Ecg interpretations. How to analyze a rhythm. Normal sinus rhythm. Heart arrhythmias. Diagnosing a myocardial infarction
Содержание
- 2. Course Objectives To recognize the normal rhythm of the heart - “Normal Sinus Rhythm.” To recognize
- 3. Learning Modules ECG Basics How to Analyze a Rhythm Normal Sinus Rhythm Heart Arrhythmias Diagnosing a
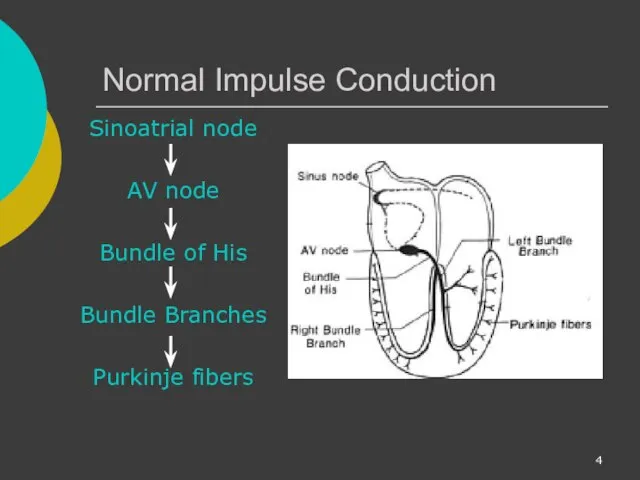
- 4. Normal Impulse Conduction Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers
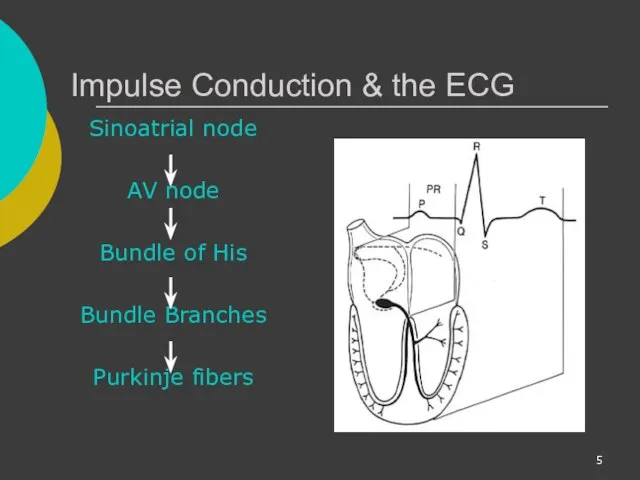
- 5. Impulse Conduction & the ECG Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers
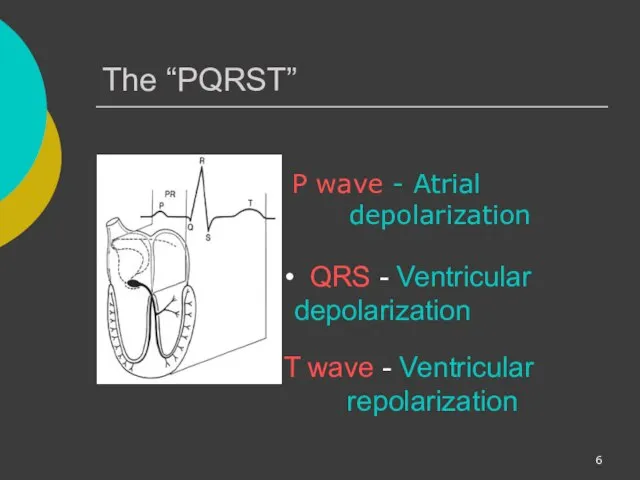
- 6. The “PQRST” P wave - Atrial depolarization T wave - Ventricular repolarization QRS - Ventricular depolarization
- 7. The PR Interval Atrial depolarization + delay in AV junction (AV node/Bundle of His) (delay allows
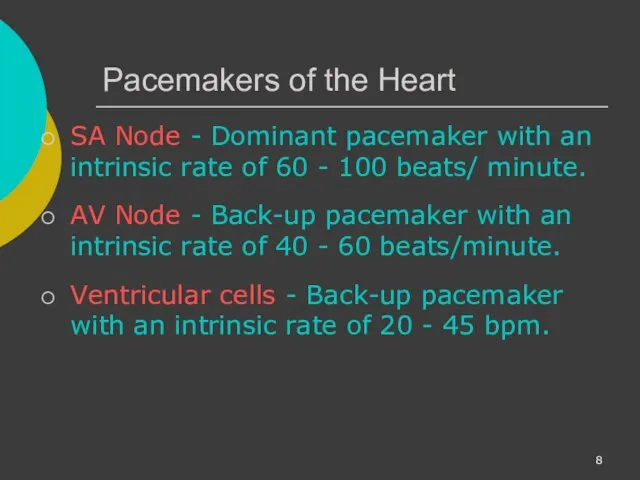
- 8. Pacemakers of the Heart SA Node - Dominant pacemaker with an intrinsic rate of 60 -
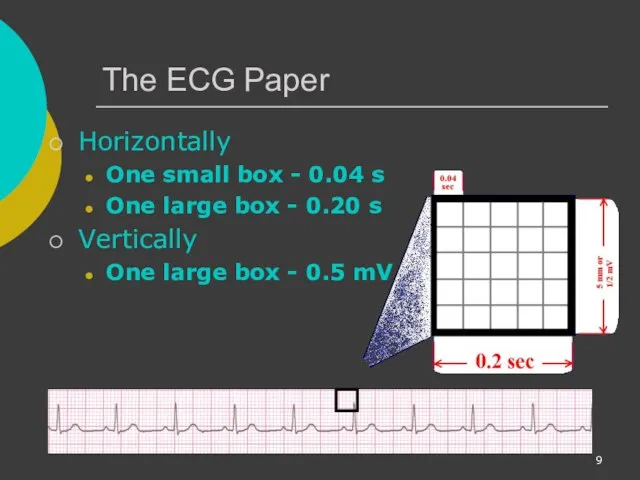
- 9. The ECG Paper Horizontally One small box - 0.04 s One large box - 0.20 s
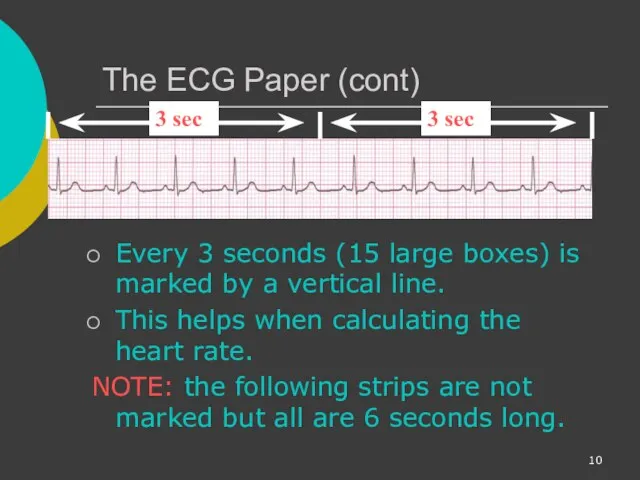
- 10. The ECG Paper (cont) Every 3 seconds (15 large boxes) is marked by a vertical line.
- 11. ECG Rhythm Interpretation Really Very Easy How to Analyze a Rhythm
- 12. Rhythm Analysis Step 1: Calculate rate. Step 2: Determine regularity. Step 3: Assess the P waves.
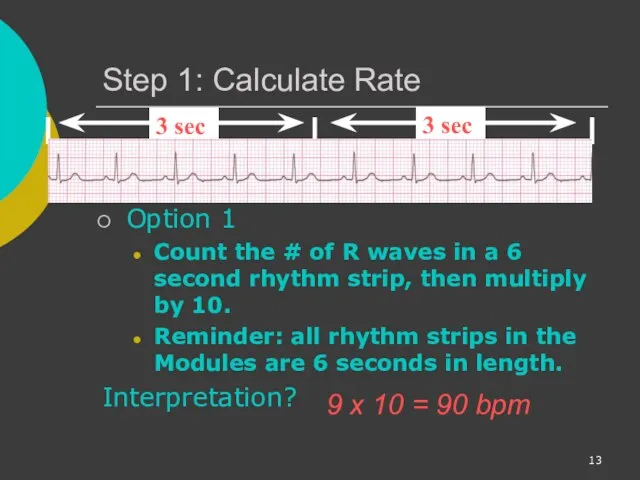
- 13. Step 1: Calculate Rate Option 1 Count the # of R waves in a 6 second
- 14. Step 1: Calculate Rate Option 2 Find a R wave that lands on a bold line.
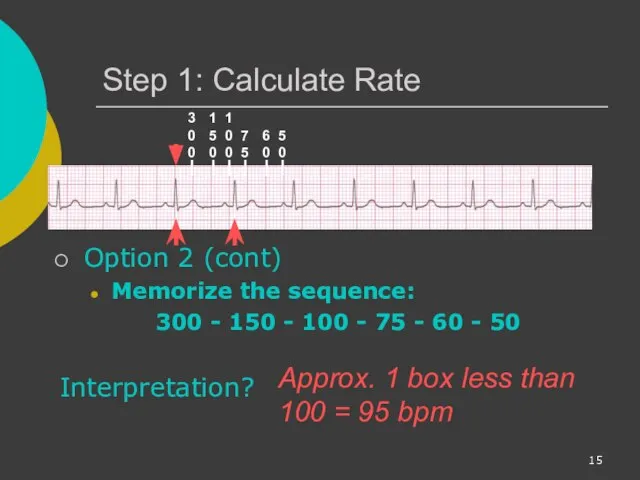
- 15. Step 1: Calculate Rate Option 2 (cont) Memorize the sequence: 300 - 150 - 100 -
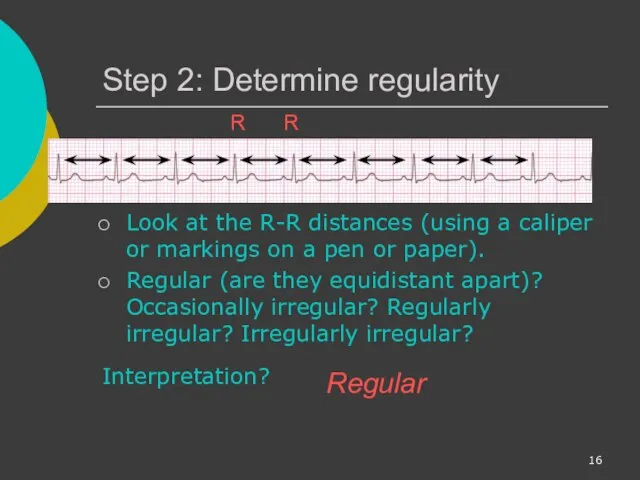
- 16. Step 2: Determine regularity Look at the R-R distances (using a caliper or markings on a
- 17. Step 3: Assess the P waves Are there P waves? Do the P waves all look
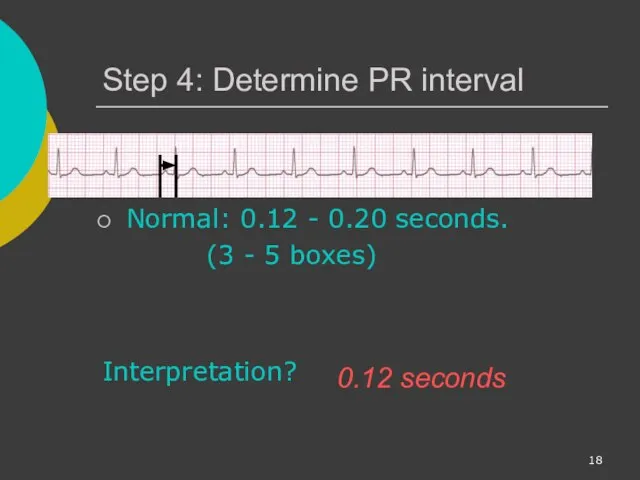
- 18. Step 4: Determine PR interval Normal: 0.12 - 0.20 seconds. (3 - 5 boxes) Interpretation? 0.12
- 19. Step 5: QRS duration Normal: 0.04 - 0.12 seconds. (1 - 3 boxes) Interpretation? 0.08 seconds
- 20. Rhythm Summary Rate 90-95 bpm Regularity regular P waves normal PR interval 0.12 s QRS duration
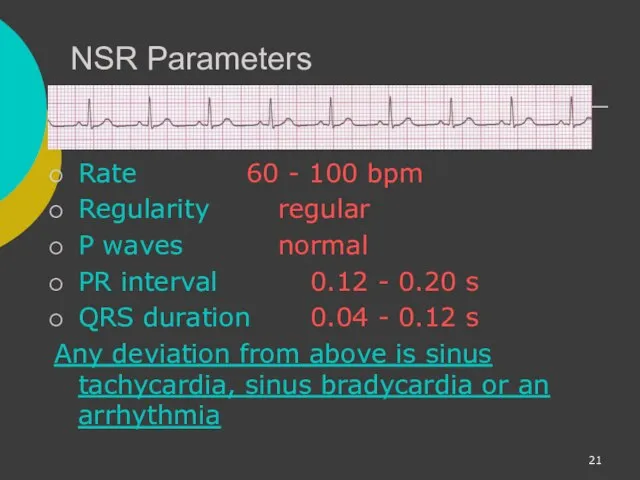
- 21. NSR Parameters Rate 60 - 100 bpm Regularity regular P waves normal PR interval 0.12 -
- 22. Arrhythmia Formation Arrhythmias can arise from problems in the: Sinus node Atrial cells AV junction Ventricular
- 23. SA Node Problems The SA Node can: fire too slow fire too fast Sinus Bradycardia Sinus
- 24. Atrial Cell Problems Atrial cells can: fire occasionally from a focus fire continuously due to a
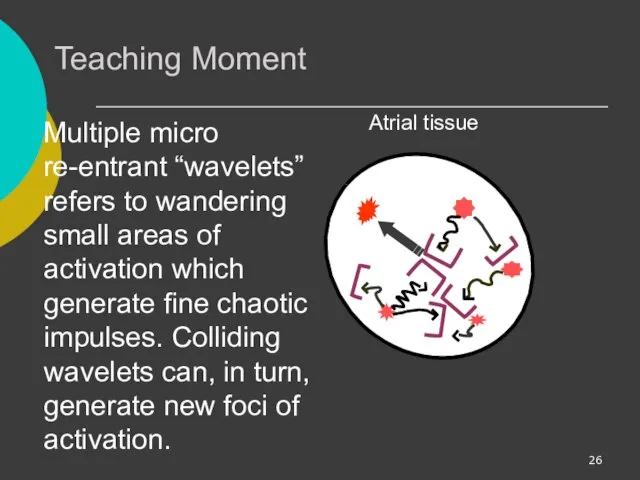
- 25. Atrial Cell Problems Atrial cells can also: • fire continuously from multiple foci or fire continuously
- 26. Teaching Moment Multiple micro re-entrant “wavelets” refers to wandering small areas of activation which generate fine
- 27. AV Junctional Problems The AV junction can: fire continuously due to a looping re-entrant circuit block
- 28. Ventricular Cell Problems Ventricular cells can: fire occasionally from 1 or more foci fire continuously from
- 29. Arrhythmias Sinus Rhythms Premature Beats Supraventricular Arrhythmias Ventricular Arrhythmias AV Junctional Blocks
- 30. Sinus Rhythms Sinus Bradycardia Sinus Tachycardia Sinus Arrest Normal Sinus Rhythm
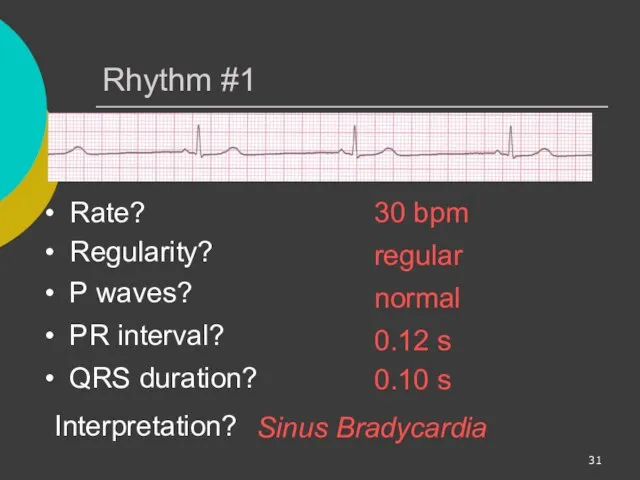
- 31. Rhythm #1 30 bpm Rate? Regularity? regular normal 0.10 s P waves? PR interval? 0.12 s
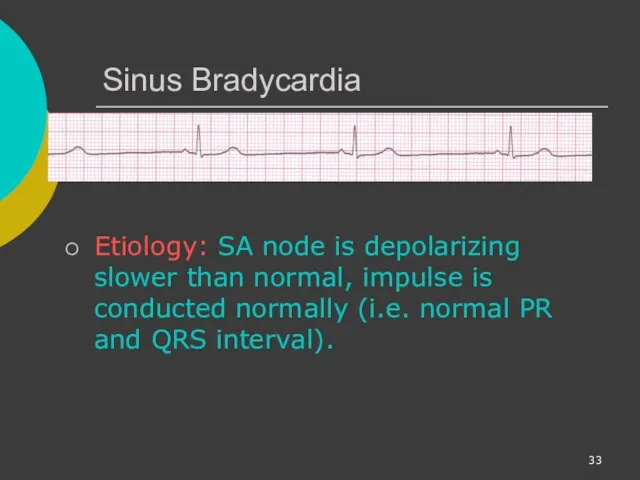
- 32. Sinus Bradycardia Deviation from NSR - Rate
- 33. Sinus Bradycardia Etiology: SA node is depolarizing slower than normal, impulse is conducted normally (i.e. normal
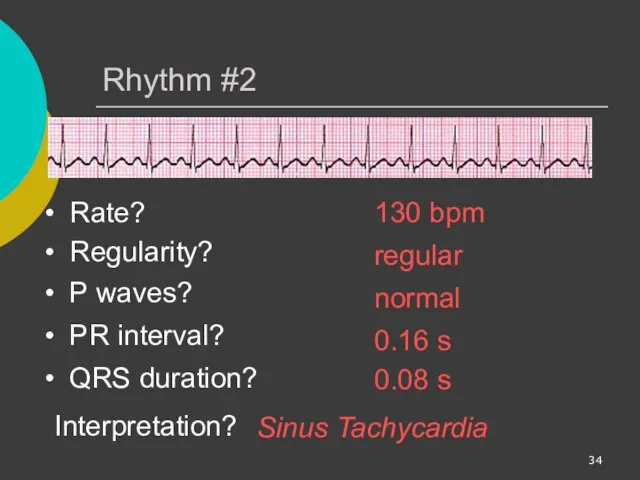
- 34. Rhythm #2 130 bpm Rate? Regularity? regular normal 0.08 s P waves? PR interval? 0.16 s
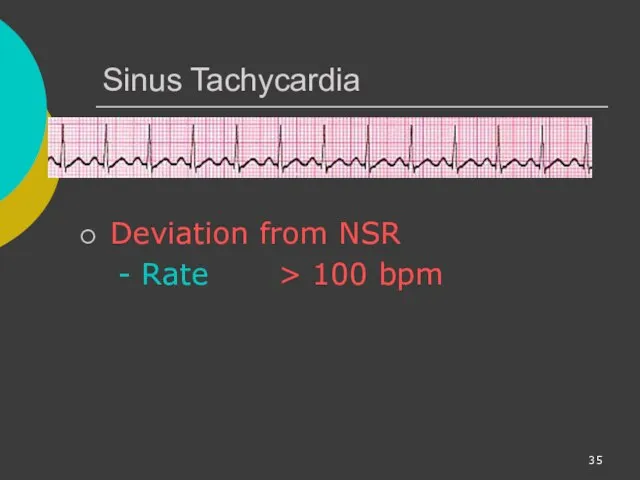
- 35. Sinus Tachycardia Deviation from NSR - Rate > 100 bpm
- 36. Sinus Tachycardia Etiology: SA node is depolarizing faster than normal, impulse is conducted normally. Remember: sinus
- 37. Sinus Arrest Etiology: SA node fails to depolarize and no compensatory mechanisms take over Sinus arrest
- 38. Premature Beats Premature Atrial Contractions (PACs) Premature Ventricular Contractions (PVCs)
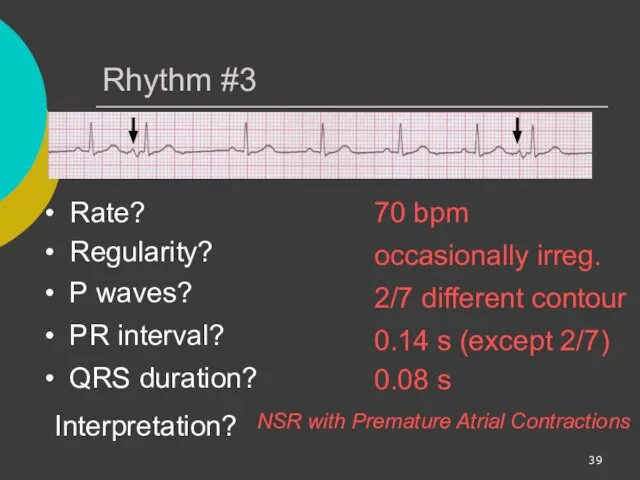
- 39. Rhythm #3 70 bpm Rate? Regularity? occasionally irreg. 2/7 different contour 0.08 s P waves? PR
- 40. Premature Atrial Contractions Deviation from NSR These ectopic beats originate in the atria (but not in
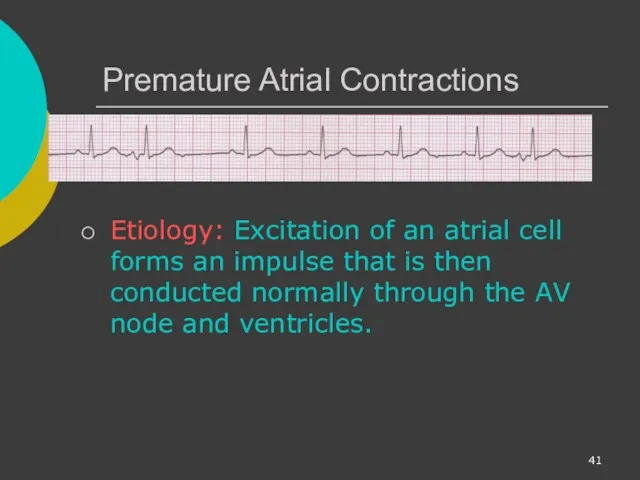
- 41. Premature Atrial Contractions Etiology: Excitation of an atrial cell forms an impulse that is then conducted
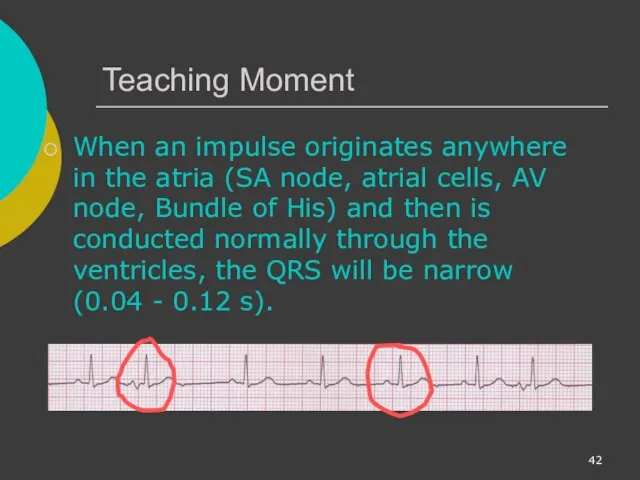
- 42. Teaching Moment When an impulse originates anywhere in the atria (SA node, atrial cells, AV node,
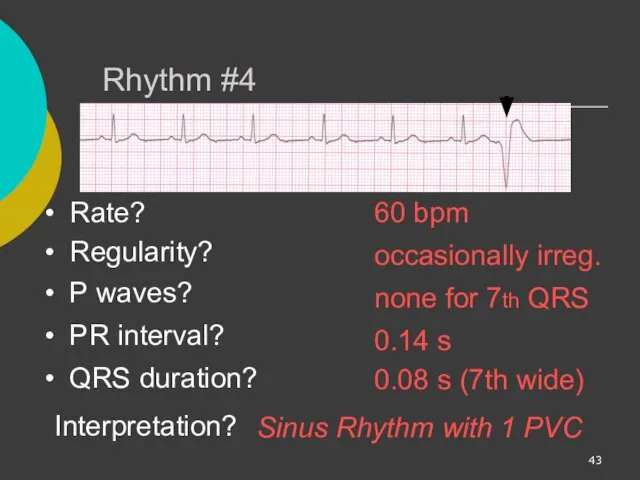
- 43. Rhythm #4 60 bpm Rate? Regularity? occasionally irreg. none for 7th QRS 0.08 s (7th wide)
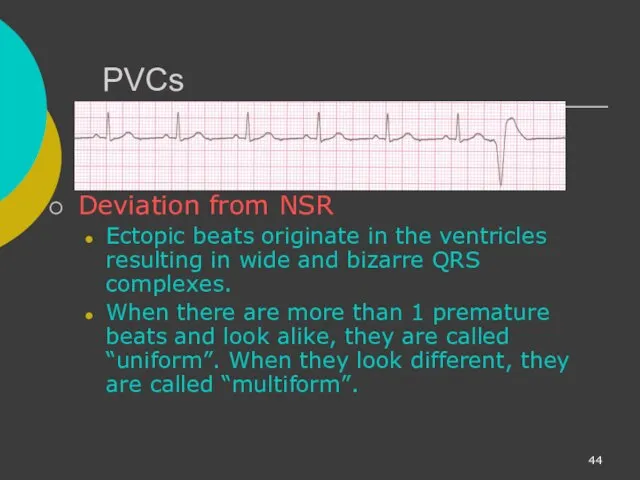
- 44. PVCs Deviation from NSR Ectopic beats originate in the ventricles resulting in wide and bizarre QRS
- 45. PVCs Etiology: One or more ventricular cells are depolarizing and the impulses are abnormally conducting through
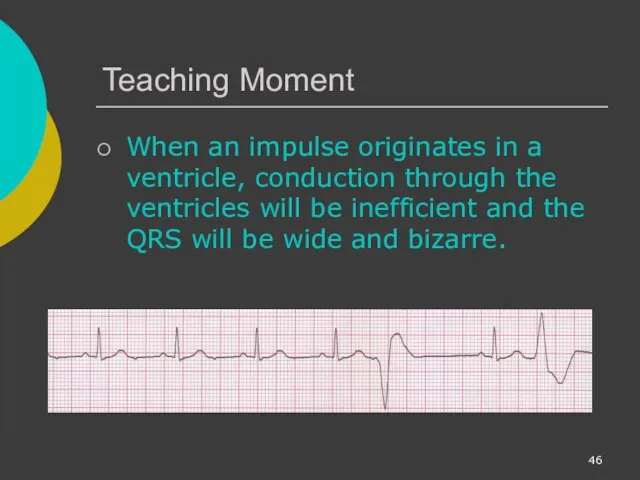
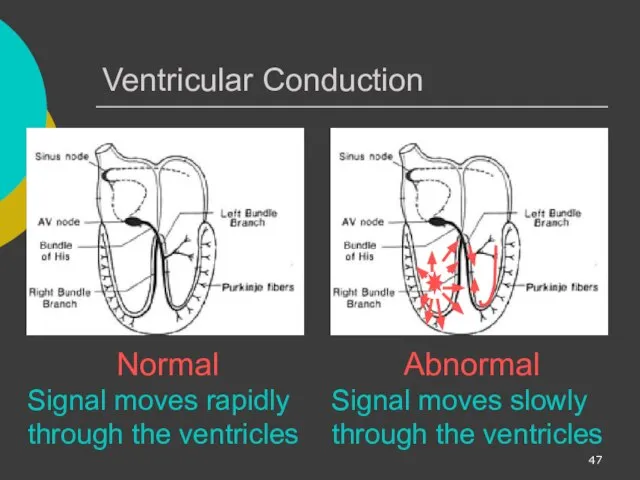
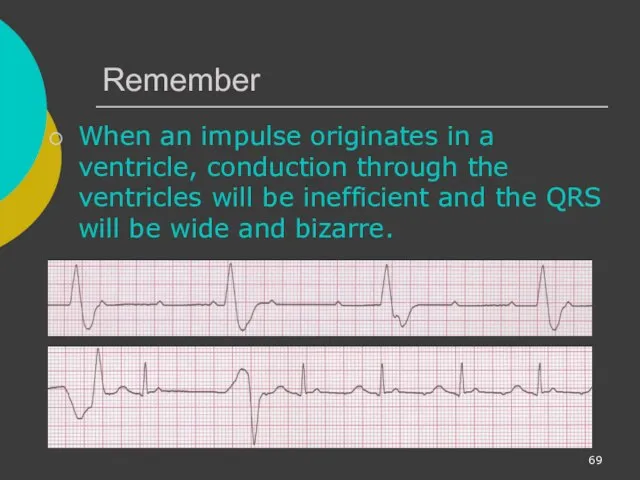
- 46. Teaching Moment When an impulse originates in a ventricle, conduction through the ventricles will be inefficient
- 47. Ventricular Conduction Normal Signal moves rapidly through the ventricles Abnormal Signal moves slowly through the ventricles
- 48. Supraventricular Arrhythmias Atrial Fibrillation Atrial Flutter Paroxysmal Supra Ventricular Tachycardia (PSVT)
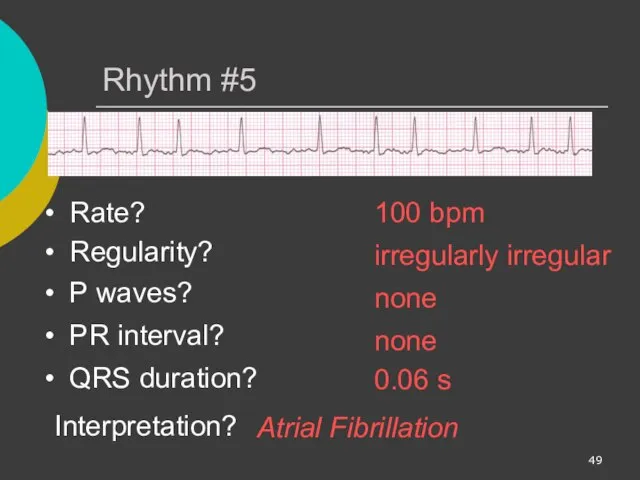
- 49. Rhythm #5 100 bpm Rate? Regularity? irregularly irregular none 0.06 s P waves? PR interval? none
- 50. Atrial Fibrillation Deviation from NSR No organized atrial depolarization, so no normal P waves (impulses are
- 51. Atrial Fibrillation Etiology: due to multiple re-entrant wavelets conducted between the R & L atria and
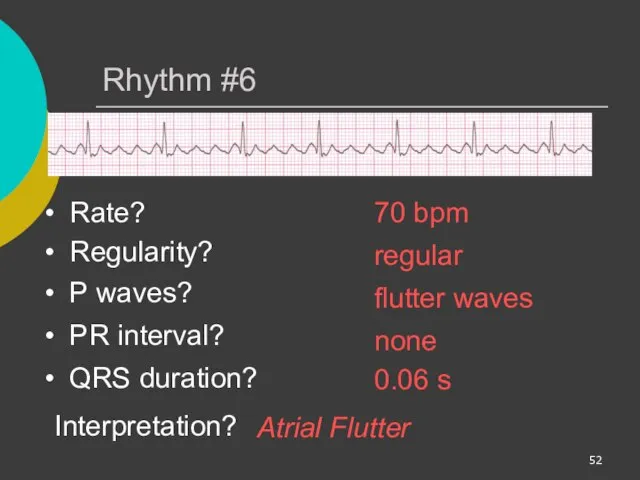
- 52. Rhythm #6 70 bpm Rate? Regularity? regular flutter waves 0.06 s P waves? PR interval? none
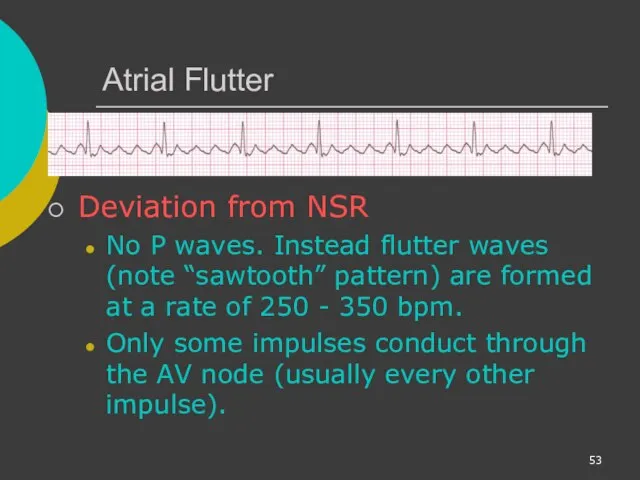
- 53. Atrial Flutter Deviation from NSR No P waves. Instead flutter waves (note “sawtooth” pattern) are formed
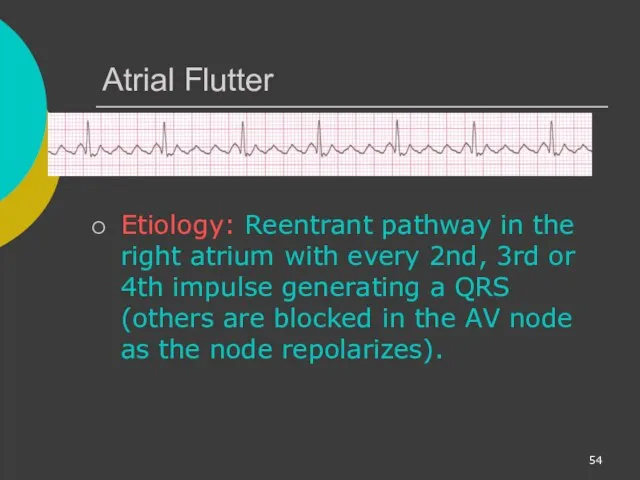
- 54. Atrial Flutter Etiology: Reentrant pathway in the right atrium with every 2nd, 3rd or 4th impulse
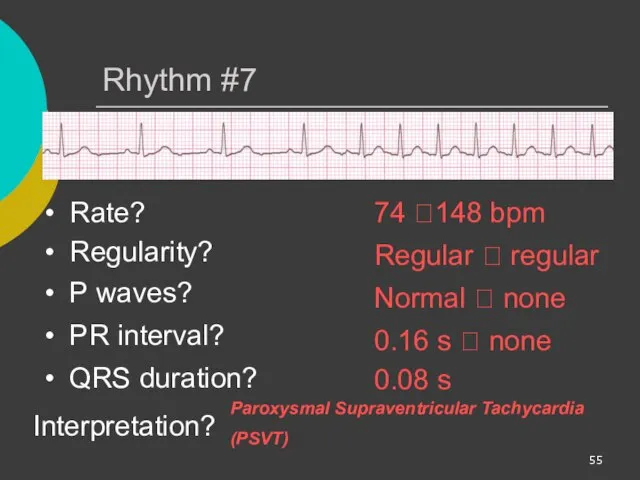
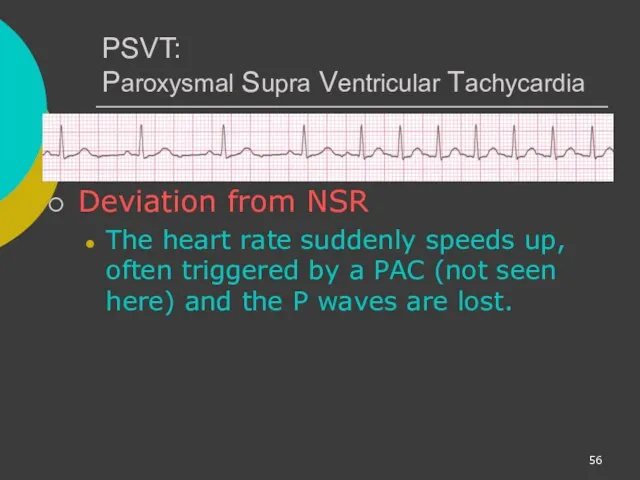
- 55. Rhythm #7 74 ?148 bpm Rate? Regularity? Regular ? regular Normal ? none 0.08 s P
- 56. PSVT: Paroxysmal Supra Ventricular Tachycardia Deviation from NSR The heart rate suddenly speeds up, often triggered
- 57. AV Nodal Blocks 1st Degree AV Block 2nd Degree AV Block, Type I 2nd Degree AV
- 58. Rhythm #10 60 bpm Rate? Regularity? regular normal 0.08 s P waves? PR interval? 0.36 s
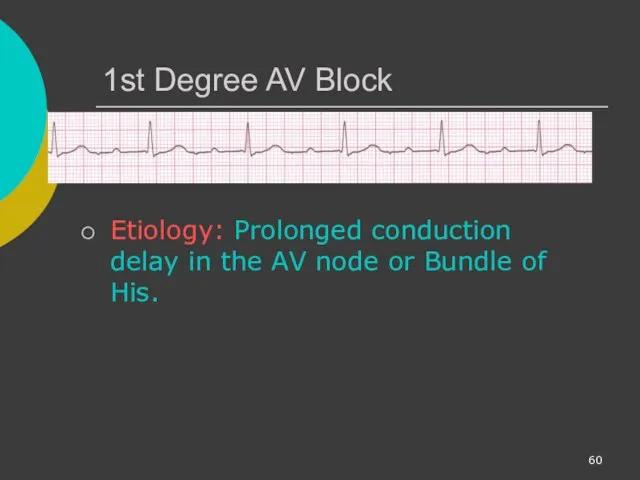
- 59. 1st Degree AV Block Deviation from NSR PR Interval > 0.20 s
- 60. 1st Degree AV Block Etiology: Prolonged conduction delay in the AV node or Bundle of His.
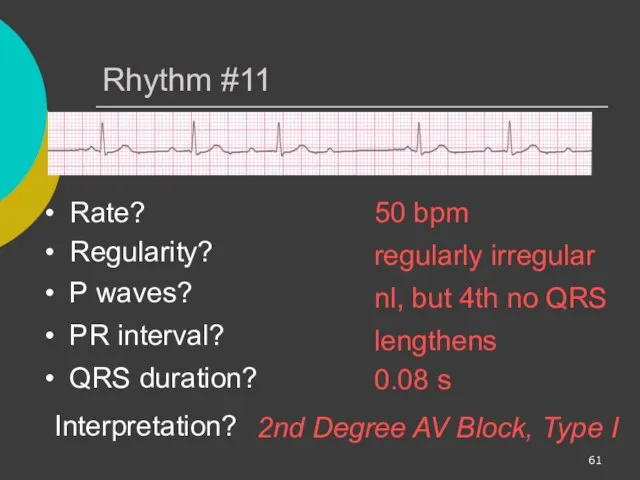
- 61. Rhythm #11 50 bpm Rate? Regularity? regularly irregular nl, but 4th no QRS 0.08 s P
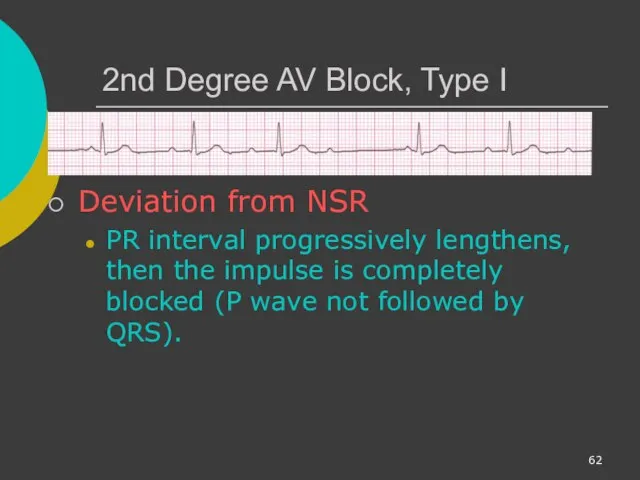
- 62. 2nd Degree AV Block, Type I Deviation from NSR PR interval progressively lengthens, then the impulse
- 63. 2nd Degree AV Block, Type I Etiology: Each successive atrial impulse encounters a longer and longer
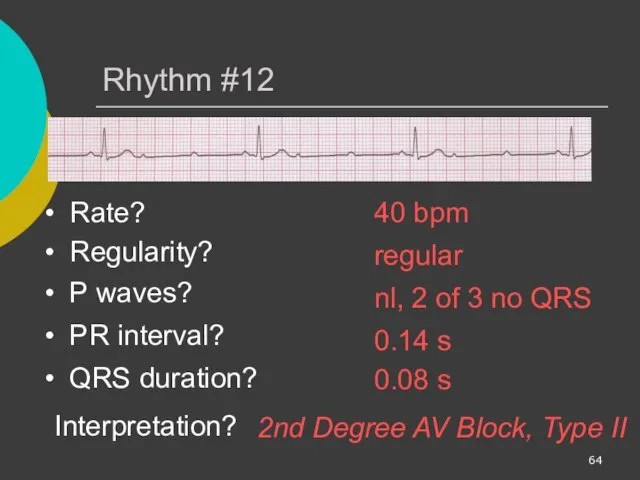
- 64. Rhythm #12 40 bpm Rate? Regularity? regular nl, 2 of 3 no QRS 0.08 s P
- 65. 2nd Degree AV Block, Type II Deviation from NSR Occasional P waves are completely blocked (P
- 66. Rhythm #13 40 bpm Rate? Regularity? regular no relation to QRS wide (> 0.12 s) P
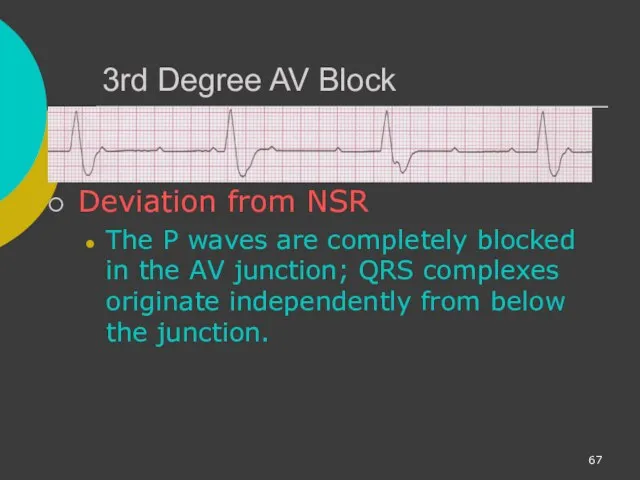
- 67. 3rd Degree AV Block Deviation from NSR The P waves are completely blocked in the AV
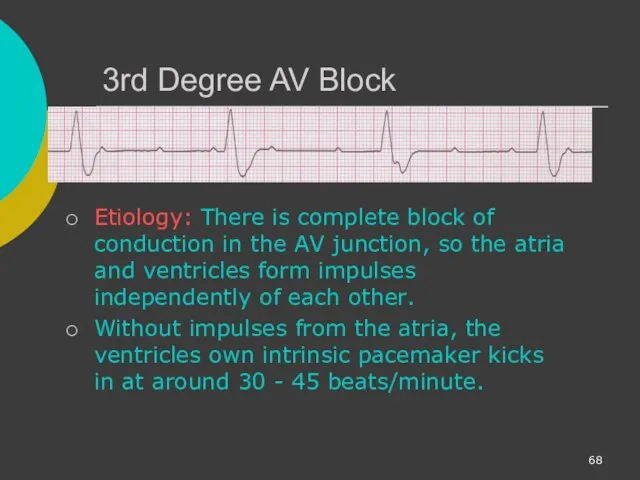
- 68. 3rd Degree AV Block Etiology: There is complete block of conduction in the AV junction, so
- 69. Remember When an impulse originates in a ventricle, conduction through the ventricles will be inefficient and
- 70. Ventricular Fibrillation Rhythm: irregular-coarse or fine, wave form varies in size and shape Fires continuously from
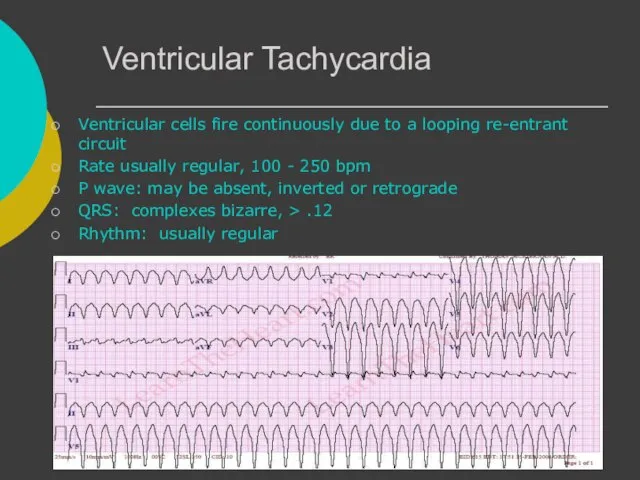
- 71. Ventricular Tachycardia Ventricular cells fire continuously due to a looping re-entrant circuit Rate usually regular, 100
- 72. Asystole Ventricular standstill, no electrical activity, no cardiac output – no pulse! Cardiac arrest, may follow
- 73. IdioVentricular Rhythm Escape rhythm (safety mechanism) to prevent ventricular standstill HIS/purkinje system takes over as the
- 74. Diagnosing a MI To diagnose a myocardial infarction you need to go beyond looking at a
- 75. The 12-Lead ECG The 12-Lead ECG sees the heart from 12 different views. Therefore, the 12-Lead
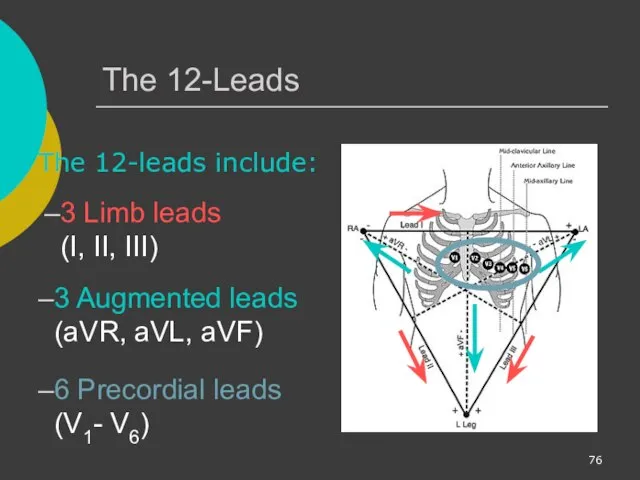
- 76. The 12-Leads The 12-leads include: 3 Limb leads (I, II, III) 3 Augmented leads (aVR, aVL,
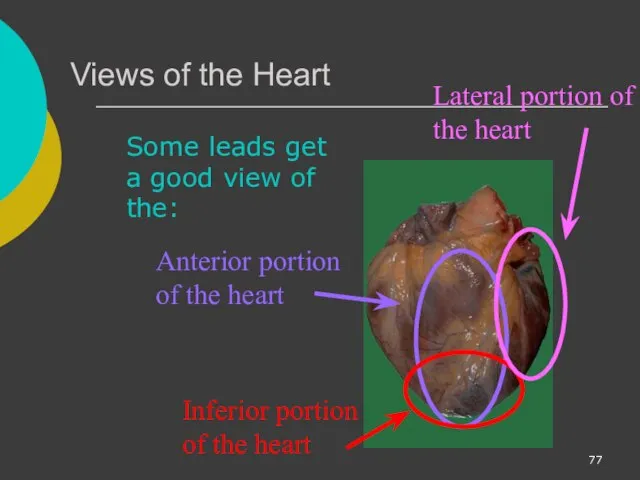
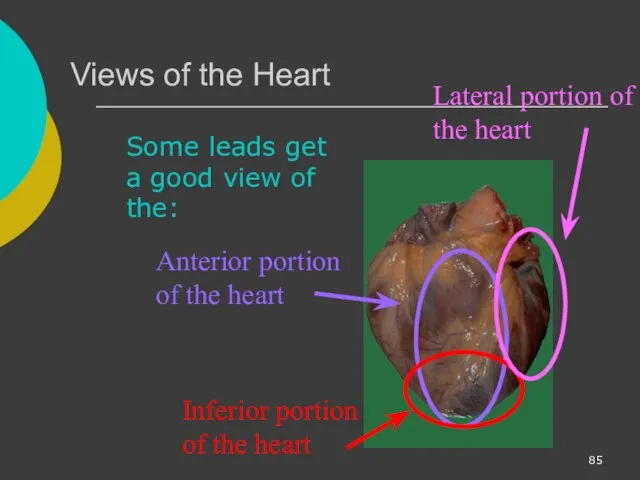
- 77. Views of the Heart Some leads get a good view of the: Anterior portion of the
- 78. ST Elevation One way to diagnose an acute MI is to look for elevation of the
- 79. ST Elevation (cont) Elevation of the ST segment (greater than 1 small box) in 2 leads
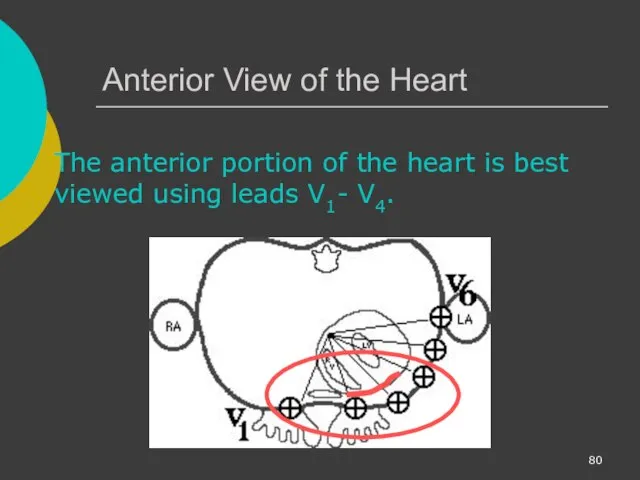
- 80. Anterior View of the Heart The anterior portion of the heart is best viewed using leads
- 81. Anterior Myocardial Infarction If you see changes in leads V1 - V4 that are consistent with
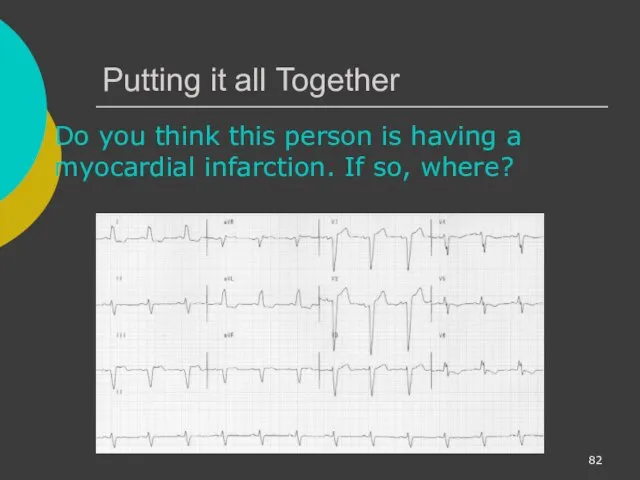
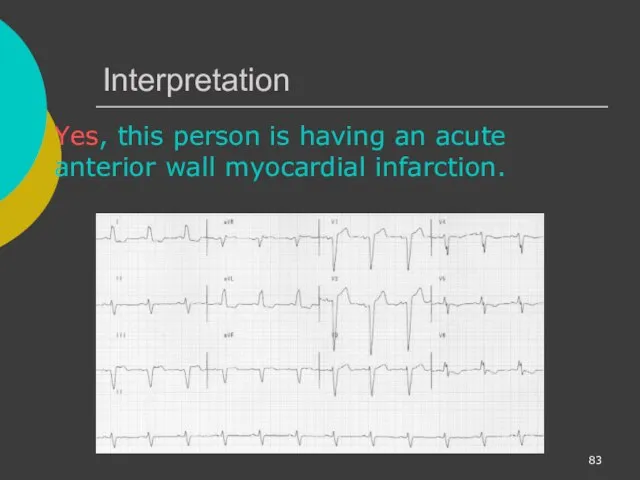
- 82. Putting it all Together Do you think this person is having a myocardial infarction. If so,
- 83. Interpretation Yes, this person is having an acute anterior wall myocardial infarction.
- 84. Other MI Locations Now that you know where to look for an anterior wall myocardial infarction
- 85. Views of the Heart Some leads get a good view of the: Anterior portion of the
- 86. Other MI Locations Second, remember that the 12-leads of the ECG look at different portions of
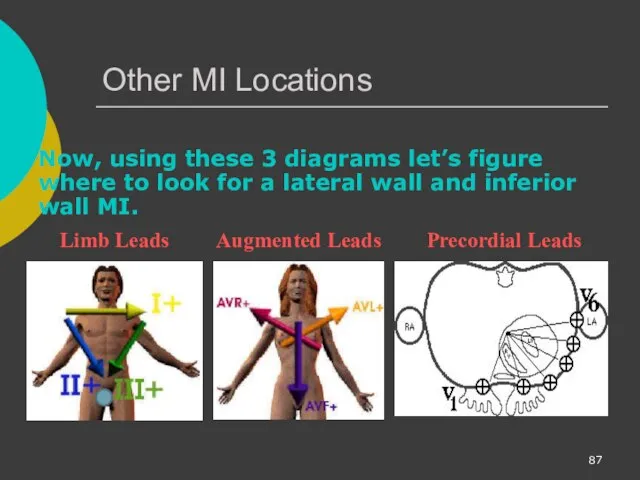
- 87. Other MI Locations Now, using these 3 diagrams let’s figure where to look for a lateral
- 88. Anterior MI Remember the anterior portion of the heart is best viewed using leads V1- V4.
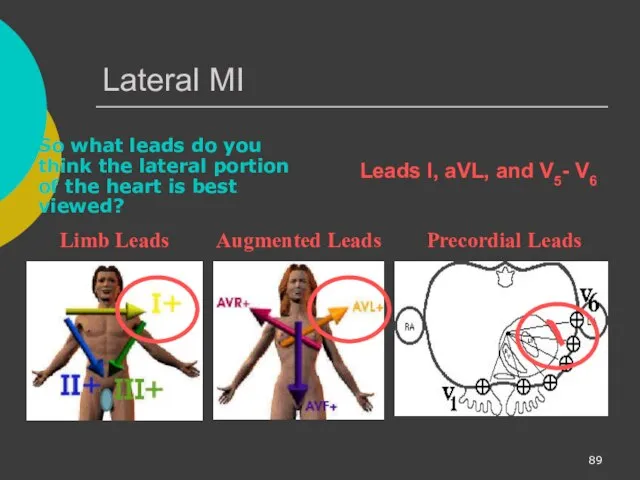
- 89. Lateral MI So what leads do you think the lateral portion of the heart is best
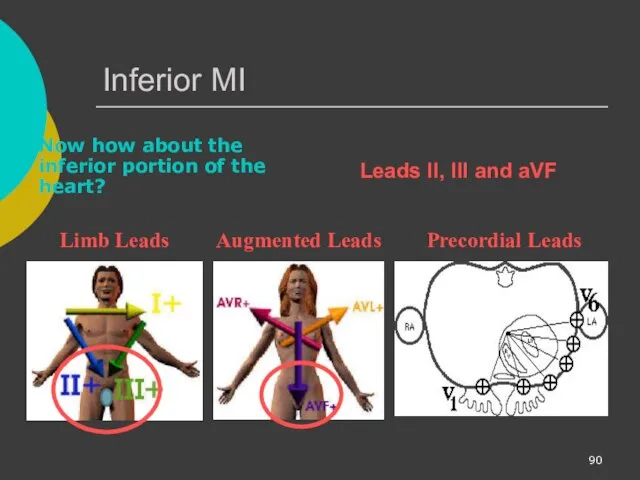
- 90. Inferior MI Now how about the inferior portion of the heart? Limb Leads Augmented Leads Precordial
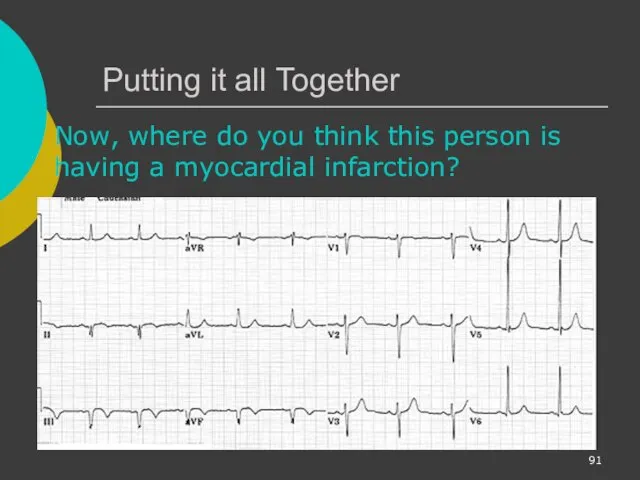
- 91. Putting it all Together Now, where do you think this person is having a myocardial infarction?
- 92. Inferior Wall MI This is an inferior MI. Note the ST elevation in leads II, III
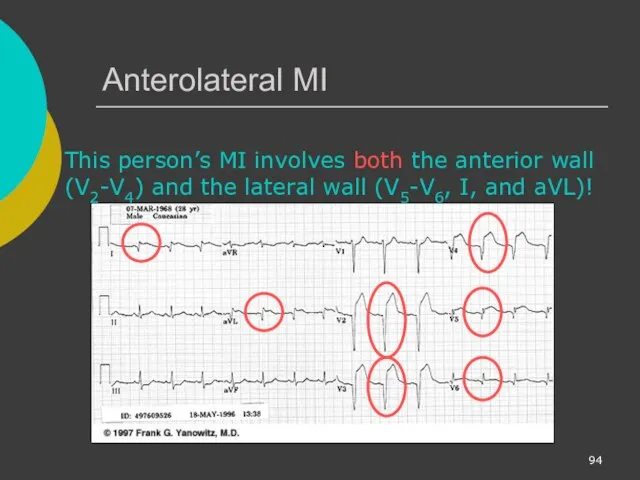
- 93. Putting it all Together How about now?
- 94. Anterolateral MI This person’s MI involves both the anterior wall (V2-V4) and the lateral wall (V5-V6,
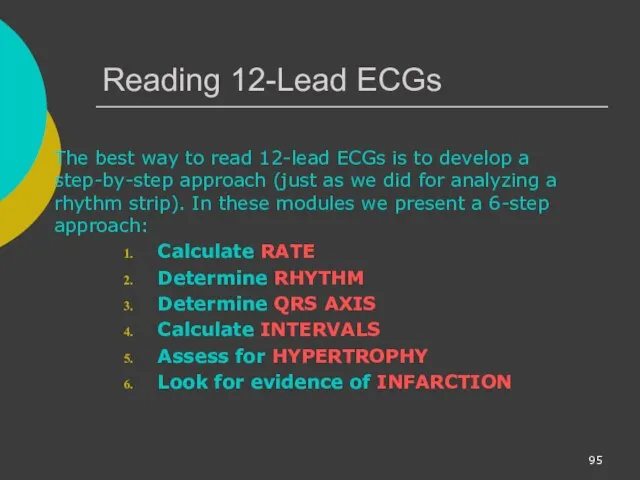
- 95. Reading 12-Lead ECGs The best way to read 12-lead ECGs is to develop a step-by-step approach
- 96. Rate Rhythm Axis Intervals Hypertrophy Infarct In Module II you learned how to calculate the rate.
- 98. Скачать презентацию



































 Опухоли. Строение опухолей
Опухоли. Строение опухолей Колоректальный рак
Колоректальный рак Органы нервной системы. Спинной и головной мозг. Рефлекторные дуги. Гистология
Органы нервной системы. Спинной и головной мозг. Рефлекторные дуги. Гистология Визначення типу складності випадку та особливості його ведення, залежно від наявних ризиків
Визначення типу складності випадку та особливості його ведення, залежно від наявних ризиків Типы старения кожи лица
Типы старения кожи лица Лимфоаденопатии
Лимфоаденопатии Важные этапы РОФ
Важные этапы РОФ Сравнительная характеристика селективного ИДС по IgA и транзиторного ИДС
Сравнительная характеристика селективного ИДС по IgA и транзиторного ИДС Принципы и концепция доказательной медицины. Лекция 1
Принципы и концепция доказательной медицины. Лекция 1 Лекция №22. Общие вопросы хирургической инфекции
Лекция №22. Общие вопросы хирургической инфекции Paediatric Anaesthesia
Paediatric Anaesthesia Лечение периодонтитов молочных зубов
Лечение периодонтитов молочных зубов Қоғамдық денсаулық сақтау мамандығы бойынша
Қоғамдық денсаулық сақтау мамандығы бойынша Алкоголизм и его последствия для здоровья
Алкоголизм и его последствия для здоровья ЛФК при заболеваниях, травмах и повреждениях опорно-двигательного аппарата и нервной системы. (Лекция 3)
ЛФК при заболеваниях, травмах и повреждениях опорно-двигательного аппарата и нервной системы. (Лекция 3) Факторы риска атеросклероза
Факторы риска атеросклероза Синдром Кавасаки
Синдром Кавасаки Качество медицинской помощи и его обеспечение
Качество медицинской помощи и его обеспечение Понятие дезинфекции
Понятие дезинфекции Рентгенография
Рентгенография Артикуляторы, окклюдаторы. Изготовление восковых базисов
Артикуляторы, окклюдаторы. Изготовление восковых базисов Лечение артериальной гипертензии
Лечение артериальной гипертензии Основы клинической онкологии
Основы клинической онкологии Помощь в коррекции речевой функции заикающихся детей в школьном возрасте
Помощь в коррекции речевой функции заикающихся детей в школьном возрасте Телефон доверия. Технологии оказания экстренной психологической помощи
Телефон доверия. Технологии оказания экстренной психологической помощи Острое инфекционное заболевание - дифтерия
Острое инфекционное заболевание - дифтерия Ботулизм - тағамдық токсикоздың ауыр түріне жатады
Ботулизм - тағамдық токсикоздың ауыр түріне жатады Шок. Классификация, диагностика, лечение
Шок. Классификация, диагностика, лечение