Содержание
- 2. Calcium An essential intracellular and extracellular cation Extracellular calcium is required to maintain normal biological function
- 3. calcium 40-45 % ionized 40-45 % albumin bound 10% complexed citrate, sulphate 8.5–10.5 mg/dl ECF Filtration
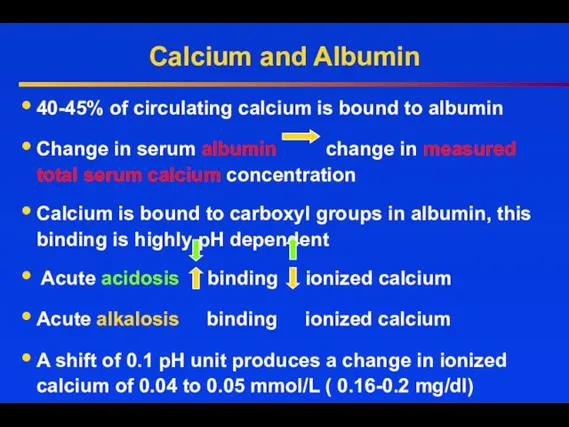
- 4. Calcium and Albumin 40-45% of circulating calcium is bound to albumin Change in serum albumin change
- 5. Calcium and Albumin At pH 7.4 each g/dl of serum albumin binds 0.8 mg/dl of calcium
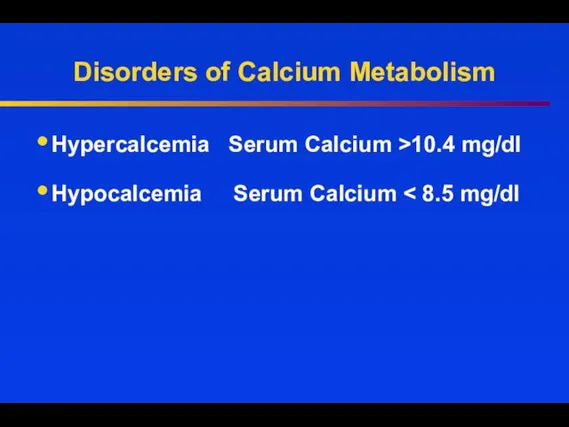
- 6. Disorders of Calcium Metabolism Hypercalcemia Serum Calcium >10.4 mg/dl Hypocalcemia Serum Calcium
- 7. Causes of hypercalcemia PTH-mediated Primary hyperparathyroidism (sporadic) –solitary adenoma or hyperplasia Familial MEN1 and -2a FHH
- 8. Causes of hypercalcemia Vitamin D intoxication Chronic granulomatous disorders: Activation of extrarenal 1 alpha-hydroxylase (increased calcitriol)
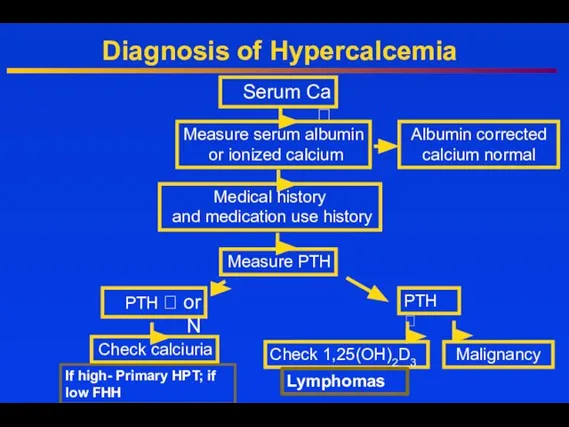
- 9. Diagnosis of Hypercalcemia Serum Ca ⭡ Measure serum albumin or ionized calcium Albumin corrected calcium normal
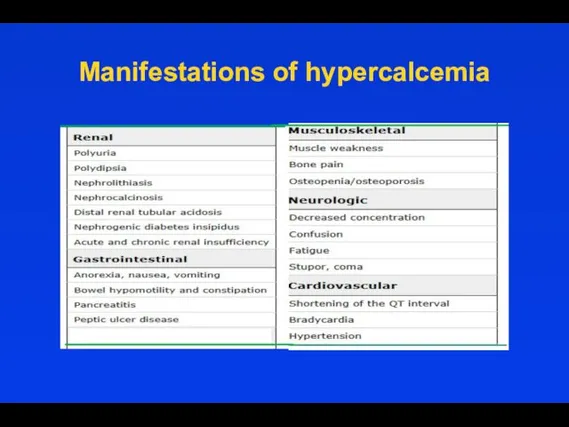
- 10. Manifestations of hypercalcemia
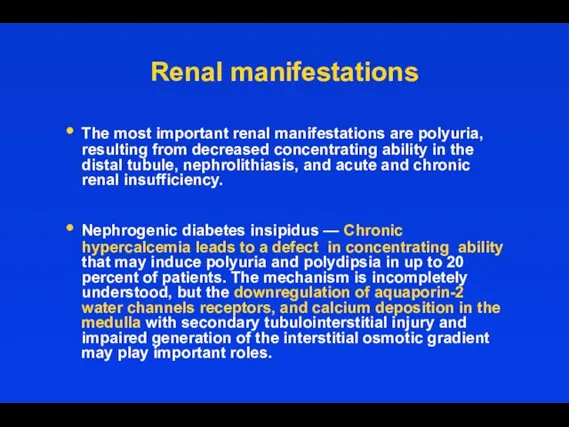
- 11. Renal manifestations The most important renal manifestations are polyuria, resulting from decreased concentrating ability in the
- 12. Renal manifestations Nephrolithiasis — When hypercalcemia is due to primary hyperparathyroidism or sarcoidosis, it is often
- 13. Gastrointestinal manifestations Nausea. Constipation may be related to decreased smooth muscle tone and/or abnormal autonomic function.
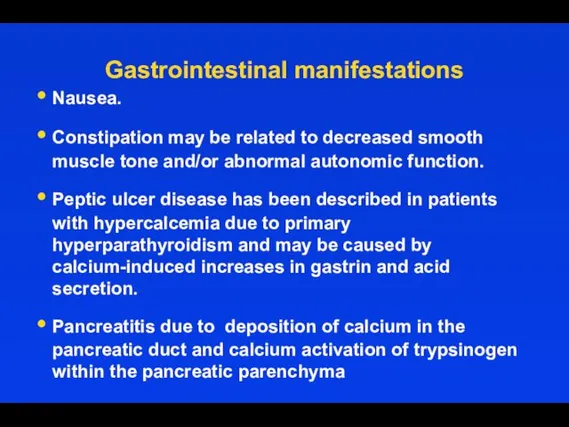
- 14. Cardiovascular symptoms Shortened QT interval Ventricular arrhythmias ST-segment elevation mimicking myocardial Long-standing hypercalcemia, as occurs in
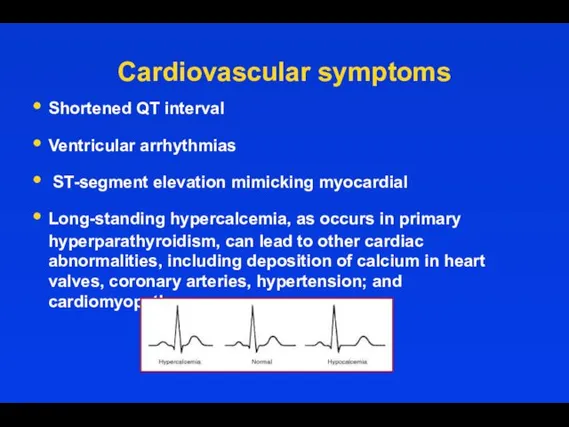
- 15. Hyperparathyroidism Secondary hyperparatroidism: due to vitamin D deficiency; renal failure Tertiary hyperparathyroidism: in longstanding renal failure
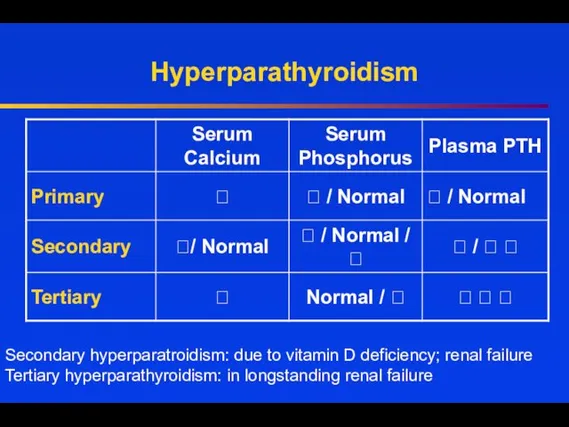
- 16. Primary Hyperparathyroidism Incidence 1/1000- 42/100 000 Postmenopausal women 1/200; ⭡ X 3.0 in women then in
- 17. or multiple adenomas, nearly 100% 15-20% up to 60% nearly 100% 30-100% 10-25%
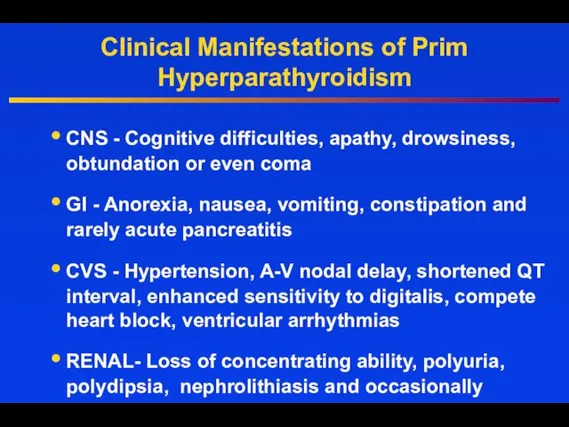
- 18. Clinical Manifestations of Prim Hyperparathyroidism CNS - Cognitive difficulties, apathy, drowsiness, obtundation or even coma GI
- 19. Bone and Joint Manifestations in Primary Hyperparathyroidism Osteoporosis Diffuse bone pain Osteitis fibrosa cystica Diffuse demineralization
- 22. Treatment When is surgery indicated in PHPT patients ?
- 23. Guidelines for Surgery
- 24. Other Considerations Neuropsychological disturbances Weakness and easy fatigability Depression Intellectual weariness Increased sleep requirements Improved by
- 25. US in the diagnosis of PTA
- 26. 99mTc- sestamibi Parathyroid Scan 20 min 3 hours 90% sensitivity in parathyroid tissue detection
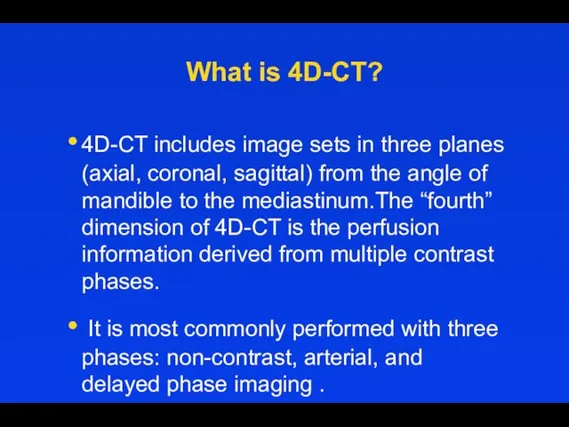
- 27. What is 4D-CT? 4D-CT includes image sets in three planes (axial, coronal, sagittal) from the angle
- 28. 4D CT in diagnosis of PHPT Arterial phase images are acquired 25 seconds after the start
- 29. Patients who weren‘t operated- Monitoring guidelines
- 30. General Measures Hydration Adequate Mobility Diet neither restrictive nor excessive in calcium Adequate vitamin D status
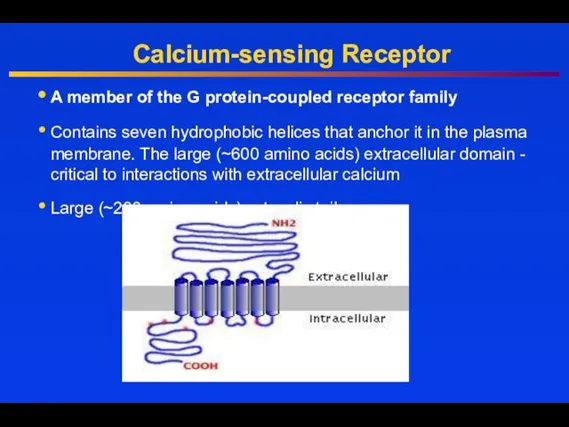
- 31. Calcium-sensing Receptor A member of the G protein-coupled receptor family Contains seven hydrophobic helices that anchor
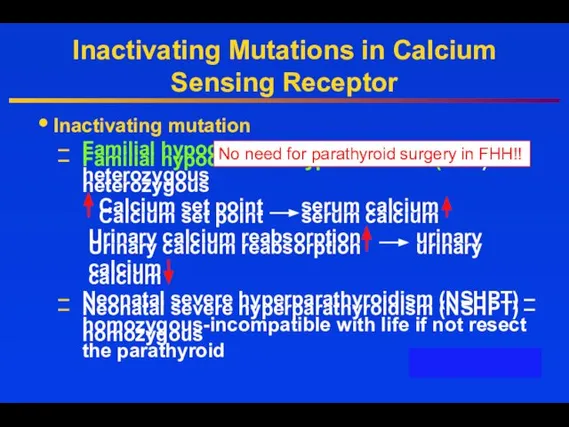
- 32. Inactivating Mutations in Calcium Sensing Receptor Inactivating mutation Familial hypocalciuric hypercalcemia (FHH) - heterozygous Calcium set
- 33. Hypercalcemia of Malignancy Lung, breast, and prostate cancer frequently invade skeleton and destroy bone tissue Damage
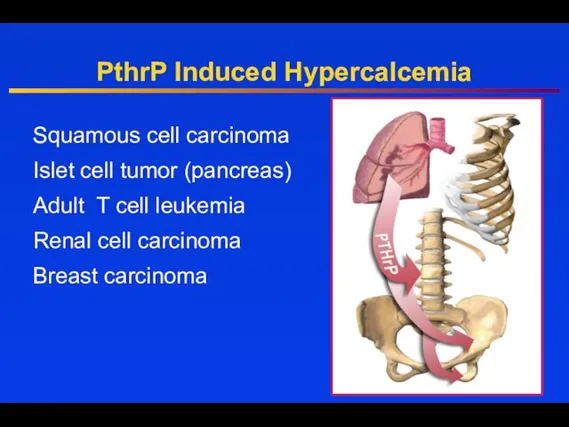
- 34. PthrP Induced Hypercalcemia Squamous cell carcinoma Islet cell tumor (pancreas) Adult T cell leukemia Renal cell
- 35. PTHrP-PTH related peptide Gen located on the chromosome 12 Gen is expressed in the embrional tissues:
- 36. Treatment Hydration Bisphosphonates IV, Denosumab Calcitonin Glucocorticoids Dialysis
- 37. Hydration First step in the management of severe hypercalcemia - Isotonic saline Usually ⭣ serum calcium
- 38. Loop Diuretics In the past intensive administration of furosemide was used (80 to 100 mg every
- 39. Calcitonin The efficacy of calcitonin (4 IU/kg every 6-12 hours) is limited to the first 48
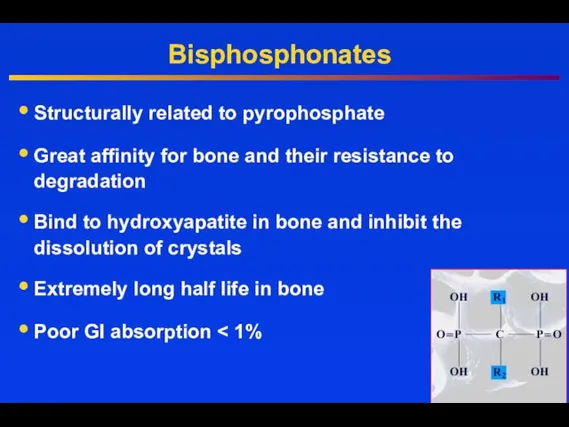
- 40. Bisphosphonates Structurally related to pyrophosphate Great affinity for bone and their resistance to degradation Bind to
- 41. Zoledronic Acid (ZOMERA) Zoledronic acid belongs to a new class of highly potent bisphosphonates Heterocyclic, nitrogen-containing
- 42. Denosumab Mechanism of Action © 2007 Amgen. All rights reserved. RANKL RANK OPG Denosumab Bone Formation
- 43. Inhibit the growth of neoplastic lymphoid tissue Counteract the effects of vitamin D Glucocorticoids
- 44. Low PTH Hypocalcemia
- 45. Hypocalcemia Low PTH (hypoparathyroidism) Genetic disorders: Abnormal parathyroid gland development Abnormal PTH synthesis; Activating mutations of
- 46. Hypocalcemia High PTH (secondary hyperparathyroidism in response to hypocalcemia) Vitamin D deficiency or resistance Parathyroid hormone
- 47. Drugs induced hypocalcemia Inhibitors of bone resorption (bisphosphonates, calcitonin, denosumab), especially in vitamin D deficiency Cinacalcet
- 48. Trousseau's sign is the induction of carpopedal spasm by inflation of a sphygmomanometer above systolic blood
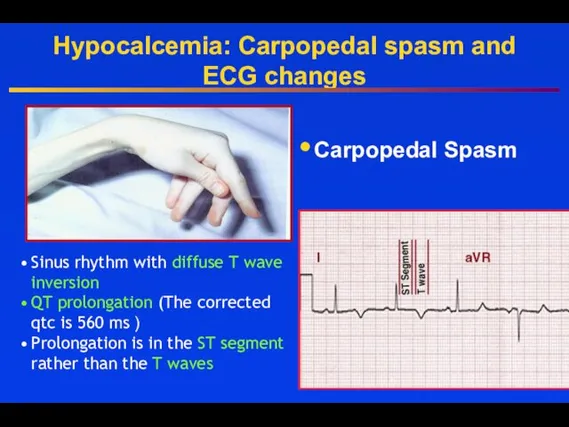
- 49. Hypocalcemia: Carpopedal spasm and ECG changes Carpopedal Spasm Sinus rhythm with diffuse T wave inversion QT
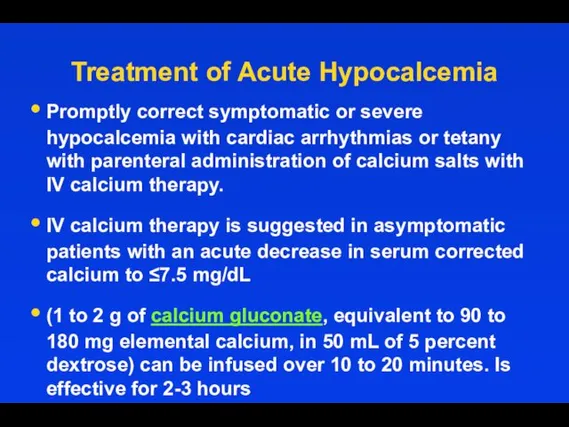
- 50. Treatment of Acute Hypocalcemia Promptly correct symptomatic or severe hypocalcemia with cardiac arrhythmias or tetany with
- 51. Treatment of Acute Hypocalcemia For those with milder symptoms of neuromuscular irritability (paresthesias) and corrected serum
- 52. To prevent Hypocalcemia due to Hungry bone syndrome Start oral calcium and vitamin D treatment early.
- 53. Primary hypoparathyroidism
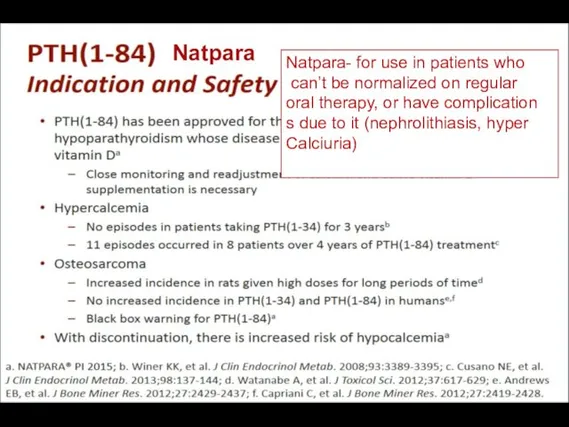
- 58. Natpara Natpara- for use in patients who can’t be normalized on regular oral therapy, or have
- 59. Causes of magnesium depletion Causes of magnesium depletion Renal losses Gasro-intestinal losses
- 60. Treatment of Hypomagnesemia If the serum magnesium concentration is low, 2 g (16 mEq) of magnesium
- 61. Treatment of Hypomagnesemia Oral repletion- if available and tolerable. A typical daily dose in a patient
- 63. Скачать презентацию




































 Окклюзионные нарушения мезентериального кровообращения
Окклюзионные нарушения мезентериального кровообращения Роль взрослого в развитии общения ребенка
Роль взрослого в развитии общения ребенка философия и медицина
философия и медицина Исследование маркеров эффективности трансляции в постуральной мышце человека в условиях 3 - суточной женской иммерсии
Исследование маркеров эффективности трансляции в постуральной мышце человека в условиях 3 - суточной женской иммерсии Венозное полнокровие. Кровоизлияния
Венозное полнокровие. Кровоизлияния Анатомо-физиологические особенности недоношенных детей
Анатомо-физиологические особенности недоношенных детей Методология консультирования женщин, идущих на прерывание беременности
Методология консультирования женщин, идущих на прерывание беременности Зудящие дерматозы
Зудящие дерматозы Биологический метод лечения пульпита. Показания, противопоказания, методика
Биологический метод лечения пульпита. Показания, противопоказания, методика Снотворные, противосудорожные (противоэпилептические, противопаркинсонические), обезболивающие ЛС
Снотворные, противосудорожные (противоэпилептические, противопаркинсонические), обезболивающие ЛС Воронкообразная деформация грудины у котёнка
Воронкообразная деформация грудины у котёнка Острая почечная недостаточность
Острая почечная недостаточность Современный подросток. Физическое здоровье (Методическое пособие)
Современный подросток. Физическое здоровье (Методическое пособие) Инфекционные заболевания
Инфекционные заболевания Проблемы защиты персональных данных в медицине
Проблемы защиты персональных данных в медицине Новорожденные щенки. Содержание, болезни, документы
Новорожденные щенки. Содержание, болезни, документы Медицинская реабилитация в гинекологии
Медицинская реабилитация в гинекологии Клиническая иммунология детского возраста
Клиническая иммунология детского возраста Проблемы нечистоплотности кошек и собак. Поведенческий и клинический аспекты
Проблемы нечистоплотности кошек и собак. Поведенческий и клинический аспекты Йогатерапия дисменореи в сочетании с варикозной болезнью нижних конечностей и малого таза
Йогатерапия дисменореи в сочетании с варикозной болезнью нижних конечностей и малого таза Учения об иммунитете
Учения об иммунитете Септический шок в акушерско-гинекологической практике
Септический шок в акушерско-гинекологической практике Современные методы хирургического лечения варикозной болезни нижних конечностей
Современные методы хирургического лечения варикозной болезни нижних конечностей Снижение смертности от болезней системы кровообращения
Снижение смертности от болезней системы кровообращения Гнойные заболевания пальцев и кисти
Гнойные заболевания пальцев и кисти ЛФК при заболеваниях дыхательной системы
ЛФК при заболеваниях дыхательной системы Эндокринология. Физиология половой дисфункции
Эндокринология. Физиология половой дисфункции Основы лечебно - эвакуационного обеспечения пораженных
Основы лечебно - эвакуационного обеспечения пораженных