Содержание
- 2. PART 1 Anatomy of the heart
- 15. Cardiac arrest Checking airway, breathing and circulation 1) Start CPR 30 compression: 2 breath Minimize interruption
- 16. PART 2 Electrically conductive disorders
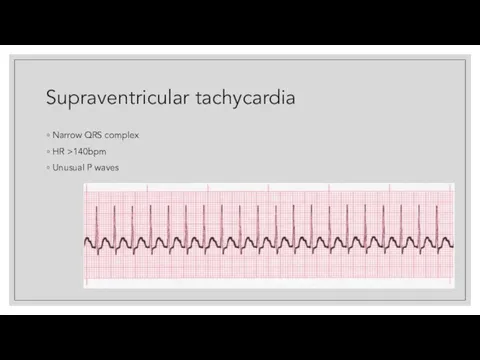
- 17. Supraventricular tachycardia Narrow QRS complex HR >140bpm Unusual P waves
- 18. Supraventricular tachycardia Management: For unstable patients: synchronized cardioversion BP below 90/60 or in syncope For stable
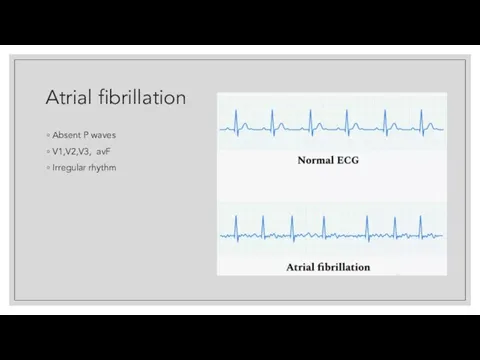
- 20. Atrial fibrillation Absent P waves V1,V2,V3, avF Irregular rhythm
- 21. Atrial fibrillation Management: For unstable patients: synchronized cardioversion For stable patients: Beta blockers (Metoprolol) Diltiazem Verapamil
- 22. Atrial flutter Management For unstable patients: synchronized cardioversion For stable: rate control + warfarin
- 23. Premature ventricular beat Causes: post myocardial infarction, hypokalemia Symptoms: Dyspnea Multiple/multifocal ectopic beats Management If no
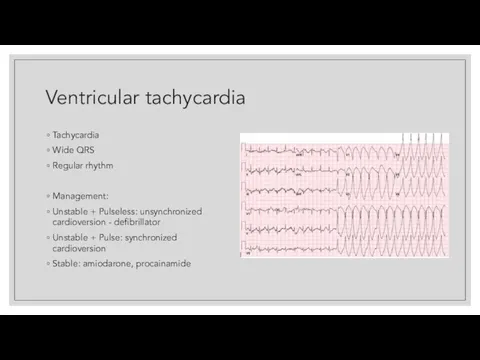
- 24. Ventricular tachycardia Tachycardia Wide QRS Regular rhythm Management: Unstable + Pulseless: unsynchronized cardioversion - defibrillator Unstable
- 25. Ventricular fibrillation Zigzag pattern Managment
- 26. Bradycardia Causes: Sinus node dysfunction Conduction blocks The rhythm with a rate of 50 bpm If
- 27. Wolff Parkinson-white syndrome Short PR interval Wide QRS Delta wave Management Unstable patient: cardioversion Stable: Amiodarone,
- 28. Torsades De Pointes Twisting of the QRS complex around the isoelectric line No P wave Irregular
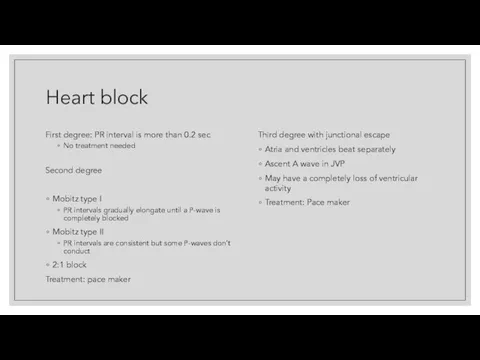
- 29. Heart block First degree: PR interval is more than 0.2 sec No treatment needed Second degree
- 30. Heart block
- 31. Hyperkalemia K+ nomal level 3.5-5.5 If there is ECG changes give IV calcium gluconate If no
- 32. Hypokalemia
- 33. LBBB M shaped comlex usually in leads in V% and V6
- 34. LBBB
- 35. Right Bundle branch block M shapes complex in leads usually in V1 and V2 Usually associated
- 36. Pericarditis Caused by Viral coxsackie virus Diffuse ST segment elevation Treatment: NSAIDs Symptoms of pericarditis Chest
- 37. Hypertrophic obstructive cardiomyopathy Clinical features Sudden loss of consciousness while on exertion, family history, young age
- 38. PART 3
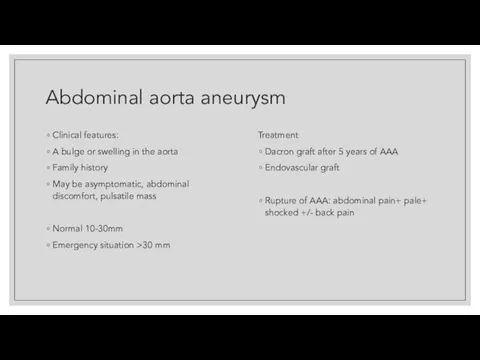
- 39. Abdominal aorta aneurysm Clinical features: A bulge or swelling in the aorta Family history May be
- 40. Aortic dissection Symptoms: severe, sudden, midline tearing or rippig sensation Occlusion of the coronary or kidney
- 41. Superior vena cava syndrome Caused by: external compression or thrombosis Malignant mediastinal tumour Bronchogenic carcinoma Non-Hodgkin
- 42. Superior vena cava syndrome Signs Distended venous distention of the neck and chest wall Facial oedema
- 43. Superior vena cava syndrome
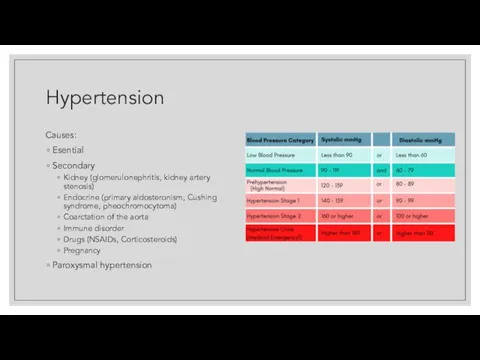
- 44. Hypertension Causes: Esential Secondary Kidney (glomerulonephritis, kidney artery stenosis) Endocrine (primary aldosteronism, Cushing syndrome, pheochromocytoma) Coarctation
- 45. Hypertension Diagnosis: ambulatory 24 hours monitoring Management: Diet, exercises, weight control ACE inhibitors (-pril: Captopril, Lisinopril,
- 46. Dilated Cardiomyopathy Most common causes: Alcohol, Coxsackie virus, drugs (doxorubicin, anthracycline) Clinical features: Pedal oedema Orthopnea
- 47. PART 4
- 48. Mitral Stenosis Clinical features: murmur(mid-diastolic with presystolic accentuation) loud S1 The character is rumbling Site is
- 49. Mitral Regurgitation The most common cause: mitral valve prolapse Clinical features: History of Rheumatic fever Murmur
- 50. Mitral valve prolapse Clinical features: Young females (with familial connection) Atypical chest pain Palpitations Hyperventilation Migranes
- 52. Aortic stenosis Clinical features: Chest pain Syncope SOB Sudden death Loss of consciousness Microangiopathic hemolytic anemia
- 53. Aortic regurgitation Causes by: 80% idiopatic Marfan Syndrome Rheumatic fever Murmur: Early diastolic decrescendo over left
- 55. Constrictive pericarditis Causes: Tb, autoimmune disorders Clinical features: Systemic congestion Paradoxical increase in JVP distention and
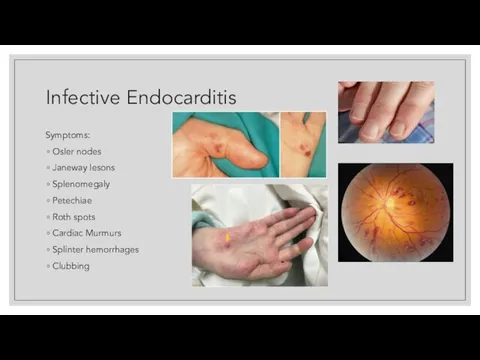
- 56. Infective Endocarditis Infection of the cardiac valves or endometrium Clinical feature: Fever of unknown region Cardiac
- 57. Infective Endocarditis Symptoms: Osler nodes Janeway lesons Splenomegaly Petechiae Roth spots Cardiac Murmurs Splinter hemorrhages Clubbing
- 58. Infective Endocarditis Diagnosis: ERS increase, anemia and leucocytosis In urine: proteinuria and hematuria Blood culture Transesophageal
- 59. Myocardial infarction Criteria of MI: History of prolonged ischemic pain Typical ECG appearance Rise and fall
- 61. Myocardial infarction Management: Provide ABC (Airway, breathing, compression) Aspirin BB and ACE inhibitors Coronary angioplasty Nitrates
- 62. Rheumatic fever Clinical features: Young people 5-15 Acute onset fever, joint pain, malaise Fitting arthralgia mainly
- 64. Rheumatic fever erythema marginatum
- 68. Скачать презентацию























































 Анестезия в амбулаторной травматологии
Анестезия в амбулаторной травматологии Место и значение реабилитации в современной медицине
Место и значение реабилитации в современной медицине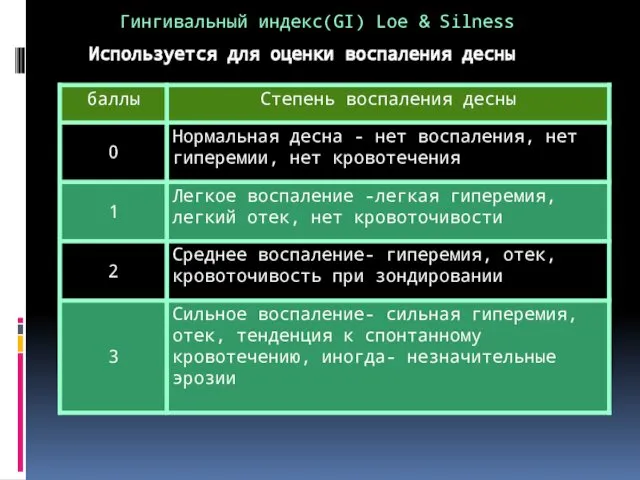 Гингивальный индекс (GI) для оценки воспаления десны
Гингивальный индекс (GI) для оценки воспаления десны Синдром уплотнения легочной ткани. Синдром нарушения бронхиальной проходимости. Особенности у детей
Синдром уплотнения легочной ткани. Синдром нарушения бронхиальной проходимости. Особенности у детей Клинческая анестезиология
Клинческая анестезиология Қан айналымының бұзылыстары
Қан айналымының бұзылыстары Лучевые методы диагностики органов пищеварительной системы у детей
Лучевые методы диагностики органов пищеварительной системы у детей Антисептические и дезинфицирующие средства
Антисептические и дезинфицирующие средства Моббинг и его профилактика
Моббинг и его профилактика Артықшылықты режим. Науқастардың санаттары
Артықшылықты режим. Науқастардың санаттары Дифференциальная диагностика воспалительных заболеваний одонтогенной этиологии
Дифференциальная диагностика воспалительных заболеваний одонтогенной этиологии Внимание и воля
Внимание и воля Блокада левой ножки пучка Гиса
Блокада левой ножки пучка Гиса Инфекционные заболевания методы профилактики
Инфекционные заболевания методы профилактики Шабуылдағы мотоатқыштар бригадасының медициналық қамтамасыз етілуін ұйымдастыру
Шабуылдағы мотоатқыштар бригадасының медициналық қамтамасыз етілуін ұйымдастыру Сахарный диабет
Сахарный диабет Митральная недостаточность
Митральная недостаточность Гистероскопическое лечение раннего рака эндометрия у пациентов высокого хирургического риска
Гистероскопическое лечение раннего рака эндометрия у пациентов высокого хирургического риска Этические проблемы ВИЧ-инфекции
Этические проблемы ВИЧ-инфекции Конституциональные и психосоматические аспекты туберкулезного спондилита (параплегии потта)
Конституциональные и психосоматические аспекты туберкулезного спондилита (параплегии потта) Түсті металлургия саласындағы жұмысшылардың кәсіби аурушаңдығы және алдын - алу жолдары
Түсті металлургия саласындағы жұмысшылардың кәсіби аурушаңдығы және алдын - алу жолдары Изучение хромосом человека в норме и при патологии
Изучение хромосом человека в норме и при патологии Топографическая анатомия передней брюшной стенки. Хирургия грыж
Топографическая анатомия передней брюшной стенки. Хирургия грыж Дети с ограниченными возможностями здоровья
Дети с ограниченными возможностями здоровья Первая помощь при кровотечениях. Правила наложения жгута
Первая помощь при кровотечениях. Правила наложения жгута Расслабляющий массаж ног
Расслабляющий массаж ног Энтеральные вирусные гепатиты А, Е
Энтеральные вирусные гепатиты А, Е Лапароскопічна герніопластика: прогрес чи технологічні вибрики
Лапароскопічна герніопластика: прогрес чи технологічні вибрики