Содержание
- 2. Postpartum infection – is a septic wound infection distinguished by anatomic features of female reproductive organs
- 3. Classification principles - By prevalence: local, generalized forms. - By infection localization: vagina, uterus, ovaries, parametric
- 4. Factors making patients susceptible to infection Changes in vaginal biocenose in final stages
- 5. Sponsored Medical Lecture Notes – All Subjects USMLE Exam (America) – Practice
- 6. Important!!! In the postpartum period the intra- uterine wall is a traumatic surface easily infected
- 7. Etiology Iron-deficiency anemia. Gestosis. Placental presentation. Pyelonephritis.
- 8. Postpartum ulcer – is caused by contamination of abrasions, fissures, ruptures of vulval and vaginal mucous
- 9. Diagnostics Hyperemia. Edema. Necrotic or purulent wound incrustation.
- 10. Treatment The wounds are cleansed with antiseptics locally (hydrogen peroxide, furacilin, chlorhexidine, dioxidine,
- 11. Postpartum endomyometritis. The most common infection in the postpartum period!
- 12. CLINICAL SYMPTOMS. ACUTE FORM. Temperature elevation › 38° on 2-5th day following delivery. Chills. Abdominal pain.
- 13. DIAGNOSTICS Bimanual examination (the uterus is enlarged,
- 14. TREATMENT Bed rest. Antibiotic therapy (semisynthetic penicillin, combination
- 15. Important!!! If the examination reveals placental tissues or membranes in the uterine cavity, it is necessary
- 16. Postpartum salpingo- oophoritis is rarely observed. The ovaries are normally affected on one side. The
- 17. Postnatal parametritis – the process normally begins when lacerations or infections of the cervix are
- 18. Clinical symptoms Chills on the 10-12th day following delivery. Temperature elevation to
- 19. On bimanual examination a painful infiltrate is found in the fornices, the fornices are shortened.
- 20. Postnatal trombophlebitis (affecting pelvis minor veins, superficial and deep veins of lower limbs). Causes Hypercoagulation. Vessel
- 21. Clinical symptoms Temperature elevation. Hyperemia and tenderness along of varix dilatated shin veins.
- 22. 22 Treatment Bed rest, lower limb should be maintained uplifted. Antibacterial
- 23. Obstetric peritonitis. Causes. Consequence of endomyometritis. Perforation of inflammatory tubo-ovarian mass.
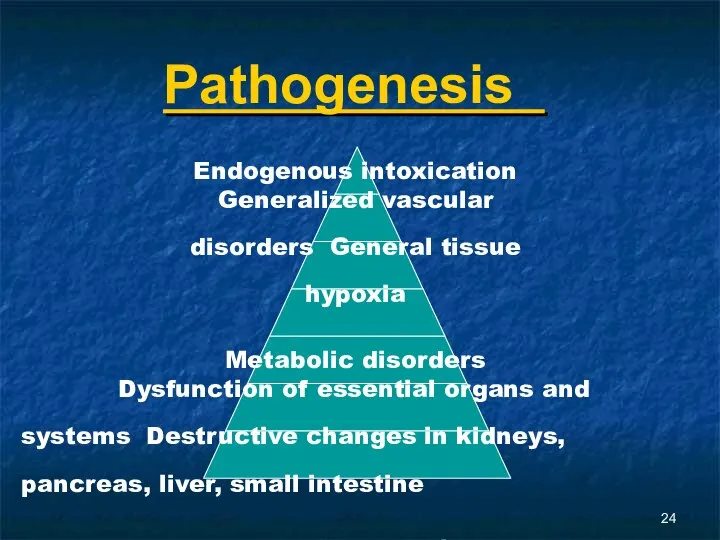
- 24. Pathogenesis Endogenous intoxication Generalized vascular disorders General tissue hypoxia Metabolic disorders Dysfunction of essential organs and
- 25. Enteroparesis. Motor, secretion, and absorption functions are affected. Significant amounts of protein and electrolyte containing
- 26. Obstetric peritonitis phases Reactive phase (compensatory mechanisms preserved). Toxic phase. Terminal phase.
- 27. Clinical symptoms psychomotor agitation thirst dryness of mucous membranes general weakness tachycardia (does not correspond to
- 28. unsatisfactory sleep absence of appetite pallor of the skin nausea eructation flatulence vomiting (not always)
- 29. On palpation: the abdomen is distended, the uterus is enlarged, softened, the contours are indistinct,
- 30. Treatment. Preoperative preparation (2 hours): stomach decompression, infusion therapy intended for liquidation of hypovolemia
- 31. Postoperative period: liquidation of hypovolemia and improvement of rheological properties of
- 32. - antibiotic therapy; - cardio-vascular collapse prevention and treatment; - vitamin therapy; - motor and evacuation
- 33. Postpartum sepsis – severe non-specific infective process developing and progressing when normal reactivity of the
- 34. Clinical symptoms Septicemia occurs on the 3-4th day following delivery, progresses violently. Septicopyemia progresses unevenly: periods
- 35. IMPORTANT!!! The diagnosis is based on the following prerequisites: - presence of an infection nidus; -
- 36. Impaired CNS function: euphoria, depression, sleep disturbance. Dyspnea. Cyanosis.
- 37. Diagnostics Clinical blood analysis. Clinical
- 38. Treatment Preoperative preparation during 6-8 hours, hypervolemic hemodilution mode. Operative treatment – hysterectomy and
- 39. Postoperative period: liquidation of hypovolemia and improvement of rheological properties of
- 40. - antibiotic therapy; - cardio-vascular collapse prevention and treatment; - vitamin therapy; - motor and evacuation
- 41. Postpartum lactational mastitis is an inflammation of breast tissue. The most common organism reported in
- 42. Classification Serous mastitis. Infiltrative mastitis (diffuse, nodular). Suppurative mastitis (intramammary, phlegmonous or necrotic
- 43. Clinical symptoms Rapid elevation in temperature to 39˚C. Chills.
- 44. Examination shows that the breast is engorged, the skin above the breast is hyperemic. With the
- 45. Treatment Antibacterial therapy. Procedures against lactostasis. Spasmolytics (no-spa) in combination
- 46. 46 With suppurative mastitis surgical treatment is indicated (incision of the abscess, bathing with antiseptics
- 48. Скачать презентацию



















 Окклюзионные нарушения мезентериального кровообращения
Окклюзионные нарушения мезентериального кровообращения Роль взрослого в развитии общения ребенка
Роль взрослого в развитии общения ребенка философия и медицина
философия и медицина Исследование маркеров эффективности трансляции в постуральной мышце человека в условиях 3 - суточной женской иммерсии
Исследование маркеров эффективности трансляции в постуральной мышце человека в условиях 3 - суточной женской иммерсии Венозное полнокровие. Кровоизлияния
Венозное полнокровие. Кровоизлияния Анатомо-физиологические особенности недоношенных детей
Анатомо-физиологические особенности недоношенных детей Методология консультирования женщин, идущих на прерывание беременности
Методология консультирования женщин, идущих на прерывание беременности Зудящие дерматозы
Зудящие дерматозы Биологический метод лечения пульпита. Показания, противопоказания, методика
Биологический метод лечения пульпита. Показания, противопоказания, методика Снотворные, противосудорожные (противоэпилептические, противопаркинсонические), обезболивающие ЛС
Снотворные, противосудорожные (противоэпилептические, противопаркинсонические), обезболивающие ЛС Воронкообразная деформация грудины у котёнка
Воронкообразная деформация грудины у котёнка Острая почечная недостаточность
Острая почечная недостаточность Современный подросток. Физическое здоровье (Методическое пособие)
Современный подросток. Физическое здоровье (Методическое пособие) Инфекционные заболевания
Инфекционные заболевания Проблемы защиты персональных данных в медицине
Проблемы защиты персональных данных в медицине Новорожденные щенки. Содержание, болезни, документы
Новорожденные щенки. Содержание, болезни, документы Медицинская реабилитация в гинекологии
Медицинская реабилитация в гинекологии Клиническая иммунология детского возраста
Клиническая иммунология детского возраста Проблемы нечистоплотности кошек и собак. Поведенческий и клинический аспекты
Проблемы нечистоплотности кошек и собак. Поведенческий и клинический аспекты Йогатерапия дисменореи в сочетании с варикозной болезнью нижних конечностей и малого таза
Йогатерапия дисменореи в сочетании с варикозной болезнью нижних конечностей и малого таза Учения об иммунитете
Учения об иммунитете Септический шок в акушерско-гинекологической практике
Септический шок в акушерско-гинекологической практике Современные методы хирургического лечения варикозной болезни нижних конечностей
Современные методы хирургического лечения варикозной болезни нижних конечностей Снижение смертности от болезней системы кровообращения
Снижение смертности от болезней системы кровообращения Гнойные заболевания пальцев и кисти
Гнойные заболевания пальцев и кисти ЛФК при заболеваниях дыхательной системы
ЛФК при заболеваниях дыхательной системы Эндокринология. Физиология половой дисфункции
Эндокринология. Физиология половой дисфункции Основы лечебно - эвакуационного обеспечения пораженных
Основы лечебно - эвакуационного обеспечения пораженных