Содержание
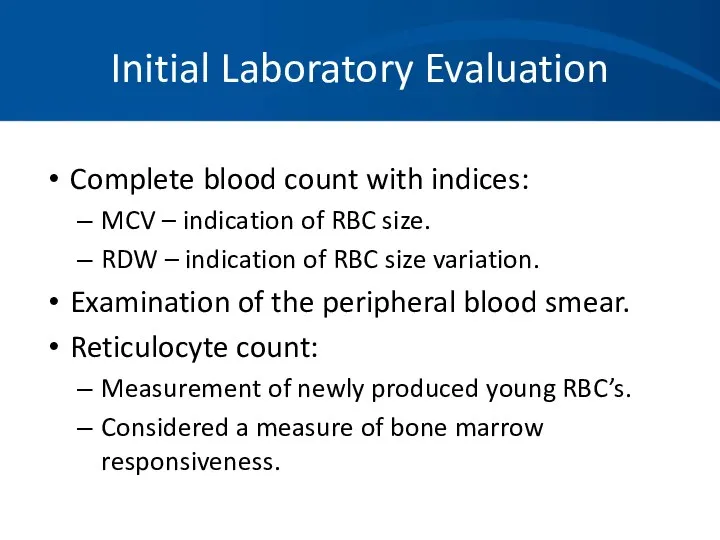
- 2. Initial Laboratory Evaluation Complete blood count with indices: MCV – indication of RBC size. RDW –
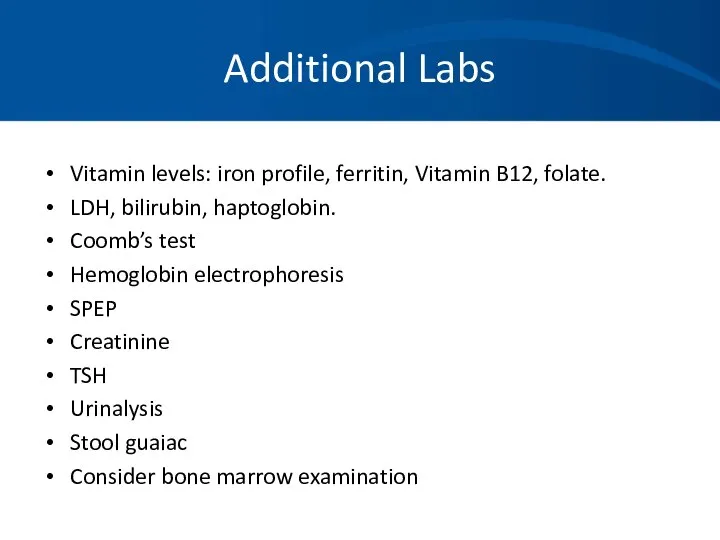
- 3. Additional Labs Vitamin levels: iron profile, ferritin, Vitamin B12, folate. LDH, bilirubin, haptoglobin. Coomb’s test Hemoglobin
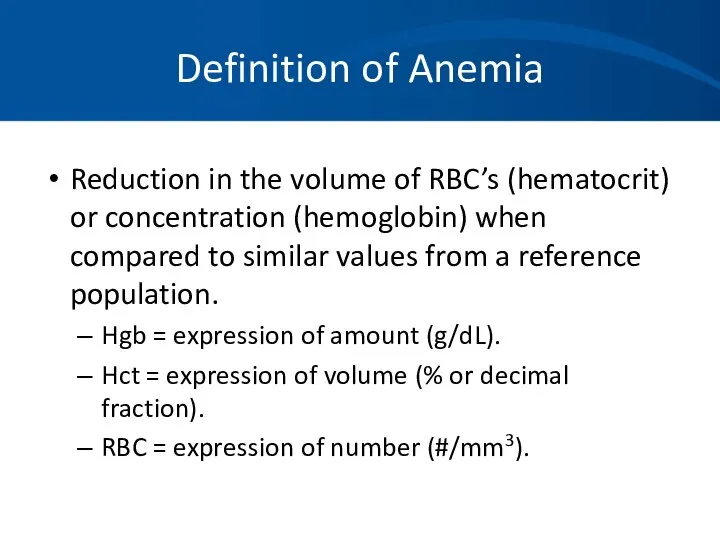
- 4. Definition of Anemia Reduction in the volume of RBC’s (hematocrit) or concentration (hemoglobin) when compared to
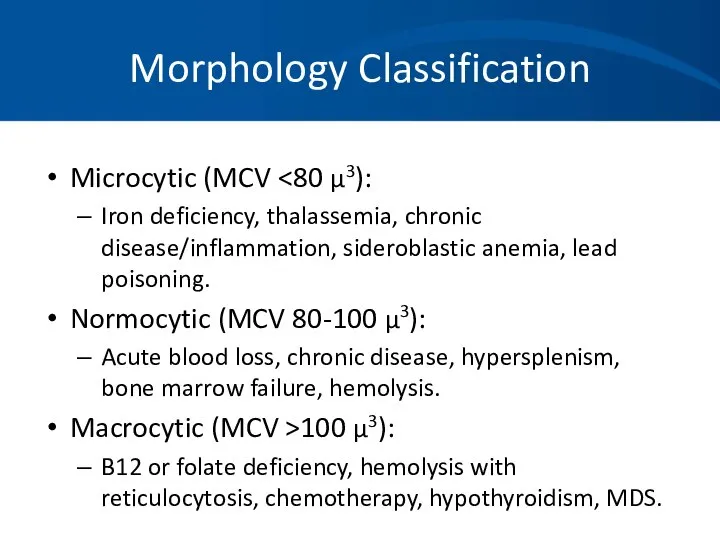
- 5. Morphology Classification Microcytic (MCV Iron deficiency, thalassemia, chronic disease/inflammation, sideroblastic anemia, lead poisoning. Normocytic (MCV 80-100
- 6. Case 1 A 35 year old woman has a history of pleurisy and has been told
- 7. Case 1 Initial Labs: Hemoglobin 7.9 gm/dL HCT 23.9% WBC 4000/mm3 with a normal differential Platelet
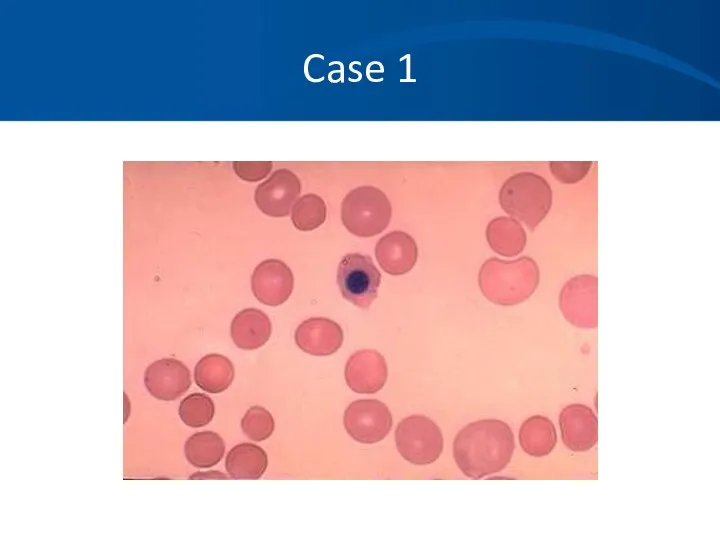
- 8. Case 1 MCV 114 Uncorrected Retic count 14.2% LDH 2343 U/L Bilirubin 4.3mg/dL Direct bili .8mg/dL
- 9. Case 1
- 10. Case 1 You suspect an autoimmune hemolytic anemia based on her history, Physical Exam, labs, and
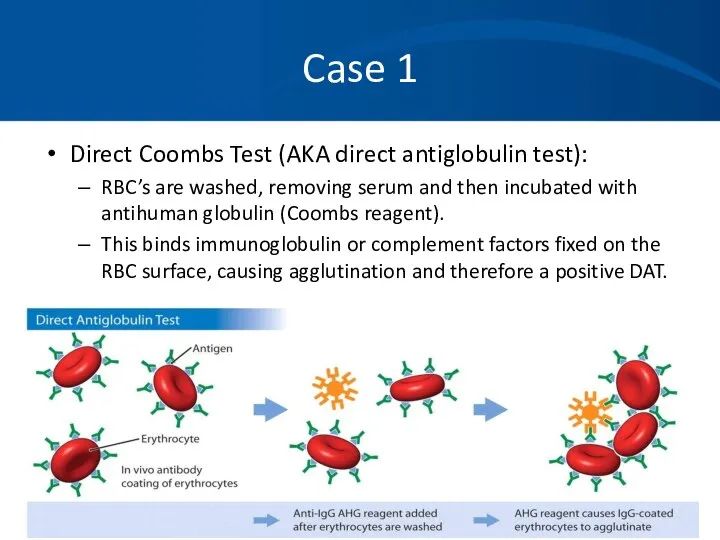
- 11. Case 1 Direct Coombs Test (AKA direct antiglobulin test): RBC’s are washed, removing serum and then
- 12. Case 1 Direct Coombs test results are as follows: DAT: Positive 3+ IgG: Positive 3+ Complement:
- 13. Case 1 You diagnose a warm-antibody hemolytic anemia and suspect an underlying autoimmune disorder. Etiology: Idiopathic
- 14. Case 1 You decide to avoid blood transfusion because of: The difficulties in obtaining cross match
- 15. Case 1 Treatment: Prednisone Splenectomy Rituximab (monoclonal antibody) Immunosuppressive agents Cytoxan, imuran, cyclosporin Danazol Plasma exchange
- 16. Case 1 You begin her on 60 mg Prednisone and she has a good response. Upon
- 17. Case 1 She responds well to splenectomy, but still requires very low maintenance doses of Prednisone.
- 18. Case 2 You are referred a pleasant 34 year old African American woman who has been
- 19. Case 2 Labs: HCT 31-34% Hgb 10.6-11.4gm/dL PLT 232-312K/mm3 WBC 6500-8000/mm3 with a normal differential MCV
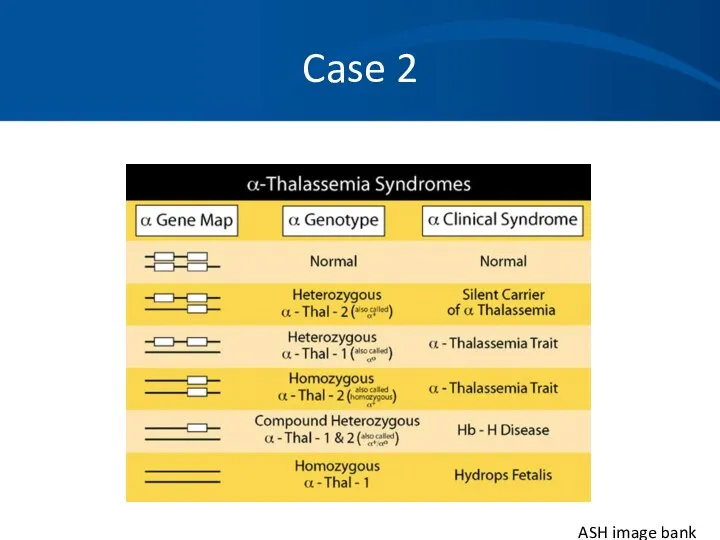
- 20. Case 2 Differential Diagnosis: Iron deficiency anemia Noncompliance, inadequate dosing, incorrect formulation. Beta thalassemia Alpha thalassemia
- 21. Case 2 Iron studies are normal. Chemistries, liver function tests, thyroid studies are normal. No history
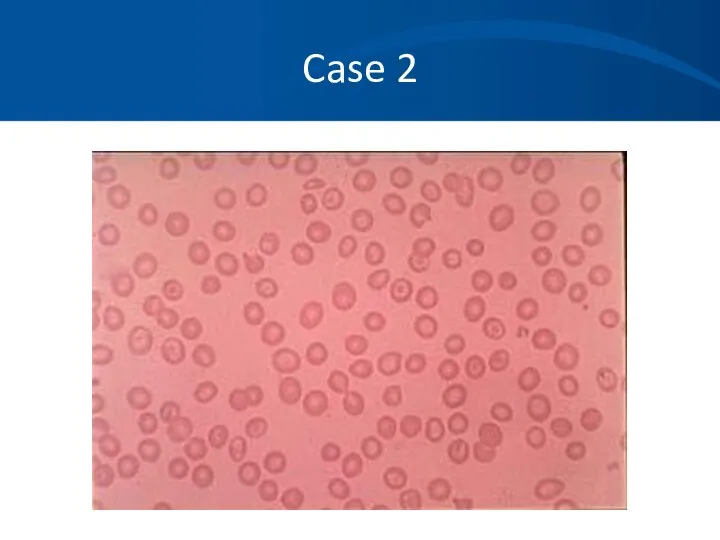
- 22. Case 2
- 23. Case 2 ASH image bank
- 24. Case 2 You also request a hemoglobin electrophoresis. Hgb A = 97.5% Hgb A2 = 2.1%
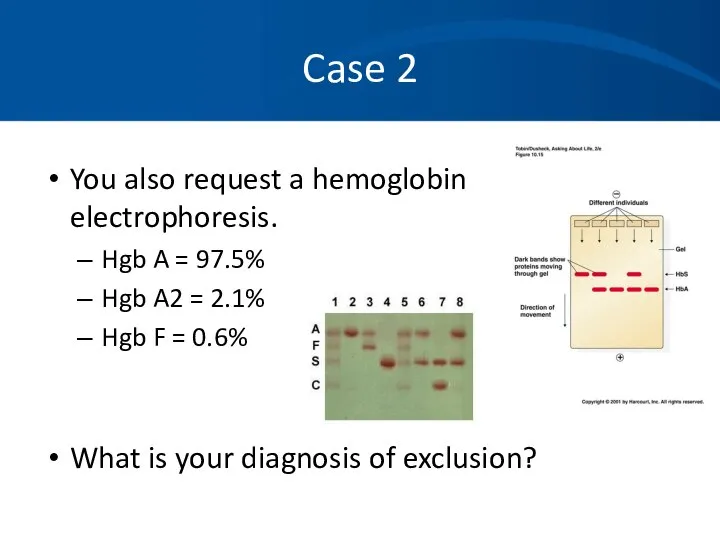
- 25. Case 2 Alpha thalassemia with a double gene deletion. No treatment is necessary. Anemia is not
- 26. Case 3 A 32 year old previously healthy woman with no prior medical history presents to
- 27. Case 3 Physical exam confirms an ill appearing woman. T = 38.6, pulse 122, BP 123/54
- 28. Case 3 Routine labs: WBC = 1700/mm3 Hgb = 5.6 gm/dL HCT 18.2% Platelet – 12,000/mm3
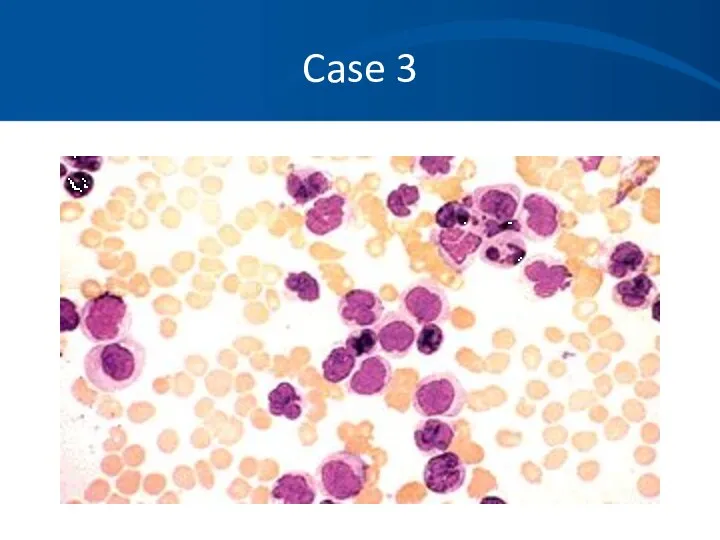
- 29. Case 3 Differential of the white blood cell count reveals at least 50% of young white
- 30. Case 3
- 31. Case 3
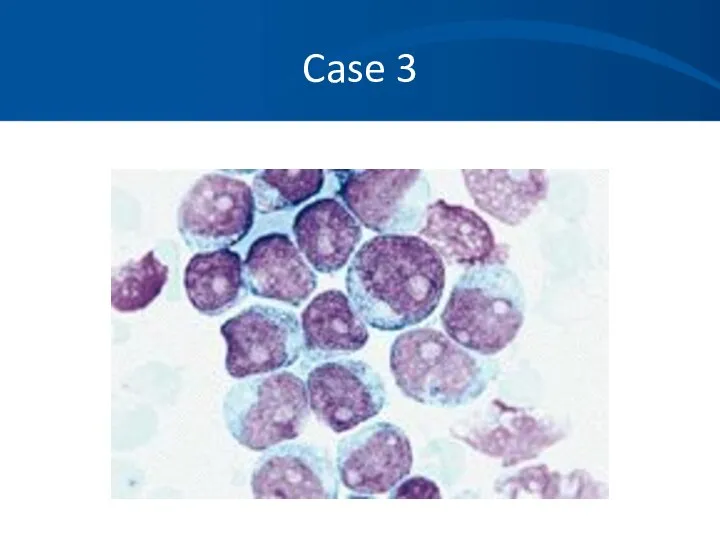
- 32. Case 3
- 33. Case 3 Hematopathology evaluation revealed AML subtype M1. Chromosomal studies were normal. What should you do
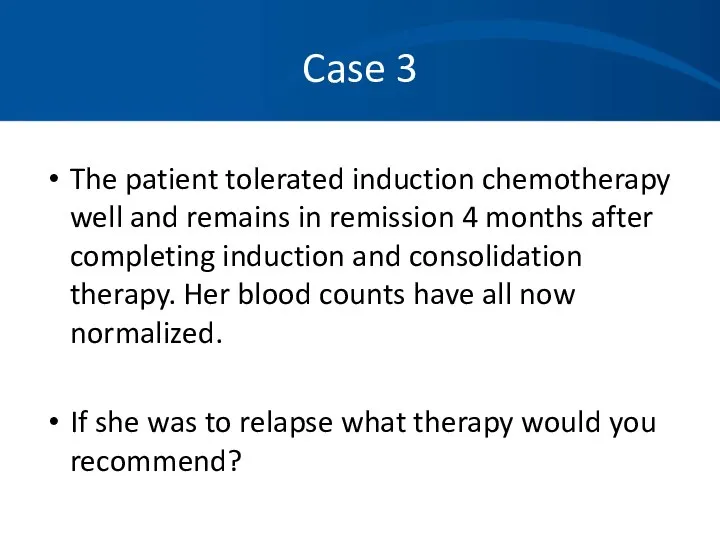
- 34. Case 3 The patient tolerated induction chemotherapy well and remains in remission 4 months after completing
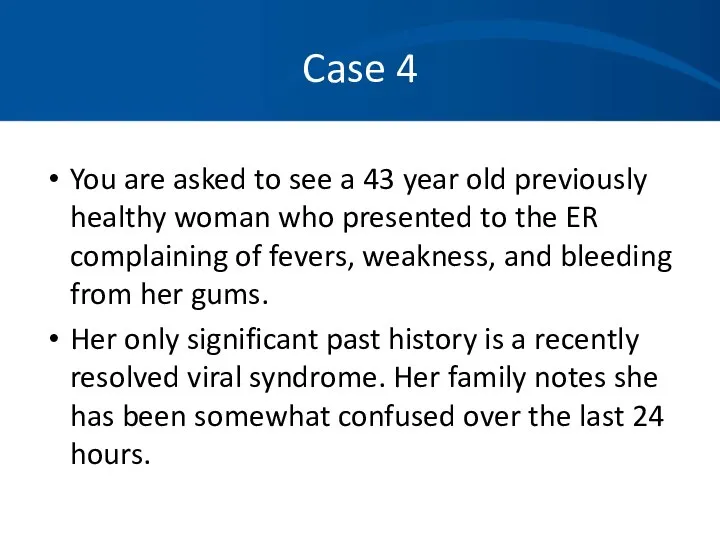
- 35. Case 4 You are asked to see a 43 year old previously healthy woman who presented
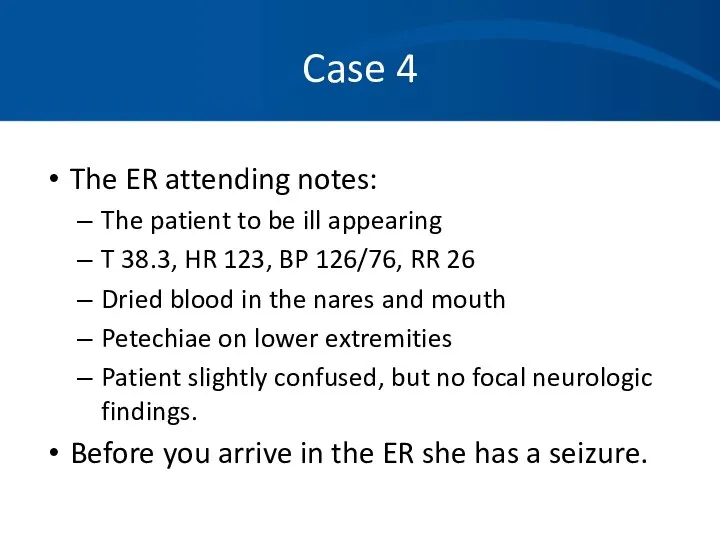
- 36. Case 4 The ER attending notes: The patient to be ill appearing T 38.3, HR 123,
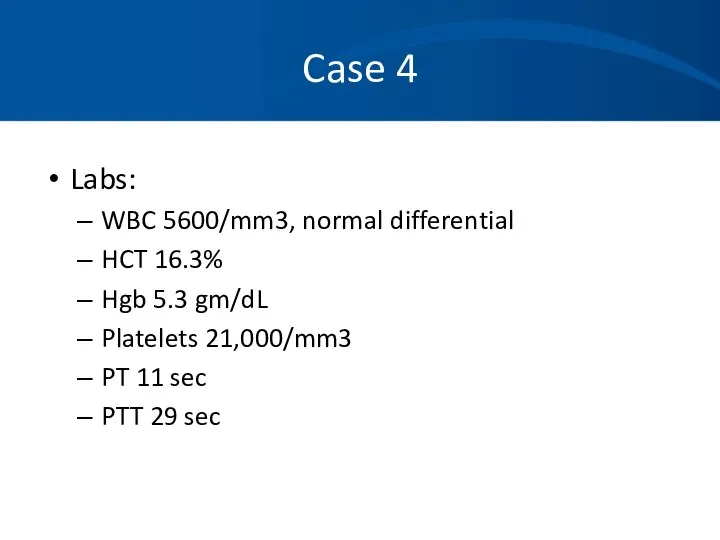
- 37. Case 4 Labs: WBC 5600/mm3, normal differential HCT 16.3% Hgb 5.3 gm/dL Platelets 21,000/mm3 PT 11
- 38. Case 4 Labs: Creatinine 2.4 mg/dL LDH 3000 U/L Bili 3.2 mg/dL, mostly indirect Reticulocyte count
- 39. Case 4
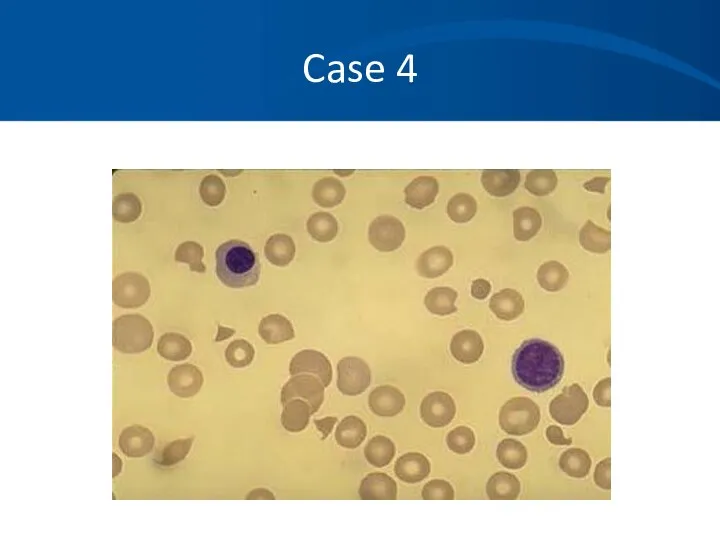
- 40. Case 4 What is your differential diagnosis based on the history, physical, labs and blood smear?
- 41. Case 4 You diagnosis TTP based on the classic pentad and consistent blood smear: Microangiopathic hemolytic
- 42. Case 4 You begin daily plasma exchange procedures using FFP as your replacement fluid. Her mental
- 43. Case 4 Pathophysiology: Typically an inhibitor against ADAMTS- 13, a vWF cleaving to protease leading to
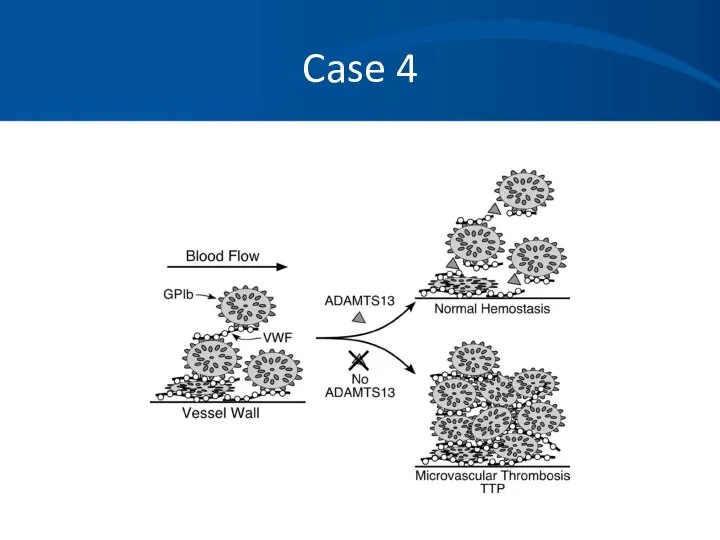
- 44. Case 4
- 45. Case 5 A 36 year old Caucasian man with a history of progressive renal failure over
- 46. Case 5 Physical exam is significant for pale sclera and an AV shunt in his left
- 47. Case 5 Prior labs reveal a hematocrit that was normal 4 years ago, but has steadily
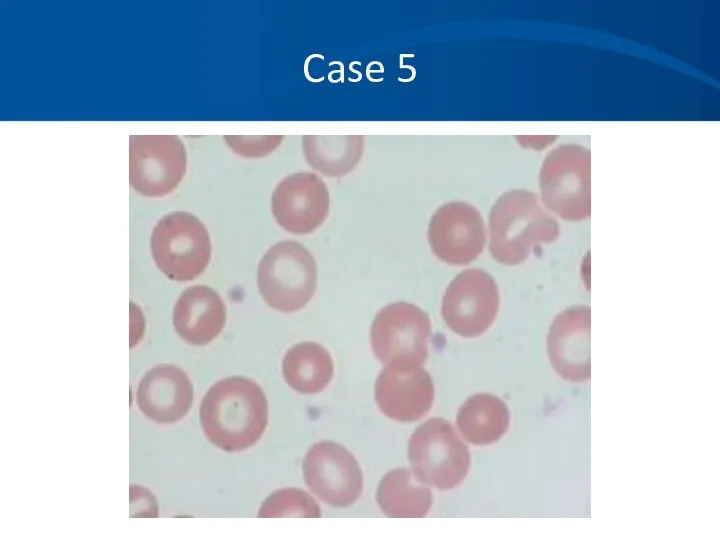
- 48. Case 5
- 49. Case 5 Differential Diagnosis: Anemia of renal failure Iron deficiency anemia Thalassemia Lead poisoning Myelodysplasia Mixed
- 50. Case 5 You order an erythropoietin level which returns at 12 IU ( 4.1-19.5 ) within
- 51. Case 5 You place the patient on 10,000 units of EPO SQ tiw with dialysis. He
- 52. Case 5 He continues on his EPO injections for four months. Soon after he again becomes
- 53. Case 5
- 54. Case 5 You suspect with his increased reticulocytosis and hgb/hct over the last few months he
- 55. Case 5 He again feels much improved and is tolerating the iron fairly well. His hematocrit
- 56. Case 5: Anemia of Chronic Inflammation Mild to moderate anemia that is persistent for greater than
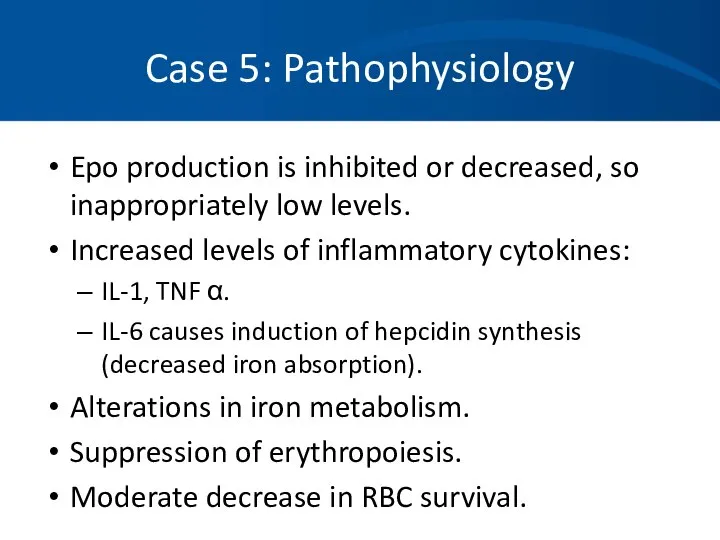
- 57. Case 5: Pathophysiology Epo production is inhibited or decreased, so inappropriately low levels. Increased levels of
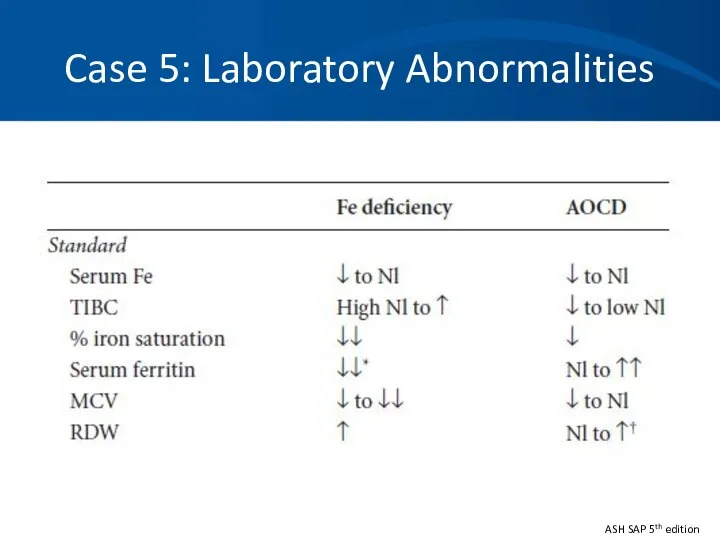
- 58. Case 5: Laboratory Abnormalities ASH SAP 5th edition
- 59. Case 5 ACI does not usually require treatment. Iron replacement is typically not necessary. Erythrocyte-stimulating agent
- 60. Case 6 A 53 year-old female complains of fatigue for 3 months. She falls and breaks
- 61. Case 6 What is the most likely diagnosis? How do you want to proceed with your
- 62. Case 6 Serum protein electrophoresis (SPEP) M- spike of 4.2 gm/dl Immunofixation (IFE) IgG lambda noted
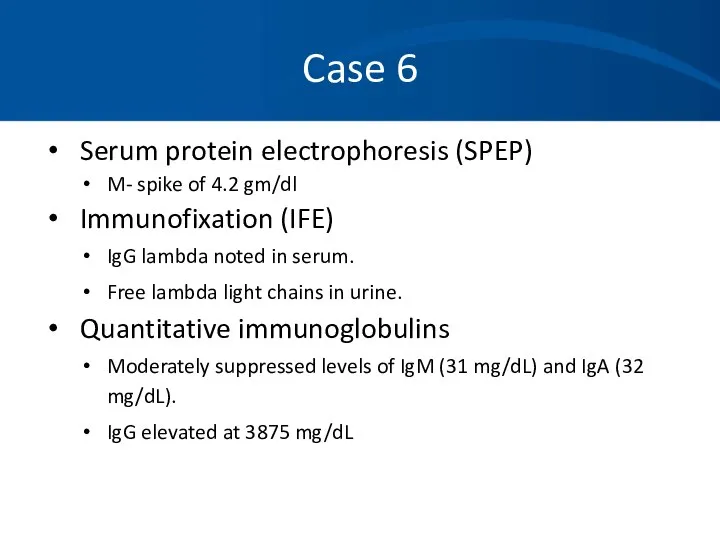
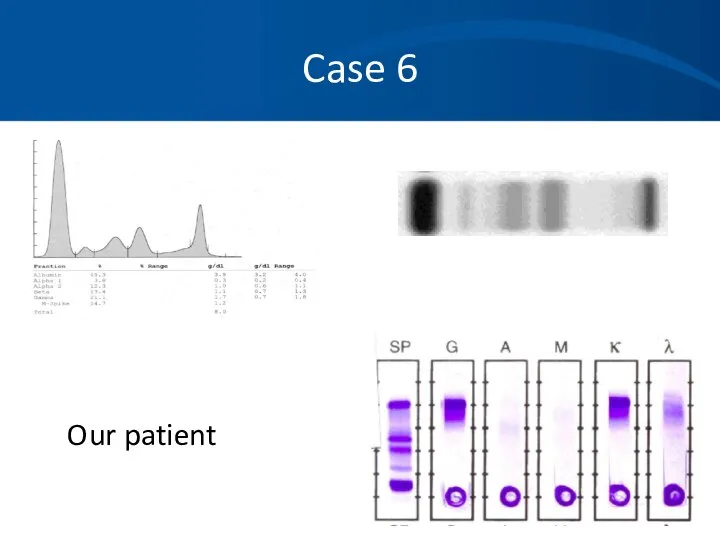
- 63. Case 6 Skeletal survey Multiple lytic lesions throughout the skeleton Bone Marrow aspirate and biopsy Sheets
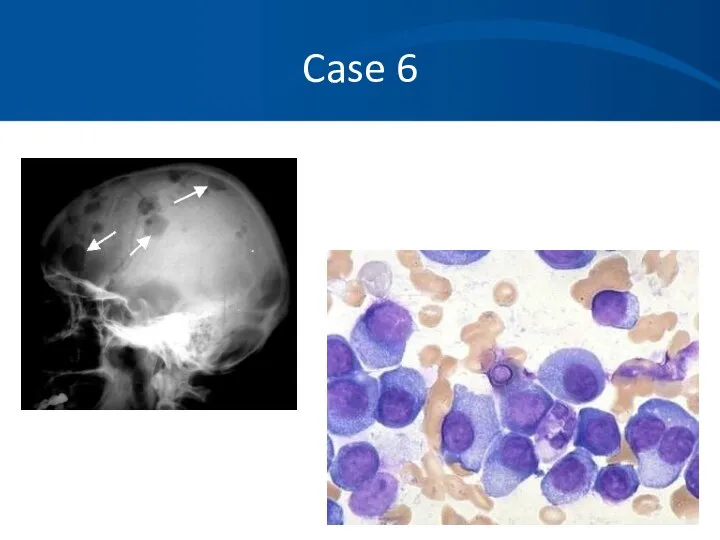
- 64. Case 6 An M-protein is usually seen as a discrete band on agarose gel electrophoresis in
- 65. Case 6: SPEP
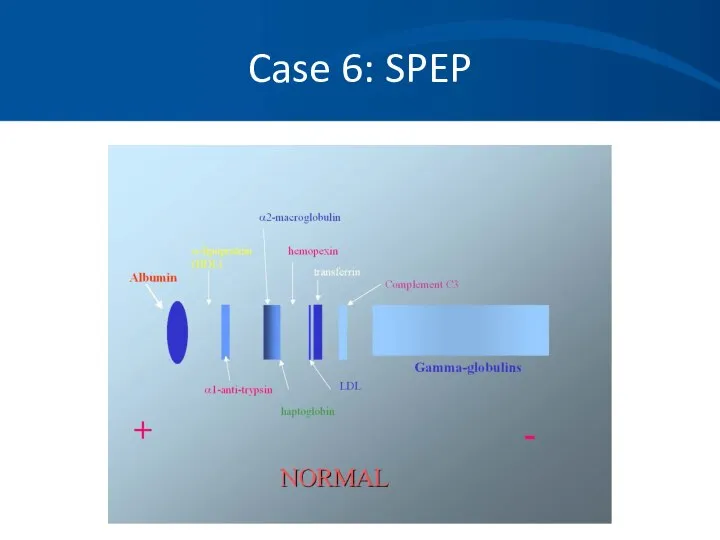
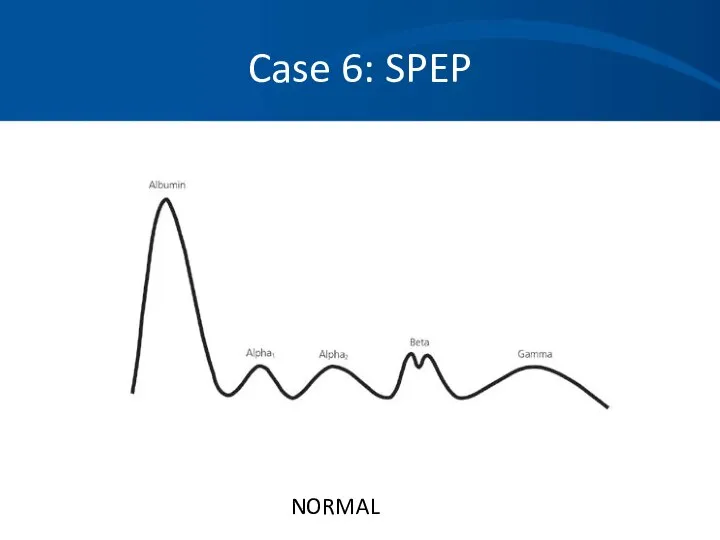
- 66. Case 6: SPEP NORMAL
- 67. Case 6: Myeloma + - α1 α2 β γ *
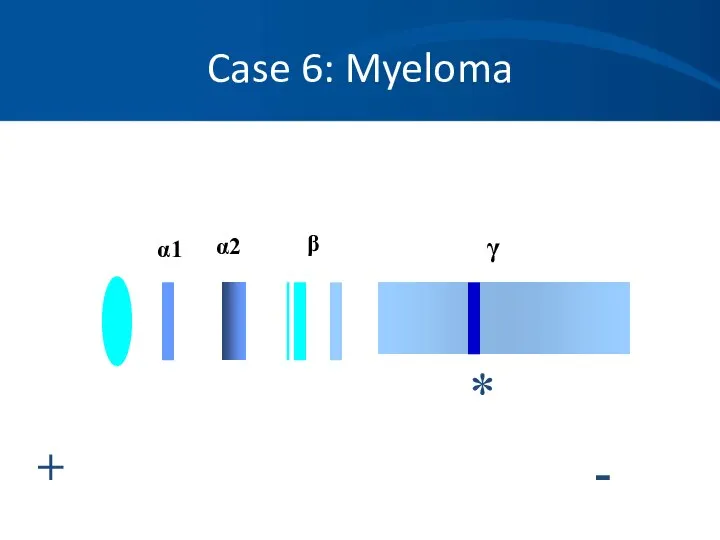
- 68. Case 6: Density Scan + - Albumin α-1 α-2 β
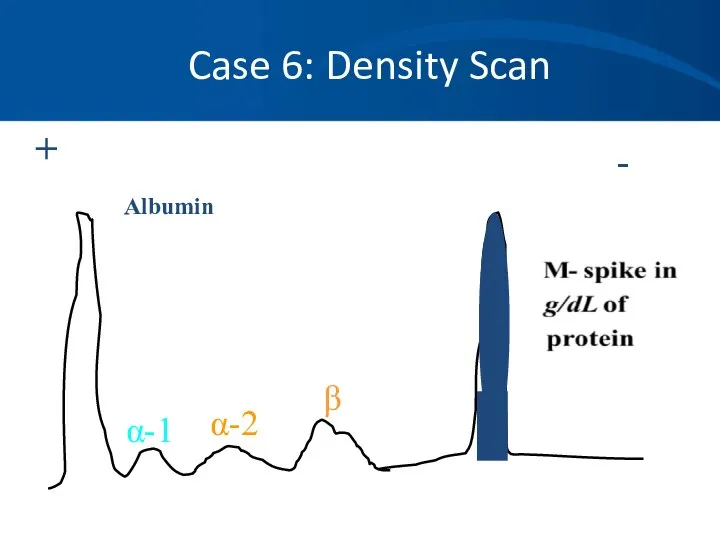
- 69. Case 6 When to order an SPEP: When you suspect multiple myeloma, Waldenstrom’s macroglobulinemia or amyloidosis.
- 70. Case 6 Immunofixation (IFE): Proteins are fractioned on electrophoretic strips: Each lane overlaid with monospecific antisera
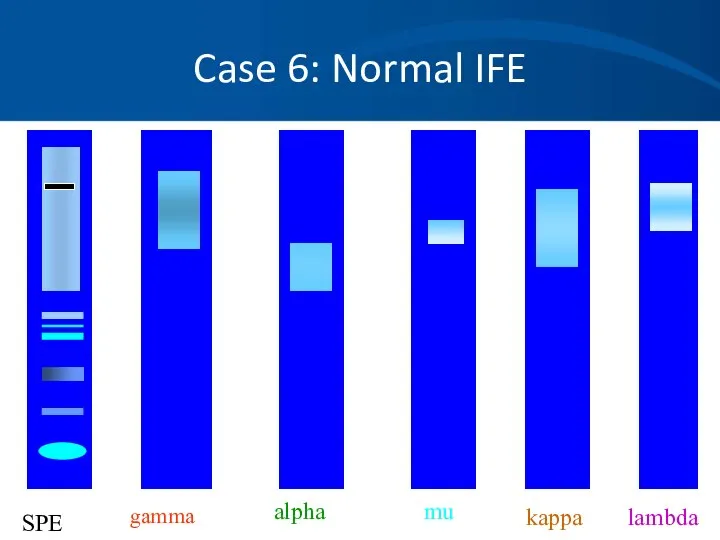
- 71. Case 6: Normal IFE gamma alpha mu kappa lambda SPE
- 72. Case 6 When to order an IFE: To type the paraprotein (M spike) identified on SPEP
- 73. Case 6: Quantitative Immunoglobulins Useful to quantitate: The amount of monoclonal protein Suppression of uninvolved immunoglobulins
- 74. Case 6 Serum light chain assays are newer and a very sensitive technique for measuring serum
- 75. Case 6: Quantitative Immunoglobulins + - Albumin “M-spike”, “Paraprotein” or “M- α-1 α-2 β Note loss
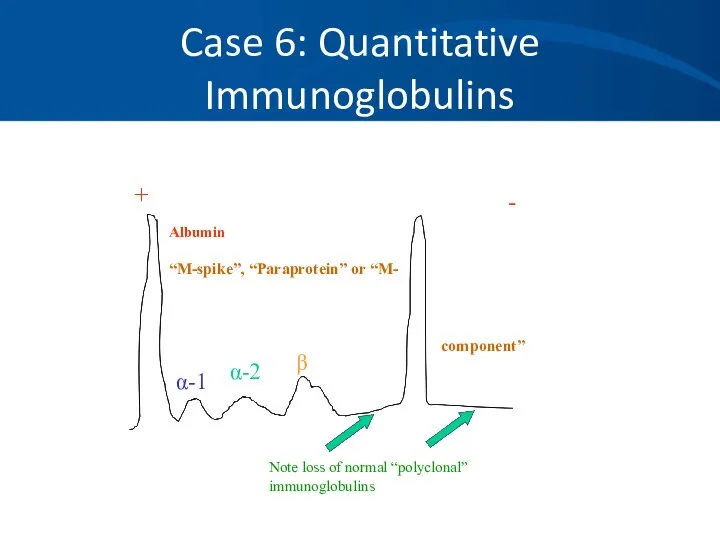
- 76. Case 6 Our patient
- 77. Case 6
- 78. Case 6: Stage III Multiple Myeloma The patient is started on systemic chemotherapy and an autologous
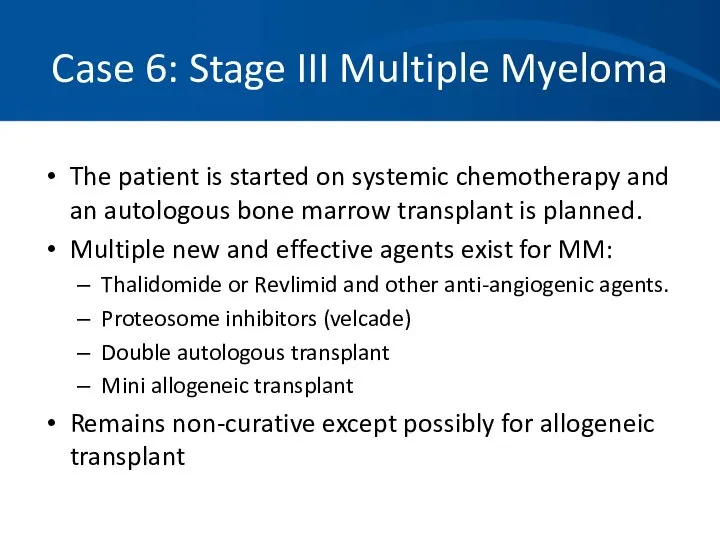
- 79. Case A A 45 yo white male presents to his physician complaining of tiredness and fatigue
- 80. Case A Progression of symptoms Blood in stool Other medications or toxins, including EToH Prior history
- 81. Case A The patient does note he has had black tarry stools for a few weeks
- 82. Case A You order a CBC which shows the following results: Hbg 8.2 gm/dL HCT 26%
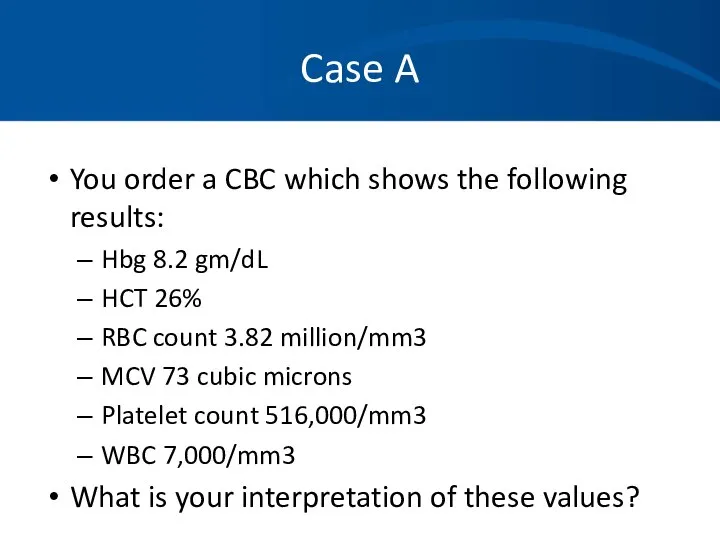
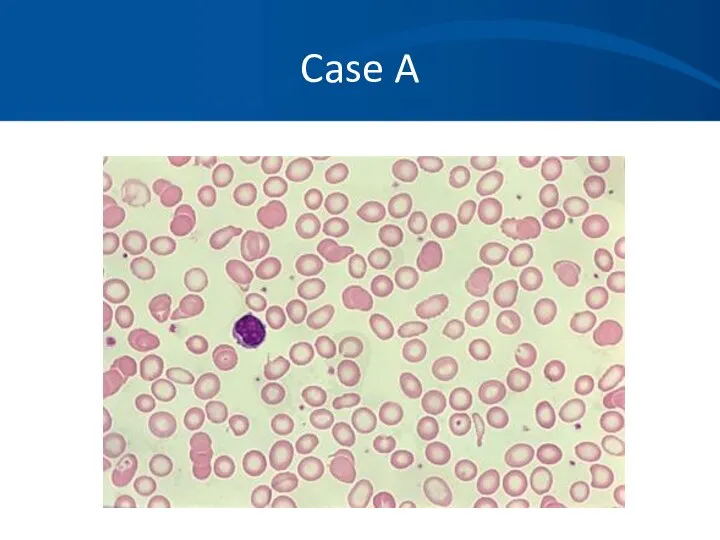
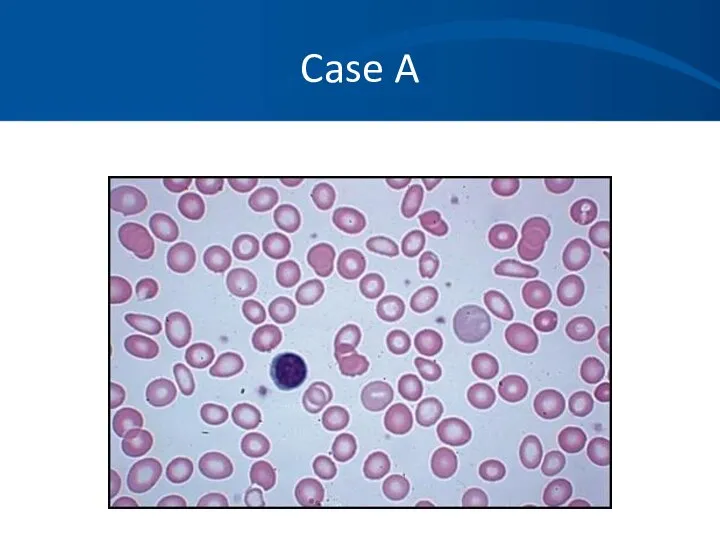
- 83. Case A
- 84. Case A Iron studies: Fe 14 ug/dL TIBC 426 ug/dL % sat 3% Ferritin 10ng/mL Corrected
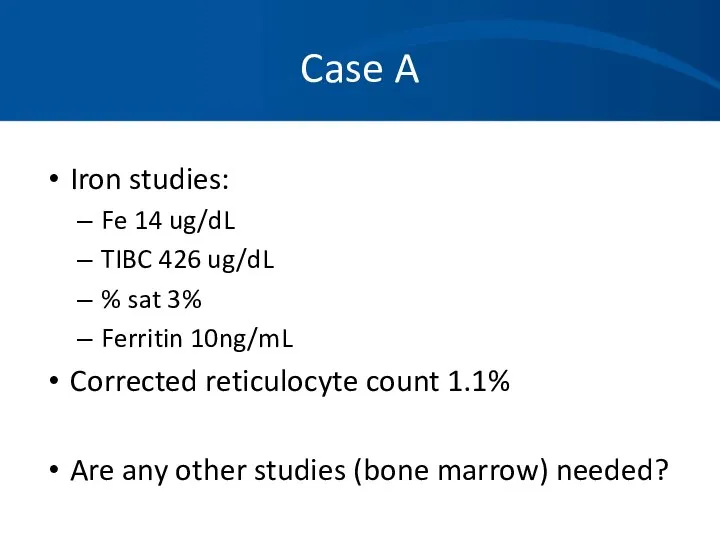
- 85. Case A You confirm iron deficiency likely secondary to NSAID use. An endoscopy confirms a H.pylori
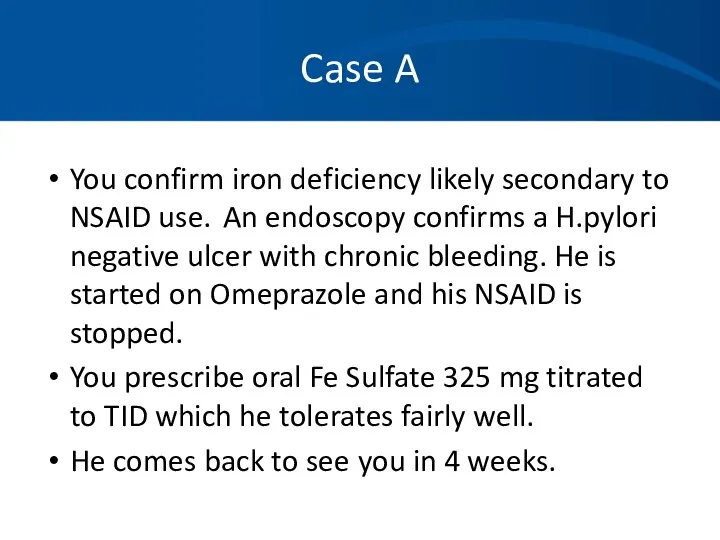
- 86. Case A He feels much better and has experienced resolution of his fatigue and lethargy. Hgb
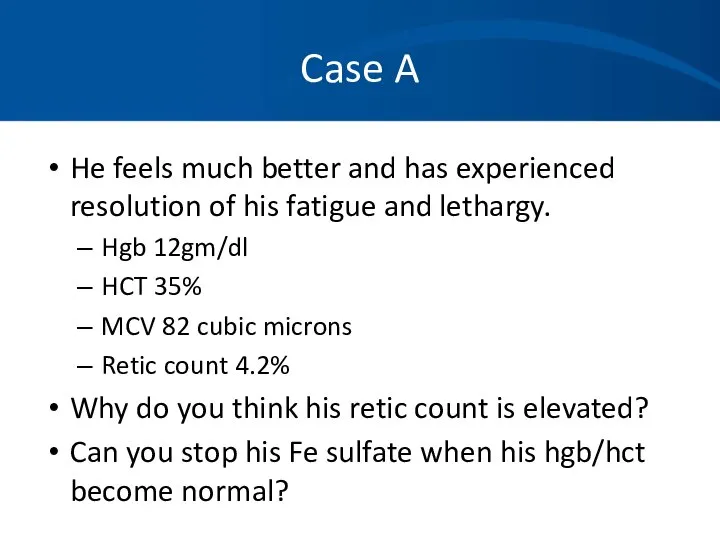
- 87. Case A
- 88. Case B A 67 year old woman with a history of IDDM and treated hypothyroidism is
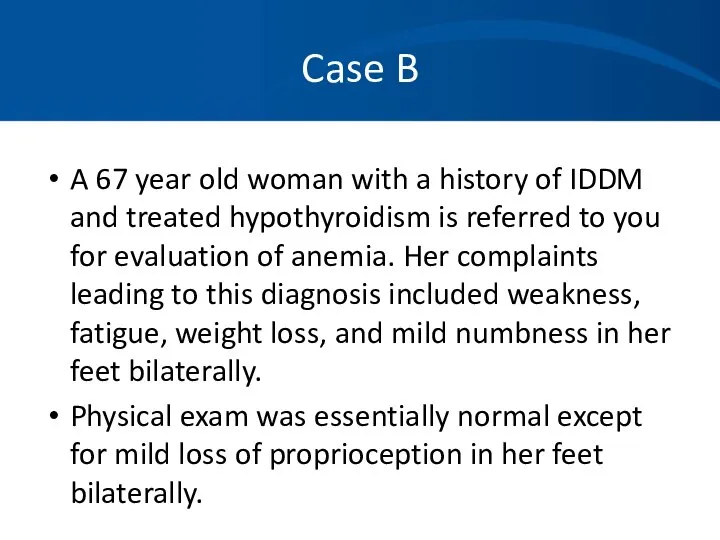
- 89. Case B Current Labs: 2 years ago: How do you interpret these values?
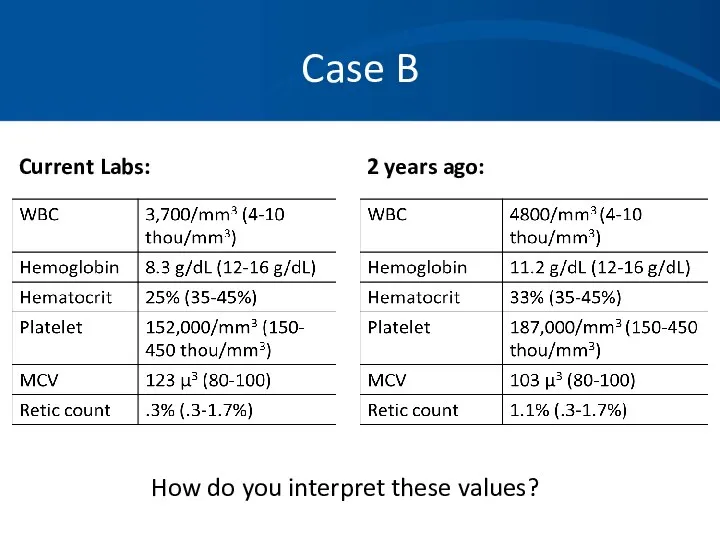
- 90. Case B *Hypersegmented neutrophil, macroovalocytes
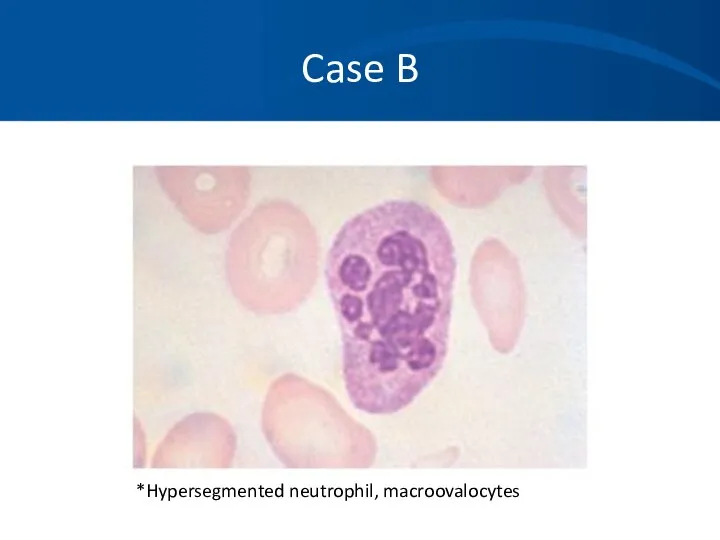
- 91. Case B What tests or procedures do you want to perform to further evaluate this patient?
- 92. Case B You diagnose B12 deficiency and prescribe B12 injections 1000ug weekly x4 then 1000ug a
- 93. Case B: Vitamin B12 Deficiency Found primarily in animal meats. Large hepatic reservoir. Deficiency from decreased
- 94. Case B: Vitamin B12 Deficiency Clinical findings: Insidious onset. Glossitis, weight loss, pale yellow skin. Neurologic
- 95. Case B: Vitamin B12 Deficiency Lab findings: Cobalamin If low-normal (200-350ng/L), check homocysteine and MMA. Both
- 97. Скачать презентацию


 Б±ќаралыќ аќпарат ќ±ралдары
Б±ќаралыќ аќпарат ќ±ралдары Защити себя от ВИЧ
Защити себя от ВИЧ Состояние здоровья и физическое развитие детей и подростков
Состояние здоровья и физическое развитие детей и подростков ЗОЖ
ЗОЖ Гепатит A, C, G, T вирусы
Гепатит A, C, G, T вирусы Остеохондроз позвоночника. Рентгенографические признаки остеохондроза
Остеохондроз позвоночника. Рентгенографические признаки остеохондроза Вплив алкоголю та паління на репродуктивну систему і потомство
Вплив алкоголю та паління на репродуктивну систему і потомство Причины нарушений зрения
Причины нарушений зрения Регуляторные системы организма. Органы иммунной системы. Нормальные и патологические реакции иммунной системы
Регуляторные системы организма. Органы иммунной системы. Нормальные и патологические реакции иммунной системы Гематологические исследования
Гематологические исследования Хронический бронхит
Хронический бронхит Заболевания щитовидной железы
Заболевания щитовидной железы Партограмма
Партограмма Сестринский уход при различных заболеваниях и состояниях. Сестринская помощь в хирургии. Кровотечение и гемостаз
Сестринский уход при различных заболеваниях и состояниях. Сестринская помощь в хирургии. Кровотечение и гемостаз Туберкулез кезіндегі шаралар стандарттары мен алгоритмдері
Туберкулез кезіндегі шаралар стандарттары мен алгоритмдері ICH процесі шеңберіндегі CTD жалпы техникалық құжаты
ICH процесі шеңберіндегі CTD жалпы техникалық құжаты Тестовый контроль по теме: Инфузии и основы трансфузиологии для специальности Сестринское дело
Тестовый контроль по теме: Инфузии и основы трансфузиологии для специальности Сестринское дело Рентгенографическая и компьютерно-томографическая диагностика острых и хронических синуситов
Рентгенографическая и компьютерно-томографическая диагностика острых и хронических синуситов Витамины
Витамины Вербальные и невербальные коммуникации
Вербальные и невербальные коммуникации Правильные ответы викторины по станции Медицинская
Правильные ответы викторины по станции Медицинская Вегетативная нервная система и синдромы ее нарушения
Вегетативная нервная система и синдромы ее нарушения Антибиотики: лечат или калечат
Антибиотики: лечат или калечат То что просто для детей, невозможно для взрослых. 2 класс
То что просто для детей, невозможно для взрослых. 2 класс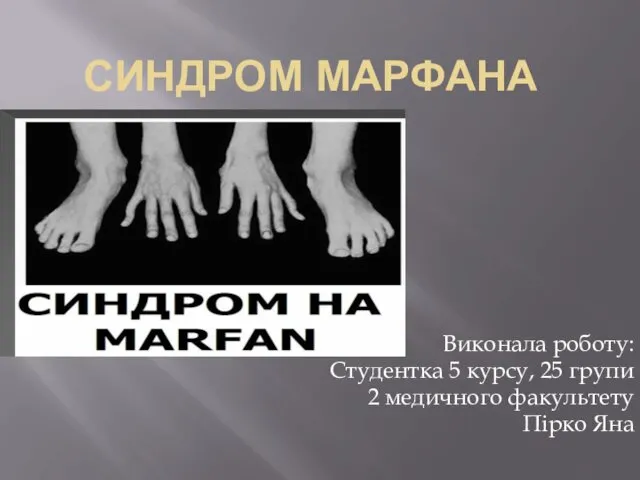 Синдром марфана
Синдром марфана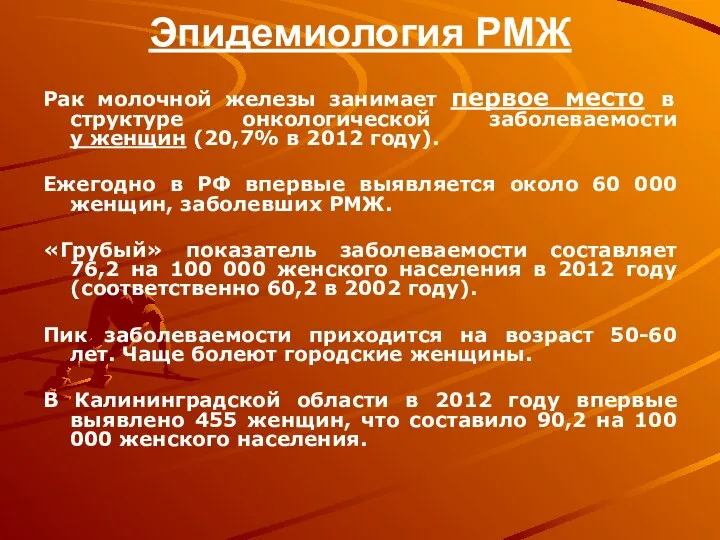 Эпидемиология РМЖ
Эпидемиология РМЖ Комбинированные поражения (лекция № 5)
Комбинированные поражения (лекция № 5) Обследование больного в ортопедическом отделении. Оформление документации. Деонтология и этика в ортопедической стоматологии
Обследование больного в ортопедическом отделении. Оформление документации. Деонтология и этика в ортопедической стоматологии