреждения и заболевания коленного сустава
Внутренние повреждения и заболевания коленного сустава Безопасность использования в медицинских целях листьев подорожника, произрастающего в антропогенно нарушенных местообитаниях
Безопасность использования в медицинских целях листьев подорожника, произрастающего в антропогенно нарушенных местообитаниях Влияние окружающей среды на здоровье человека
Влияние окружающей среды на здоровье человека Eurokappa. Как работает фабрика ровных улыбок?
Eurokappa. Как работает фабрика ровных улыбок? Санитарные требования к рабочему месту технолога-эстетиста. Средства и методы дезинфекции. Средства и методы стерилизации
Санитарные требования к рабочему месту технолога-эстетиста. Средства и методы дезинфекции. Средства и методы стерилизации Профилактика короновирусной инфекции – COVID-19
Профилактика короновирусной инфекции – COVID-19 Беседа о гипер и гипогликемических состояниях
Беседа о гипер и гипогликемических состояниях Альфред Адлер
Альфред Адлер СРС: Қазақстанда тағамдық уланудың таралуы
СРС: Қазақстанда тағамдық уланудың таралуы Клиническая картина реанимации. Плановые анестезии. Экстренные анестезии. Интенсивная терапия
Клиническая картина реанимации. Плановые анестезии. Экстренные анестезии. Интенсивная терапия Набор в детский оздоровительный санаторий в г. Евпатория для детей от 10 до 14 лет,
Набор в детский оздоровительный санаторий в г. Евпатория для детей от 10 до 14 лет, Неотложные состояния в офтальмологии
Неотложные состояния в офтальмологии Диабетическая полинейропатия
Диабетическая полинейропатия Роль медицинской сестры в профилактике ожирения
Роль медицинской сестры в профилактике ожирения Инфекция. Патогенные и вирулентные свойства бактерий
Инфекция. Патогенные и вирулентные свойства бактерий Жүрек ырғағы мен өткізгіштігінің жіті бұзылыстары. Кенеттен болған өлім
Жүрек ырғағы мен өткізгіштігінің жіті бұзылыстары. Кенеттен болған өлім Берже ауруы. Созылмалы нефрит синдромы. Анықтамасы. Этиологиясы. Патогенезі. Клиникасы
Берже ауруы. Созылмалы нефрит синдромы. Анықтамасы. Этиологиясы. Патогенезі. Клиникасы Инфекционный бронхит кур
Инфекционный бронхит кур Стресс у детей
Стресс у детей Современное представление о патогенезе болезни Альцгеймера
Современное представление о патогенезе болезни Альцгеймера Перспективые направления терапии остеоартроза мультимедийный атлас к практическим занятиям кафедра госпитальной терапии
Перспективые направления терапии остеоартроза мультимедийный атлас к практическим занятиям кафедра госпитальной терапии Хронические диффузные заболевания печени: циррозы печени
Хронические диффузные заболевания печени: циррозы печени Бактериологическая диагностика туберкулеза. Молекулярно–генетические методы диагностки
Бактериологическая диагностика туберкулеза. Молекулярно–генетические методы диагностки Эмоциональный ум
Эмоциональный ум Клинический случай сочетанного туберкулеза
Клинический случай сочетанного туберкулеза AB блокада. Клиническая классификация АВ блокады
AB блокада. Клиническая классификация АВ блокады Первая медицинская помощь при термических ожогах
Первая медицинская помощь при термических ожогах Пароксизмальные расстройства сознания. Синкопальные расстройства сознания. Классификация, дифференциальная диагностика, лечение
Пароксизмальные расстройства сознания. Синкопальные расстройства сознания. Классификация, дифференциальная диагностика, лечение