Содержание
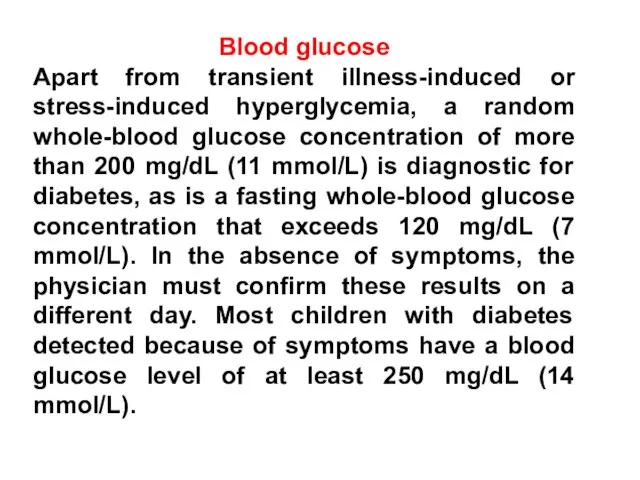
- 5. Blood glucose Apart from transient illness-induced or stress-induced hyperglycemia, a random whole-blood glucose concentration of more
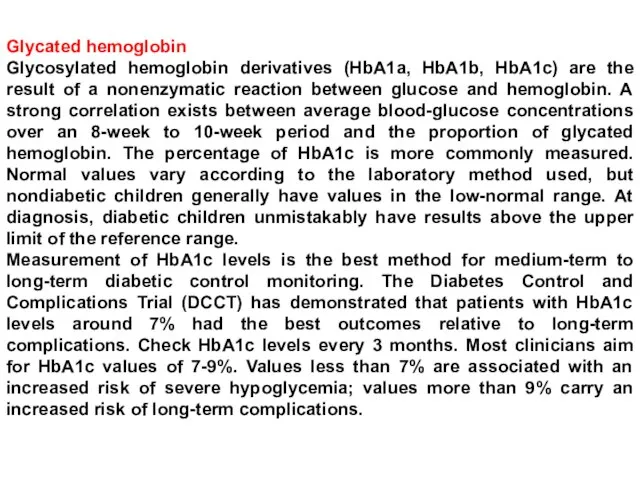
- 6. Glycated hemoglobin Glycosylated hemoglobin derivatives (HbA1a, HbA1b, HbA1c) are the result of a nonenzymatic reaction between
- 7. Islet cell antibodies Islet cell antibodies may be present at diagnosis but are not needed to
- 8. Oral glucose tolerance test (OGTT) Although unnecessary in diagnosing type 1 diabetes mellitus, an OGTT can
- 9. Long-term complications include the following: Retinopathy Cataracts Hypertension Progressive renal failure Early coronary artery disease Peripheral
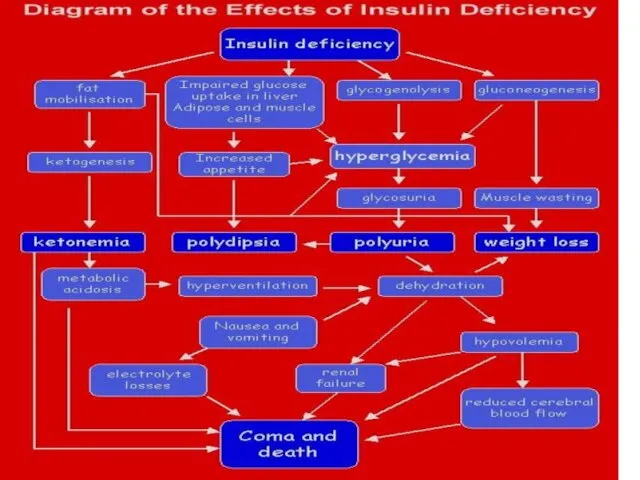
- 10. Symptoms of ketoacidosis Severe dehydration Smell of ketones Acidotic breathing (ie, Kussmaul respiration), masquerading as respiratory
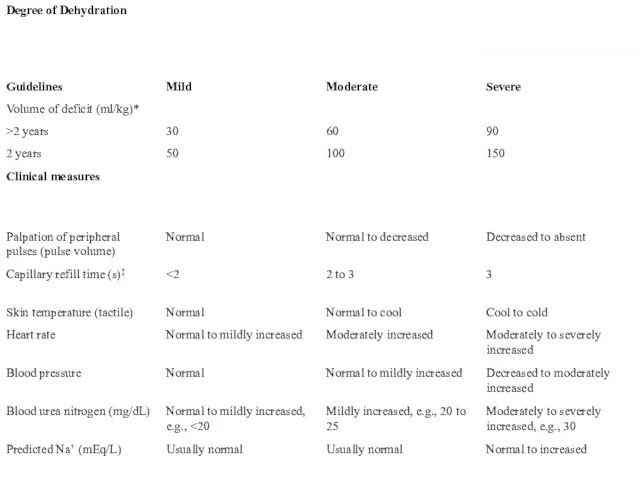
- 11. Peripheral perfusion
- 13. Скачать презентацию

 История ортодонтии
История ортодонтии Заготовка лекарственного растительного сырья (ЛРС). Правила сбора
Заготовка лекарственного растительного сырья (ЛРС). Правила сбора Антибиотики. Нежелательные эффекты химиотерапии
Антибиотики. Нежелательные эффекты химиотерапии Сборы как лекарственная форма. Требования ГФ к степени измельченности ЛРС, виды упаковки сборов. Лекция 6
Сборы как лекарственная форма. Требования ГФ к степени измельченности ЛРС, виды упаковки сборов. Лекция 6 Медицинская арахноэнтомология. Лекция 08
Медицинская арахноэнтомология. Лекция 08 Язвенная болезнь
Язвенная болезнь Вакцинопрофилактика
Вакцинопрофилактика Introduction to the Endocrine System
Introduction to the Endocrine System Основы иммунотерапии
Основы иммунотерапии Аномалии развития органов дыхания человека
Аномалии развития органов дыхания человека Повреждения грудной клетки
Повреждения грудной клетки Возрастная психология
Возрастная психология Черепно - мозговая травма
Черепно - мозговая травма презентация
презентация Холинэргические средства
Холинэргические средства Боли в сердце
Боли в сердце Острые заболевания наружного уха
Острые заболевания наружного уха Анатомия человека
Анатомия человека Фитолеум жшс өндірісінде ошаған майының өндірісін техникалық қайта жабдықтау
Фитолеум жшс өндірісінде ошаған майының өндірісін техникалық қайта жабдықтау Лекарственный препарат Эпокрин
Лекарственный препарат Эпокрин Биоритмология
Биоритмология Щитовидная железа
Щитовидная железа Мостовидные протезы
Мостовидные протезы Укусы насекомых. Консультация для родителей
Укусы насекомых. Консультация для родителей Организация онкостоматологической помощи
Организация онкостоматологической помощи Технологии оптимизации психоэмоционального состояния педагога
Технологии оптимизации психоэмоционального состояния педагога Нарушения проводимости. Атриовентрикулярные блокады. ЭКГ
Нарушения проводимости. Атриовентрикулярные блокады. ЭКГ Порушення зору
Порушення зору