Содержание
- 3. Otitis Externa Inflammation of the external auditory canal Most common in children 7-14 years old Risk
- 4. Otitis Externa Diagnosis: clinical, otoscopy, culture (for refractory cases), imaging (mastoiditis) Treatment: Clean the ear canal
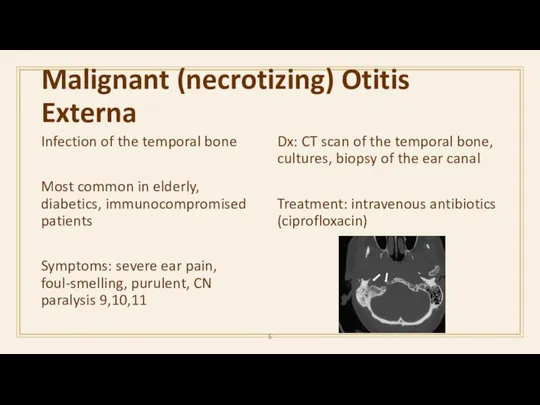
- 5. Malignant (necrotizing) Otitis Externa Infection of the temporal bone Most common in elderly, diabetics, immunocompromised patients
- 6. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
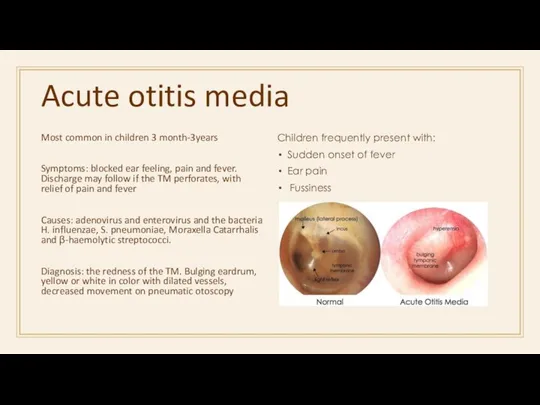
- 7. Acute otitis media Most common in children 3 month-3years Symptoms: blocked ear feeling, pain and fever.
- 9. Acute otitis media Treatment Analgesics to relieve pain Adequate rest in a warm room Nasal decongestants
- 10. Acute otitis media Complications: Conductive hearing loss Sensorineural hearing loss Tympanic membrane perforation Retraction pocket Mastoiditis
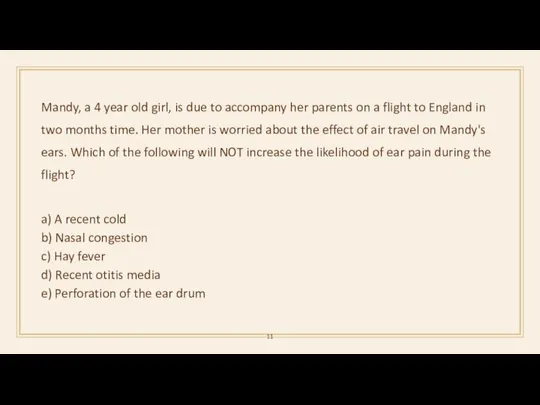
- 11. Mandy, a 4 year old girl, is due to accompany her parents on a flight to
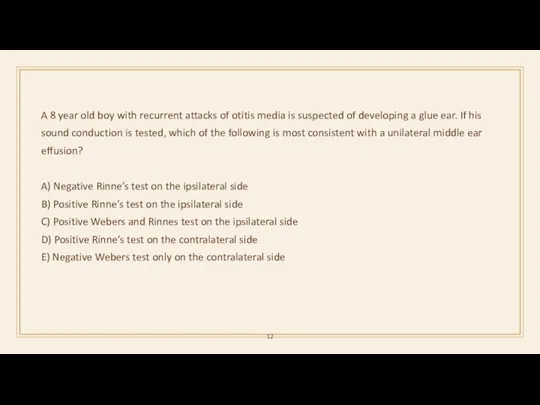
- 12. A 8 year old boy with recurrent attacks of otitis media is suspected of developing a
- 13. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
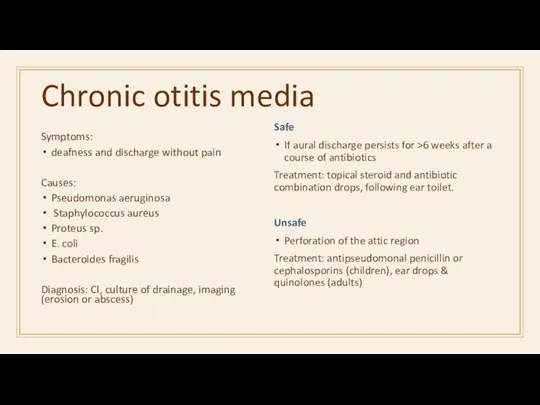
- 14. Chronic otitis media Symptoms: deafness and discharge without pain Causes: Pseudomonas aeruginosa Staphylococcus aureus Proteus sp.
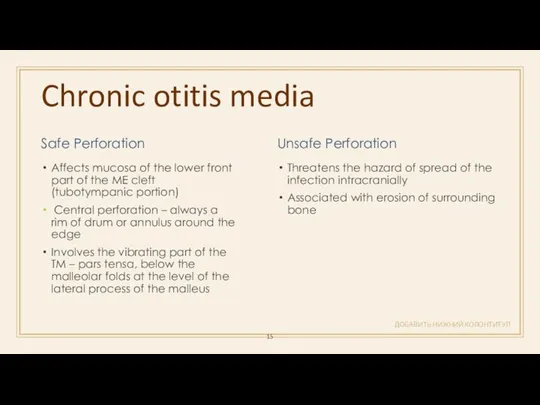
- 15. Chronic otitis media ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Safe Perforation Affects mucosa of the lower front part of
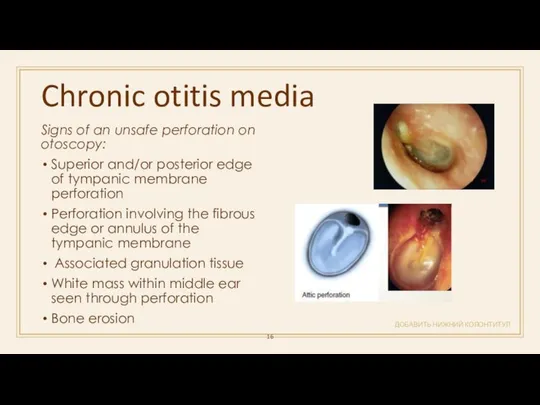
- 16. Chronic otitis media ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Signs of an unsafe perforation on otoscopy: Superior and/or posterior
- 17. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ A 14-year old teenager is diagnosed with a tympanic membrane perforation secondary to
- 18. Cholesteatoma ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Expanding lesions of the temporal bone composed of a stratified squamous outer
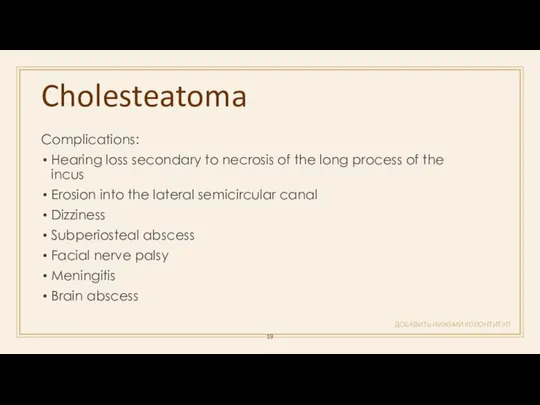
- 19. Cholesteatoma ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Complications: Hearing loss secondary to necrosis of the long process of the
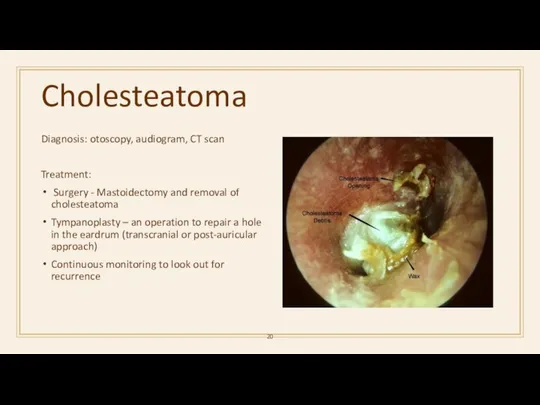
- 20. Cholesteatoma Diagnosis: otoscopy, audiogram, CT scan Treatment: Surgery - Mastoidectomy and removal of cholesteatoma Tympanoplasty –
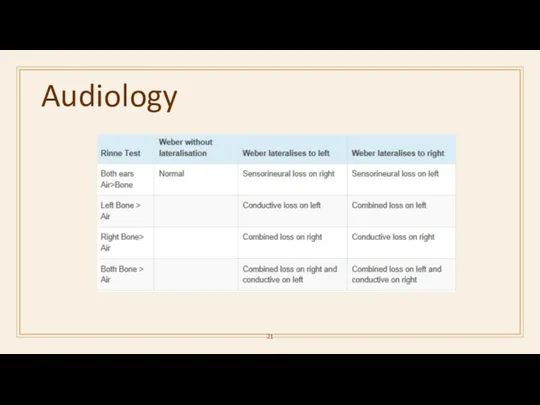
- 21. Audiology
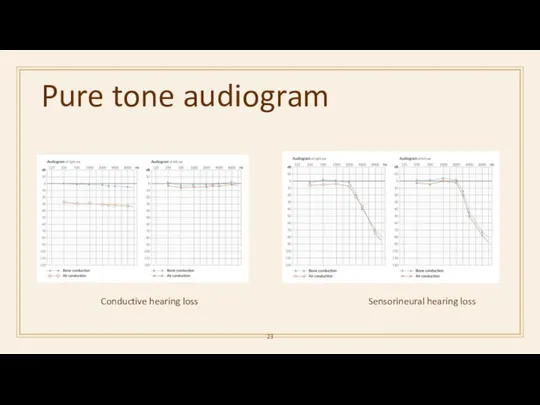
- 23. Pure tone audiogram Sensorineural hearing loss Conductive hearing loss
- 24. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ This pure tone audiogram is recorded from a 12 year old Maori girl
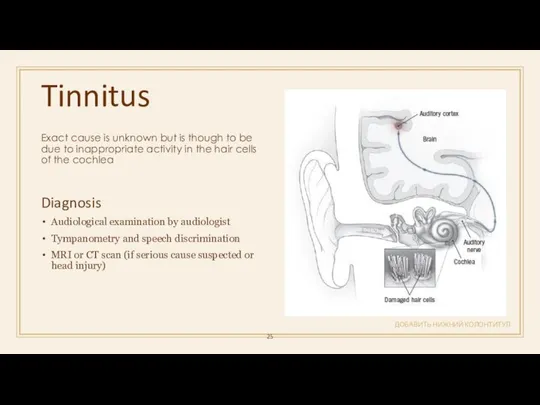
- 25. Tinnitus ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Exact cause is unknown but is though to be due to inappropriate
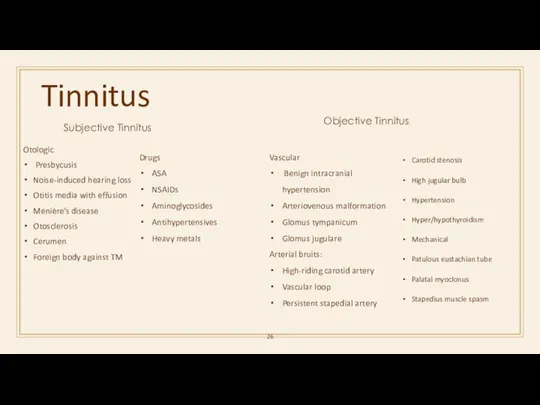
- 26. Tinnitus Subjective Tinnitus Otologic Presbycusis Noise-induced hearing loss Otitis media with effusion Menière’s disease Otosclerosis Cerumen
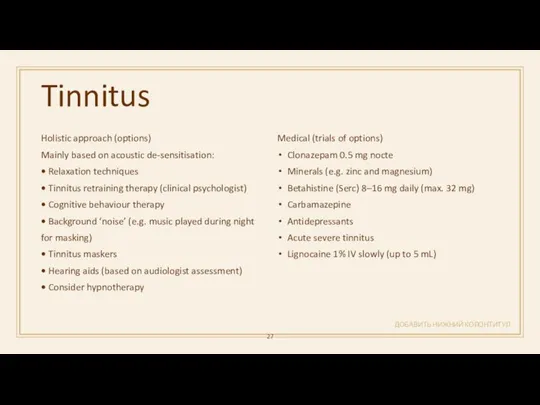
- 27. Tinnitus ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Holistic approach (options) Mainly based on acoustic de-sensitisation: • Relaxation techniques •
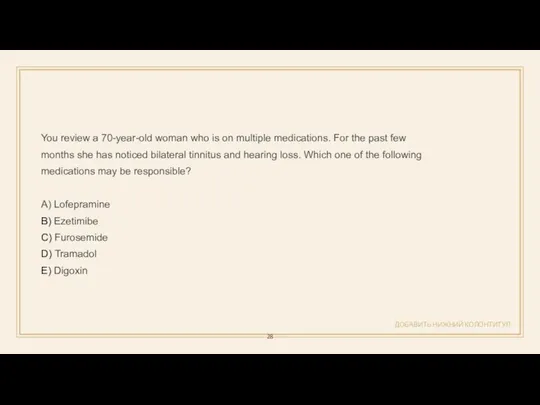
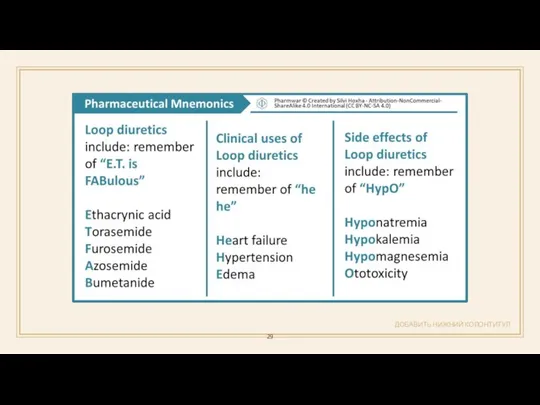
- 28. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ You review a 70-year-old woman who is on multiple medications. For the past
- 29. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
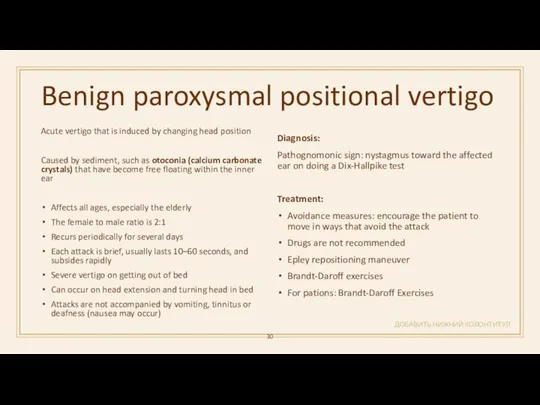
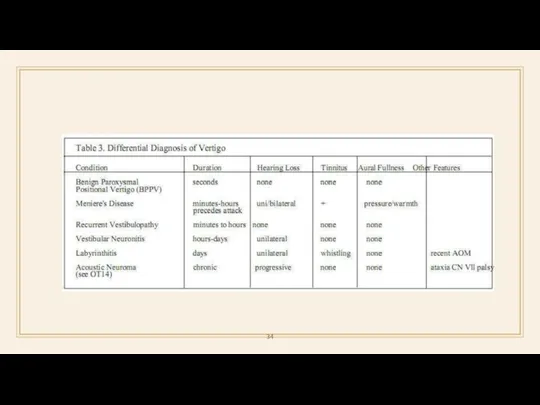
- 30. Benign paroxysmal positional vertigo ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Acute vertigo that is induced by changing head position
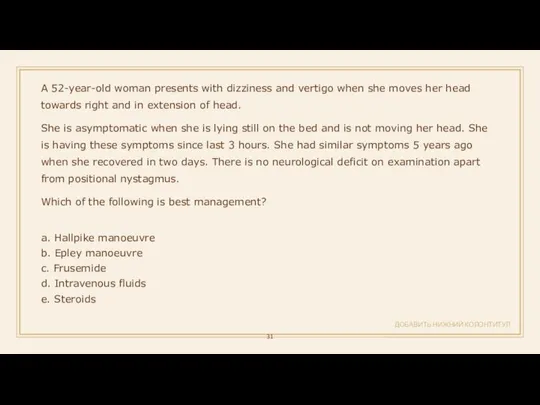
- 31. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ A 52-year-old woman presents with dizziness and vertigo when she moves her head
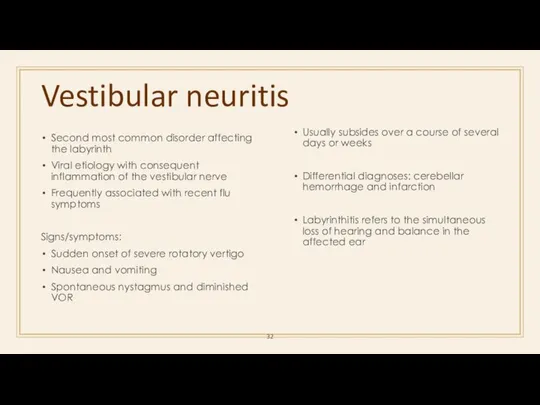
- 32. Vestibular neuritis Second most common disorder affecting the labyrinth Viral etiology with consequent inflammation of the
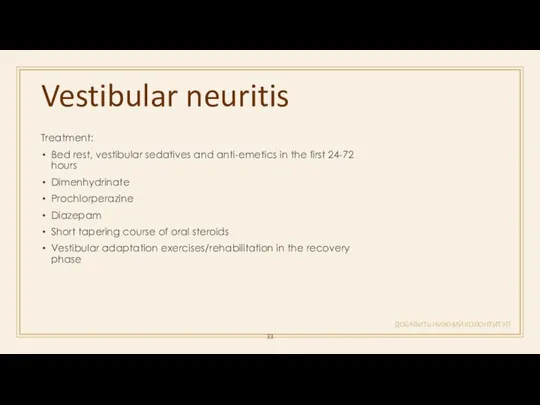
- 33. Vestibular neuritis ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Treatment: Bed rest, vestibular sedatives and anti-emetics in the first 24-72
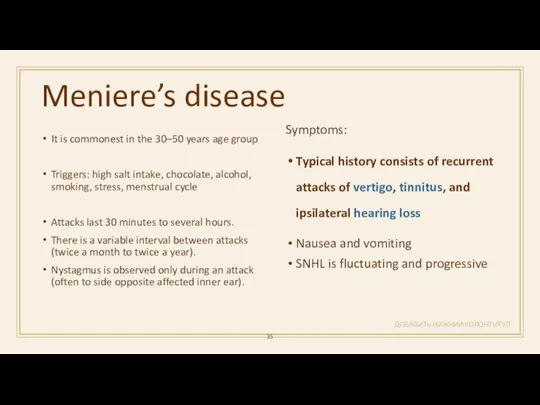
- 35. Meniere’s disease ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ It is commonest in the 30–50 years age group Triggers: high
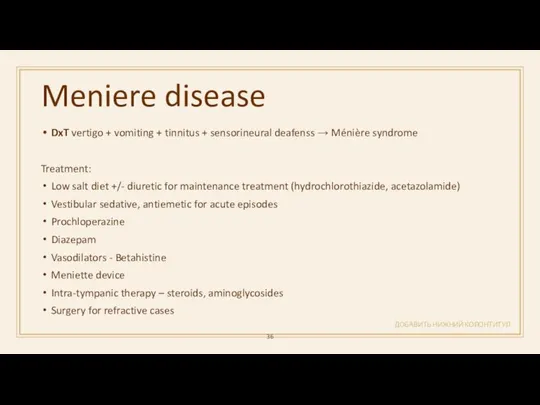
- 36. Meniere disease ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ DxT vertigo + vomiting + tinnitus + sensorineural deafenss → Ménière
- 37. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ An elderly patient has acute onset unilateral deafness, tinnitis & vertigo. What is
- 38. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ A 39-year-old woman arrives at the hospital after her third episode of dizziness.
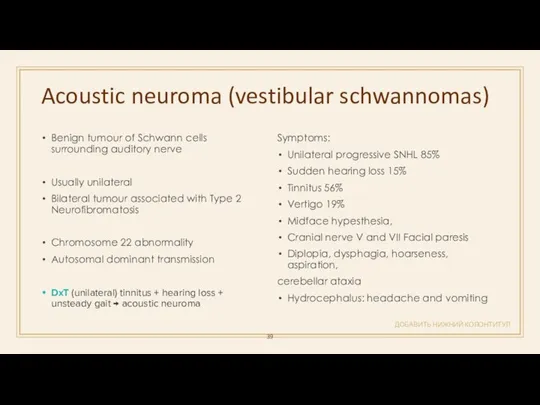
- 39. Acoustic neuroma (vestibular schwannomas) ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Benign tumour of Schwann cells surrounding auditory nerve Usually
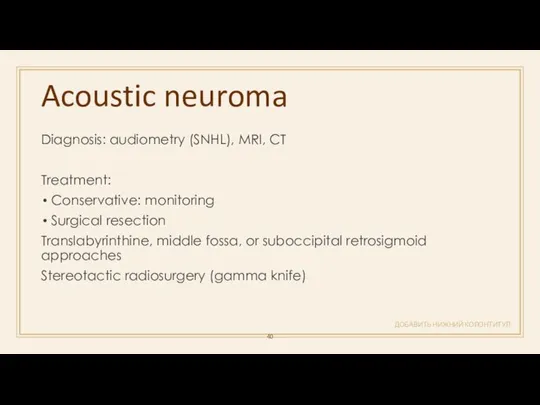
- 40. Acoustic neuroma ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Diagnosis: audiometry (SNHL), MRI, CT Treatment: Conservative: monitoring Surgical resection Translabyrinthine,
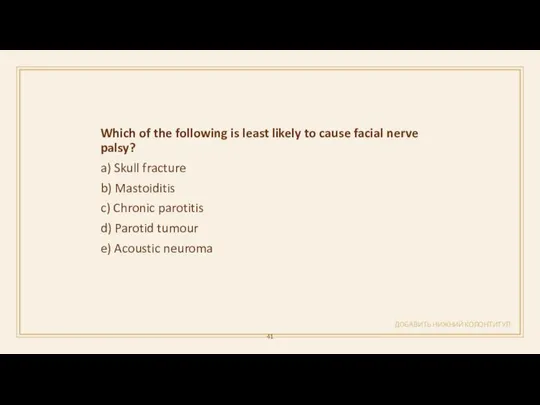
- 41. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Which of the following is least likely to cause facial nerve palsy? a)
- 42. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
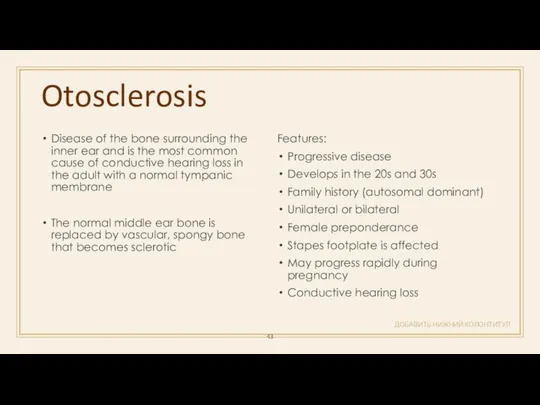
- 43. Otosclerosis ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Disease of the bone surrounding the inner ear and is the most
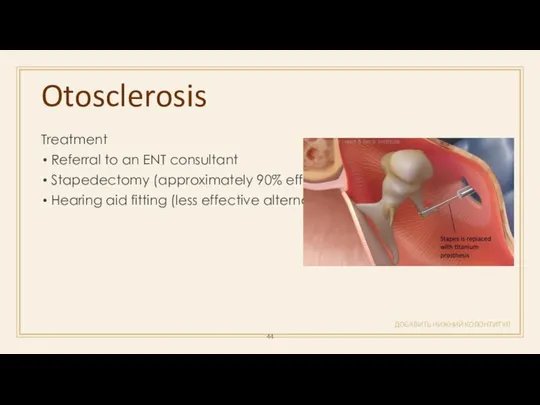
- 44. Otosclerosis ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Treatment Referral to an ENT consultant Stapedectomy (approximately 90% effective) Hearing aid
- 45. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Which of the following is most likely to be associated with otosclerosis? a)
- 46. ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
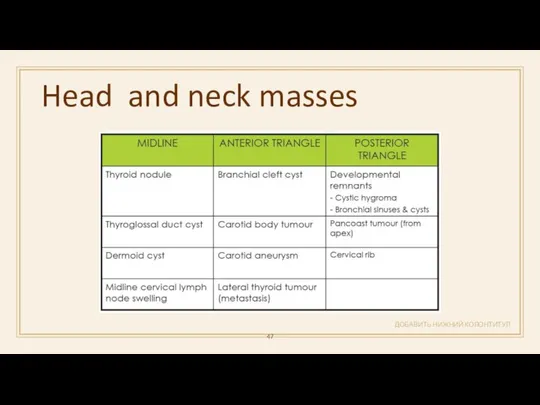
- 47. Head and neck masses ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
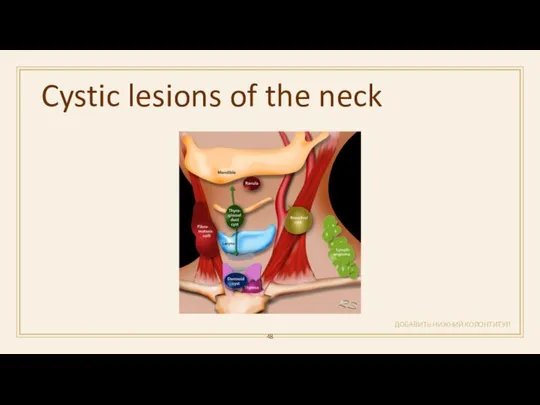
- 48. Cystic lesions of the neck ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ
- 49. Cystic hygroma ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Commonly involves the posterior cervical space May be macrocystic or
- 50. Branchial deft cyst ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ located inferior to the external auditory meatus or anterior to
- 51. Thyroglossal duct cyst ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ the most common childhood midline neck swelling It moves with
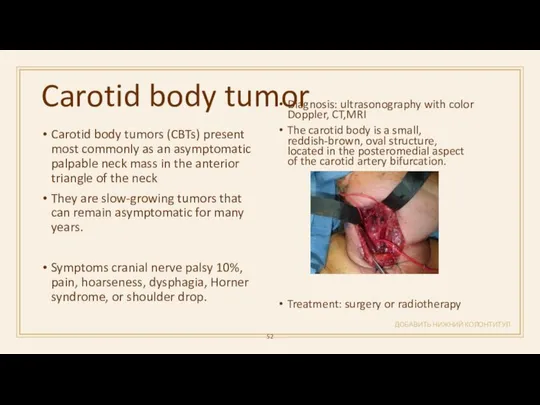
- 52. Carotid body tumor ДОБАВИТЬ НИЖНИЙ КОЛОНТИТУЛ Carotid body tumors (CBTs) present most commonly as an asymptomatic
- 54. Скачать презентацию


 Вирусология - наука изменившая жизнь
Вирусология - наука изменившая жизнь Uşaqlığın mioması
Uşaqlığın mioması Переломы и вывихи
Переломы и вывихи Фетоплаценталық жүйенің физиологиясы мен патологиясы
Фетоплаценталық жүйенің физиологиясы мен патологиясы Өкпе қатерлі ісігі
Өкпе қатерлі ісігі Дифтерия. Инфекционные заболевания у детей
Дифтерия. Инфекционные заболевания у детей худойдотов 2
худойдотов 2 Патология иммунной системы. Иммунодефицит
Патология иммунной системы. Иммунодефицит Организация трансфузионной помощи. Донорство
Организация трансфузионной помощи. Донорство Применение металлоконструкций и биодеградируемых материалов при переломах дистального отдела плечевой кости у детей
Применение металлоконструкций и биодеградируемых материалов при переломах дистального отдела плечевой кости у детей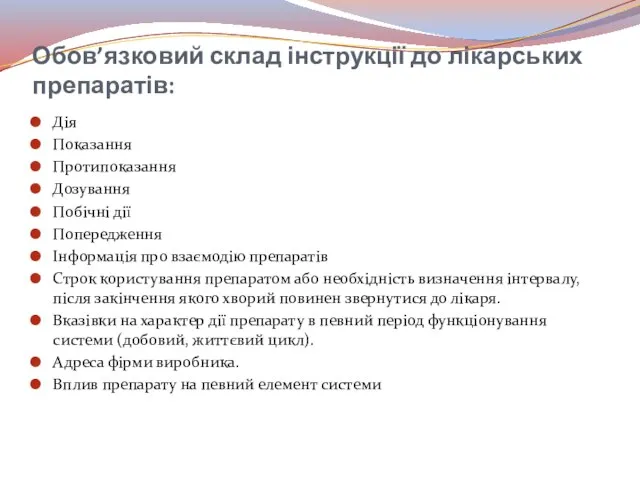 Обов’язковий склад інструкції до лікарських препаратів
Обов’язковий склад інструкції до лікарських препаратів Жедел бүйрек жетіспеушілігінің клиникалық көріністері
Жедел бүйрек жетіспеушілігінің клиникалық көріністері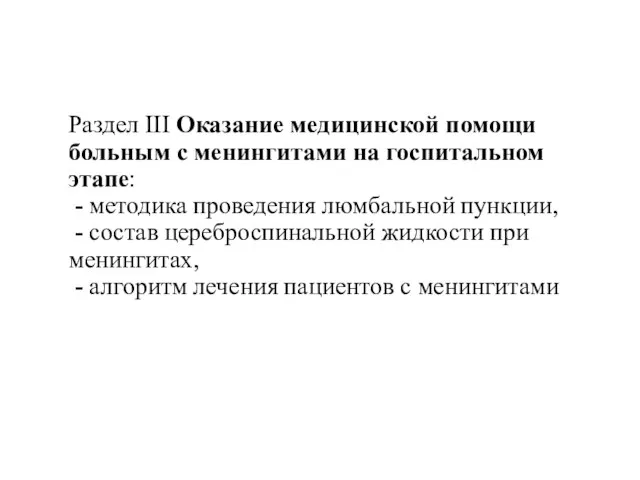 Медицинская помощь больным с менингитами на госпитальном этапе
Медицинская помощь больным с менингитами на госпитальном этапе TRALI. Минимизация риска
TRALI. Минимизация риска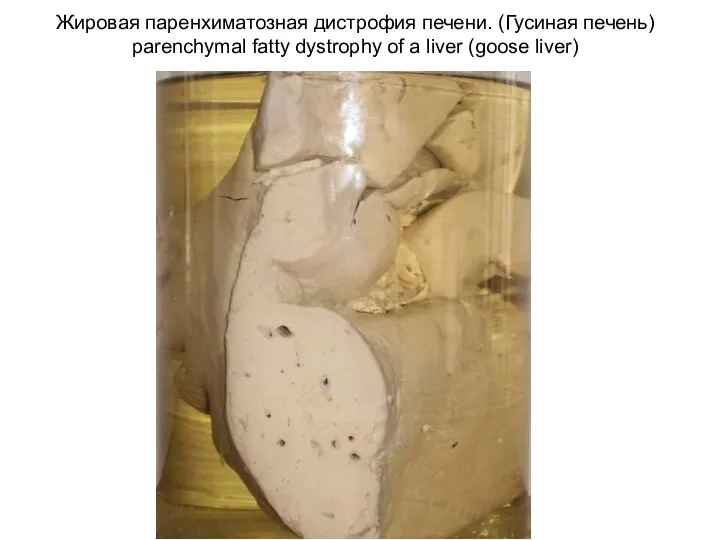 Гистология
Гистология Доказательная профилактика. Основные виды, проблемы внедрения и анализа результатов скрининговых программ
Доказательная профилактика. Основные виды, проблемы внедрения и анализа результатов скрининговых программ Кровотечі, їх класифікація. Перша допомога при кровотечах
Кровотечі, їх класифікація. Перша допомога при кровотечах Метод использования виртуальной реальности у детей с синдромом гипермобильности суставов
Метод использования виртуальной реальности у детей с синдромом гипермобильности суставов Туберкулинодиагностика
Туберкулинодиагностика Расстройства интеллекта
Расстройства интеллекта Гериатрическая фармакотерапия
Гериатрическая фармакотерапия Дополнительные методы обследования в клинике ортопедической стоматологии. Диагноз, дифференциальный диагноз
Дополнительные методы обследования в клинике ортопедической стоматологии. Диагноз, дифференциальный диагноз Рак предстательной железы
Рак предстательной железы Секреты правильного питания. Овощи и фрукты – полезные продукты
Секреты правильного питания. Овощи и фрукты – полезные продукты Механическая асфиксия
Механическая асфиксия Генитальный пролапс у женщин с дисплазией соединительной ткани
Генитальный пролапс у женщин с дисплазией соединительной ткани Статус участника проекта Сколково
Статус участника проекта Сколково Организация работы специализированных (БИТ) и линейных бригад скорой помощи
Организация работы специализированных (БИТ) и линейных бригад скорой помощи