Содержание
- 2. Other Psychotic Disorders Brief Psychotic Disorder Schizophreniform Disorder Schizoaffective Disorder Delusional Disorder Shared Psychotic Disorder Axis
- 3. Brief Psychotic Disorder Diagnostic Criteria: Presence of 1 or more of the following: Delusions Hallucinations Disorganized
- 4. Brief Psychotic Disorder Per definition- always full recovery! Good prognosis- 50-80% never develop any psychiatric disease.
- 5. Specifiers for Brief Psychotic Disorder With Marked Stressors= brief reactive psychosis Without Marked Stressors With Postpartum
- 6. Epidemiology Rare. Prevalence unknown. Most patients- young (20-30y), women, from developing countries Personality disorders Low SES
- 7. Clinical Presentation Typically- extreme emotional lability, bizzarre behavior, either screaming or complete mutism, severe impairment of
- 8. Good Prognostic Indicators No prodrome, acute onset Good premorbid level of functioning Few schizoid personality traits
- 9. DDX דליריום (במקום הראשAny substance (intoxication, withdrawal, secondary psychosis) Any other general medical condition Schizophreniform Delusional
- 10. Treatment Hospitalization Antipsychotics- usually good and fast response Psychotherapy to deal with the potential trigger and
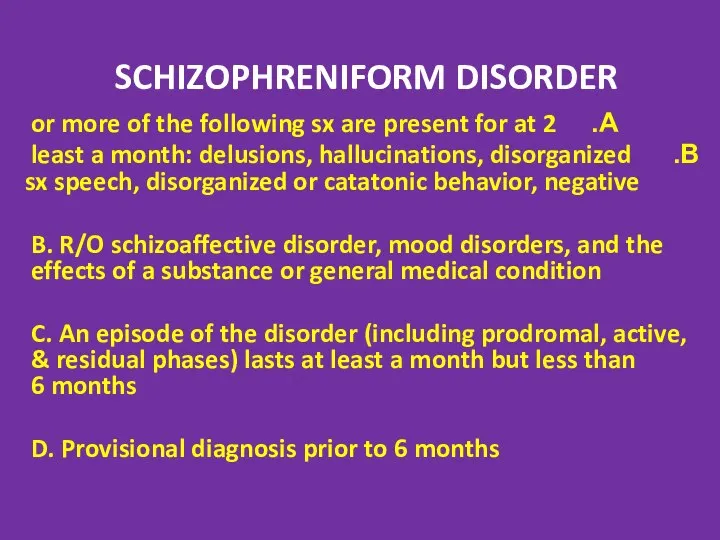
- 11. SCHIZOPHRENIFORM DISORDER 2 or more of the following sx are present for at least a month:
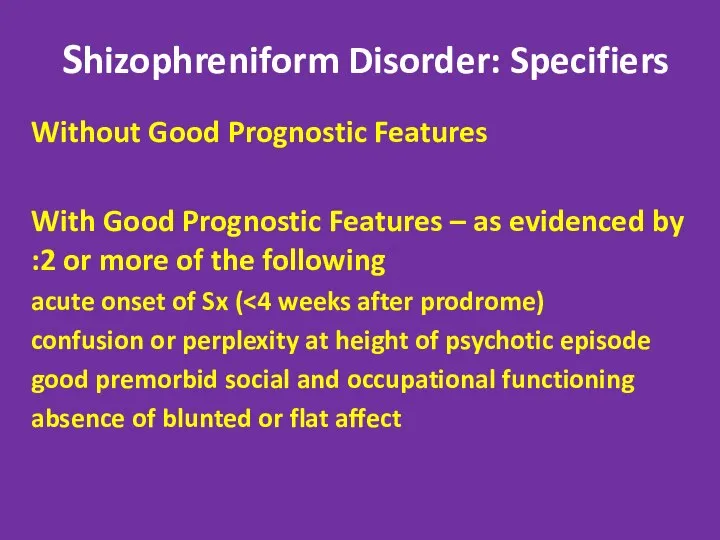
- 12. Shizophreniform Disorder: Specifiers Without Good Prognostic Features With Good Prognostic Features – as evidenced by 2
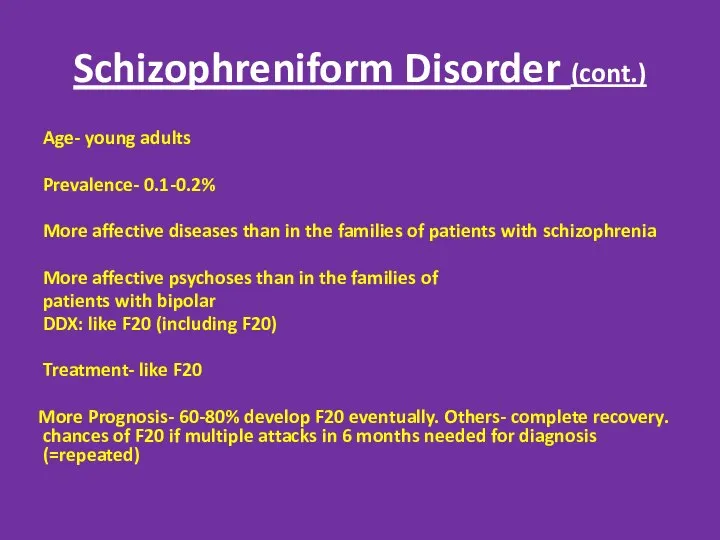
- 13. Schizophreniform Disorder (cont.) Age- young adults Prevalence- 0.1-0.2% More affective diseases than in the families of
- 14. Treatment 3-6 months of neuroleptics. React faster and better than F20 ECT in patients with affective
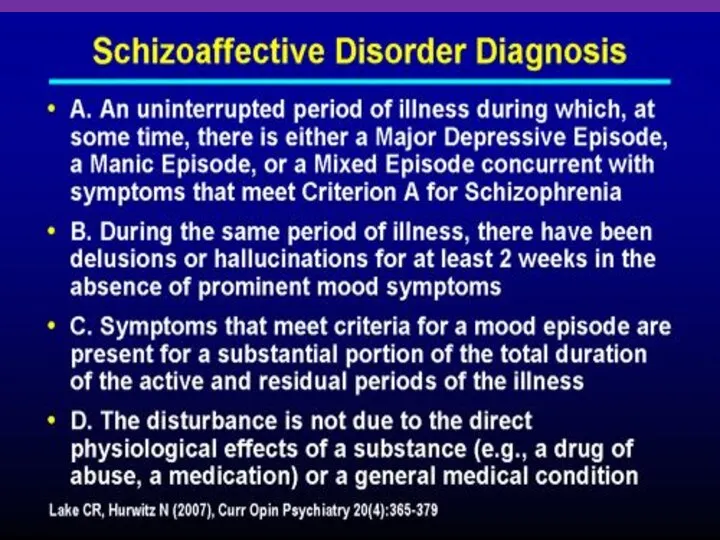
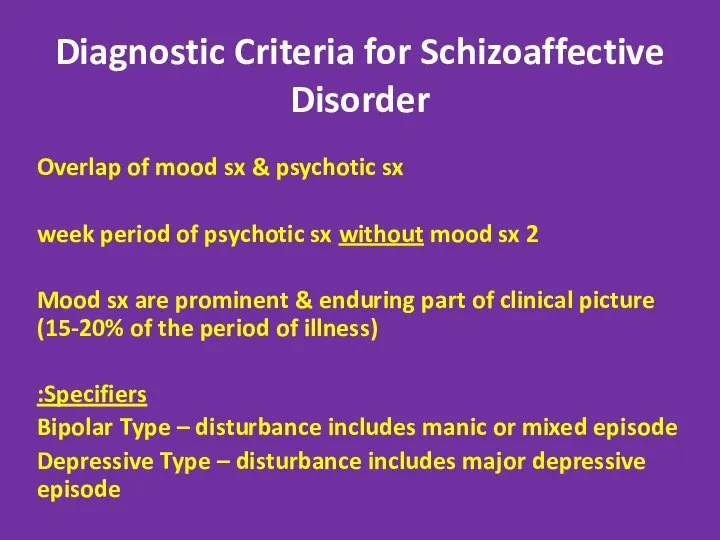
- 16. Diagnostic Criteria for Schizoaffective Disorder Overlap of mood sx & psychotic sx 2 week period of
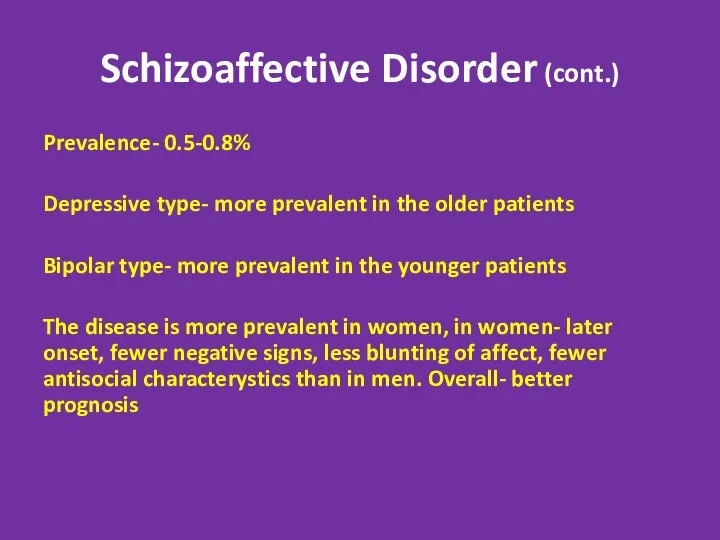
- 17. Schizoaffective Disorder (cont.) Prevalence- 0.5-0.8% Depressive type- more prevalent in the older patients Bipolar type- more
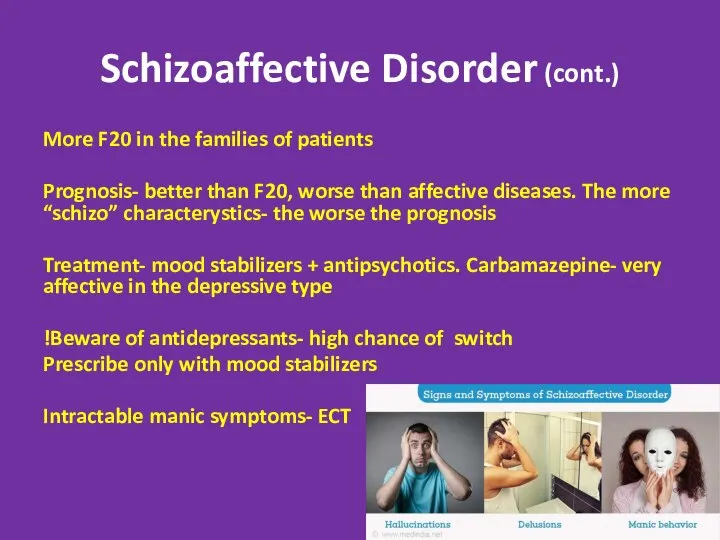
- 18. Schizoaffective Disorder (cont.) More F20 in the families of patients Prognosis- better than F20, worse than
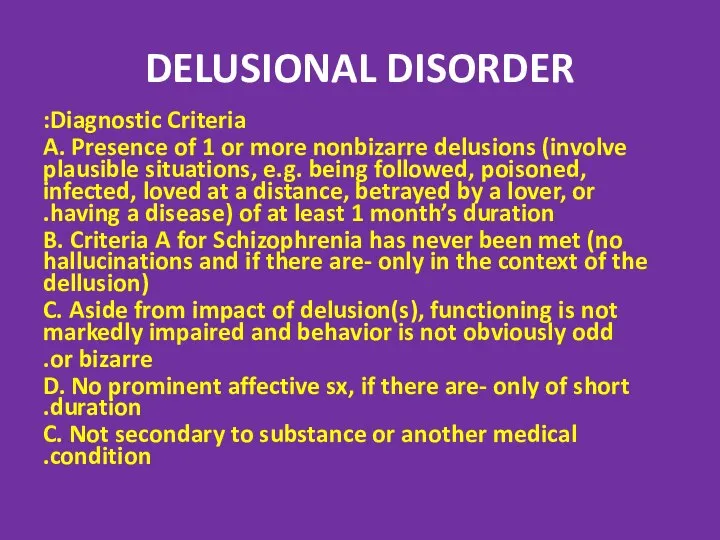
- 19. DELUSIONAL DISORDER Diagnostic Criteria: A. Presence of 1 or more nonbizarre delusions (involve plausible situations, e.g.
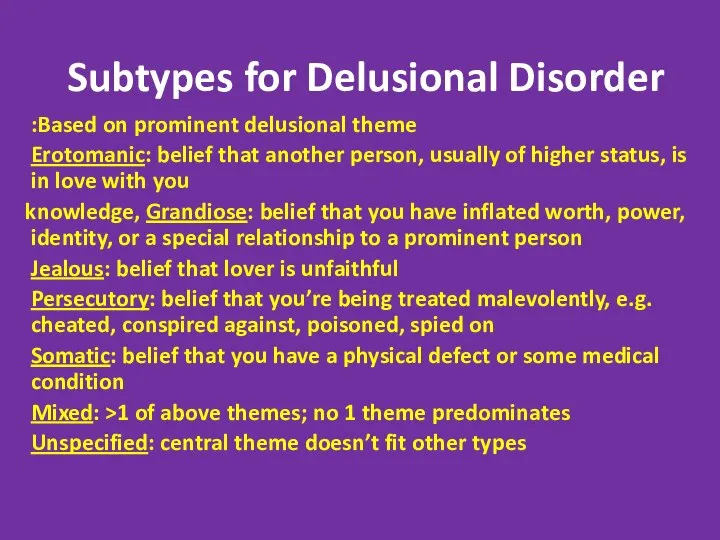
- 20. Subtypes for Delusional Disorder Based on prominent delusional theme: Erotomanic: belief that another person, usually of
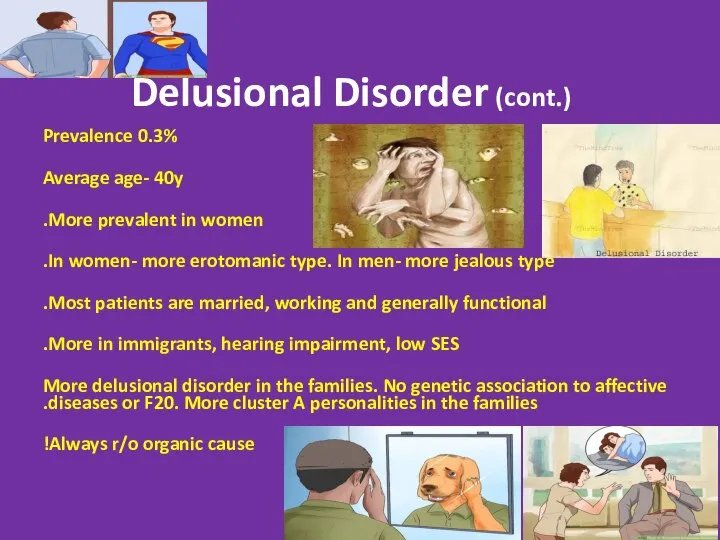
- 21. Delusional Disorder (cont.) Prevalence 0.3% Average age- 40y More prevalent in women. In women- more erotomanic
- 22. Delusional Disorder (cont.) Stable diagnosis: Therefore- a separate disease. Prognosis is good in women, good overall
- 23. Delusional Disorder (cont.) Treatment- extremely treatment- resistant. Most patients refuse treatment because they do not feel
- 24. Postpartum Psychosis (PPP) 1-2/1000 births Risk factors- personal or family HX of bipolar, schizoaffective or isolated
- 25. PPP- “the Rule of 50%” 50-60%- first childbirth 50%- no previous psychiatric HX that is- the
- 26. Clinical Presentation Acute onset- 2days- 2 weeks after childbirth. Almost all cases within 1 month Presenting
- 27. Treatment of PPP Always hospitalize! In many cases- compulsory hospitalization is imminent Since this is usually
- 28. Shared Delusional Disorder (Folie a Deux) A delusion develops in an individual in the context of
- 29. Shared Delusional Disorder (Folie a Deux) Extremely rare. Only case reports, no controlled studies Usually in
- 30. Culture- Bound Syndromes
- 31. Piblokto/Pibloktoq Region/Culture: Arctic and Subarctic Eskimos Piblokto = "arctic hysteria," prolonged, extreme excitement sometimes followed by
- 32. Amok (running amok)/Berserker Region/Culture: Southeast Asia, Scandinavia Violent, disorderly, or homicidal rage directed against other objects
- 33. Taijin Kyofusho Region/Culture: Japan Patients with taijin kyofusho (literally "the disorder of fear") experience extreme self-consciousness
- 34. Koro Region/Culture: Asia, Southeast Asia intense anxiety related to the belief that one's own genitalia are
- 35. Zar Region/Culture: Northern Africa, Middle East Attributed to spirit possession -- and not considered a pathology
- 36. Gururumba Region/Culture: New Guinea Gururumba describes an episode in which the afflicted person (usually a married
- 37. Axis II Disorders associated with Psychosis Stress + Predisposition Borderline and Schizotypal. In some cases- schizotypal
- 38. Test Yourself!
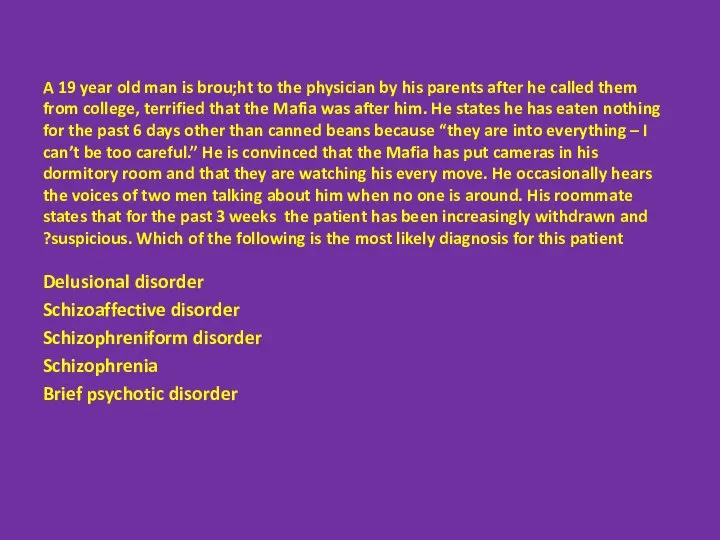
- 39. A 19 year old man is brou;ht to the physician by his parents after he called
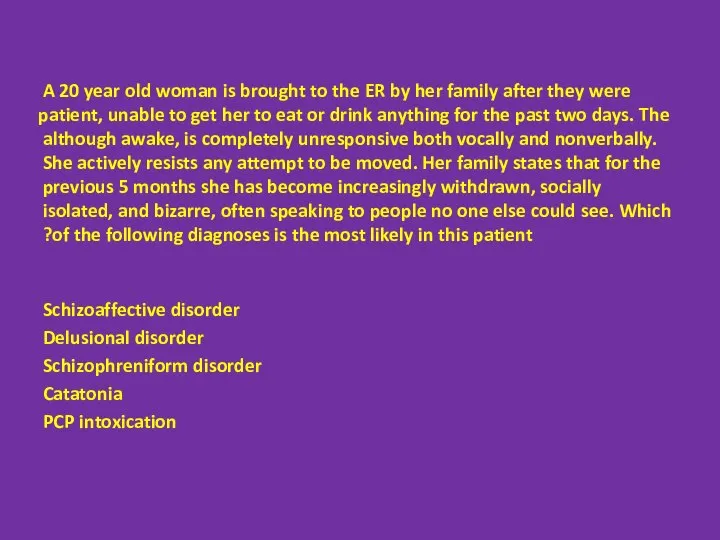
- 40. A 20 year old woman is brought to the ER by her family after they were
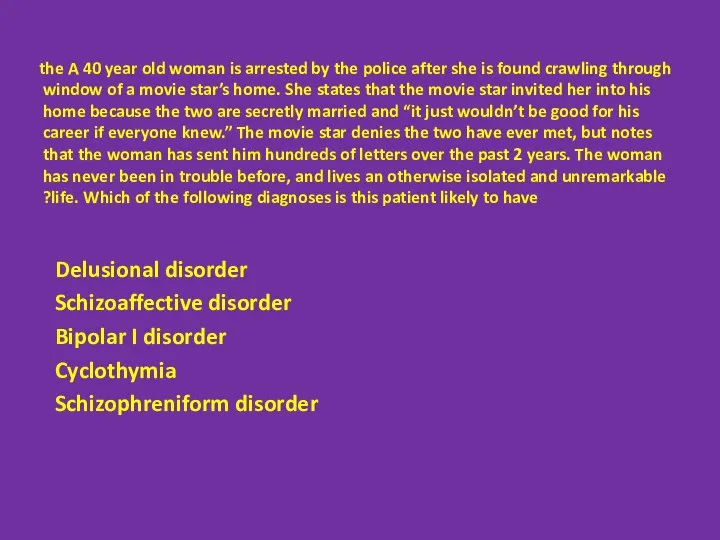
- 41. A 40 year old woman is arrested by the police after she is found crawling through
- 43. Скачать презентацию

 Патофизиология и диагностика вегетативных и коматозных состояний
Патофизиология и диагностика вегетативных и коматозных состояний Диагностика мотивации карьеры
Диагностика мотивации карьеры Психиатрия мен наркологиядағы экспертиза
Психиатрия мен наркологиядағы экспертиза Общественное здоровье и здравоохранение как наука, предмет преподавания и область практической деятельности
Общественное здоровье и здравоохранение как наука, предмет преподавания и область практической деятельности Личностный рост через снятие блоков и зажимов
Личностный рост через снятие блоков и зажимов Генодерматозы (наследственные заболевания кожи)
Генодерматозы (наследственные заболевания кожи) Other Psychotic Disorders
Other Psychotic Disorders Нарушения ритма при ишемической болезни сердца (ИБС)
Нарушения ритма при ишемической болезни сердца (ИБС) Психология лиц с нарушением зрения
Психология лиц с нарушением зрения Физиология беременности
Физиология беременности Вирусы герпеса
Вирусы герпеса Санитарно-эпидемиологический режим в педиатрическом отделении
Санитарно-эпидемиологический режим в педиатрическом отделении Миокард негізгі функцияларына әсер ететін. Дәрілік заттардың клиникалық фармакологиясы
Миокард негізгі функцияларына әсер ететін. Дәрілік заттардың клиникалық фармакологиясы Заболевания вен нижних конечностей
Заболевания вен нижних конечностей Методы исследования в неврологии
Методы исследования в неврологии Легочное сердце. Гемодинамические и электрофизиологические основы ремоделирования сердца
Легочное сердце. Гемодинамические и электрофизиологические основы ремоделирования сердца Дезинфицирующие средства
Дезинфицирующие средства Нормальная и вариантная рентгенангиографическая анатомия сердца. Аномалии коронарных артерий
Нормальная и вариантная рентгенангиографическая анатомия сердца. Аномалии коронарных артерий Қатерлі ісікті онкомаркерінің ерте диагностикасында диагностикалық маңызы
Қатерлі ісікті онкомаркерінің ерте диагностикасында диагностикалық маңызы Проект Соляная комната
Проект Соляная комната Антропометрія, як спосіб вимірювання частин тіла спортсмена. Соматотипування
Антропометрія, як спосіб вимірювання частин тіла спортсмена. Соматотипування Цветоощущение и восприятие цвета
Цветоощущение и восприятие цвета Мескалин как наркотик – действие, эффект, трип, привыкание
Мескалин как наркотик – действие, эффект, трип, привыкание ТФР
ТФР Переломы. Обучающая программа
Переломы. Обучающая программа Тірі ағзаға электр және магнит өрістерінің әсері. ЯМР және ЭПР құбылыстарды медициналық зерттеулерде қолдану
Тірі ағзаға электр және магнит өрістерінің әсері. ЯМР және ЭПР құбылыстарды медициналық зерттеулерде қолдану Создание здоровьесберегающей среды
Создание здоровьесберегающей среды Молекулярная диагностика рака молочной железы
Молекулярная диагностика рака молочной железы