Содержание
- 2. Urinary Tract Infections UTI: Growth of significant number of organisms of a single species in the
- 3. Signs & Symptoms of UTIs Features of UTI in infants are nonspecific: thus a high degree
- 4. Urine Sample Collection & Diagnostic Testing Methods Prevent contamination!!!!! Send urine within 1 hour for accurate
- 5. Who needs X-Ray evaluation? Any child with febrile UTI or recurrent UTIs. ALL females “Non-febrile” UTIs
- 6. Vesicoureteral Reflux “Backwash” or retrograde flow of urine from the bladder into the ureters, and usually
- 7. Primary: (Congenital) defect of UVJ (ureterovesical junction) – Most common –deficient tunnel / laterally displaced orifices
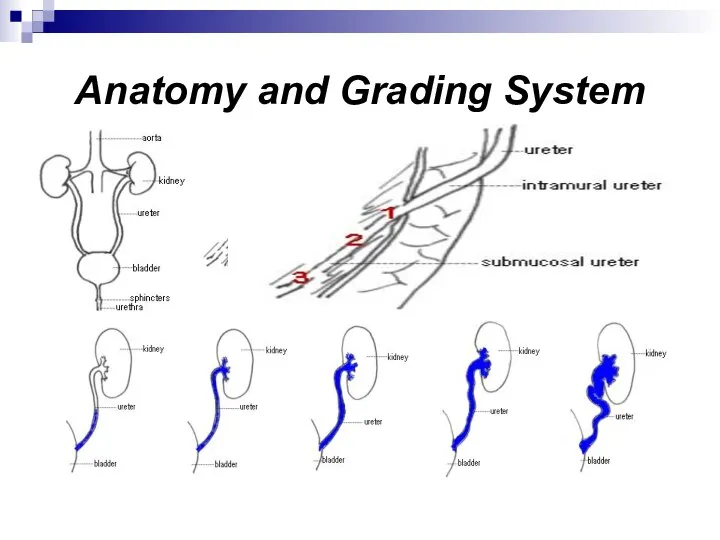
- 8. Anatomy and Grading System
- 9. Management Trends / Rx A person can NEVER be cured of UTIs A person CAN BE
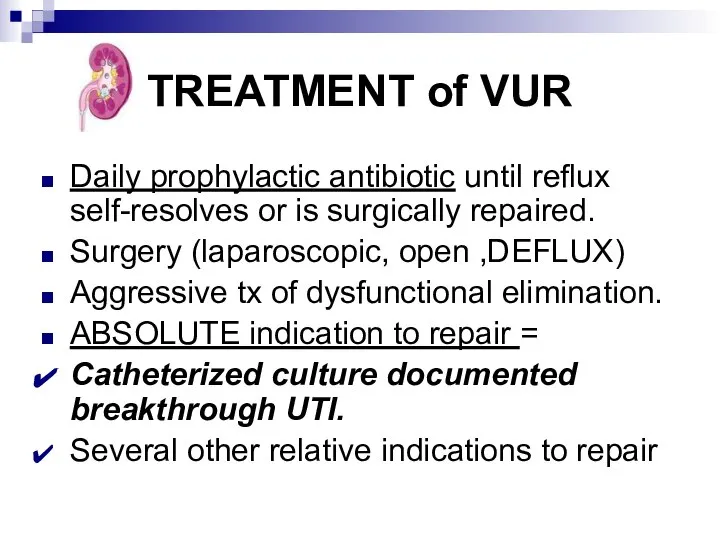
- 10. TREATMENT of VUR Daily prophylactic antibiotic until reflux self-resolves or is surgically repaired. Surgery (laparoscopic, open
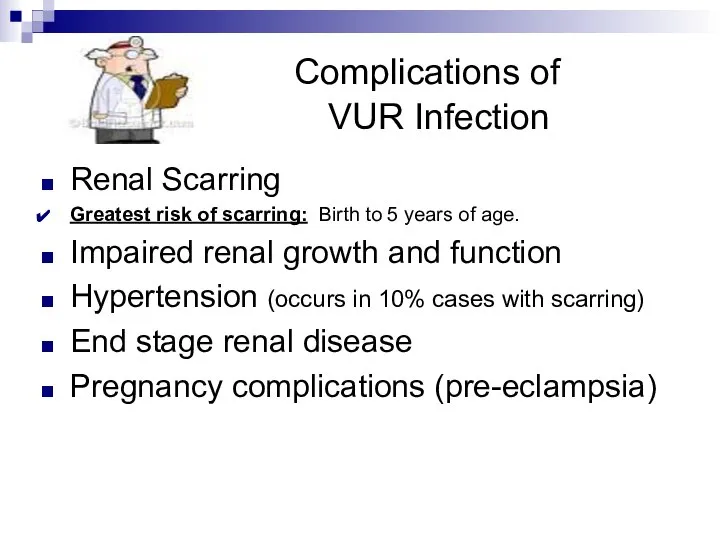
- 11. Complications of VUR Infection Renal Scarring Greatest risk of scarring: Birth to 5 years of age.
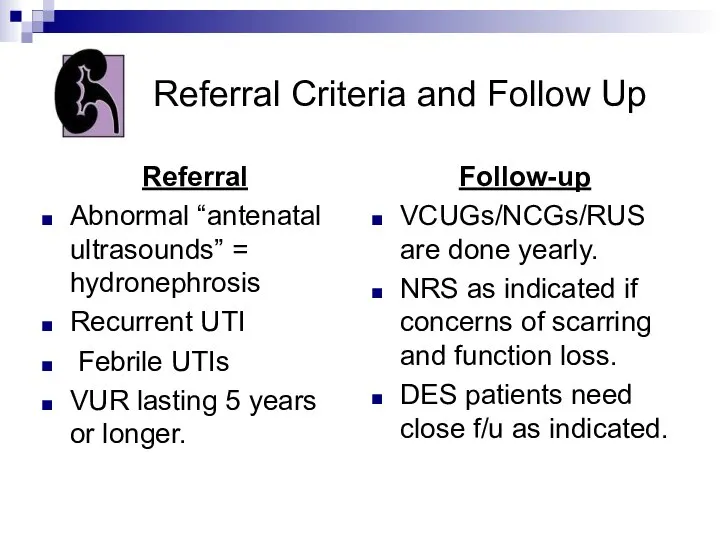
- 12. Referral Criteria and Follow Up Referral Abnormal “antenatal ultrasounds” = hydronephrosis Recurrent UTI Febrile UTIs VUR
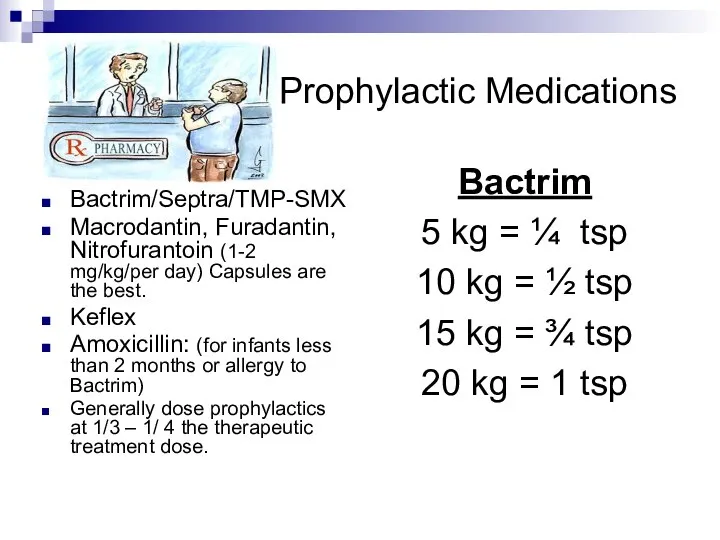
- 13. Prophylactic Medications Bactrim/Septra/TMP-SMX Macrodantin, Furadantin, Nitrofurantoin (1-2 mg/kg/per day) Capsules are the best. Keflex Amoxicillin: (for
- 14. Evolution in VUR management Changes Minimally invasive surgery Observation off RX Aggressive management DES Prenatal detection
- 15. The END!
- 17. Скачать презентацию
 Неврологические аспекты адаптации детей в школе, пути профилактики
Неврологические аспекты адаптации детей в школе, пути профилактики Оказание первой помощи при попадании инородного тела в дыхательные пути
Оказание первой помощи при попадании инородного тела в дыхательные пути Органы кроветворения и иммуногенеза
Органы кроветворения и иммуногенеза Принятие решений: ловушки
Принятие решений: ловушки Eating disorders
Eating disorders История развития психопатологии в зарубежный странах
История развития психопатологии в зарубежный странах Медицинское обеспечение
Медицинское обеспечение Острые кишечные инфекции
Острые кишечные инфекции Медична послуга. Поняття та терміни
Медична послуга. Поняття та терміни Доброкачественные опухоли толстой кишки
Доброкачественные опухоли толстой кишки Пилоростеноз у детей. Дифференциальная диагностика
Пилоростеноз у детей. Дифференциальная диагностика Дифтерия у детей
Дифтерия у детей Клинический случай. Лечение
Клинический случай. Лечение Расстройства внимания
Расстройства внимания Структура психиатрической службы в РФ. Организация психиатрической службы. Законы о психиатрической помощи
Структура психиатрической службы в РФ. Организация психиатрической службы. Законы о психиатрической помощи Методики АФК для детей с нарушением слуха
Методики АФК для детей с нарушением слуха Созылмалы лимфолейкоз
Созылмалы лимфолейкоз Грибковые заболевания. Лишай
Грибковые заболевания. Лишай Перелом. Оказание помощи
Перелом. Оказание помощи Закупки медицинских организаций здравоохранения Кузбасса по состоянию в 2021 году
Закупки медицинских организаций здравоохранения Кузбасса по состоянию в 2021 году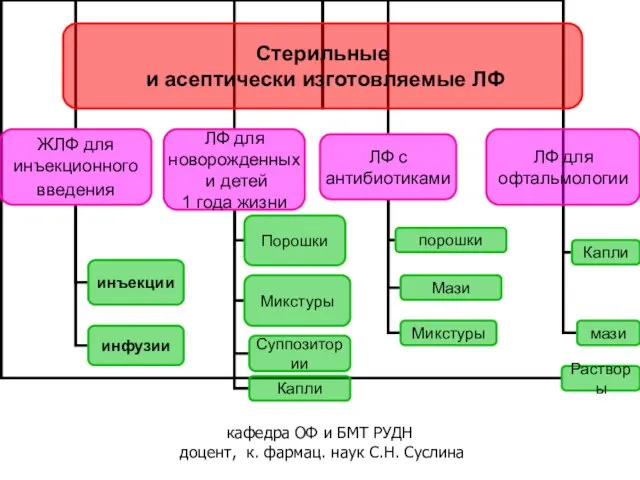 Стерильные и асептически изготовляемые ЛФ
Стерильные и асептически изготовляемые ЛФ Когнитивно-поведенческая терапия обсессивно-компульсивного расстройства
Когнитивно-поведенческая терапия обсессивно-компульсивного расстройства Тошнота и рвота беременных
Тошнота и рвота беременных Ортопедиялық стоматологияда қазіргі заманғы визуализация
Ортопедиялық стоматологияда қазіргі заманғы визуализация Инфаркт миокарда, шок и коллапс
Инфаркт миокарда, шок и коллапс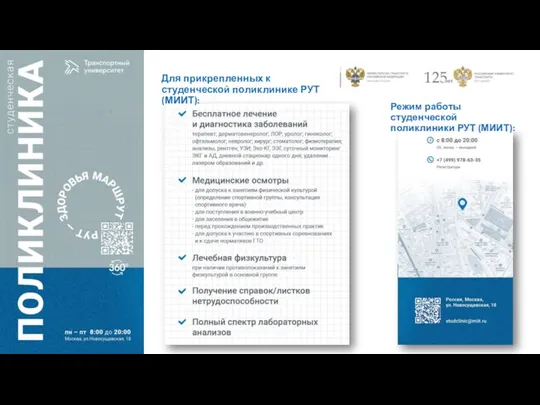 Студенческая поликлиника РУТ
Студенческая поликлиника РУТ Глядя в будущее, создаём настоящее
Глядя в будущее, создаём настоящее Иммунитет. Виды иммунитета. Врожденный и адаптивный иммунитет. Функциональная организация иммунной системы. (Лекция 1)
Иммунитет. Виды иммунитета. Врожденный и адаптивный иммунитет. Функциональная организация иммунной системы. (Лекция 1)