Содержание
- 2. HORMONES are biologically active substances, which are produced by the cells of the endocrine system and
- 3. Types of hormone therapy 1.Specific: Substitutive (replacement therapy) Stimulating Inhibitory (suppressive) 2.Non-specific: glucocorticoids as anti-inflammatory and
- 4. Thyroid hormone 1.Calcitonin 2.Iodine-containing hormones: tetraiodothyronine (thyroxine, T4), triiodothyronine (T3).
- 5. T3, T4 are formed in the follicles of the thyroid gland by iodination of tyrosine. Peroxidase
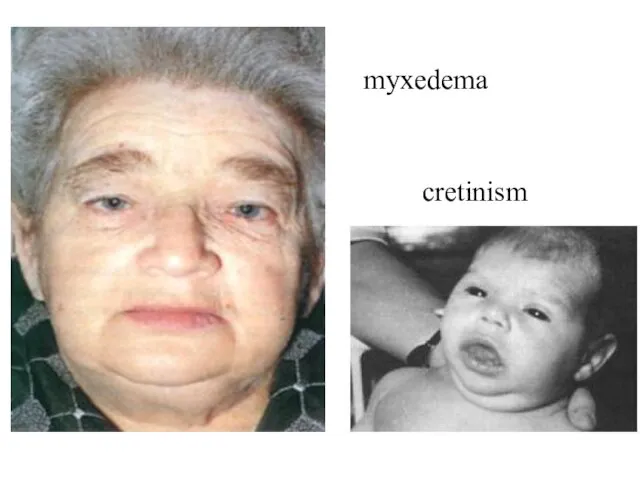
- 6. myxedema cretinism
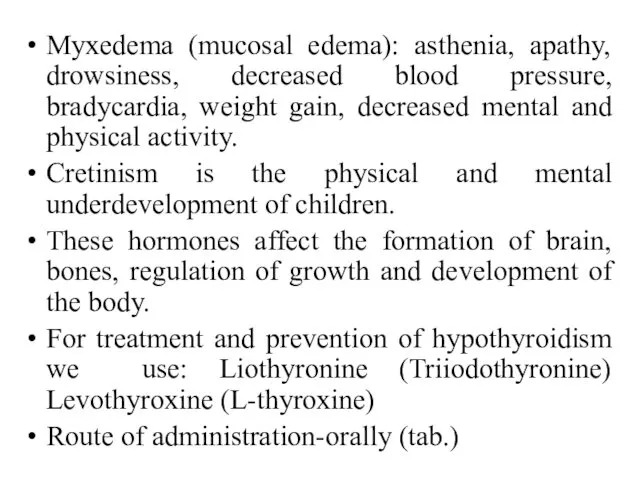
- 7. Myxedema (mucosal edema): asthenia, apathy, drowsiness, decreased blood pressure, bradycardia, weight gain, decreased mental and physical
- 8. They penetrate through the membranes of the cells. T4 is converted to T3 → penetrate into
- 10. Thyroxin effect develops gradually and reaches its maximum after 8-10 days. The effect lasts for several
- 11. Hyperthyroidism: hyperexcitability, sleep disturbance, asthenia, fervescence, tachycardia, exophthalmus, enlargement of the thyroid gland.
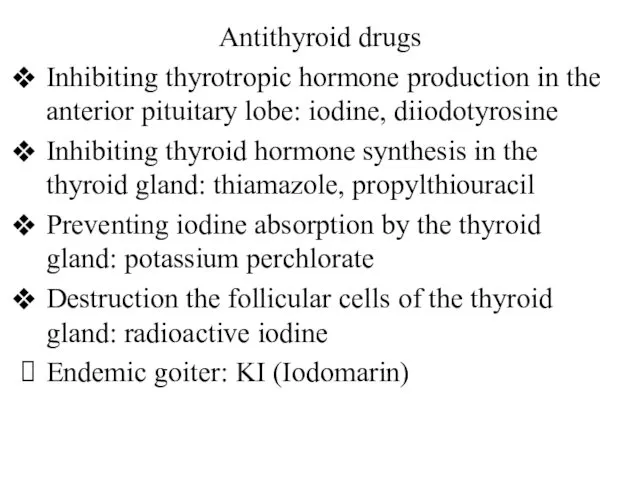
- 12. Antithyroid drugs Inhibiting thyrotropic hormone production in the anterior pituitary lobe: iodine, diiodotyrosine Inhibiting thyroid hormone
- 14. Thiamazol and carbimazole block peroxidase, reduce iodization of tyrosine, reduce the formation of mono-, diiodtyrosin, their
- 16. Calcitonin inhibits bone resorption by direct action on osteoclasts and promotes calcium deposition by osteoblasts. It
- 17. Parathormone is a polypeptide. It increases the palsma calcium level. It activates hydroxylase, which converts calcidiol
- 19. Diabetes mellitus is a metabolic disorder characterized by hyperglycaemia, glycosuria, hyperlipidaemia, negative nitrogen balance and sometimes
- 21. Insulin is a two chain polypeptide. It is synthesized in the β cells of pancreatic islets.
- 23. Insulin acts on specific receptors located on the cell membrane. There are many receptors in liver
- 25. Insulin inhibits the conversion of aminoacids into glucose (gluconeogenesis). It stimulates protein synthesis and promotes storage
- 27. Preparations of insulin: highly purified pork/beef insulins; recombinant human insulins; insulin analogues. Ultra-short-acting insulin: I. Lispro,
- 28. Average duration of action: Isophane (contains protamine) Monotard MC (contains Zn) The beginning of the effect
- 29. Insulin preparations and blood level-time curves
- 30. Combined preparation. HUMAN MIXTARD: Human soluble insulin (30%) and isophane insulin (70%), 40 U/ml. and 100
- 31. Indications for use IDDM, hyperglycemic coma, NIDDM (ineffectiveness of oral drugs, special conditions - pregnancy, operations,
- 32. Oral hypoglycaemic drugs (They are used for the treatment of type 2 diabetes mellitus) A. Enhance
- 33. B. Overcome Insulin resistance 1. Biguanide (AMPK activator)- Metformin 2. Thiazolidinediones (insulin sensitizers) -Pioglitazone C. Miscellaneous
- 34. Derivatives of sulfonylureas. Mechanism of action: Blockade of ATP-sensitive K+-channels ↓ Depolarization of the β-cells membranes
- 35. They promote the regeneration of ß cells, ↑ their number. They potentiate the action of insulin:
- 36. Repaglinide and Nateglinide are KATP channel blockers with a quick and short lasting insulinemic action. They
- 37. Metformin ↓absorption of glucose from the intestine, ↑ its uptake by the muscles, ↑ glycolysis, ↓gluconeogenesis,
- 39. Glucagon-like peptide-1 (GLP-1) is an important incretin released from the gut in response to ingested glucose.
- 40. Exenatide is a synthetic DPP-4 resistant analogue of GLP-1 and activates its receptors. It is injected
- 41. Acarbose is a blocker of α-glucosidase. It ↓digestion and absorption of carbohydrates in the small intestine.
- 43. Скачать презентацию



















 Фізіологічна та окулярна оптика. Обладнання та інструменти для стоматології
Фізіологічна та окулярна оптика. Обладнання та інструменти для стоматології Порядок обследования больного животного
Порядок обследования больного животного Асқазан қыжылы
Асқазан қыжылы Творим своё здоровье. Осанка
Творим своё здоровье. Осанка Новые технологии и их применение в области трансформации социально-личностных установок для достижения индивидуальных целей
Новые технологии и их применение в области трансформации социально-личностных установок для достижения индивидуальных целей Нарушения зрения
Нарушения зрения Профилактика гриппа и ОРВИ
Профилактика гриппа и ОРВИ Өндірістегі шаңдану және газданудың гигиеналық нормалау мен бағалау және олардың алдын-алу әдістері. (Тақырып 7)
Өндірістегі шаңдану және газданудың гигиеналық нормалау мен бағалау және олардың алдын-алу әдістері. (Тақырып 7) Обследование слуховой дифференциации фонем
Обследование слуховой дифференциации фонем Инфаркт миокарда, патанатомия, осложнения, причины смерти. Взаимоотношение атеросклероза и ИБС
Инфаркт миокарда, патанатомия, осложнения, причины смерти. Взаимоотношение атеросклероза и ИБС Паразитизм, патогенность и паразитарные системы
Паразитизм, патогенность и паразитарные системы Екстремальні умови з психологічних позицій
Екстремальні умови з психологічних позицій Кардиомиопатии
Кардиомиопатии Травмы мягких тканей и костей лица. Клиника, диагностика, лечение
Травмы мягких тканей и костей лица. Клиника, диагностика, лечение Здоровье - это состояние полного физического, социального и психического благополучия
Здоровье - это состояние полного физического, социального и психического благополучия Многоплодная беременность
Многоплодная беременность Экзаменационный билет. Препараты
Экзаменационный билет. Препараты Денсаулық жағдайының ауытқулары мен даму ақаулары бар балалар мен жасөспірімдерге арналған мекемелерде
Денсаулық жағдайының ауытқулары мен даму ақаулары бар балалар мен жасөспірімдерге арналған мекемелерде Табиғи ошақтардың қалыптасу факторы мен жағдайы
Табиғи ошақтардың қалыптасу факторы мен жағдайы Асептика и антисептика. Стерилизация перевязочного материала и хирургического белья автоклавированием. Подготовка рук
Асептика и антисептика. Стерилизация перевязочного материала и хирургического белья автоклавированием. Подготовка рук Средства действующие на ЦНС
Средства действующие на ЦНС Общ психотерапевтичен подход в обгрижването на пациентите
Общ психотерапевтичен подход в обгрижването на пациентите Общие понятия о здоровье как основной ценности человека
Общие понятия о здоровье как основной ценности человека Раны. Классимфикации
Раны. Классимфикации Национальные особенности деловой культуры европейских стран
Национальные особенности деловой культуры европейских стран Биорезонансноая терапия аллергических заболеваний
Биорезонансноая терапия аллергических заболеваний Болезни челюстных костей. Одонтогенная инфекция. Сепсис
Болезни челюстных костей. Одонтогенная инфекция. Сепсис Acute and chronic glomerulonephritis
Acute and chronic glomerulonephritis