Содержание
- 2. DEFINITIONS Myeloproliferative Neoplasms (MPNs): are a group of clonal myeloid neoplasms in which a genetic alteration
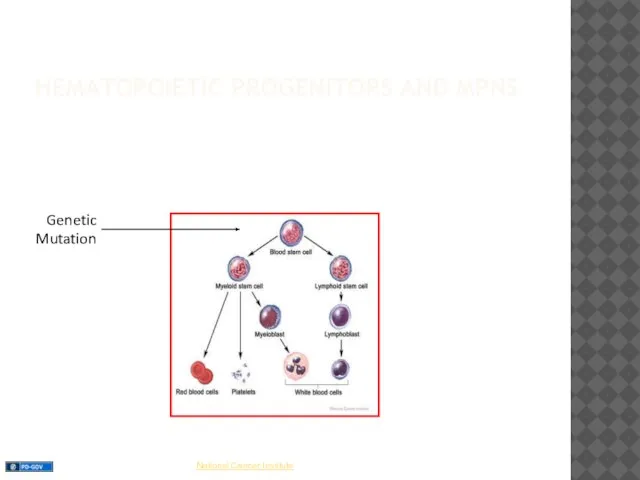
- 3. HEMATOPOIETIC PROGENITORS AND MPNS Genetic Mutation
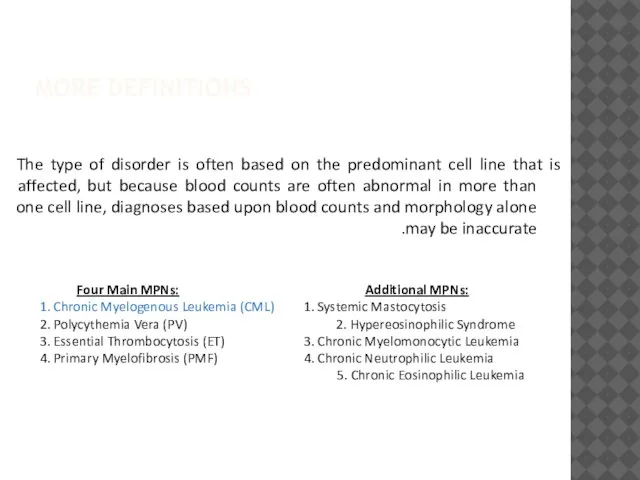
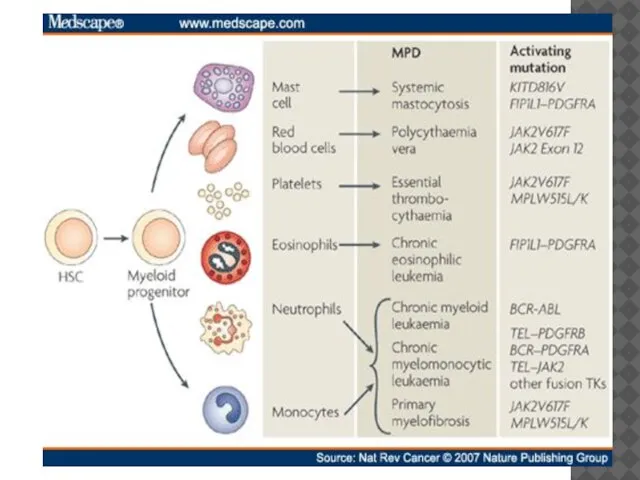
- 4. MORE DEFINITIONS The type of disorder is often based on the predominant cell line that is
- 6. CML DEFINITION A pluripotent stem cell disease characterized by anemia, extreme blood granulocytosis and granulocytic immaturity,
- 7. EPIDEMIOLOGY OF CML Approximately 5,050 cases in the U.S. in 2009 (11% of all leukemias) with
- 8. ETIOLOGY OF CML The risk of getting CML does not seem to be affected by smoking,
- 9. PROJECTION OF CML PREVALENCE UP TO 2050 Modified from R. Hehlmann Assumptions: Population: 500 Mill., mortality:
- 10. CML The first malignancy with identified cytogenetic abnormality, molecular mechanism and specific therapy 1960 – Nowell
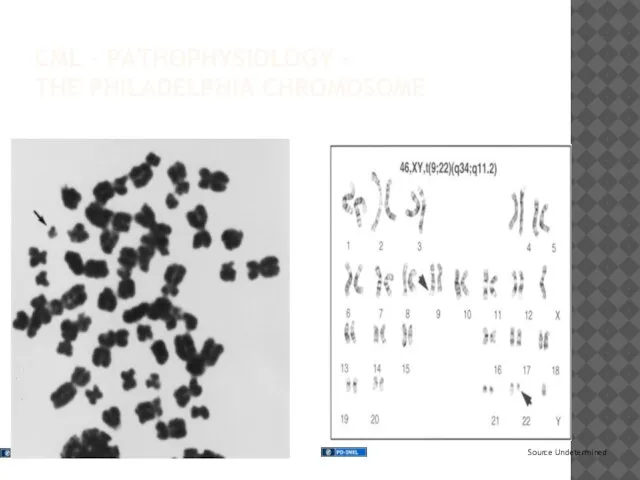
- 11. CML – PATHOPHYSIOLOGY – THE PHILADELPHIA CHROMOSOME
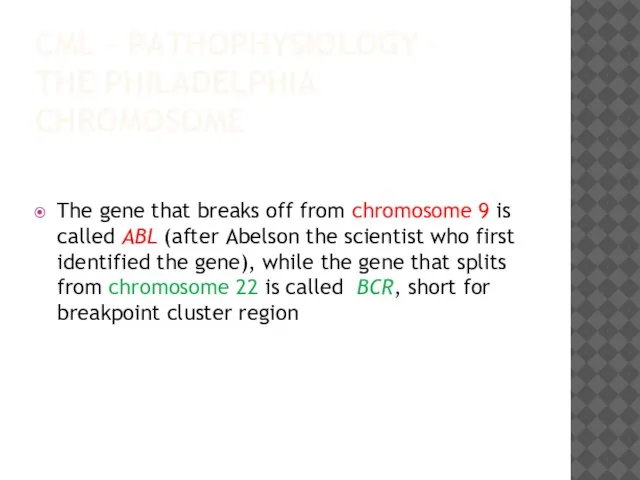
- 12. CML – PATHOPHYSIOLOGY – THE PHILADELPHIA CHROMOSOME The gene that breaks off from chromosome 9 is
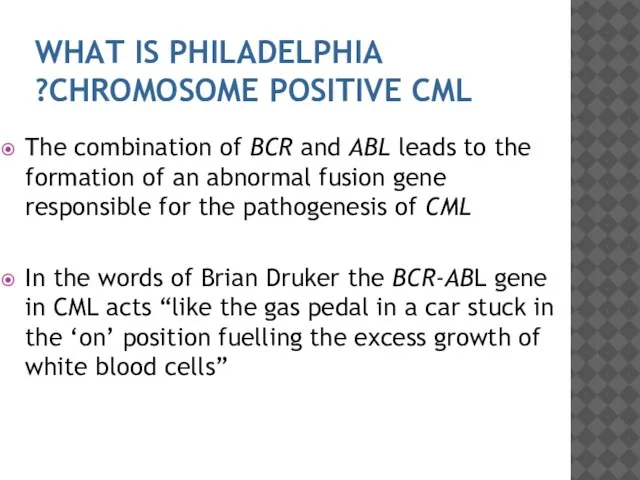
- 13. WHAT IS PHILADELPHIA CHROMOSOME POSITIVE CML? The combination of BCR and ABL leads to the formation
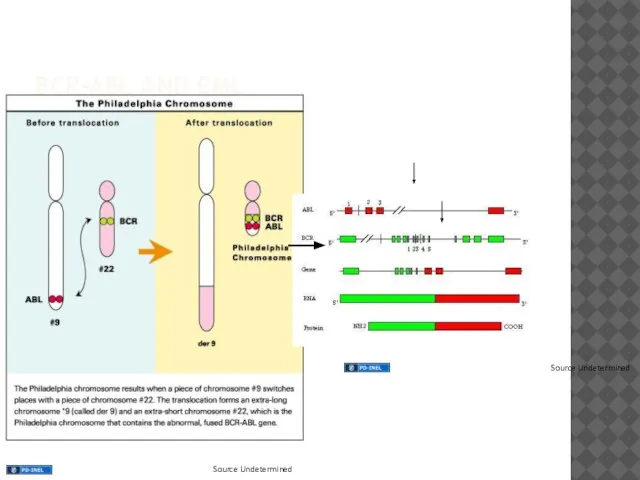
- 14. BCR-ABL AND CML
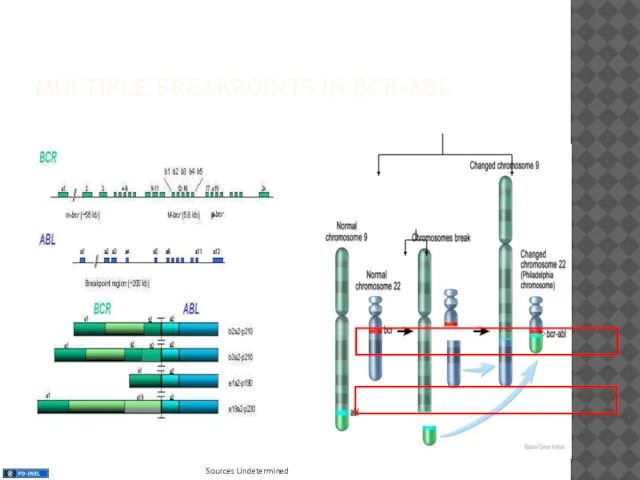
- 15. MULTIPLE BREAKPOINTS IN BCR-ABL
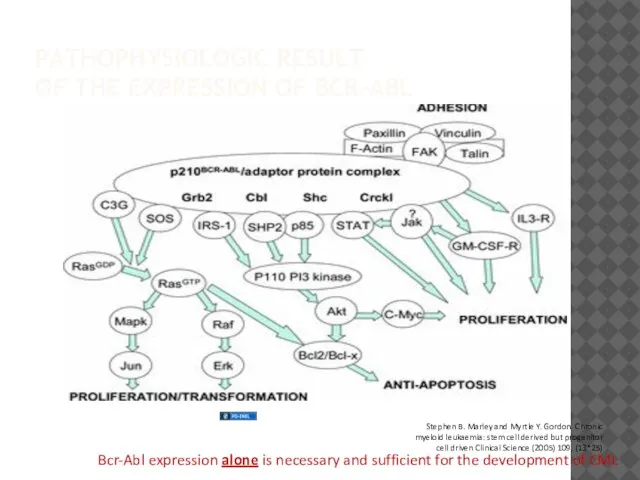
- 16. PATHOPHYSIOLOGIC RESULT OF THE EXPRESSION OF BCR-ABL Bcr-Abl expression alone is necessary and sufficient for the
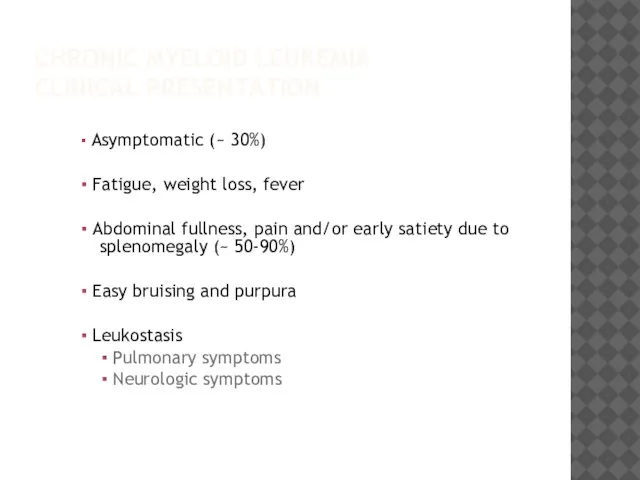
- 17. CHRONIC MYELOID LEUKEMIA CLINICAL PRESENTATION ▪ Asymptomatic (~ 30%) ▪ Fatigue, weight loss, fever ▪ Abdominal
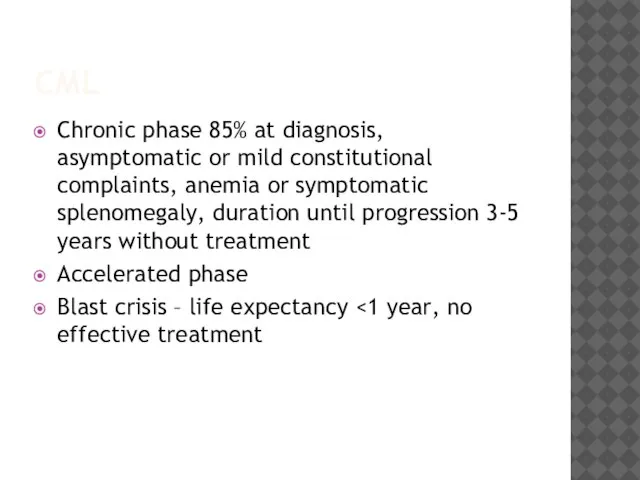
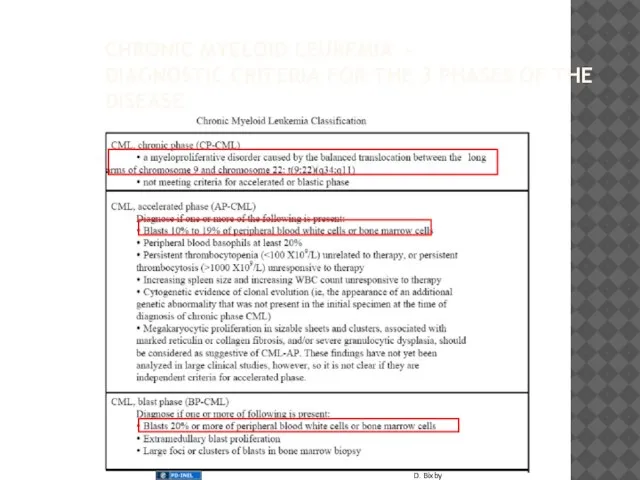
- 18. CML Chronic phase 85% at diagnosis, asymptomatic or mild constitutional complaints, anemia or symptomatic splenomegaly, duration
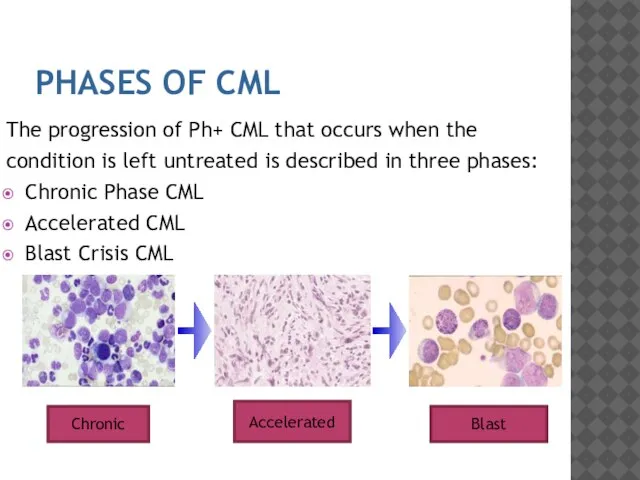
- 19. PHASES OF CML The progression of Ph+ CML that occurs when the condition is left untreated
- 20. CHRONIC MYELOID LEUKEMIA - DIAGNOSTIC CRITERIA FOR THE 3 PHASES OF THE DISEASE
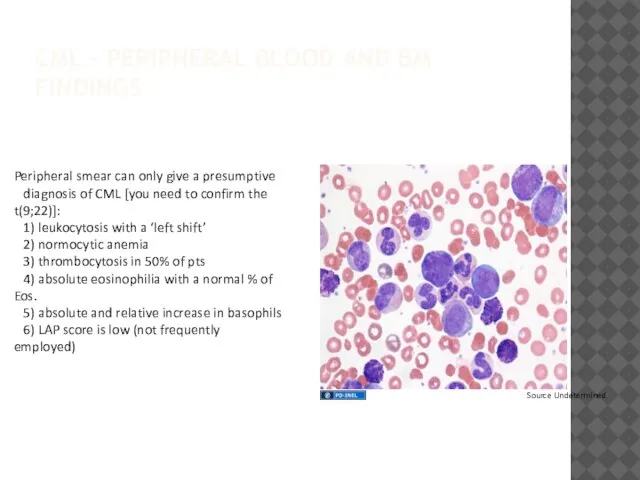
- 21. CML – PERIPHERAL BLOOD AND BM FINDINGS Peripheral smear can only give a presumptive diagnosis of
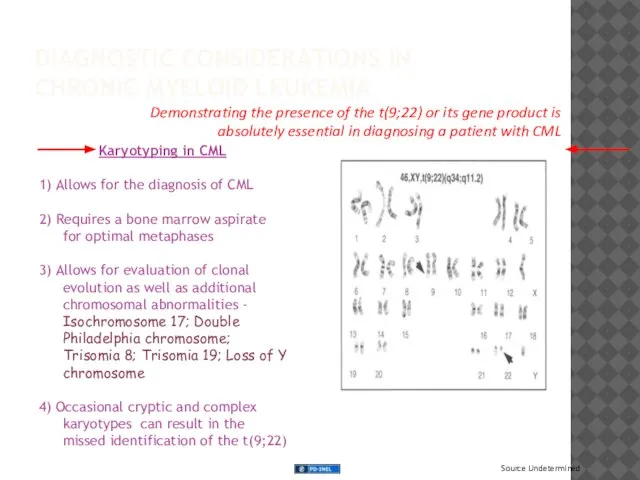
- 22. DIAGNOSTIC CONSIDERATIONS IN CHRONIC MYELOID LEUKEMIA Karyotyping in CML 1) Allows for the diagnosis of CML
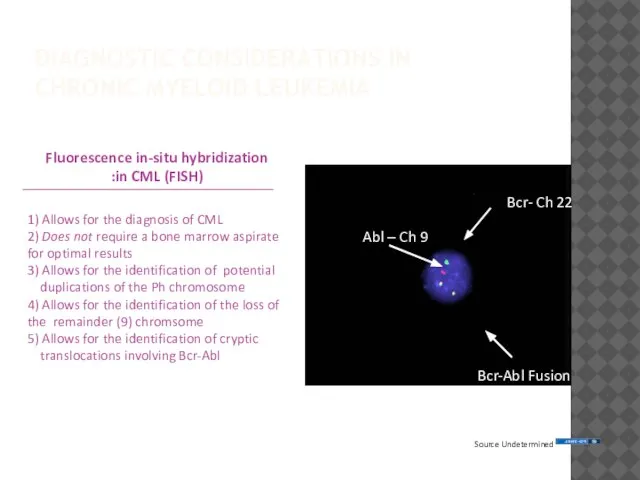
- 23. DIAGNOSTIC CONSIDERATIONS IN CHRONIC MYELOID LEUKEMIA Bcr- Ch 22 Abl – Ch 9 Bcr-Abl Fusion
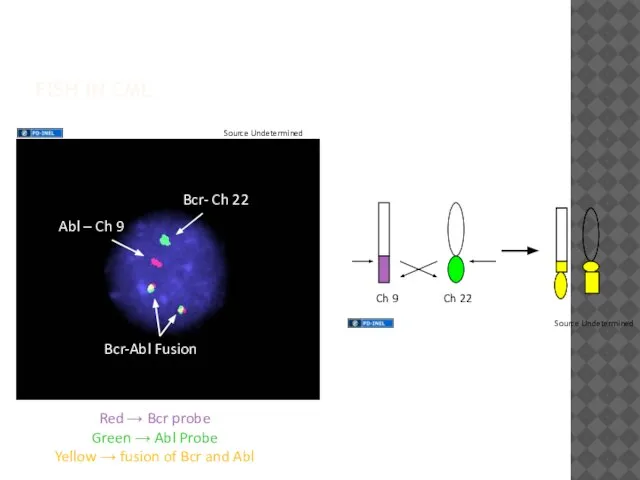
- 24. FISH IN CML Red → Bcr probe Green → Abl Probe Yellow → fusion of Bcr
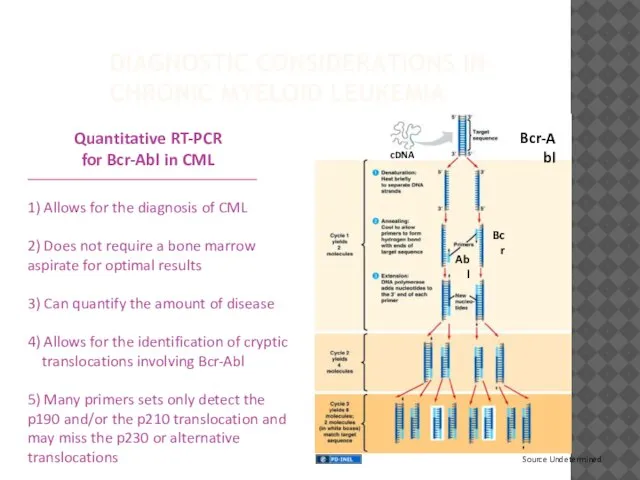
- 25. DIAGNOSTIC CONSIDERATIONS IN CHRONIC MYELOID LEUKEMIA Quantitative RT-PCR for Bcr-Abl in CML 1) Allows for the
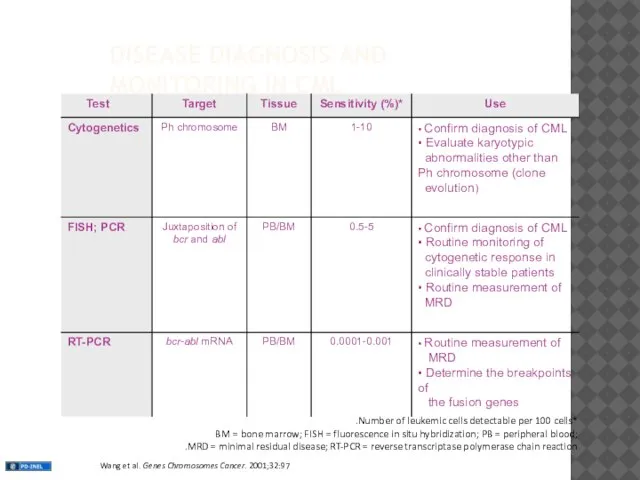
- 26. DISEASE DIAGNOSIS AND MONITORING IN CML *Number of leukemic cells detectable per 100 cells. BM =
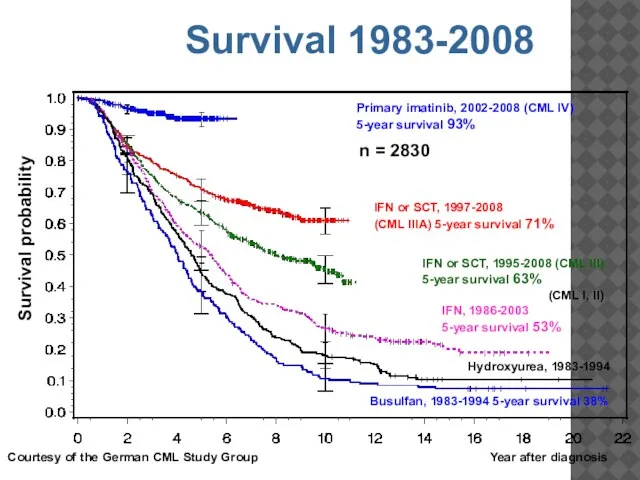
- 27. n = 2830 Year after diagnosis Survival probability Primary imatinib, 2002-2008 (CML IV) 5-year survival 93%
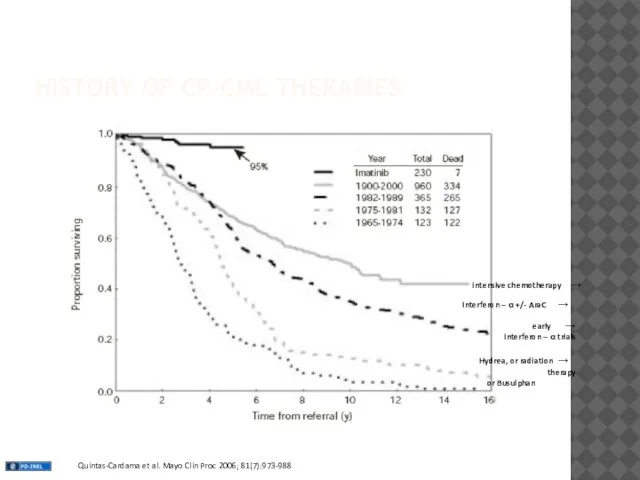
- 28. HISTORY OF CP-CML THERAPIES → Interferon – α +/- AraC → Hydrea, or radiation therapy or
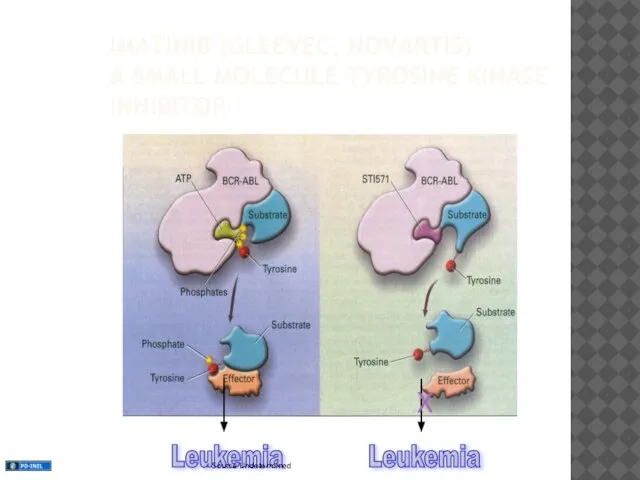
- 29. IMATINIB (GLEEVEC, NOVARTIS) A SMALL MOLECULE TYROSINE KINASE INHIBITOR Leukemia Leukemia X
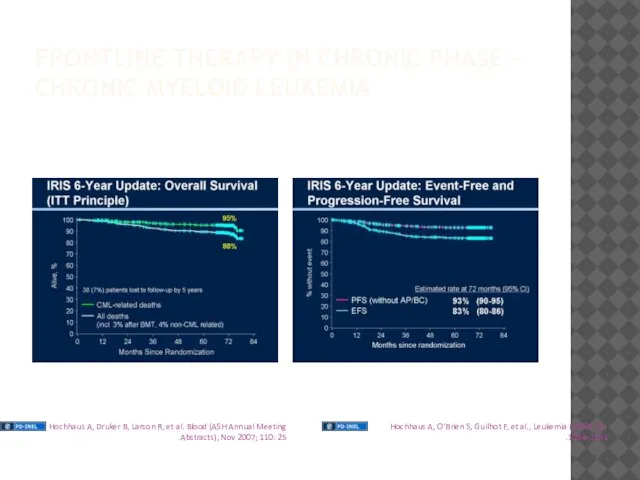
- 30. FRONTLINE THERAPY IN CHRONIC PHASE - CHRONIC MYELOID LEUKEMIA
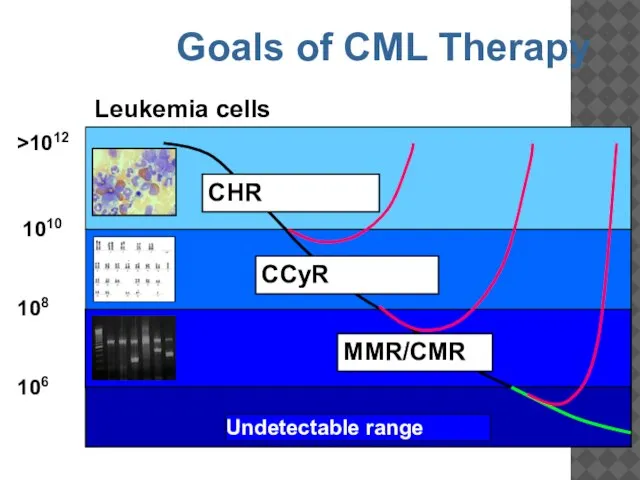
- 31. 1010 >1012 106 108 Leukemia cells CCyR MMR/CMR Undetectable range CHR Goals of CML Therapy
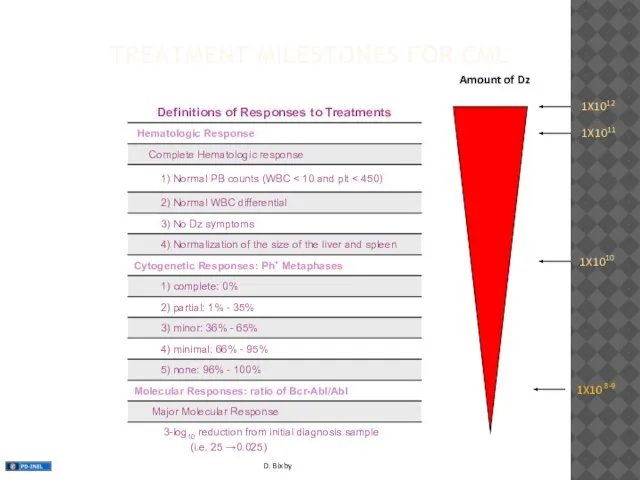
- 32. TREATMENT MILESTONES FOR CML Amount of Dz 1X1012 1X1011 1X1010 1X10 8-9
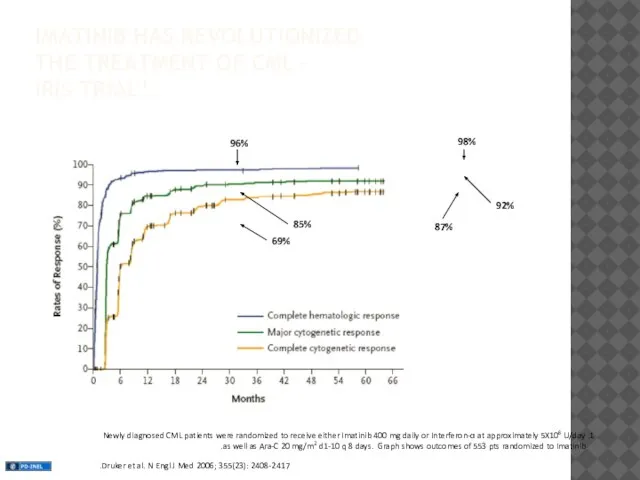
- 33. IMATINIB HAS REVOLUTIONIZED THE TREATMENT OF CML – IRIS TRIAL1 1. Newly diagnosed CML patients were
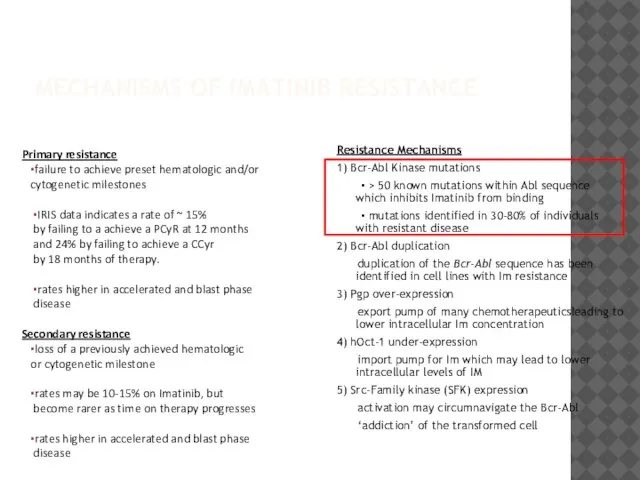
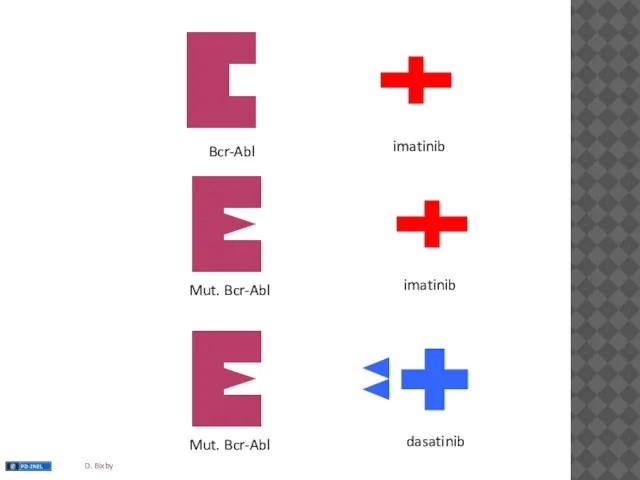
- 34. MECHANISMS OF IMATINIB RESISTANCE Resistance Mechanisms 1) Bcr-Abl Kinase mutations ▪ > 50 known mutations within
- 35. Bcr-Abl imatinib imatinib dasatinib
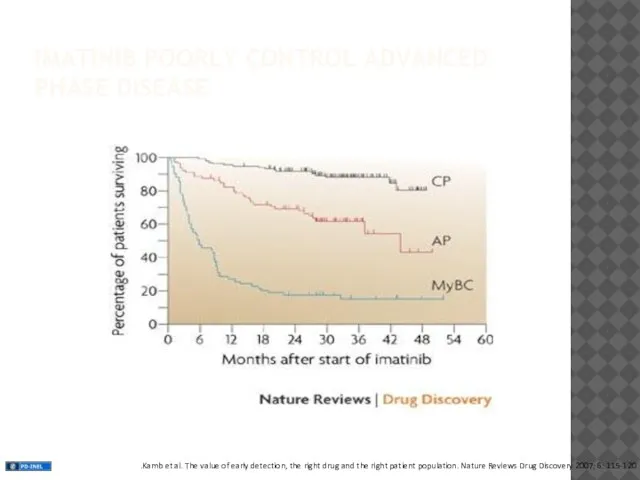
- 37. IMATINIB POORLY CONTROL ADVANCED PHASE DISEASE
- 38. TREATMENT OPTIONS FOR RESISTANT DISEASE 1) Dose Escalation of imatinib 2) Second Generation TKIs 3) Bone
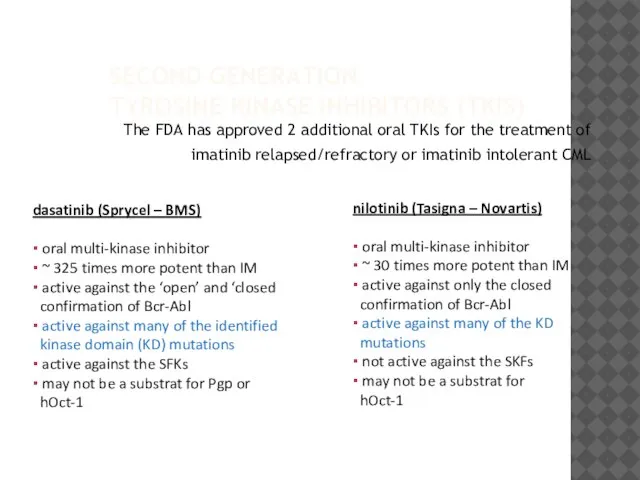
- 39. SECOND GENERATION TYROSINE KINASE INHIBITORS (TKIS) The FDA has approved 2 additional oral TKIs for the
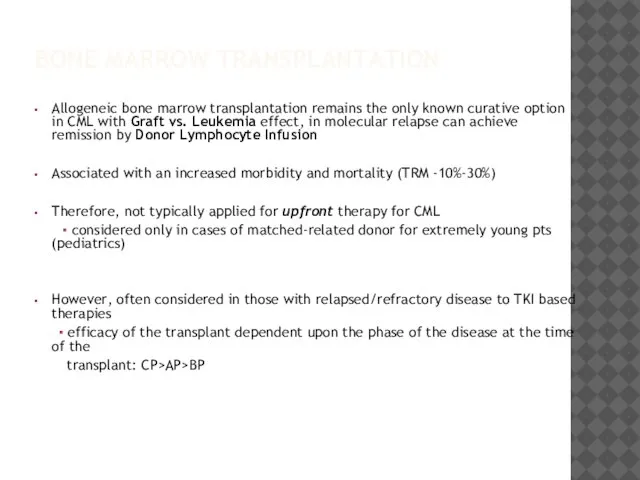
- 40. BONE MARROW TRANSPLANTATION Allogeneic bone marrow transplantation remains the only known curative option in CML with
- 42. Скачать презентацию


 Психологія учіння
Психологія учіння Rickettciaceae. Tarihçe
Rickettciaceae. Tarihçe Рак яичка. Клиническая картина
Рак яичка. Клиническая картина Токсикология ғылымындағы ТМД ғалымдарының рөлі
Токсикология ғылымындағы ТМД ғалымдарының рөлі Профилактика ВИЧ/СПИД. Профилактические программы
Профилактика ВИЧ/СПИД. Профилактические программы Перинатальная асфиксия
Перинатальная асфиксия Инородные тела верхних дыхательных путей
Инородные тела верхних дыхательных путей Современные подходы в диагностике вирусных гепатитов в и с
Современные подходы в диагностике вирусных гепатитов в и с Патофизиология системы иммунобиологического надзора. Иммунодефицитные и иммунодепрессивные состояния. (Лекция 9, 10, 11)
Патофизиология системы иммунобиологического надзора. Иммунодефицитные и иммунодепрессивные состояния. (Лекция 9, 10, 11) Поперечные и косые положения плода. Профессиональная роль акушерки
Поперечные и косые положения плода. Профессиональная роль акушерки Захворювання щитовидної залози
Захворювання щитовидної залози Саркоидоз сердца. Клинический случай
Саркоидоз сердца. Клинический случай Возможности МРТ в оценке плода в антенатальном периоде
Возможности МРТ в оценке плода в антенатальном периоде Интубация трахеи
Интубация трахеи Этика и новые репродуктивные технологии. Моральные проблемы аборта, контрацепции и стерилизации. Лекция 3
Этика и новые репродуктивные технологии. Моральные проблемы аборта, контрацепции и стерилизации. Лекция 3 Семестровое задание по практикуму по общей психологии
Семестровое задание по практикуму по общей психологии Жартылай алмалы пластиналы протезбен емдеудің І – ші клиникалық кезеңі
Жартылай алмалы пластиналы протезбен емдеудің І – ші клиникалық кезеңі Что такое ремоделирование и как этот процесс влияет на приживление имплантов
Что такое ремоделирование и как этот процесс влияет на приживление имплантов Гепатиты
Гепатиты Анастомозы головы и шеи
Анастомозы головы и шеи Көшім балалар психоневрологиялық медициналық-әлеуметтік мекемесіндегі балаларға жүргізген зерттеу нәтежиелері
Көшім балалар психоневрологиялық медициналық-әлеуметтік мекемесіндегі балаларға жүргізген зерттеу нәтежиелері Жизненные циклы семьи
Жизненные циклы семьи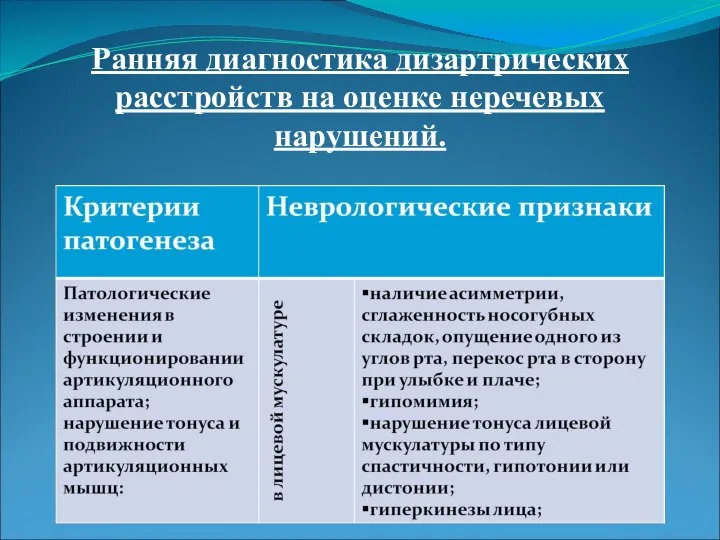 Ранняя диагностика дизартрических расстройств на оценке неречевых нарушений
Ранняя диагностика дизартрических расстройств на оценке неречевых нарушений Межличностные отношения. Вопросы
Межличностные отношения. Вопросы Лечебно-эвакуационное обеспечение населения в чрезвычайных ситуациях
Лечебно-эвакуационное обеспечение населения в чрезвычайных ситуациях Презентация по медицине Демиелинизирующие заболевания ЦНС
Презентация по медицине Демиелинизирующие заболевания ЦНС  Псориаз. Эпидемиология. Вульгарный, экссудативный, пустулезный псориаз
Псориаз. Эпидемиология. Вульгарный, экссудативный, пустулезный псориаз Причины дизонтогенеза. Общие и частные закономерности аномального развития
Причины дизонтогенеза. Общие и частные закономерности аномального развития