Содержание
- 2. Other Psychotic Disorders Brief Psychotic Disorder Schizophreniform Disorder Schizoaffective Disorder Delusional Disorder Shared Psychotic Disorder Axis
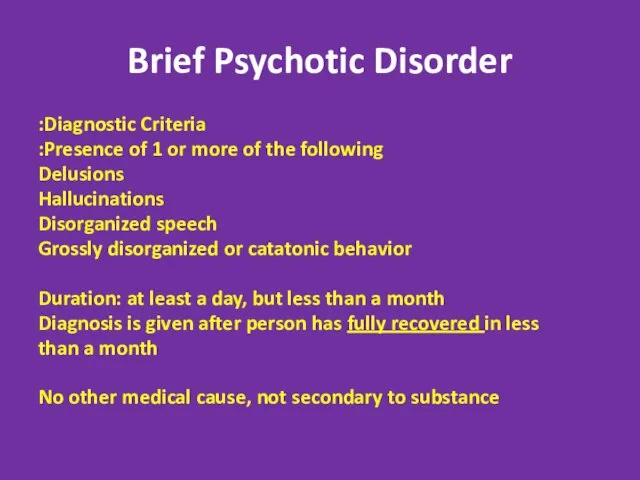
- 3. Brief Psychotic Disorder Diagnostic Criteria: Presence of 1 or more of the following: Delusions Hallucinations Disorganized
- 4. Brief Psychotic Disorder Per definition- always full recovery! Good prognosis- 50-80% never develop any psychiatric disease.
- 5. Specifiers for Brief Psychotic Disorder With Marked Stressors= brief reactive psychosis Without Marked Stressors With Postpartum
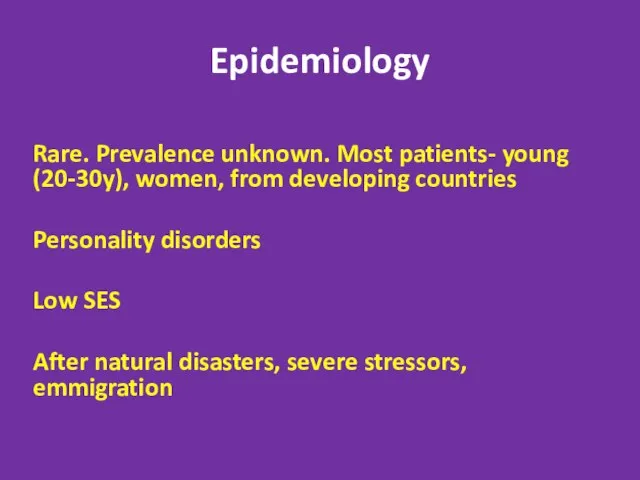
- 6. Epidemiology Rare. Prevalence unknown. Most patients- young (20-30y), women, from developing countries Personality disorders Low SES
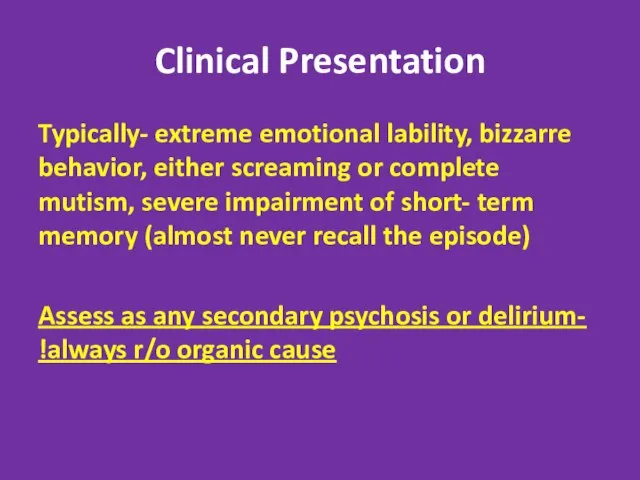
- 7. Clinical Presentation Typically- extreme emotional lability, bizzarre behavior, either screaming or complete mutism, severe impairment of
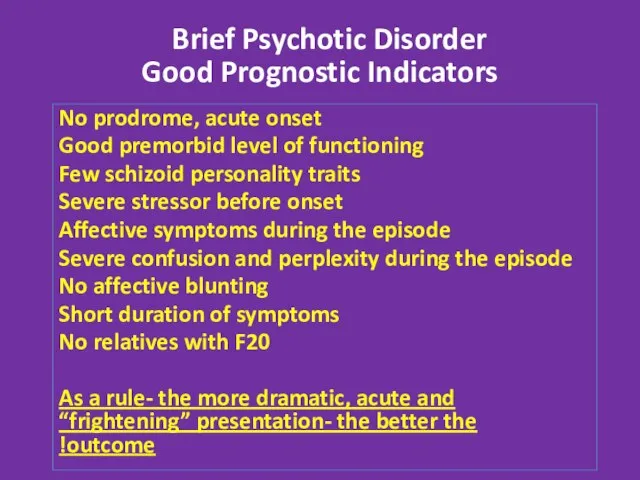
- 8. Good Prognostic Indicators No prodrome, acute onset Good premorbid level of functioning Few schizoid personality traits
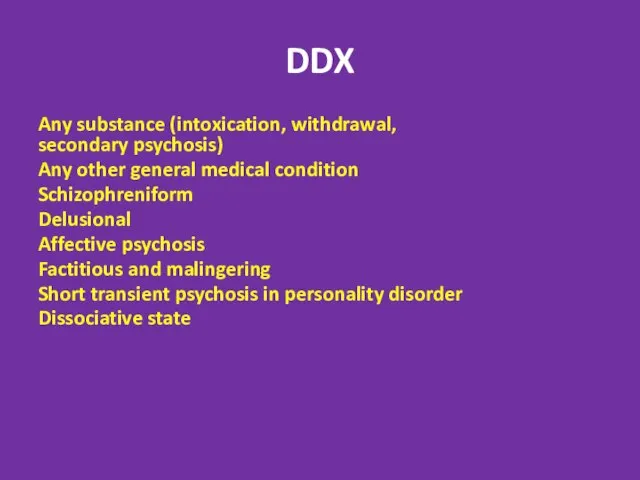
- 9. DDX דליריום (במקום הראשAny substance (intoxication, withdrawal, secondary psychosis) Any other general medical condition Schizophreniform Delusional
- 10. Treatment Hospitalization Antipsychotics- usually good and fast response Psychotherapy to deal with the potential trigger and
- 11. Postpartum Psychosis (PPP) 1-2/1000 births Risk factors- personal or family HX of bipolar, schizoaffective or isolated
- 12. PPP- “the Rule of 50%” 50-60%- first childbirth 50%- no previous psychiatric HX that is- the
- 13. Clinical Presentation Acute onset- 2days- 2 weeks after childbirth. Almost all cases within 1 month Presenting
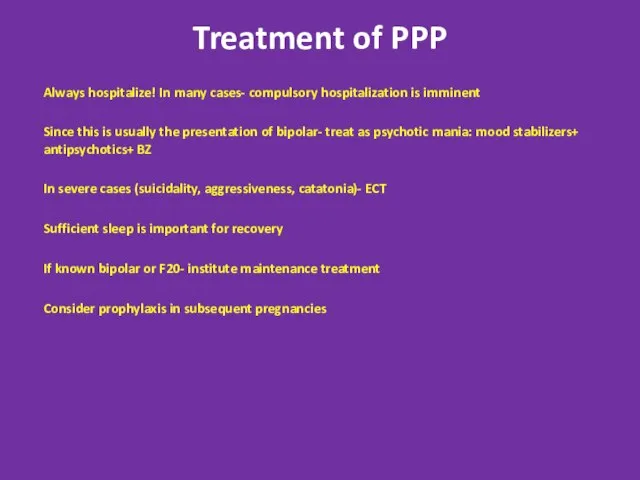
- 14. Treatment of PPP Always hospitalize! In many cases- compulsory hospitalization is imminent Since this is usually
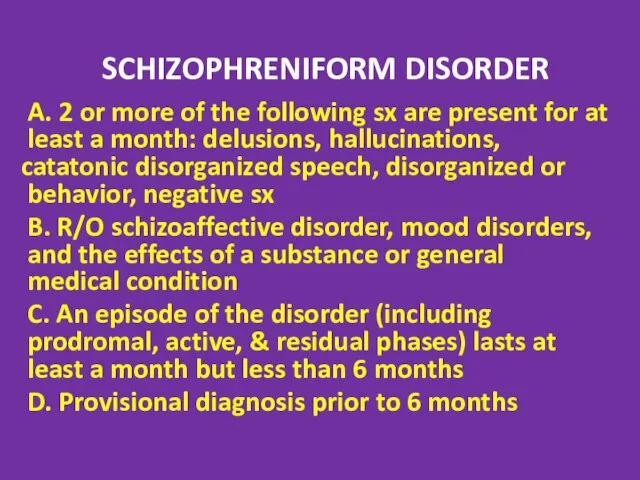
- 15. SCHIZOPHRENIFORM DISORDER A. 2 or more of the following sx are present for at least a
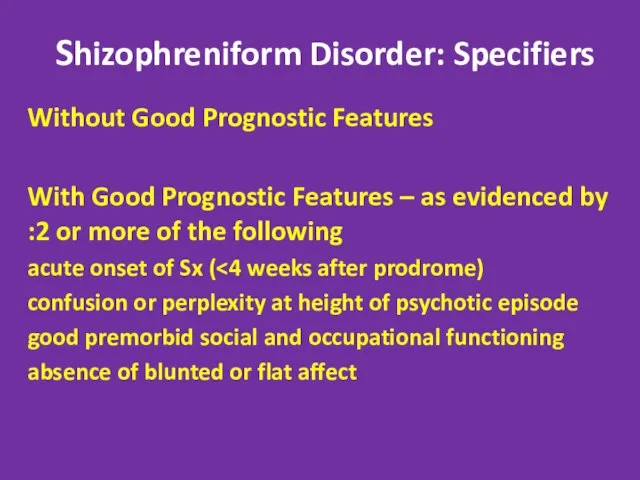
- 16. Shizophreniform Disorder: Specifiers Without Good Prognostic Features With Good Prognostic Features – as evidenced by 2
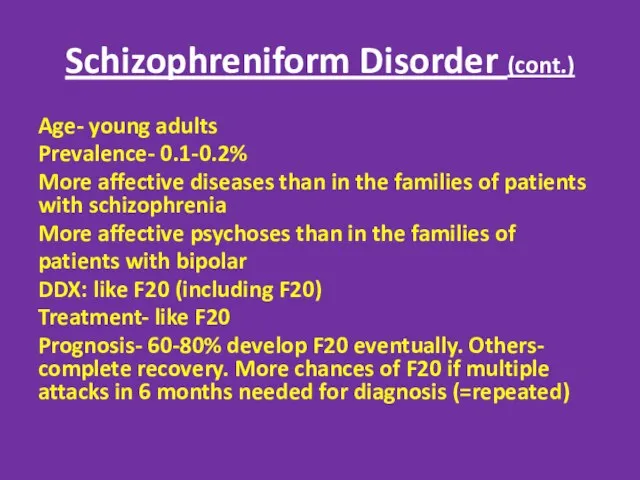
- 17. Schizophreniform Disorder (cont.) Age- young adults Prevalence- 0.1-0.2% More affective diseases than in the families of
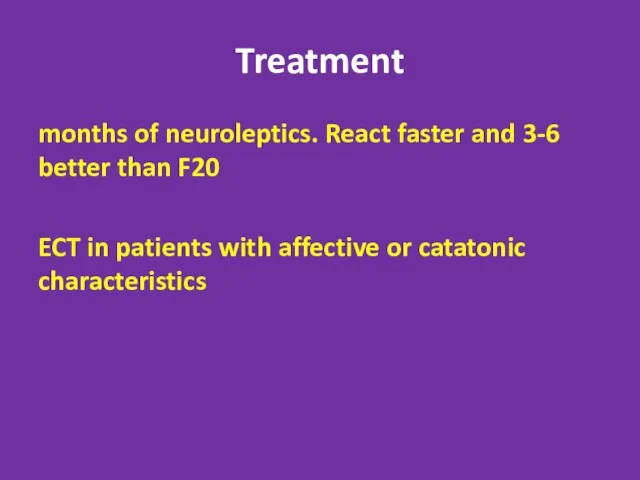
- 18. Treatment 3-6 months of neuroleptics. React faster and better than F20 ECT in patients with affective
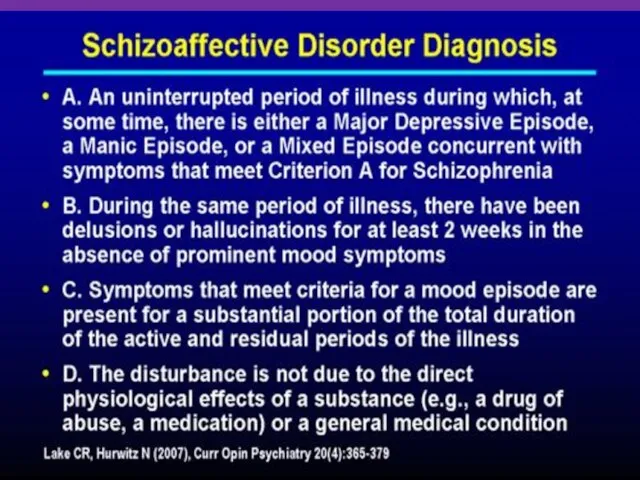
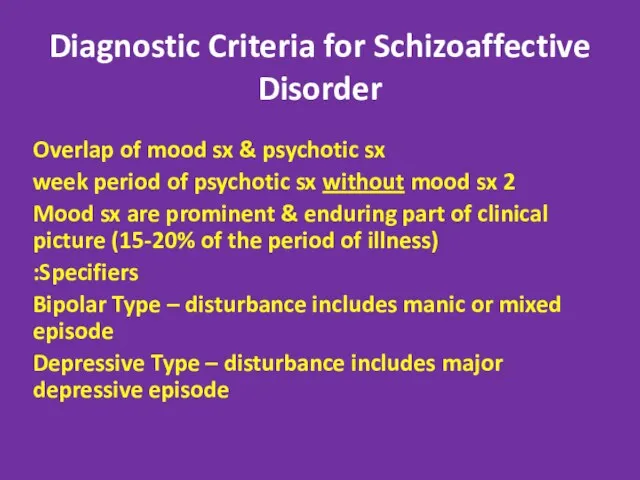
- 20. Diagnostic Criteria for Schizoaffective Disorder Overlap of mood sx & psychotic sx 2 week period of
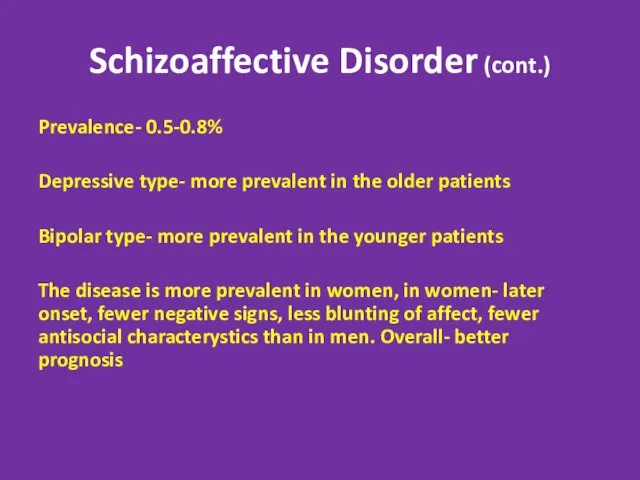
- 21. Schizoaffective Disorder (cont.) Prevalence- 0.5-0.8% Depressive type- more prevalent in the older patients Bipolar type- more
- 22. Schizoaffective Disorder (cont.) More F20 in the families of patients Prognosis- better than F20, worse than
- 23. DELUSIONAL DISORDER Diagnostic Criteria: A. Presence of 1 or more nonbizarre delusions (involve plausible situations, e.g.
- 24. Subtypes for Delusional Disorder Based on prominent delusional theme: Erotomanic: belief that another person, usually of
- 25. Delusional Disorder (cont.) Prevalence 0.3% Average age- 40y More prevalent in women. In women- more erotomanic
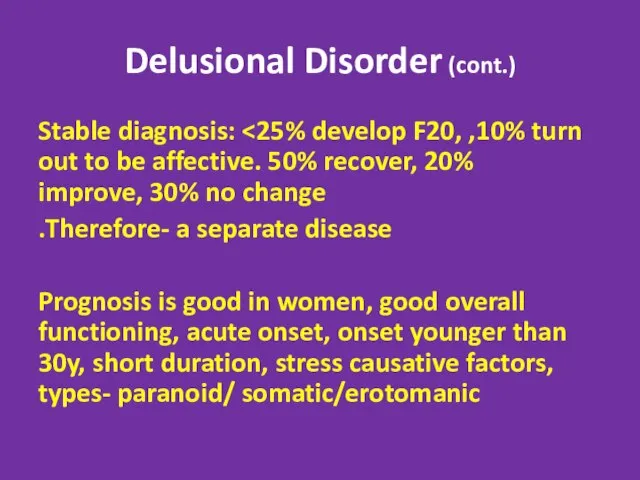
- 26. Delusional Disorder (cont.) Stable diagnosis: Therefore- a separate disease. Prognosis is good in women, good overall
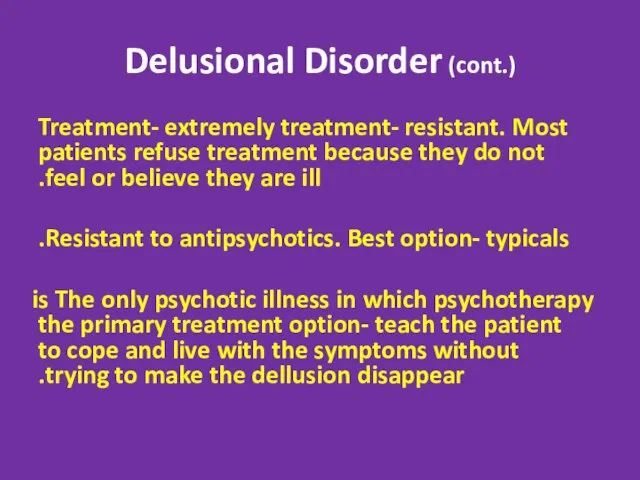
- 27. Delusional Disorder (cont.) Treatment- extremely treatment- resistant. Most patients refuse treatment because they do not feel
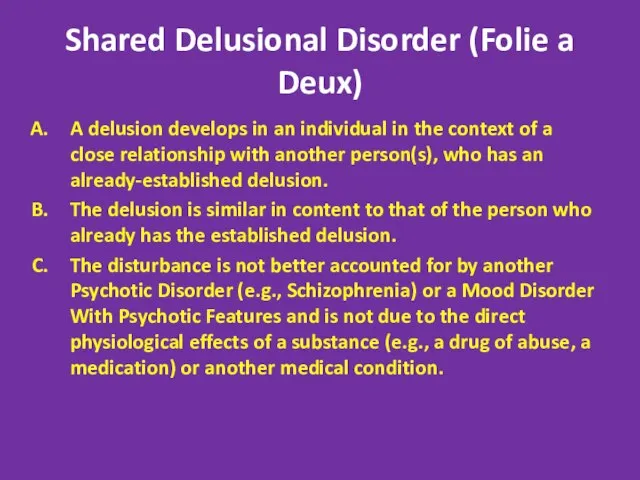
- 28. Shared Delusional Disorder (Folie a Deux) A delusion develops in an individual in the context of
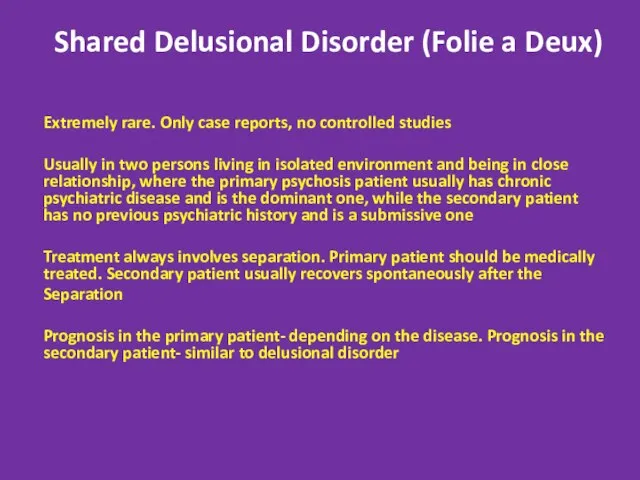
- 29. Shared Delusional Disorder (Folie a Deux) Extremely rare. Only case reports, no controlled studies Usually in
- 30. Capgras’ syndrome A delusional condition in which a patient falsely believes that someone, usually a close
- 31. Axis II Disorders associated with Psychosis Stress + Predisposition Borderline and Schizotypal. In some cases- schizotypal
- 32. Culture- Bound Syndromes
- 33. Piblokto/Pibloktoq Region/Culture: Arctic and Subarctic Eskimos Piblokto, also known as "arctic hysteria," describes a dissociative episode
- 34. Clinical Lycanthropy Region/Culture: Various Lycanthropy is a rare condition in which sufferers experience the delusion of
- 35. Wendigo Psychosis Region/Culture: Various Wendigo psychosis describes an insatiable craving for human flesh even when other
- 36. Amok (running amok)/Berserker Region/Culture: Southeast Asia, Scandinavia Loosely translated as "rampage" in Malay, amok is a
- 37. Taijin Kyofusho Region/Culture: Japan Patients with taijin kyofusho (literally "the disorder of fear") experience extreme self-consciousness
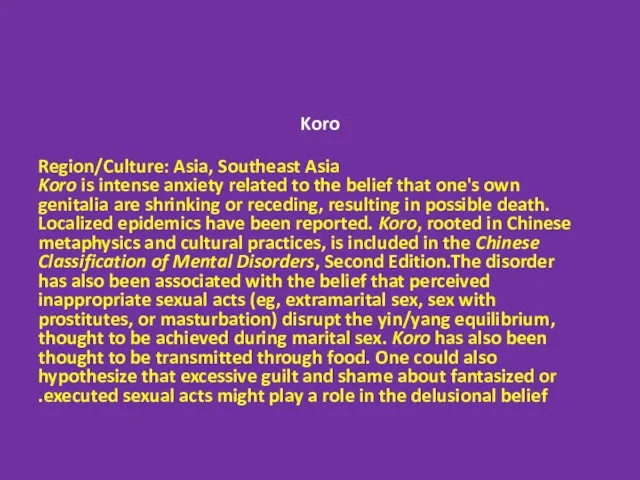
- 38. Koro Region/Culture: Asia, Southeast Asia Koro is intense anxiety related to the belief that one's own
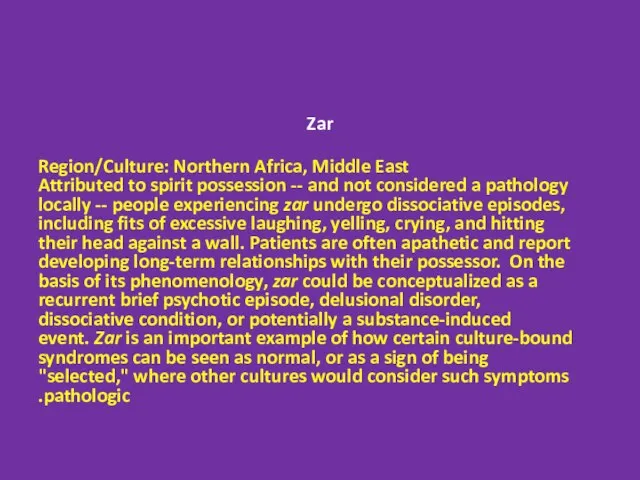
- 39. Zar Region/Culture: Northern Africa, Middle East Attributed to spirit possession -- and not considered a pathology
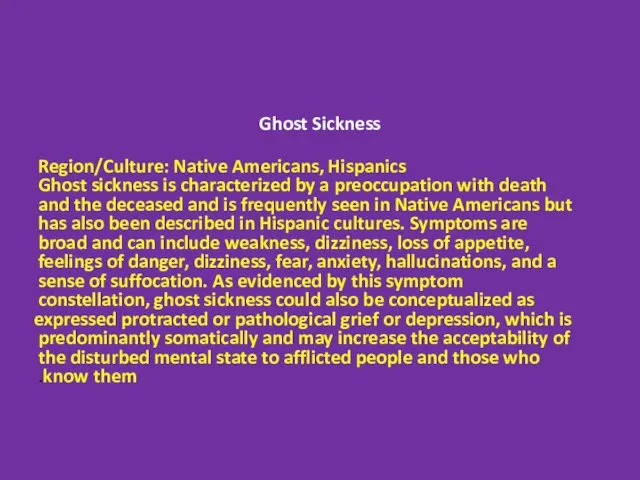
- 40. Ghost Sickness Region/Culture: Native Americans, Hispanics Ghost sickness is characterized by a preoccupation with death and
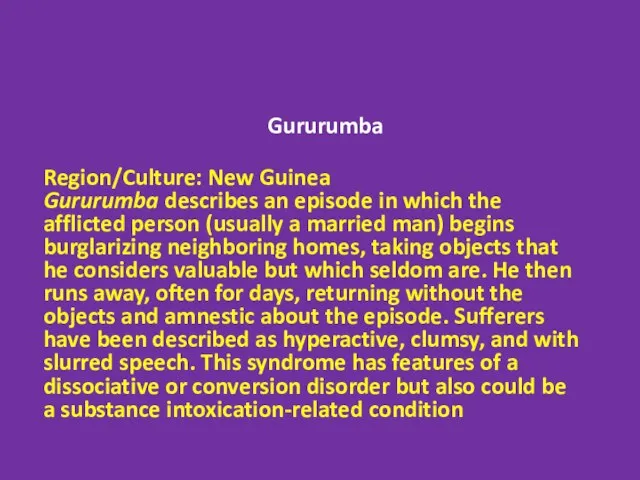
- 41. Gururumba Region/Culture: New Guinea Gururumba describes an episode in which the afflicted person (usually a married
- 42. Test Yourself!
- 43. A 19 year old man is brought to the physician by his parents after he called
- 44. A 20 year old woman is brought to the ER by her family after they were
- 45. A 40 year old woman is arrested by the police after she is found crawling through
- 47. Скачать презентацию
 Независимая оценка качества оказания услуг медицинскими организациями
Независимая оценка качества оказания услуг медицинскими организациями Диабет 2 типа
Диабет 2 типа Операционный блок хирургического отделения
Операционный блок хирургического отделения Глазные лекарственные формы
Глазные лекарственные формы Особенности логопедической работы с детьми дошкольного возраста с ринолалией
Особенности логопедической работы с детьми дошкольного возраста с ринолалией Еңбекке тәрбиелеу мен оқытуды ұйымдастыруға қойылатын талаптар
Еңбекке тәрбиелеу мен оқытуды ұйымдастыруға қойылатын талаптар Первая медицинская помощь при черепно-мозговых травмах
Первая медицинская помощь при черепно-мозговых травмах Варикозное расширение вен нижних конечностей
Варикозное расширение вен нижних конечностей Патофизиология печени
Патофизиология печени Принципи будови та функції нервової системи. Безумовні рефлекси. Система довільних рухів
Принципи будови та функції нервової системи. Безумовні рефлекси. Система довільних рухів Обида и чувство обиды
Обида и чувство обиды Современные методы комплексного лечения больных туберкулезом. Современные схемы лечения различных групп больных
Современные методы комплексного лечения больных туберкулезом. Современные схемы лечения различных групп больных Девиантное поведение. Устойчивое поведение личности, отклоняющееся от общепринятых, наиболее распространённых
Девиантное поведение. Устойчивое поведение личности, отклоняющееся от общепринятых, наиболее распространённых Иммобилизация переломов в возрастном аспекте
Иммобилизация переломов в возрастном аспекте Рассеянный склероз. Этиология и патогенез
Рассеянный склероз. Этиология и патогенез Этика и деонтология фармацевтического работника
Этика и деонтология фармацевтического работника Малыш до года. Инструкция по применению
Малыш до года. Инструкция по применению Невербальные коммуникации
Невербальные коммуникации Профилактика травматизма у детей школьного возраста. Сестринское дело
Профилактика травматизма у детей школьного возраста. Сестринское дело Коррекция кальций-фосфорного обмена у пациентов на гемодиализе
Коррекция кальций-фосфорного обмена у пациентов на гемодиализе Дифтерия у детей
Дифтерия у детей Средства, влияюшие на афферентную инервацию
Средства, влияюшие на афферентную инервацию Зачем нужна осознанность или что такое медитация
Зачем нужна осознанность или что такое медитация Введение в биохимию зубов. Биохимия межклеточного матрикса (Лекция № 1)
Введение в биохимию зубов. Биохимия межклеточного матрикса (Лекция № 1) Острый рабдомиолиз. Необычные и стертые варианты злокачественной гипертермии
Острый рабдомиолиз. Необычные и стертые варианты злокачественной гипертермии Смешанные дистрофии
Смешанные дистрофии Гепатопротекторы
Гепатопротекторы Классификация комбинированной гормональной контрацепции
Классификация комбинированной гормональной контрацепции