Содержание
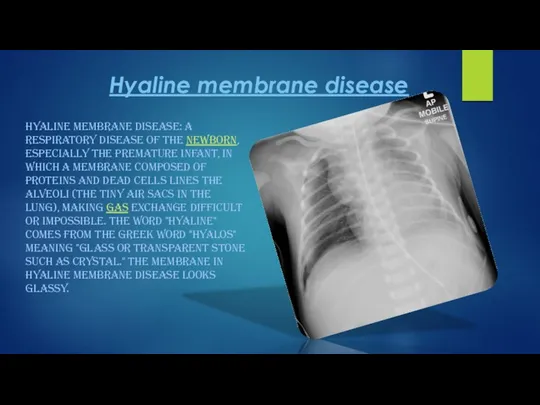
- 2. Hyaline membrane disease HYALINE MEMBRANE DISEASE: A RESPIRATORY DISEASE OF THE NEWBORN, ESPECIALLY THE PREMATURE INFANT,
- 3. Hyaline membrane disease is now commonly called respiratory distress syndrome (RDS). It is caused by a
- 4. The preterm newborn is further handicapped because his or her ribs are more easily deformed (compliant).
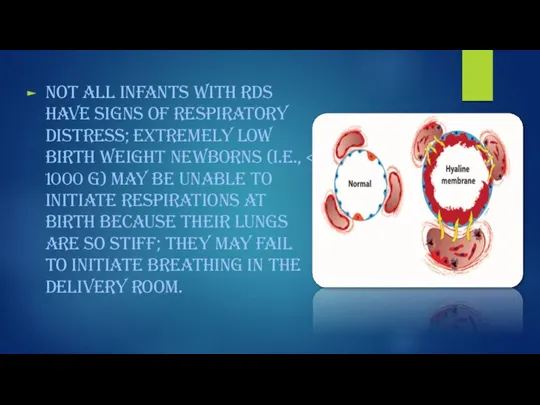
- 5. Not all infants with RDS have signs of respiratory distress; extremely low birth weight newborns (i.e.,
- 6. The incidence of RDS can be reduced by assessment of fetal lung maturity to determine the
- 7. If untreated, severe RDS can result in multiple organ failure and death. However, if the newborn's
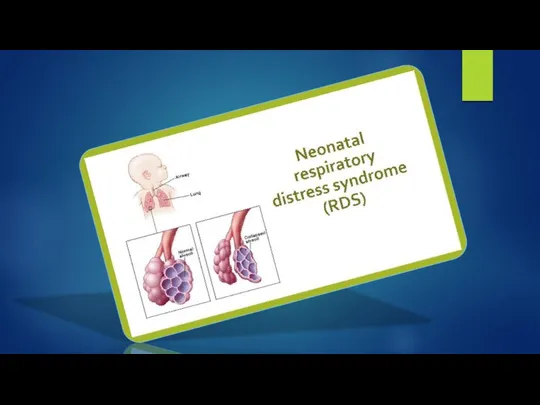
- 9. Newborn respiratory distress syndrome Newborn respiratory distress syndrome (NRDS) happens when a baby's lungs are not
- 12. Symptoms of NRDS THE SYMPTOMS OF NRDS ARE OFTEN NOTICEABLE IMMEDIATELY AFTER BIRTH AND GET WORSE
- 13. Diagnosing NRDS A number of tests can be used to diagnose NRDS and rule out other
- 14. For better understanding HTTPS://WWW.YOUTUBE.COM/WATCH?V=KED0EVBKJF8 HTTPS://WWW.YOUTUBE.COM/WATCH?V=XWE7XWH7O1Y HTTPS://WWW.YOUTUBE.COM/WATCH?V=R5-PEJFQ6WK
- 16. Скачать презентацию


 Требования к постели тяжелобольного пациента. Организация постели
Требования к постели тяжелобольного пациента. Организация постели Стадирование эндометриоза
Стадирование эндометриоза Фонокардиограф. Технические характеристики
Фонокардиограф. Технические характеристики Ведение больных с внебольничным абортом
Ведение больных с внебольничным абортом Антибиотиктер. Алкалоидтар. Гормондар
Антибиотиктер. Алкалоидтар. Гормондар Медицинская демография
Медицинская демография Нарушения кровообращения при тяжелой внебольничной пневмонии, осложненной ОРДС
Нарушения кровообращения при тяжелой внебольничной пневмонии, осложненной ОРДС Медицинский центр Арника
Медицинский центр Арника Профилактика коронавируса средствами природы
Профилактика коронавируса средствами природы Основные аспекты кардиохирургии
Основные аспекты кардиохирургии Антибиотики. Нежелательные эффекты химиотерапии
Антибиотики. Нежелательные эффекты химиотерапии Энергетическая капсула Витамакс
Энергетическая капсула Витамакс Публичное обсуждение результатов мониторинга наркоситуации в ХМАО – Югре за 2018 год
Публичное обсуждение результатов мониторинга наркоситуации в ХМАО – Югре за 2018 год Острый панкреатит
Острый панкреатит Клиникалық диагнозды негiздеу
Клиникалық диагнозды негiздеу Клинико-фармакологические аспекты в пульмонологии
Клинико-фармакологические аспекты в пульмонологии Темперамент и характер человека
Темперамент и характер человека Патогенные стафилококки
Патогенные стафилококки Бионика. Статистика
Бионика. Статистика Алгоритм диагностики и неотложной помощи при судорожном синдроме у детей
Алгоритм диагностики и неотложной помощи при судорожном синдроме у детей GCP стандарт. Инновационный результат
GCP стандарт. Инновационный результат Азбука здорового питания
Азбука здорового питания Современные методы диагностики и лечения эндокринной офтальмопатии
Современные методы диагностики и лечения эндокринной офтальмопатии Дәрігермен науқас арасындағы қарым-қатынас түрлерін қолдану
Дәрігермен науқас арасындағы қарым-қатынас түрлерін қолдану Кафедра мобилизационной подготовки здравоохранения и медицины катастроф
Кафедра мобилизационной подготовки здравоохранения и медицины катастроф Гепатит. Лабараторлы инструментальді диагностикасы
Гепатит. Лабараторлы инструментальді диагностикасы Александера болезнь
Александера болезнь Сознание. Бессознание
Сознание. Бессознание