Содержание
- 2. CHRONIC HEART FAILURE Definition Cardiac failure is the inability of the heart to maintain an adequate
- 3. CHF - ETIOLOGY Reduced Ejection fraction ( Preserved Ejection Fraction (>40-50%) High output states Reduced Ejection
- 4. B.Preserved Ejection Fraction (>40-50%) • Pathologic hypertrophy – Primary hypertrophic cardiomyopathy – Secondary to Hypertension –
- 5. CHF - PATHOPHYSIOLOGY Pathophysiology • Low cardiac output leading to organ hypoperfusion and inadequate oxygen supply
- 6. CLASSIFICATION AND CLINICAL MANIFESTATION CLASSIFICATION 1) High output and Low output Failure 2) Right and Left
- 7. CLINICAL MANIFESTATION Major Criteria * Paroxysmal Nocturnal dyspnoea * Neck vein distension * Crackles–Lung fields *
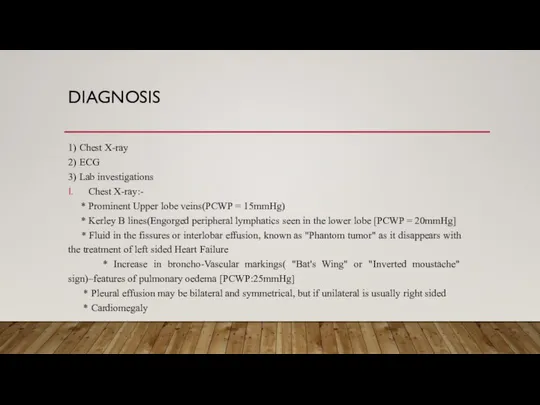
- 8. DIAGNOSIS 1) Chest X-ray 2) ECG 3) Lab investigations Chest X-ray:- * Prominent Upper lobe veins(PCWP
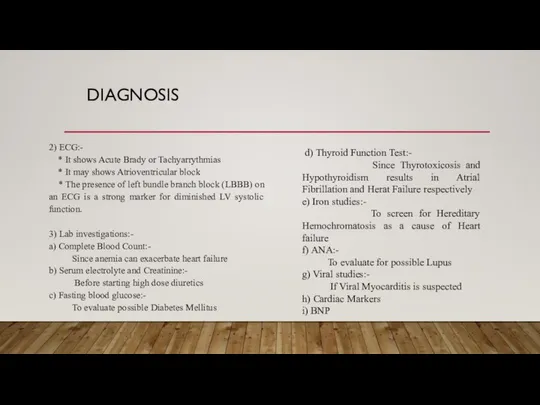
- 9. DIAGNOSIS 2) ECG:- * It shows Acute Brady or Tachyarrythmias * It may shows Atrioventricular block
- 10. MANAGEMENT General principles of Management are 1. Removal of precipitating causes i.e. anemia, arrhythmias, infection, smoking,
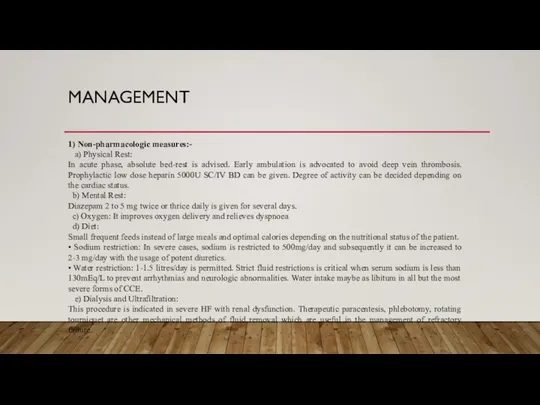
- 11. MANAGEMENT 1) Non-pharmacologic measures:- a) Physical Rest: In acute phase, absolute bed-rest is advised. Early ambulation
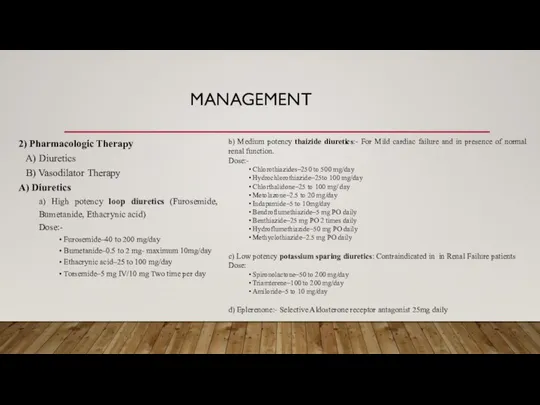
- 12. MANAGEMENT 2) Pharmacologic Therapy A) Diuretics B) Vasodilator Therapy A) Diuretics a) High potency loop diuretics
- 13. MANAGEMENT B) Vasodilator Therapy It is used to Minimise the Workload to the Heart a) Oral
- 14. b) Parenteral Vasodilators They are useful in severe HF. Central Hemodynamic monitoring and optimal titration of
- 15. MANAGEMENT 3) Digitalis:- Digoxin is the most effective drug in the management of heart failure especially
- 16. MANAGEMENT 4) Sympathomimetic Amines:- Norepinephrine, epinephrine, isoprenaline, dopamine and dobutamine. • Dopamine: It increases renal blood
- 17. MANAGEMENT Dose:- Initial bolus dose 12 microgram/kg followed by maintenance dose 0.1 to 0.3 microgram/kg/min Agents
- 18. 1)CONGESTIVE HEART FAILURE HAS BECOME AN EMERGING EPIDEMIC THE IN THE WORLD TODAY, AFFECTING OVER 5
- 20. Скачать презентацию
CHRONIC HEART FAILURE
Definition
Cardiac failure is the inability of the heart to
CHRONIC HEART FAILURE
Definition
Cardiac failure is the inability of the heart to
The terms "Systolic" and "Diastolic" heart failure are replaced by heart failure with reduced ejection fraction (HFrEF - formerly systolic failure) and heart failure with preserved ejection fraction (HFpEF - Formerly diastolic failure).
CHF - ETIOLOGY
Reduced Ejection fraction (<40%)
Preserved Ejection Fraction (>40-50%)
High output
CHF - ETIOLOGY
Reduced Ejection fraction (<40%)
Preserved Ejection Fraction (>40-50%)
High output
Reduced Ejection fraction (<40%)
• Coronary artery disease
– Myocardial infarction
– Myocardial ischaemia
• Chronic pressure overload
– Hypertension
– Obstructive valvular disease
• Chronic volume overload
– Regurgitation valvular disease
– Shunt lesions
– Extracardiac Shunting
• Chronic lung disease
– Corpulmonale
– Pulmonary vascular disorders
• Non-ischaemic dilated cardiomyopathy
– Familial / Genetic disorders
– Infiltrative disorders
• Toxic/drug induced damage
– Metabolic disorders
– Viral
• Chaga's disease
• Disorders of rate and rhythm
• Chronic tachyarrythmias
B.Preserved Ejection Fraction (>40-50%)
• Pathologic hypertrophy
– Primary hypertrophic cardiomyopathy
B.Preserved Ejection Fraction (>40-50%)
• Pathologic hypertrophy
– Primary hypertrophic cardiomyopathy
– Ageing
• Restrictive Cardiomyopathy
Infiltrative disorders (Amyloidosis,Sarcoidosis)
– Storage disorders
• Fibrosis
• Endomyocardial disorders
C.High output states
• Metabolic disorders
– Thyrotoxicosis
– Nutritional (Beriberi)
• Excessive blood flow requirements
– Systemic arteriovenous shunting
– Chronic anemia
CHF - ETIOLOGY
CHF - PATHOPHYSIOLOGY
Pathophysiology
• Low cardiac output leading to organ hypoperfusion and
CHF - PATHOPHYSIOLOGY
Pathophysiology
• Low cardiac output leading to organ hypoperfusion and
• Compensatory adaptations
– Increase in left ventricular mass(LVH) and Volume(dilation)
– Increased Systemic Vascular Resistance
– Activation of Renin-Angiotensin-Aldosterone and Vasopressin (ADH) Systems.
Left ventricular Remodeling:-
• Alterations in myocyte biology
– Excitation-Contraction coupling
– Myosin heavy chain (Foetal) expression
– B-adrenergic desensitization
– Hypertrophy
– Myocytolysis
– Cytoskeletal proteins
• Myocardial changes
– Myocyte loss - necrosis, apoptosis, autophagy
– Matrix degradation and myocardial fibrosis
• Geometry alterations of LV chamber
– LV dilation with increased LV sphericity
– LV wall thinning and Mitral valve incompetence
Preload:-
Preload is the left ventricular end-diastolic pressure and it depends on left ventricular compliance and venous return.
After load:-
Afterload is the left ventricular systolic wall tension that develops during ventricular systole and is determined by aortic valve resistance, the peripheral vascular resistance and the elasticity of major blood vessels.
CLASSIFICATION AND CLINICAL MANIFESTATION
CLASSIFICATION
1) High output and Low output Failure
2) Right
CLASSIFICATION AND CLINICAL MANIFESTATION
CLASSIFICATION
1) High output and Low output Failure
2) Right
3) Forward and Backward Heart Failure
4) Systolic and Diastolic Failure
Clinical Manifestations
Major Criteria
Minor Criteria
Major/Minor criteria
CLINICAL MANIFESTATION
Major Criteria
* Paroxysmal Nocturnal dyspnoea
* Neck vein distension
CLINICAL MANIFESTATION
Major Criteria
* Paroxysmal Nocturnal dyspnoea
* Neck vein distension
* Cardiomegaly
* Acute pulmonary edema
* Third Heart sound– Gallop
* Increased Venous pressure(>16cm H²O)
* Positive (+) Hepato- Jugular reflex
Minor Criteria
* Peripheral(Extremity) Edema
* Nocturnal cough
* Dyspnoea on exertion
* Hepatomegaly
* Pleural Effusion
* Tachycardia
* Decreased vital capacity by 1/3
Major/Minor criteria
*Five days treatment causing weight loss ≥ 4.5kg
* For Diagnosis 1 Major + 2 minor Criterias
DIAGNOSIS
1) Chest X-ray
2) ECG
3) Lab investigations
Chest X-ray:-
* Prominent Upper
DIAGNOSIS
1) Chest X-ray
2) ECG
3) Lab investigations
Chest X-ray:-
* Prominent Upper
* Kerley B lines(Engorged peripheral lymphatics seen in the lower lobe [PCWP = 20mmHg]
* Fluid in the fissures or interlobar effusion, known as "Phantom tumor" as it disappears with the treatment of left sided Heart Failure
* Increase in broncho-Vascular markings( "Bat's Wing" or "Inverted moustache" sign)–features of pulmonary oedema [PCWP:25mmHg]
* Pleural effusion may be bilateral and symmetrical, but if unilateral is usually right sided
* Cardiomegaly
DIAGNOSIS
2) ECG:-
* It shows Acute Brady or Tachyarrythmias
* It
DIAGNOSIS
2) ECG:-
* It shows Acute Brady or Tachyarrythmias
* It
* The presence of left bundle branch block (LBBB) on an ECG is a strong marker for diminished LV systolic function.
3) Lab investigations:-
a) Complete Blood Count:-
Since anemia can exacerbate heart failure
b) Serum electrolyte and Creatinine:-
Before starting high dose diuretics
c) Fasting blood glucose:-
To evaluate possible Diabetes Mellitus
d) Thyroid Function Test:-
Since Thyrotoxicosis and Hypothyroidism results in Atrial Fibrillation and Herat Failure respectively
e) Iron studies:-
To screen for Hereditary Hemochromatosis as a cause of Heart failure
f) ANA:-
To evaluate for possible Lupus
g) Viral studies:-
If Viral Myocarditis is suspected
h) Cardiac Markers
i) BNP
MANAGEMENT
General principles of Management are
1. Removal of precipitating causes i.e. anemia,
MANAGEMENT
General principles of Management are
1. Removal of precipitating causes i.e. anemia,
2. Correction of underlying causes, i.e congenital heart disease, rheumatic heart disease, IHD
3. Control of fluid and sodium retention
4. Enhancement of myocardial contractility
5. Reduction of pulmonary and systemic venous congestion
6. Minimisation of Cardiac workload
MANAGEMENT
1) Non-pharmacologic measures:-
a) Physical Rest:
In acute phase, absolute bed-rest is
MANAGEMENT
1) Non-pharmacologic measures:-
a) Physical Rest:
In acute phase, absolute bed-rest is
b) Mental Rest:
Diazepam 2 to 5 mg twice or thrice daily is given for several days.
c) Oxygen: It improves oxygen delivery and relieves dyspnoea
d) Diet:
Small frequent feeds instead of large meals and optimal calories depending on the nutritional status of the patient.
• Sodium restriction: In severe cases, sodium is restricted to 500mg/day and subsequently it can be increased to 2-3 mg/day with the usage of potent diuretics.
• Water restriction: 1-1.5 litres/day is permitted. Strict fluid restrictions is critical when serum sodium is less than 130mEq/L to prevent arrhythmias and neurologic abnormalities. Water intake maybe as libitum in all but the most severe forms of CCE.
e) Dialysis and Ultrafiltration:
This procedure is indicated in severe HF with renal dysfunction. Therapeutic paracentesis, phlebotomy, rotating tourniquet are other mechanical methods of fluid removal which are useful in the management of refractory failure.
MANAGEMENT
2) Pharmacologic Therapy
A) Diuretics
B) Vasodilator Therapy
A) Diuretics
a) High potency
MANAGEMENT
2) Pharmacologic Therapy
A) Diuretics
B) Vasodilator Therapy
A) Diuretics
a) High potency
Dose:-
• Furosemide–40 to 200 mg/day
• Bumetanide–0.5 to 2 mg- maximum 10mg/day
• Ethacrynic acid–25 to 100 mg/day
• Torsemide–5 mg IV/10 mg Two time per day
b) Medium potency thaizide diuretics:- For Mild cardiac failure and in presence of normal renal function.
Dose:-
• Chlorothiazides–250 to 500 mg/day
• Hydrochlorothiazide–25to 100 mg/day
• Chlorthalidone–25 to 100 mg/ day
• Metolazone–2.5 to 20 mg/day
• Indapamide–5 to 10mg/day
• Bendroflumethiazide–5 mg PO daily
• Benthiazide–25 mg PO 2 times daily
• Hydroflumethiazide–50 mg PO daily
• Methyclothiazide–2.5 mg PO daily
c) Low potency potassium sparing diuretics: Contraindicated in in Renal Failure patients
Dose:
• Spironolactone–50 to 200 mg/day
• Triamterene–100 to 200 mg/day
• Amiloride–5 to 10 mg/day
d) Eplerenone:- Selective Aldosterone receptor antagonist 25mg daily
MANAGEMENT
B) Vasodilator Therapy
It is used to Minimise the Workload to the
MANAGEMENT
B) Vasodilator Therapy
It is used to Minimise the Workload to the
a) Oral vasodilators:-
* ACE inhibitors:- Inhibit the formation of angiotensin 2
* Nitrates:- They are predominantly Venodilators and are useful in CHD with HF
* Hydralazine:- Arterial dilator and it reduces the afterload. Useful in the presence of valvular regurgitant lesions with volume overload
* Adrenergic blockers
° Alpha blockers:- powerful vasodilators and they reduce the systemic vascular resistance and thereby reduce the afterload
° Beta blockers: The adverse effects of endogenous catecholamines on the failing heart can be antagonized by by beta blockers. Beta blockers with ISA activity like pindolol, Xamoterol have been tried. A minimum of two months therapy is required to demonstrate improvement in ejection fraction and exercise tolerance. The drugs approved for use in cardiac failure are carvedilol, metoprolol and bisoprolol.
* Calcium channel blockers: Even though they dilate the vascular smooth muscle, their negative inotropic effect limit the usage in HF. Amlodipine and Felodipine are preferable than Verapamil and Diltiazem in the management of heart failure especially in the presence of Diastolic dysfunction. They enhance the diastolic relaxation of the ventricle. They are absolutely contraindicated in Cardiac Failure with low ejection fraction (below 40%)
b) Parenteral Vasodilators
They are useful in severe HF. Central Hemodynamic monitoring
b) Parenteral Vasodilators
They are useful in severe HF. Central Hemodynamic monitoring
• Nitroglycerin: It is potent venodilator and it relives systemic and pulmonary venous congestion. This drug is useful in Myocardial infarction
Dose:- 10 to 200 microgram/minute
• Sodium nitroprusside: It is very useful in severe hypertensive heart failure and in valvular regurgitant lesions with volume overload
Dose:- 10 to 300 microgram/minute
• Enalaprilat: It can be used in the dose of 1.25 to 5 mg IV six hourly. The indications and adverse effects are similar to oral form of enalapril
• Recombinant BNP-Nesitride: It can be used as a parenteral vasodilators in a dose of 2 microgram/Kg IV bolus followed by continuous IV infusion of 0.01-0.03 microgram/kg/minute.
• Ecadotril: It is an inhibitor of Neutral endopeptidase (NEP) which causes breakdown of BNP
MANAGEMENT
MANAGEMENT
3) Digitalis:-
Digoxin is the most effective drug in the management of
MANAGEMENT
3) Digitalis:-
Digoxin is the most effective drug in the management of
* Supraventricular tachycardia
* Dilated left ventricle
* Impaired systolic function
It causes reversible inhibition of sarcolemmal sodium-potassium adenosine triphosphate. This enhances the myocardial contractility. It slows conduction and prolongs refractory period in Va node, purkinje fibres and thus reduces the ventricular rate
Dose:-
Digitalising dose: Adult– 1 to 1.5 mg. Initiate with p.5 mg and follow it with 0.25 mg 4 times daily.
Maintenance dose: Digoxin–0.25 mg 2 times daily.
• Digoxin specific Fab antibody fragment: Fab antibody fragments are considered when other modes of therapy fail. Each 40mg vial is given in the form of Infusion in 100 ml of normal saline in 30 minutes
Number of vials = Serum level × Weight in Kg/100
MANAGEMENT
4) Sympathomimetic Amines:-
Norepinephrine, epinephrine, isoprenaline, dopamine and dobutamine.
• Dopamine: It increases
MANAGEMENT
4) Sympathomimetic Amines:-
Norepinephrine, epinephrine, isoprenaline, dopamine and dobutamine.
• Dopamine: It increases
heart rate. At a higher dose of 5 to 10 microgram/kg/ minute it causes vasoconstriction.
• Dobutamine: It is a synthetic catecholamines with marked beta¹ and weak beta² and alpha receptor activity
Dose:- 2.5 mg to 10 microgram/ kg/ minute
5) Phosphodiesterase inhibitors:- (Amrinone, Milrinone, Enoximone, Primobendan)
They exert positive inotropic and vasodilator effect through the inhibition of phosphodiesterase 3 and which is a membrane bound enzyme responsible for the breakdown of cyclic AMP.
Dose:
* Amrinone– 750 microgram/kg bolus followed by 2.5 to 10 microgram/kg/minute.
* Milrinone– 50 microgram/kg bolus followed by 0.5 to 0.75 microgram/kg/ minute
• Levosimendon: By increasing the sensitivity of Cardiac muscle to calcium, cardiac contractility is increased without a rise in intracellular calcium- positive inotropic effect.
MANAGEMENT
Dose:- Initial bolus dose 12 microgram/kg followed by maintenance dose
MANAGEMENT
Dose:- Initial bolus dose 12 microgram/kg followed by maintenance dose
Agents that decrease the Mortality in CHF:-
• ACE inhibitors
• Angiotensin receptor blockers
• Beta blockers
• Aldosterone antagonist
• Isosorbide dinitrate
• Hydralazine
Mechanical circulatory support:-
This maybe considered when medical measure fail either in transient Myocardial dysfunction or when alternative procedures like CABG or Cardiac transplantation are planned
a) Intra-aortic balloon pump
b) Ventricular assist devices
c) Enhanced external counter pulsation
d) Resynchronization therapy/biventricular pacing
1)CONGESTIVE HEART FAILURE HAS BECOME AN EMERGING EPIDEMIC THE IN THE
1)CONGESTIVE HEART FAILURE HAS BECOME AN EMERGING EPIDEMIC THE IN THE
2)PHARMACOLOGIC TREATMENTS ARE CONSIDERED A FIRST OPTION FOR ITS TREATMENT, BUT WAVE OF NEW, SURGICAL COURSES OF TREATMENTS HAS BEGAN TO DEVELOP.
3)IT IS ESSENTIAL FOR CRITICAL APPRAISAL OF THESE SURGICAL THERAPIES SO THAT THEY CAN BE OFFERED TO THE GROWING POPULATION SUFFERING FROM HEART FAILURE.
4)ALTHOUGH A COMPLETE HEART TRANSPLANT IS CONSIDERED TO BE THE GOLD STANDARD OF TREATMENT FOR A FAILING HEART, THERE ARE FAR TOO FEW DONOR HEARTS TO SUPPLY AN EVER GROWING POPULATION WHO POTENTIALLY COULD BENEFIT FROM THEM.
5)THIS IS WHY IT IS CRUCIAL TO SEEK OTHER APPROACHES TO CORRECTING THIS PROBLEM.
6)DIAGNOSIS AND TREATMENT OF CHF REMAIN IMPORTANT AND CHALLENGING AND THE UTILIZATION OF AVAILABLE SOURCES AND SOUND UNDERSTANDING OF THE PATHOPHYSIOLOGY AND PHARMACOTHERAPY CAN PRODUCE REWARDING RESULTS WHEN CARING FOR THIS FREQUENTLY ENCOUNTERED AND EVER CHALLENGING DIVERSE PATIENT GROUP.





 Нейрографика
Нейрографика Изменение нервной системы при тиреодной патологии
Изменение нервной системы при тиреодной патологии Даруна - победа над вирусными инфекциями
Даруна - победа над вирусными инфекциями Болезнь Тея - Сакса
Болезнь Тея - Сакса Тірек-қимыл жүйесінің аурулары
Тірек-қимыл жүйесінің аурулары Гигиена лечебно-профилактических организаций. Современные гигиенические проблемы больничного строительства
Гигиена лечебно-профилактических организаций. Современные гигиенические проблемы больничного строительства Рак молочной железы
Рак молочной железы Гипоспадии. Эписпадии
Гипоспадии. Эписпадии Головной мозг
Головной мозг Физиология гемостаза
Физиология гемостаза Здоровый образ жизни. Здоровое полноценное питание
Здоровый образ жизни. Здоровое полноценное питание Асептика и антисептика в акушерстве
Асептика и антисептика в акушерстве Структура и деятельность первичного звена медицинской помощи сельскому населению. Экономические отношения в здравоохранении
Структура и деятельность первичного звена медицинской помощи сельскому населению. Экономические отношения в здравоохранении Государственная политика в области иммунопрофилактики инфекционных болезней
Государственная политика в области иммунопрофилактики инфекционных болезней Аускультация легких
Аускультация легких Индивидуально - психологические свойства личности
Индивидуально - психологические свойства личности Ценностные основания государственной политики в сфере образования
Ценностные основания государственной политики в сфере образования Сифилис: актуальные вопросы
Сифилис: актуальные вопросы Математика в профессии медсестры
Математика в профессии медсестры Брюшной тиф
Брюшной тиф Применение стволовых клеток
Применение стволовых клеток Диагностика и основные синдромы при патологии почек
Диагностика и основные синдромы при патологии почек Антибактериальная терапия
Антибактериальная терапия Первая помощь пострадавшим и её значение
Первая помощь пострадавшим и её значение Определение понятия гипоксия. Сущность понятия двигательная гипоксия
Определение понятия гипоксия. Сущность понятия двигательная гипоксия Стресс
Стресс Основные виды психоактивных веществ. Воздействие на организм различных видов наркотиков
Основные виды психоактивных веществ. Воздействие на организм различных видов наркотиков Аптечка неотложной помощи
Аптечка неотложной помощи