Содержание
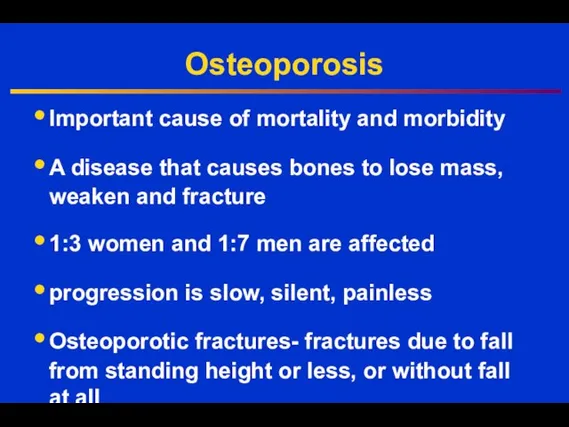
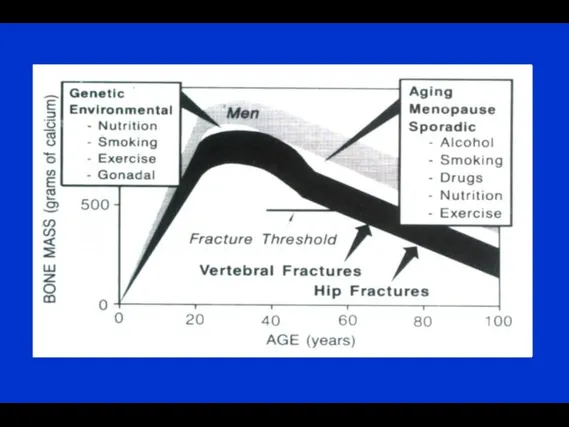
- 3. Osteoporosis Important cause of mortality and morbidity A disease that causes bones to lose mass, weaken
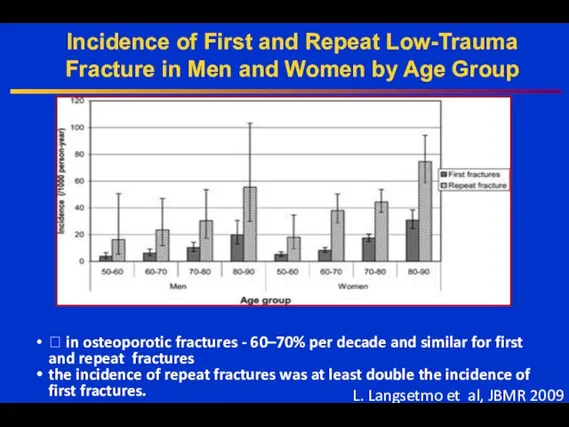
- 4. Incidence of First and Repeat Low-Trauma Fracture in Men and Women by Age Group ? in
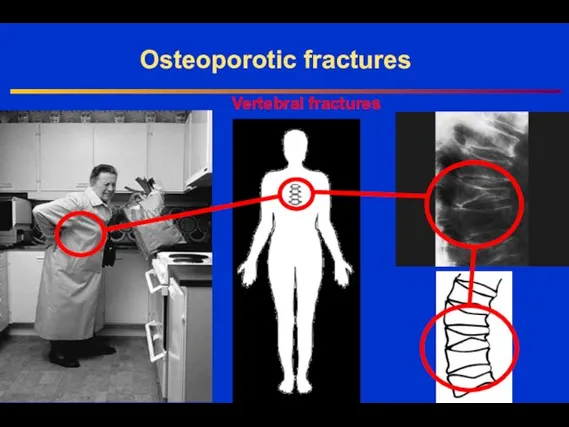
- 5. Vertebral fractures Osteoporotic fractures
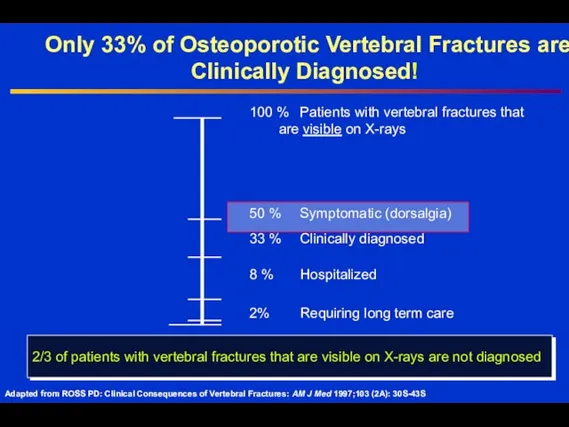
- 6. 100 % Patients with vertebral fractures that are visible on X-rays 50 % Symptomatic (dorsalgia) 33
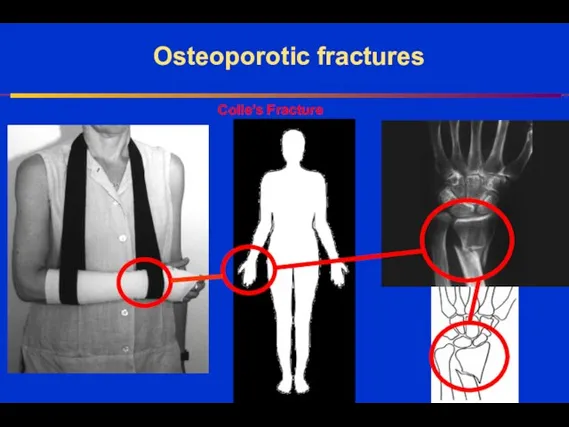
- 7. Osteoporotic fractures Colle’s Fracture
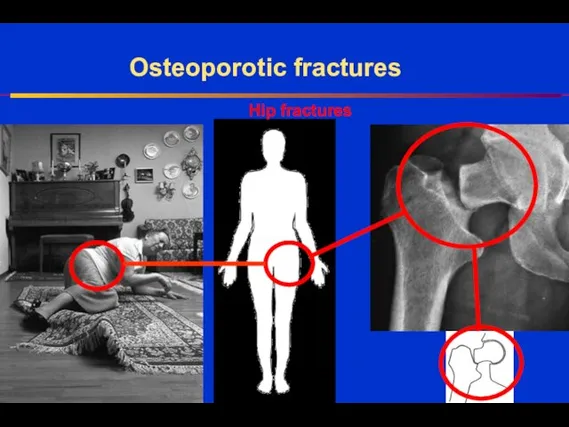
- 8. Hip fractures Osteoporotic fractures
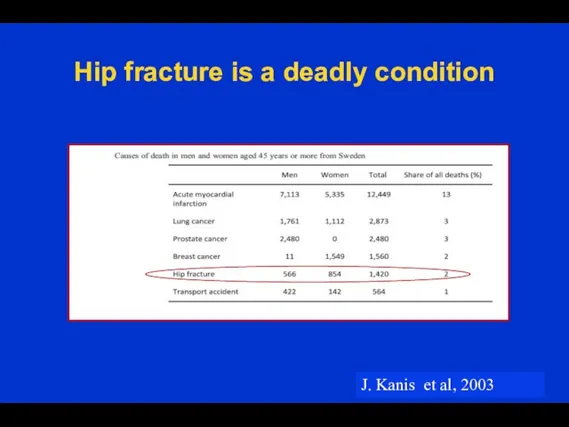
- 9. Hip fracture is a deadly condition J. Kanis et al, 2003
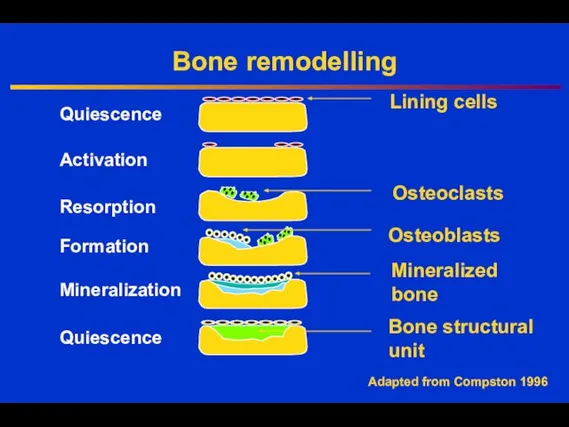
- 10. Bone remodelling Quiescence Activation Resorption Formation Quiescence Osteoclasts Osteoblasts Lining cells Mineralized bone Mineralization Bone structural
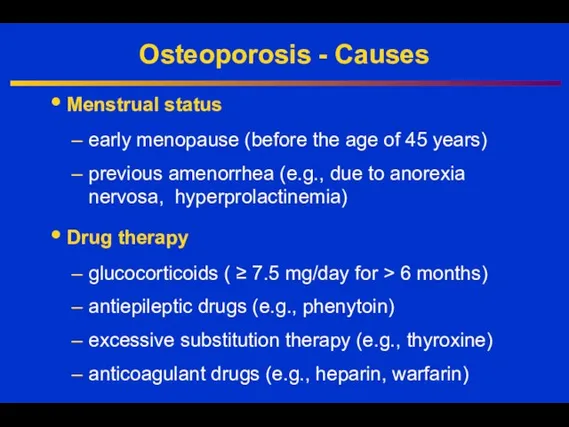
- 12. Osteoporosis - Causes Menstrual status early menopause (before the age of 45 years) previous amenorrhea (e.g.,
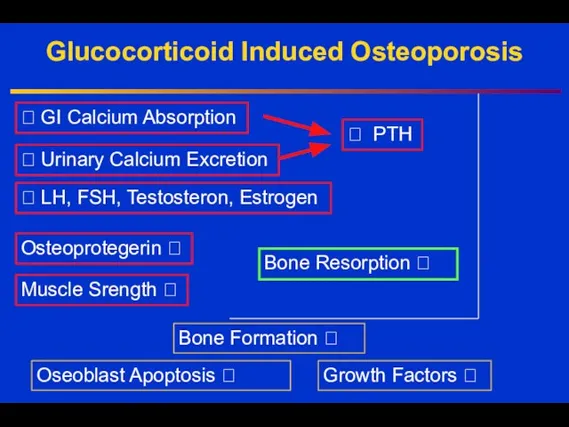
- 13. Glucocorticoid Induced Osteoporosis ? GI Calcium Absorption ? Urinary Calcium Excretion ? LH, FSH, Testosteron, Estrogen
- 14. Osteoporosis - Causes Endocrine disease primary hyperparathryroidism thyrotoxicosis Cushing’s syndrome Rheumatologic diseases rheumatoid arthritis ankylosing spondylitis
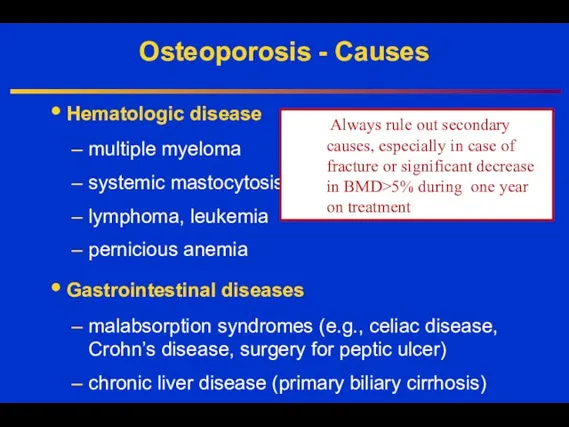
- 15. Osteoporosis - Causes Hematologic disease multiple myeloma systemic mastocytosis lymphoma, leukemia pernicious anemia Gastrointestinal diseases malabsorption
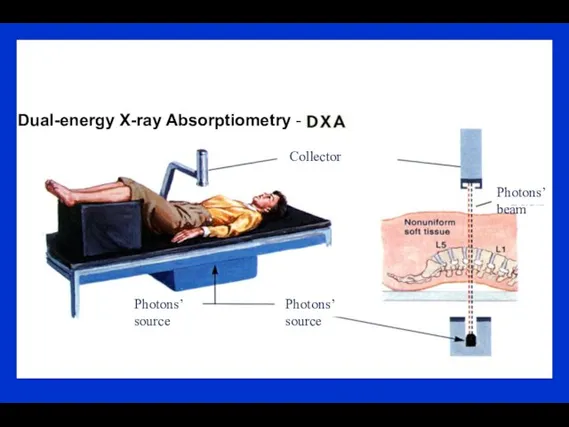
- 16. Dual-energy X-ray Absorptiometry - Photons’ source Photons’ source Photons’ beam Collector
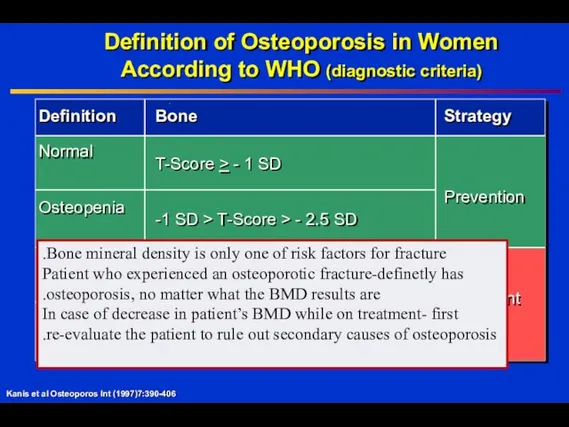
- 17. Definition of Osteoporosis in Women According to WHO (diagnostic criteria) Kanis et al Osteoporos Int (1997)7:390-406
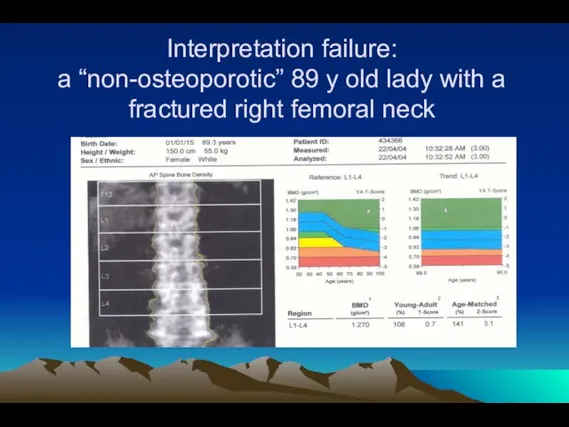
- 18. Interpretation failure: a “non-osteoporotic” 89 y old lady with a fractured right femoral neck
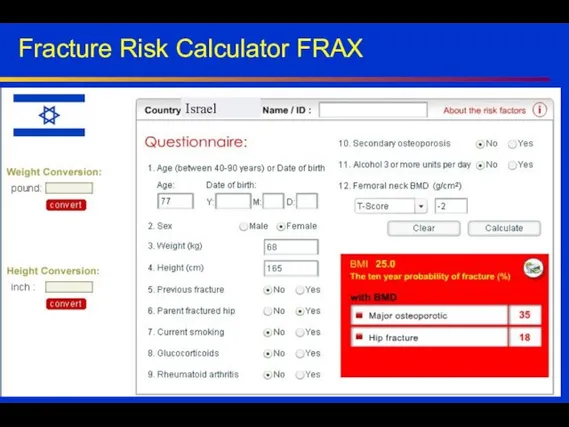
- 19. Fracture Risk Calculator FRAX Israel
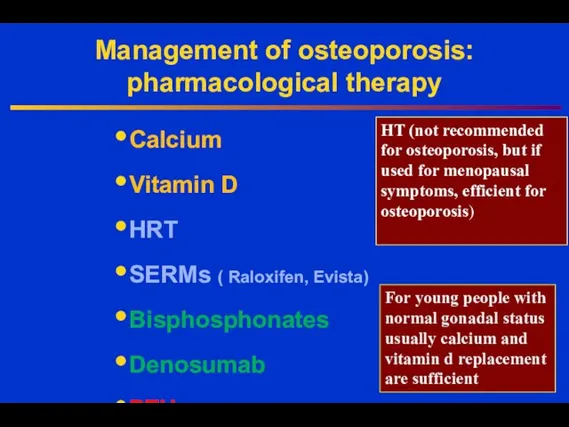
- 20. Management of osteoporosis: pharmacological therapy Calcium Vitamin D HRT SERMs ( Raloxifen, Evista) Bisphosphonates Denosumab PTH
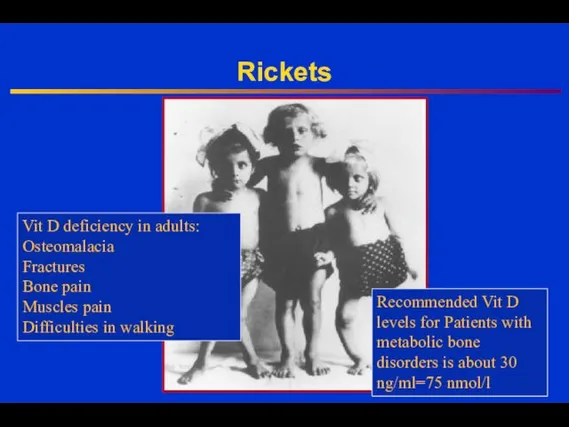
- 21. Rickets Vit D deficiency in adults: Osteomalacia Fractures Bone pain Muscles pain Difficulties in walking Recommended
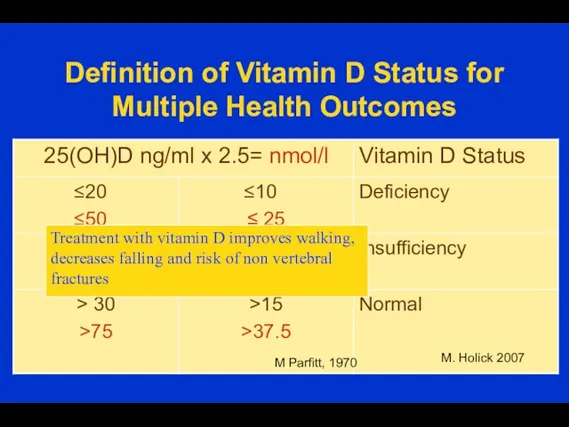
- 23. Definition of Vitamin D Status for Multiple Health Outcomes M. Holick 2007 M Parfitt, 1970 Treatment
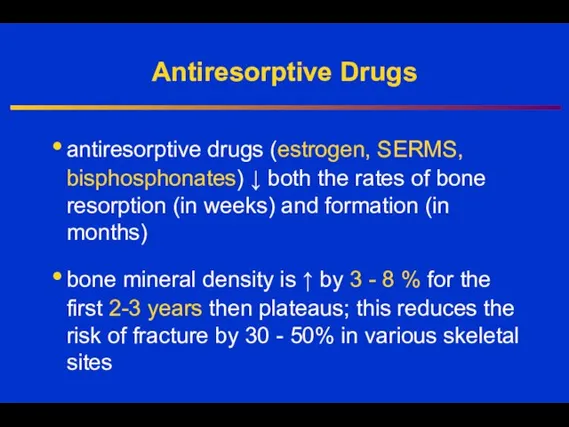
- 24. Antiresorptive Drugs antiresorptive drugs (estrogen, SERMS, bisphosphonates) ↓ both the rates of bone resorption (in weeks)
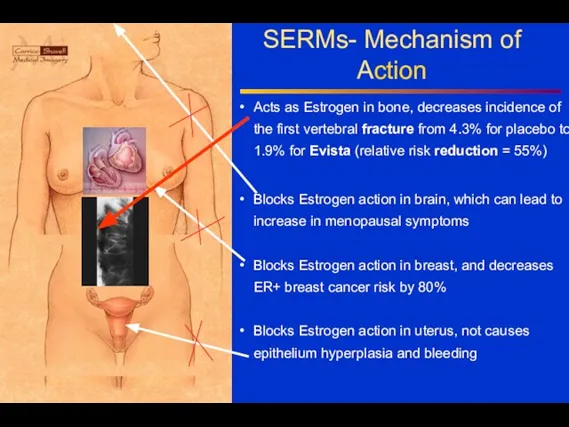
- 25. SERMs- Mechanism of Action Acts as Estrogen in bone, decreases incidence of the first vertebral fracture
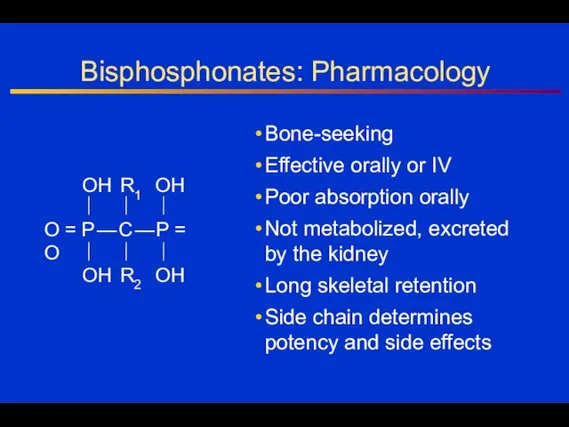
- 26. Bisphosphonates: Pharmacology Bone-seeking Effective orally or IV Poor absorption orally Not metabolized, excreted by the kidney
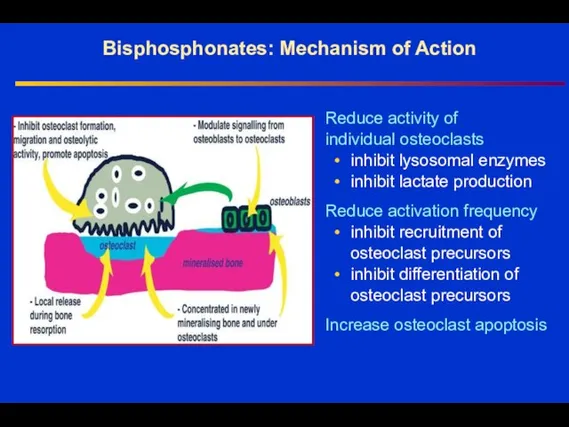
- 27. Bisphosphonates: Mechanism of Action Reduce activity of individual osteoclasts • inhibit lysosomal enzymes • inhibit lactate
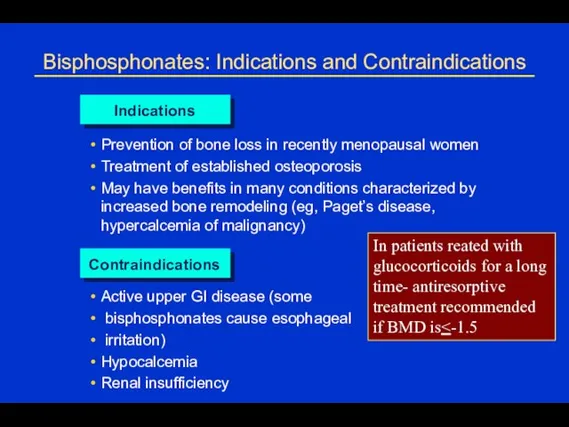
- 28. Bisphosphonates: Indications and Contraindications Indications Prevention of bone loss in recently menopausal women Treatment of established
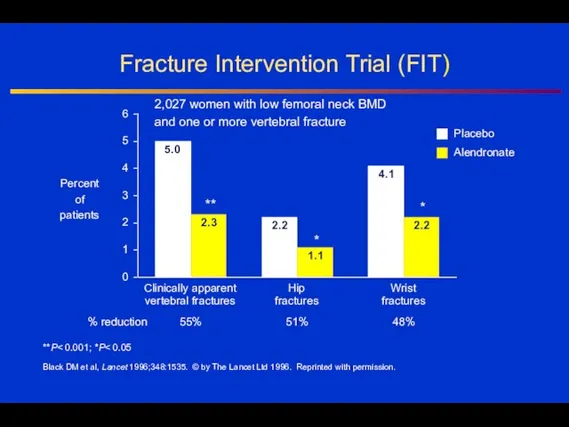
- 29. Fracture Intervention Trial (FIT) **P Black DM et al, Lancet 1996;348:1535. © by The Lancet Ltd
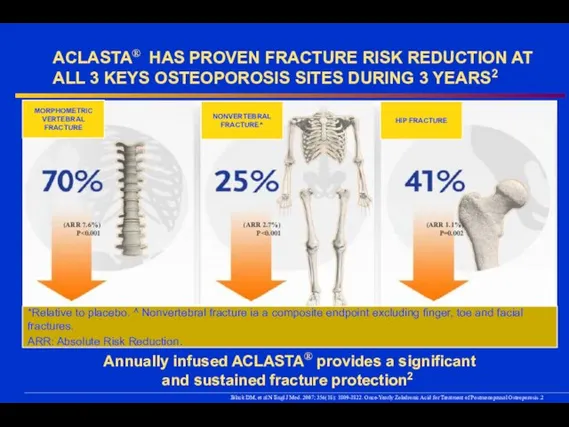
- 30. ACLASTA® HAS PROVEN FRACTURE RISK REDUCTION AT ALL 3 KEYS OSTEOPOROSIS SITES DURING 3 YEARS2 2.
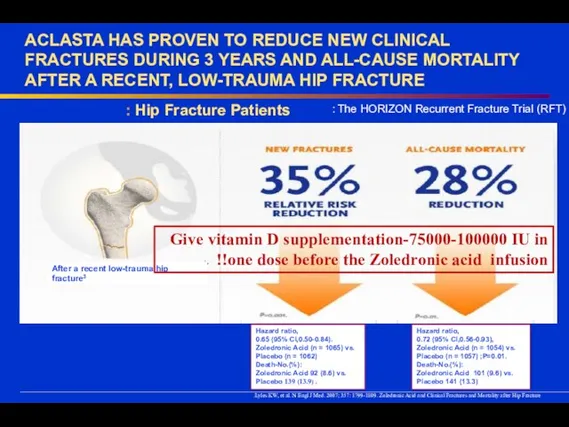
- 31. ACLASTA HAS PROVEN TO REDUCE NEW CLINICAL FRACTURES DURING 3 YEARS AND ALL-CAUSE MORTALITY AFTER A
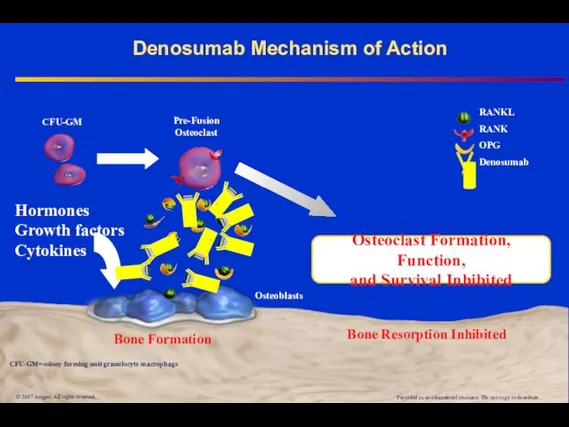
- 32. Denosumab Mechanism of Action © 2007 Amgen. All rights reserved. RANKL RANK OPG Denosumab Bone Formation
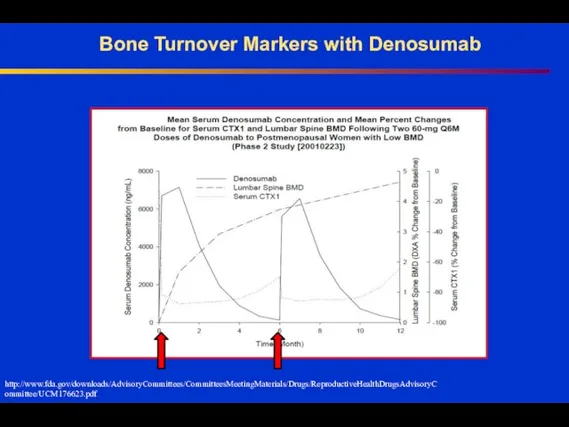
- 33. Bone Turnover Markers with Denosumab http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ReproductiveHealthDrugsAdvisoryCommittee/UCM176623.pdf
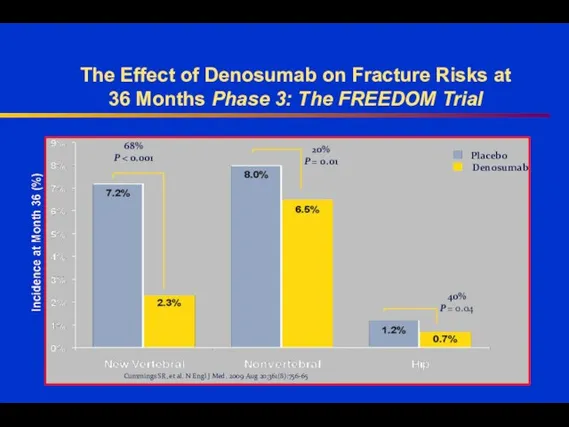
- 34. The Effect of Denosumab on Fracture Risks at 36 Months Phase 3: The FREEDOM Trial Cummings
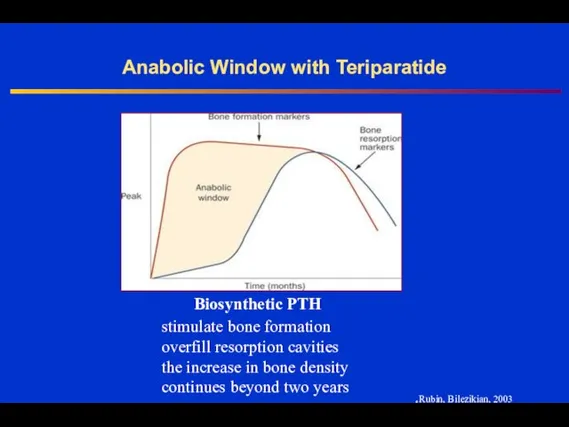
- 35. Anabolic Window with Teriparatide Rubin, Bilezikian, 2003. stimulate bone formation overfill resorption cavities the increase in
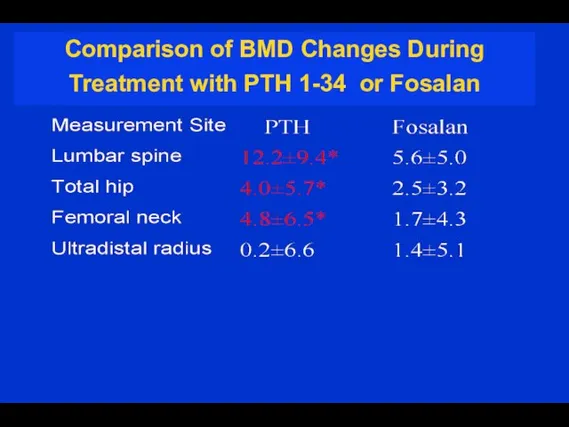
- 36. Comparison of BMD Changes During Treatment with PTH 1-34 or Fosalan
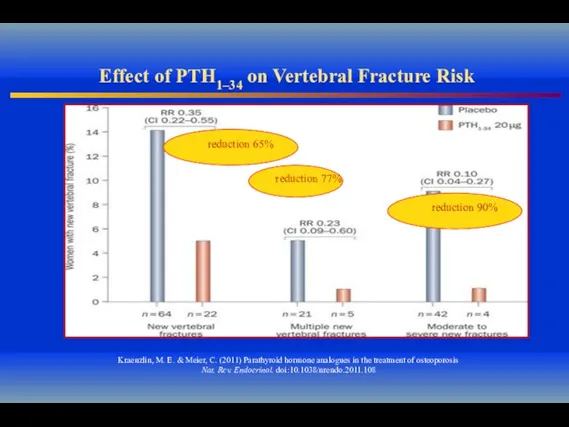
- 37. Effect of PTH1–34 on Vertebral Fracture Risk Kraenzlin, M. E. & Meier, C. (2011) Parathyroid hormone
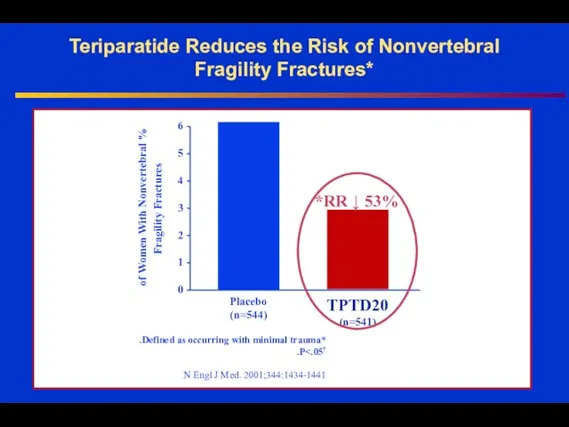
- 38. Teriparatide Reduces the Risk of Nonvertebral Fragility Fractures* Placebo (n=544) TPTD20 (n=541) % of Women With
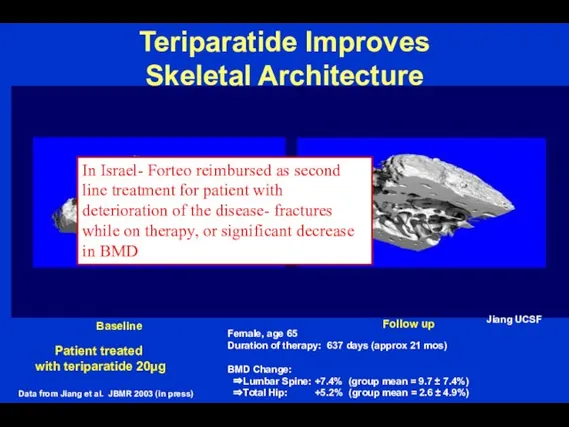
- 39. Teriparatide Improves Skeletal Architecture Patient treated with teriparatide 20µg Female, age 65 Duration of therapy: 637
- 41. Скачать презентацию


 Психосоматичні розлади: поняття та класифікація
Психосоматичні розлади: поняття та класифікація Осложнения после удаления зуба
Осложнения после удаления зуба Клиническая картина сагиттальных отклонений прикуса
Клиническая картина сагиттальных отклонений прикуса Врожденная непроходимость желудочно-кишечного тракта
Врожденная непроходимость желудочно-кишечного тракта Назначение целевого и результативного компонентов системы психолого-педагогического сопровождения
Назначение целевого и результативного компонентов системы психолого-педагогического сопровождения Многоплодная беременность
Многоплодная беременность Гигиена кожи
Гигиена кожи Методы обследования слезных органов
Методы обследования слезных органов Тыныс жетіспеушілігінің диагностикасы және емі
Тыныс жетіспеушілігінің диагностикасы және емі Аллергодерматозы
Аллергодерматозы Рентген диагностика заболеваний молочной железы
Рентген диагностика заболеваний молочной железы Доступ к материалам по методикам лечения переломов Surgery Reference на AO сайте
Доступ к материалам по методикам лечения переломов Surgery Reference на AO сайте Вирус СПИДа
Вирус СПИДа Гайморит у детей
Гайморит у детей Норма и патология речи. Речевое поведение. Эмоциональность, скорость и громкость речи
Норма и патология речи. Речевое поведение. Эмоциональность, скорость и громкость речи Адгезия. Условия адгезии. Стандартизация стоматологических материалов
Адгезия. Условия адгезии. Стандартизация стоматологических материалов Технологии развития произвольности внимания в подростковом и взрослом возрасте
Технологии развития произвольности внимания в подростковом и взрослом возрасте Витамин D
Витамин D Фенотипическая классификация первичных иммунодефицитов
Фенотипическая классификация первичных иммунодефицитов Талмажәне талма кезінде алғашқы көмек
Талмажәне талма кезінде алғашқы көмек Послеоперационное обезболивание
Послеоперационное обезболивание Интерлейкины. Перспективы биотехнологического производства и практическое применение
Интерлейкины. Перспективы биотехнологического производства и практическое применение АЧС. Медецина
АЧС. Медецина Рентгенологиялық және эндоскопиялық зерттеу әдістері
Рентгенологиялық және эндоскопиялық зерттеу әдістері Цитомегаловирусты, герпестік, хламидиялық инфекция және жүктілік
Цитомегаловирусты, герпестік, хламидиялық инфекция және жүктілік Биологические вредные и опасные производственные факторы. Классификация заболеваний, вызываемых БОиВПФ
Биологические вредные и опасные производственные факторы. Классификация заболеваний, вызываемых БОиВПФ Профилактика синдрома профессионального выгорания
Профилактика синдрома профессионального выгорания Генитальный герпес
Генитальный герпес