Содержание
- 2. An infection of the genital tract which occurs as a complication of delivery is termed puerperal
- 3. Predisposing factors of puerperal sepsis: The pathogenicity of the vaginal flora may be influenced by certain
- 4. Antepartum risk factors: (1) Malnutrition and anemia, (2) Preterm labor, (3) Premature rupture of the membranes,
- 5. Microorganisms responsible for puerperal sepsis and the major pathology; Aerobic—Group A beta-hemolytic Streptococcus (GAS)—Toxic shock
- 6. Mode of Infection: Puerperal sepsis is essentially a wound infection. Placental site (being a raw surface),
- 7. PATHOGENESIS Endometrium (placental implantation site), cervical lacerated wound, vaginal wound or perineal lacerated wound are the
- 8. Clinical Features Local infection Uterine infection Spreading infection Local infection (Wound infection): (1)
- 9. Spreading infection (extrauterine spread) is evident by presence of pelvic tenderness (pelvic peritonitis), tenderness on the
- 10. Investigation of Puerperal Pyrexia The underlying principles in investigations are: To locate the site of infection,
- 11. Investigations include: High vaginal and endocervical swabs for culture in aerobic and anaerobic media and sensitivity
- 12. Treatment General care: (i)Isolation of the patient is preferred especially when hemolytic Streptococcus is obtained on
- 13. Surgical treatment: There is little role of major surgery in the treatment of puerperal sepsis.
- 15. Скачать презентацию
An infection of the genital tract which occurs as a
An infection of the genital tract which occurs as a
Puerperal pyrexia is considered to be due to genital tract infection unless proved otherwise. There has been marked decline in puerperal sepsis during the past few years due to:
improved obstetric care,
(2) availability of wider range of antibiotics.
Puerperal sepsis is commonly due to—
endometritis,
(ii) endomyometritis, or
(iii) endoparametritis or a combination of all these when it is called pelvic cellulitis.
Predisposing factors of puerperal sepsis:
The pathogenicity of the vaginal flora
Predisposing factors of puerperal sepsis:
The pathogenicity of the vaginal flora
(1) The cervicovaginal mucous membrane is damaged even in normal delivery,
(2) The uterine surface too, especially the placental site, is converted into an open wound by the cleavage of the decidua which takes place during the third stage of labor, and
(3) The blood clots present at the placental site are excellent media for the growth of the bacteria
Antepartum risk factors: (1) Malnutrition and anemia, (2) Preterm labor, (3)
Antepartum risk factors: (1) Malnutrition and anemia, (2) Preterm labor, (3)
Intrapartum risk factors: (1) Repeated vaginal examinations, (2) Dehydration and ketoacidosis during labor, (3) Traumatic vaginal delivery, (4) Hemorrhage—antepartum or postpartum, (5) Retained bits of placental tissue or membranes, (6) Prolonged labor, (7) Obstructed labor, (8) Cesarean delivery. Due to the factors mentioned above, the organisms gain foothold either in the traumatized tissues of the uterovaginal canal or in the raw decidua left behind or in the blood clots, especially at the placental site
Microorganisms responsible for puerperal sepsis and the major pathology;
Aerobic—Group
Microorganisms responsible for puerperal sepsis and the major pathology;
Aerobic—Group
Group B beta-hemolytic Streptococcus (GBS) is a significant cause of neonatal deaths due to septicemia, respiratory disease and meningitis.
Maternal risks are also high. Methicillin-resistant S. aureus (MRSA) causes severe infection.
Others—Staphylococcus pyogenes, S. aureus, E. coli, Klebsiella, Pseudomonas, Proteus, Chlamydia.
Anaerobic—Streptococcus, Peptococcus, Bacteroides (fragilis, bivius), Fusobacteria, Mobiluncus and Clostridia.
Most of the infections in the genital tract are polymicrobial with a mixture of aerobic and anaerobic organisms
Mode of Infection:
Puerperal sepsis is essentially a wound infection. Placental
Mode of Infection:
Puerperal sepsis is essentially a wound infection. Placental
Sources of infection may be endogenous where organisms are present in the genital tract before delivery. Anaerobic Streptococcusis the predominant pathogen.
Infection may be autogenous where organisms present elsewhere (skin, throat) in the body and migrate to the genital organs by bloodstream or by the patient herself.
Beta-hemolytic Streptococcus, E. coli, Staphylococcus are important. Infection may be exogenous where infection is contracted from sources outside the patient (from hospital or attendants). Beta-hemolytic Streptococcus, Staphylococcus and E. coli are important.
PATHOGENESIS Endometrium (placental implantation site), cervical lacerated wound, vaginal wound or
PATHOGENESIS Endometrium (placental implantation site), cervical lacerated wound, vaginal wound or
The devitalized tissue,blood clots, foreign body (retained cotton swabs), and surgical trauma favor polymicrobial growth, proliferation and spread of infection. This ultimately leads to metritis, parametritis and/or cellulitis.
Clinical Features
Local infection
Uterine infection
Spreading infection
Clinical Features
Local infection
Uterine infection
Spreading infection
Local infection (Wound infection): (1) There is slight rise of temperature, generalized malaise or headache, (2) The local wound becomes red and swollen, (3) Pus may form which leads to disruption of the wound. When severe (acute), there is high rise of temperature with chills and rigor.
UTERINE INFECTION
Mild—(1) There is rise in temperature (>100.4°F) and pulse rate (>90), (2) Lochial discharge becomes offensive and copious, (3) The uterus is subinvoluted and tender.
Severe—(1) The onset is acute with high rise of temperature, often with chills and rigor, (2) Pulse rate is rapid, out of proportion to temperature, (3) Often there is breathlessness, coughs, abdominal pain and dysuria, (4) Lochia may be scanty and odorless, (5) Uterus may be subinvoluted, tender and softer. There may be associated wound infection (perineum, vagina or the cervix).
Spreading infection (extrauterine spread) is evident by presence of pelvic tenderness
Spreading infection (extrauterine spread) is evident by presence of pelvic tenderness
Bacteremia, endotoxic or septic shock is due to release of bacterial endotoxin (lipopolysaccharide) causing circulatory inadequacy and tissue hypoperfusion. It is manifested by hypotension, oliguria and adult respiratory distress syndrome
Investigation of Puerperal Pyrexia The underlying principles in investigations are:
To
Investigation of Puerperal Pyrexia The underlying principles in investigations are:
To
A case of puerperal pyrexia is considered to be due to genital sepsis unless proved otherwise. The investigations should also be directed to find out any extragenital source of infection to account for the fever as well.
Investigations of Puerperal Pyrexia History: Antenatal, intranatal and postnatal history of any high risk factor for infection like anemia, prolonged rupture of membranes or prolonged labor are to be taken.
Clinical examination includes thorough general, physical and systemic examinations. Abdominal and pelvic examinations are done to note the involution of genital organs and locate the specific site of infection. Legs should be examined for thrombophlebitis or thrombosis
Investigations include:
High vaginal and endocervical swabs for culture in aerobic
Investigations include:
High vaginal and endocervical swabs for culture in aerobic
(2) “Clean catch” midstream specimen of urine for analysis and culture including sensitivity test.
(3) Blood for total and differential white cell count, hemoglobin estimation. A low platelet count may indicate septicemia or DIC. Thick blood film should be examined for malarial parasites.
(4) Blood culture, if fever is associated with chills and rigor. Other specific investigations as per the clinical condition are needed.
(5) Pelvic ultrasound is helpful—(i) to detect any retained bits of conception within the uterus, (ii) to locate any abscess within the pelvis, (iii) to collect samples (pus or fluid) from the pelvis for culture and sensitivity, and (iv) for color flow Doppler study to detect venous thrombosis. Use of CT and MRI is needed especially when diagnosis is in doubt or there is pelvic vein thrombosis.
(6) X-ray chest (CXR) should be taken in cases with suspected pulmonary Koch’s lesion and also to detect any lung pathology like collapse and atelectasis (following inhalation anesthesia).
(7) Blood urea and electrolytes may be done in a selected case to have a baseline record in the event that renal failure develops later in the course of the disease or laparotomy is needed.
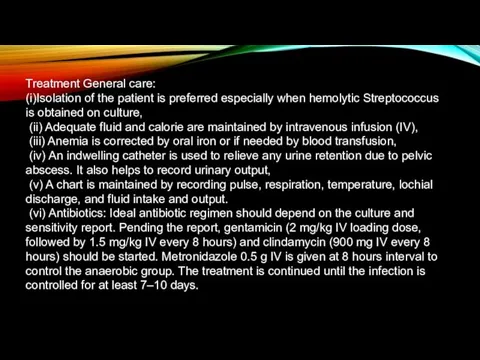
Treatment General care:
(i)Isolation of the patient is preferred especially when hemolytic
Treatment General care:
(i)Isolation of the patient is preferred especially when hemolytic
(ii) Adequate fluid and calorie are maintained by intravenous infusion (IV),
(iii) Anemia is corrected by oral iron or if needed by blood transfusion,
(iv) An indwelling catheter is used to relieve any urine retention due to pelvic abscess. It also helps to record urinary output,
(v) A chart is maintained by recording pulse, respiration, temperature, lochial discharge, and fluid intake and output.
(vi) Antibiotics: Ideal antibiotic regimen should depend on the culture and sensitivity report. Pending the report, gentamicin (2 mg/kg IV loading dose, followed by 1.5 mg/kg IV every 8 hours) and clindamycin (900 mg IV every 8 hours) should be started. Metronidazole 0.5 g IV is given at 8 hours interval to control the anaerobic group. The treatment is continued until the infection is controlled for at least 7–10 days.
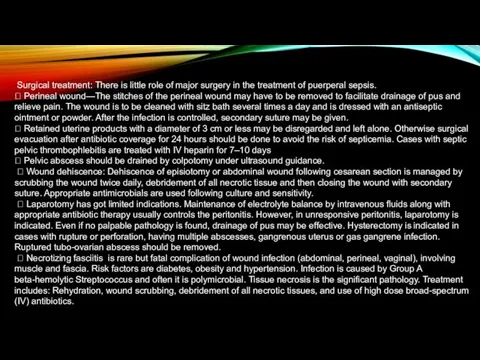
Surgical treatment: There is little role of major surgery in
Surgical treatment: There is little role of major surgery in
Perineal wound—The stitches of the perineal wound may have to be removed to facilitate drainage of pus and relieve pain. The wound is to be cleaned with sitz bath several times a day and is dressed with an antiseptic ointment or powder. After the infection is controlled, secondary suture may be given.
Retained uterine products with a diameter of 3 cm or less may be disregarded and left alone. Otherwise surgical evacuation after antibiotic coverage for 24 hours should be done to avoid the risk of septicemia. Cases with septic pelvic thrombophlebitis are treated with IV heparin for 7–10 days
Pelvic abscess should be drained by colpotomy under ultrasound guidance.
Wound dehiscence: Dehiscence of episiotomy or abdominal wound following cesarean section is managed by scrubbing the wound twice daily, debridement of all necrotic tissue and then closing the wound with secondary suture. Appropriate antimicrobials are used following culture and sensitivity.
Laparotomy has got limited indications. Maintenance of electrolyte balance by intravenous fluids along with appropriate antibiotic therapy usually controls the peritonitis. However, in unresponsive peritonitis, laparotomy is indicated. Even if no palpable pathology is found, drainage of pus may be effective. Hysterectomy is indicated in cases with rupture or perforation, having multiple abscesses, gangrenous uterus or gas gangrene infection. Ruptured tubo-ovarian abscess should be removed.
Necrotizing fasciitis is rare but fatal complication of wound infection (abdominal, perineal, vaginal), involving muscle and fascia. Risk factors are diabetes, obesity and hypertension. Infection is caused by Group A beta-hemolytic Streptococcus and often it is polymicrobial. Tissue necrosis is the significant pathology. Treatment includes: Rehydration, wound scrubbing, debridement of all necrotic tissues, and use of high dose broad-spectrum (IV) antibiotics.


 Микроклимат сипаттамасы
Микроклимат сипаттамасы Использование виртуальной реальности у детей с нарушениями осанки при синдроме гипермобильности суставов
Использование виртуальной реальности у детей с нарушениями осанки при синдроме гипермобильности суставов Комплексное обследование при дислалии. Лекция 2
Комплексное обследование при дислалии. Лекция 2 Аффективные расстройства
Аффективные расстройства Хронический гастрит. Язвенная болезнь
Хронический гастрит. Язвенная болезнь Коррекционный маршрут в дооперационный период ребенка с открытой ринолалией
Коррекционный маршрут в дооперационный период ребенка с открытой ринолалией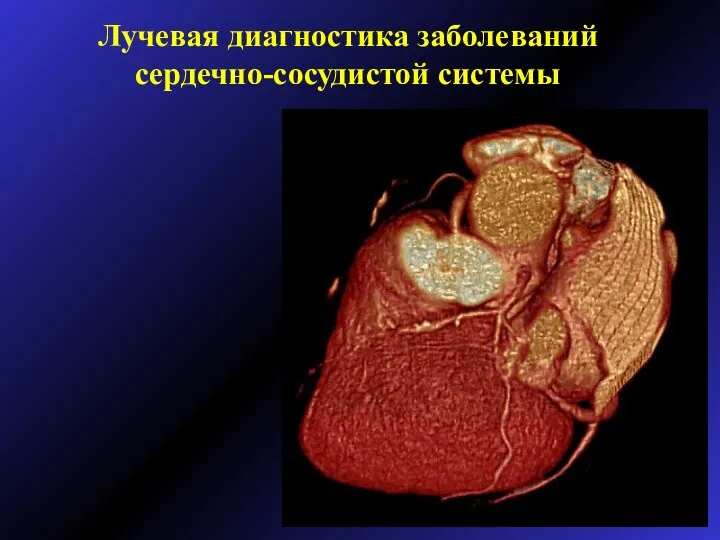 Лучевая диагностика заболеваний сердечно-сосудистой системы
Лучевая диагностика заболеваний сердечно-сосудистой системы Психологические условия полноценного психофизической развития ребенка в период новорождённости
Психологические условия полноценного психофизической развития ребенка в период новорождённости Психомоторное развитие ребенка и его оценка. Теории психического и духовного развития. Поведение детей
Психомоторное развитие ребенка и его оценка. Теории психического и духовного развития. Поведение детей Душевное здоровье детей и подростков: неврозы и неврозоподобные расстройства
Душевное здоровье детей и подростков: неврозы и неврозоподобные расстройства Черепно-мозговая травма. Основные патологические процессы
Черепно-мозговая травма. Основные патологические процессы Проблема ВИЧ/СПИД в Забайкальском крае
Проблема ВИЧ/СПИД в Забайкальском крае Ожирение
Ожирение Общая семиотика моногенных и многофакторных болезней
Общая семиотика моногенных и многофакторных болезней Жизнь современного ребенка. Интенсивный рост. Школьные нагрузки. Стрессы
Жизнь современного ребенка. Интенсивный рост. Школьные нагрузки. Стрессы Особенности гигиены полости рта у пациентов с несъемными ортопедическими конструкциями и дентальными имплантатами
Особенности гигиены полости рта у пациентов с несъемными ортопедическими конструкциями и дентальными имплантатами Гигиена лечебно-профилактических учреждений
Гигиена лечебно-профилактических учреждений Острый холецистит – неспецифическое воспаление желчного пузыря
Острый холецистит – неспецифическое воспаление желчного пузыря Мотивация теориясы. Мотивация процесі
Мотивация теориясы. Мотивация процесі Биохимия печени
Биохимия печени Акушерлік іс және гинекология
Акушерлік іс және гинекология Остеоартрит, остеоартроз. Новый взгляд на старую проблему
Остеоартрит, остеоартроз. Новый взгляд на старую проблему Неспецифический язвенный колит и болезнь Крона
Неспецифический язвенный колит и болезнь Крона Гигиена полости рта
Гигиена полости рта Бір жасқа дейінгі дені сау балалардың диспансерлік бақылау, патронаж
Бір жасқа дейінгі дені сау балалардың диспансерлік бақылау, патронаж Sweet proteins
Sweet proteins Фізична реабілітація дітей з рахітом
Фізична реабілітація дітей з рахітом Трансанальная слизисто-подслизистая резекция по методу Лонго
Трансанальная слизисто-подслизистая резекция по методу Лонго