Содержание
- 2. General characteristics Unknown etiology, multifactorial disease Involve joints, kidneys, mucous membranes, the central nervous system Variety
- 3. Epidemiology Prevalence: 50-100 /100.000 Incidence: 2-7 /100.000/year age at onset: 20-30 Female vs. male ratio: 9-10:1
- 4. Etiology Family history (1st degree relatives 1%) Genetic predisposition MHC genes: HLA DR2,DR3 DR4-DIL, DR5-APS non-MHC
- 5. Etiology Provoking factors Sunlight, UV light Infections Hormonal status:estrogen, prolactin Drugs Isoniacid Hidantoin Hydralazin Procainamid D
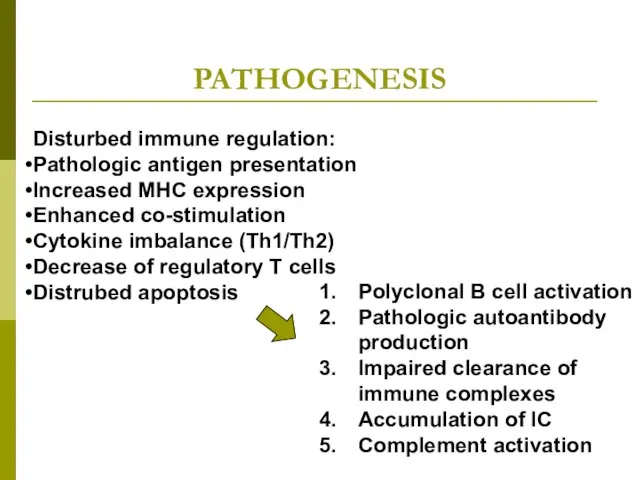
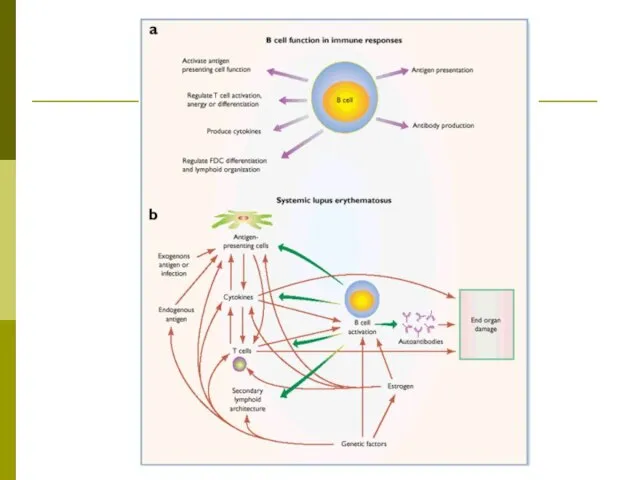
- 6. PATHOGENESIS Disturbed immune regulation: Pathologic antigen presentation Increased MHC expression Enhanced co-stimulation Cytokine imbalance (Th1/Th2) Decrease
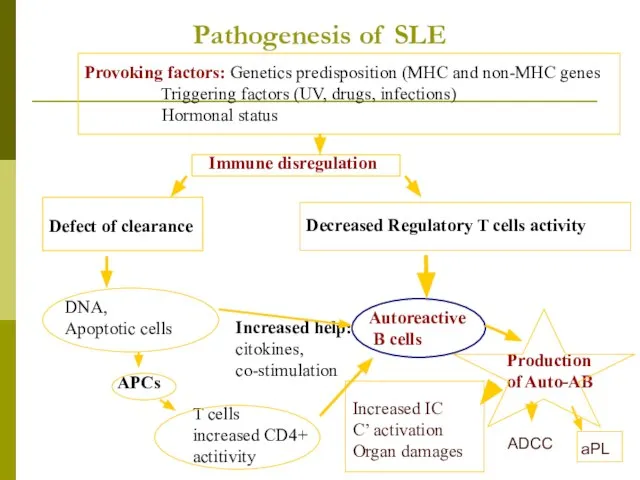
- 7. Pathogenesis of SLE Provoking factors: Genetics predisposition (MHC and non-MHC genes Triggering factors (UV, drugs, infections)
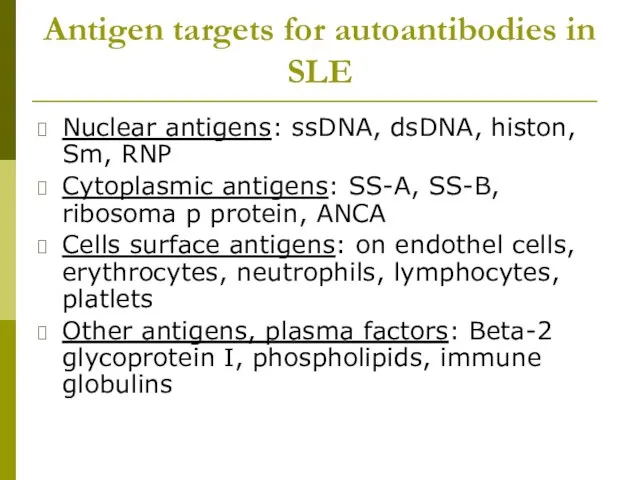
- 9. Antigen targets for autoantibodies in SLE Nuclear antigens: ssDNA, dsDNA, histon, Sm, RNP Cytoplasmic antigens: SS-A,
- 10. General symptoms Weakness Fatigue Tiredness Fever Weight loss Hair loss Lymphadenopathy
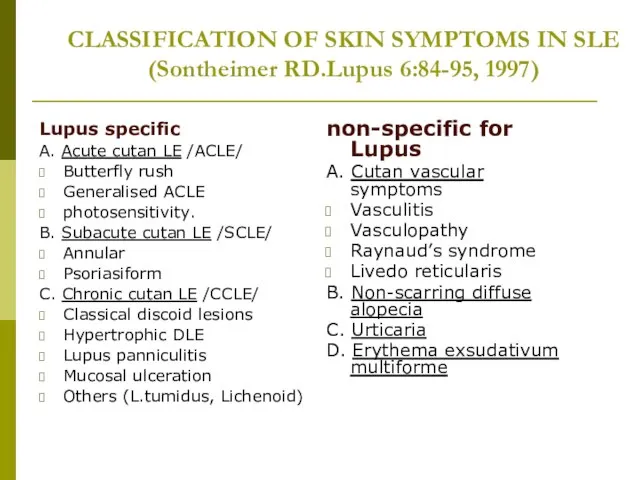
- 11. CLASSIFICATION OF SKIN SYMPTOMS IN SLE (Sontheimer RD.Lupus 6:84-95, 1997) Lupus specific A. Acute cutan LE
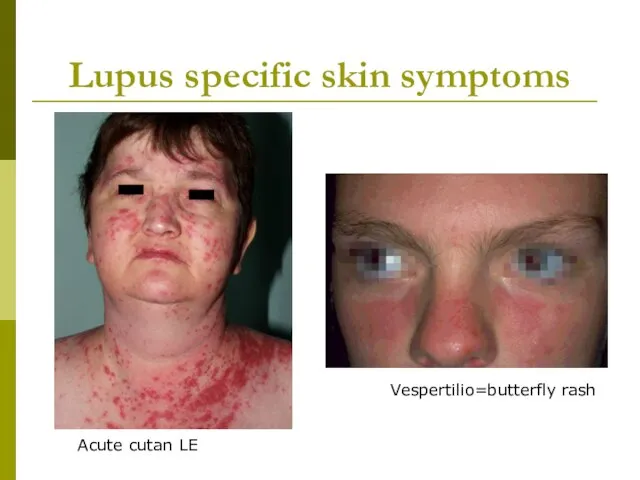
- 12. Lupus specific skin symptoms Vespertilio=butterfly rash Acute cutan LE
- 13. Lupus specific skin symptoms DLE SCLE
- 14. Non-lupus specific skin symptoms vasculitis Raynaud phenomenon
- 15. Musculosceletal involvment of lupus Small joint symmetric non erosive polyarthritis Aseptic femur neck necrosis Osteoporosis Myositis
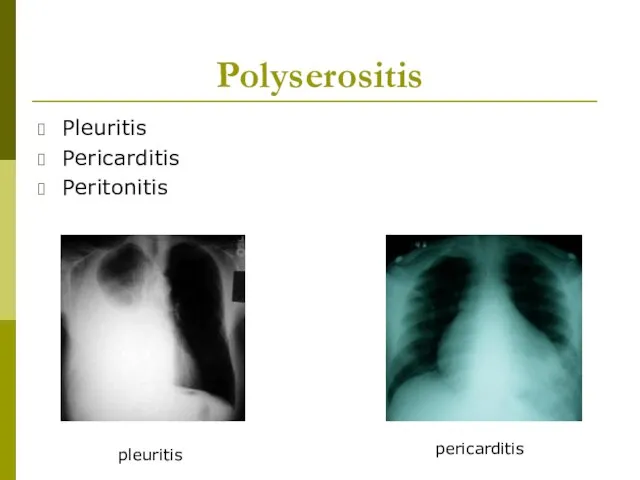
- 16. Polyserositis Pleuritis Pericarditis Peritonitis pleuritis pericarditis
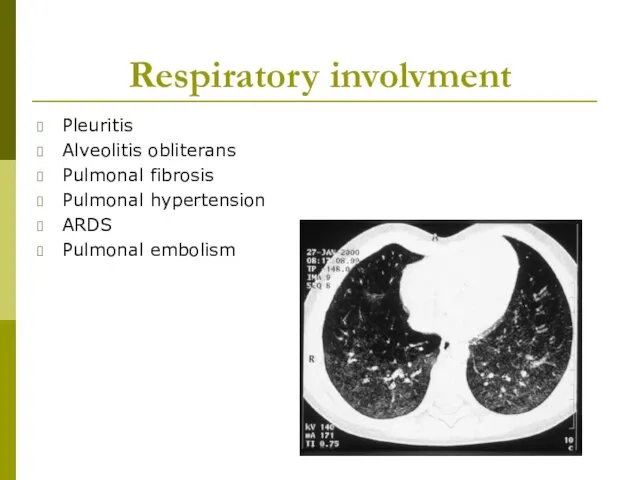
- 17. Respiratory involvment Pleuritis Alveolitis obliterans Pulmonal fibrosis Pulmonal hypertension ARDS Pulmonal embolism
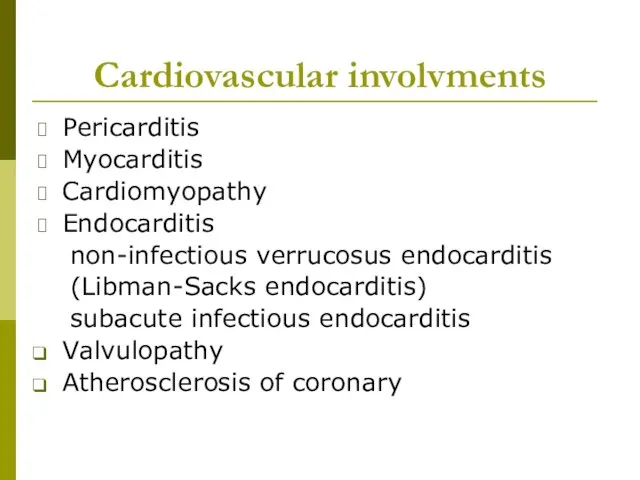
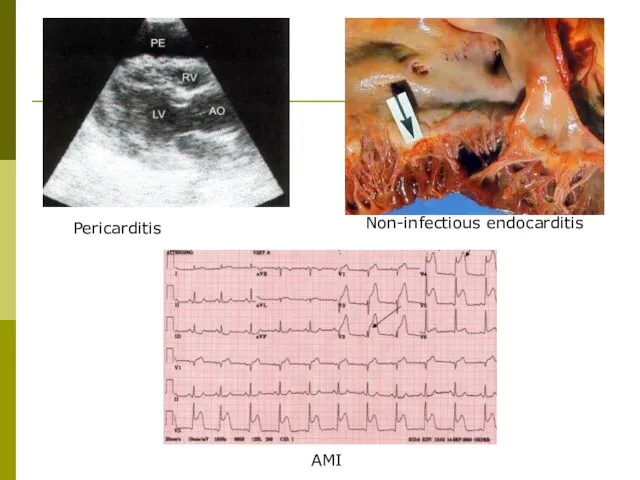
- 18. Cardiovascular involvments Pericarditis Myocarditis Cardiomyopathy Endocarditis non-infectious verrucosus endocarditis (Libman-Sacks endocarditis) subacute infectious endocarditis Valvulopathy Atherosclerosis
- 19. Pericarditis AMI Non-infectious endocarditis
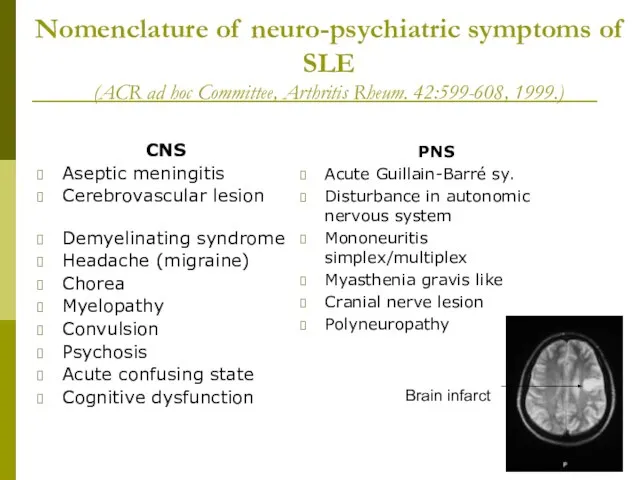
- 20. Nomenclature of neuro-psychiatric symptoms of SLE (ACR ad hoc Committee, Arthritis Rheum. 42:599-608, 1999.) CNS Aseptic
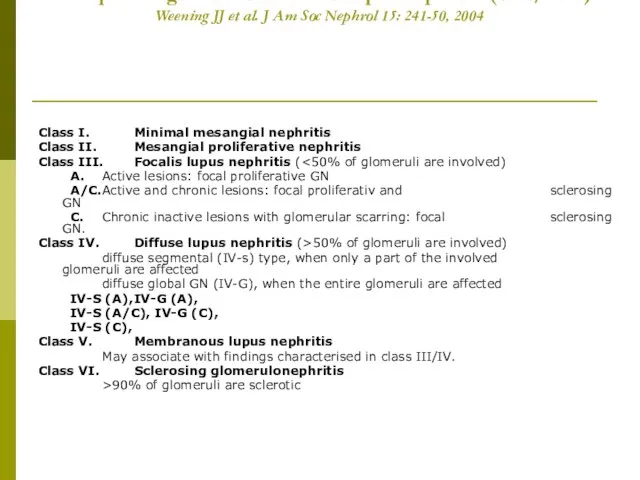
- 21. Histopathologic classification of lupus nephritis (ISN/RPS) Weening JJ et al. J Am Soc Nephrol 15: 241-50,
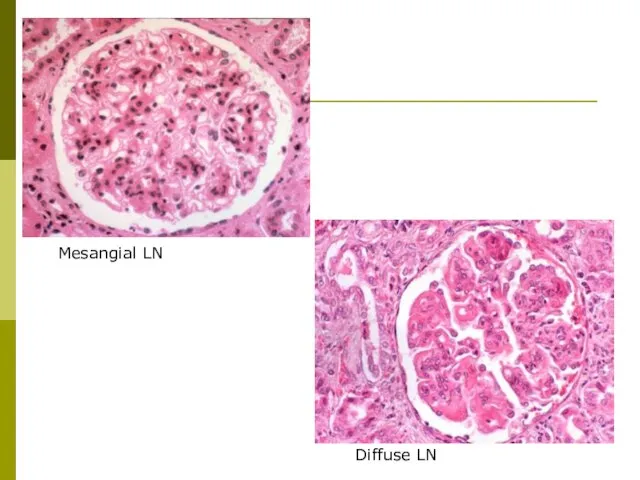
- 22. Mesangial LN Diffuse LN
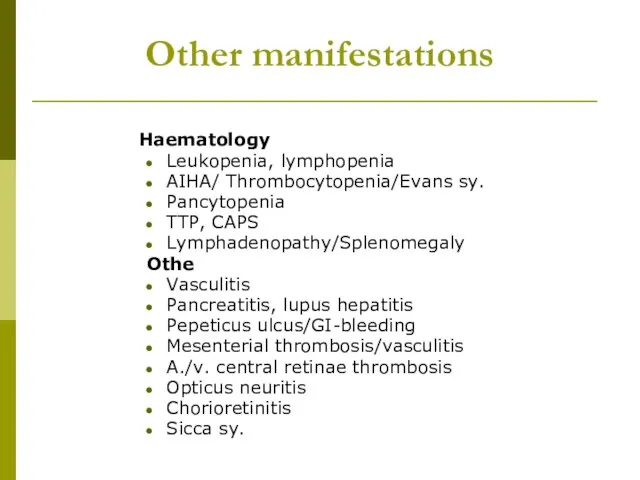
- 23. Other manifestations Haematology Leukopenia, lymphopenia AIHA/ Thrombocytopenia/Evans sy. Pancytopenia TTP, CAPS Lymphadenopathy/Splenomegaly Othe Vasculitis Pancreatitis, lupus
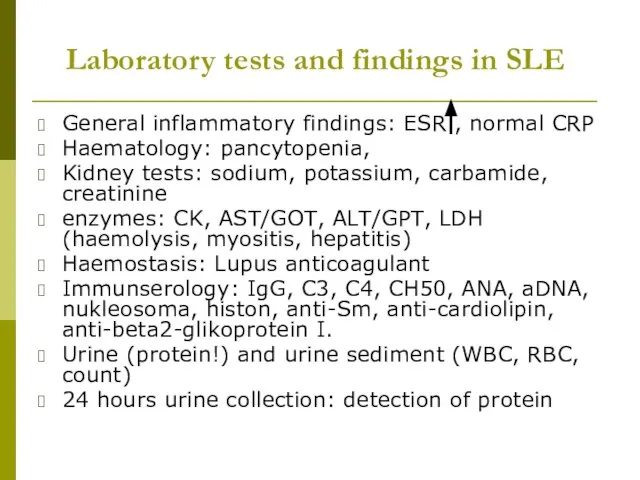
- 24. Laboratory tests and findings in SLE General inflammatory findings: ESR , normal CRP Haematology: pancytopenia, Kidney
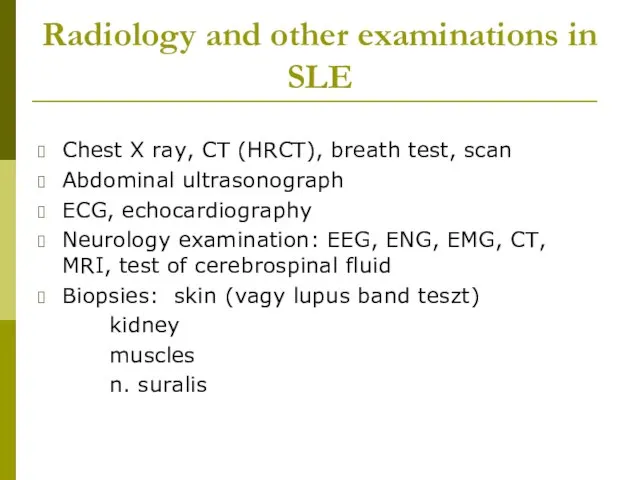
- 25. Radiology and other examinations in SLE Chest X ray, CT (HRCT), breath test, scan Abdominal ultrasonograph
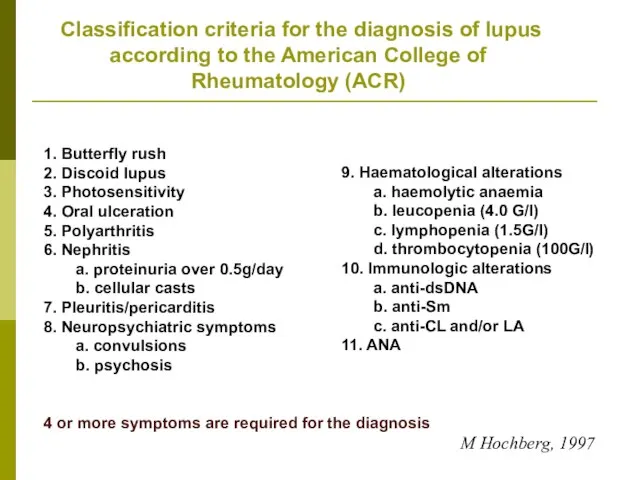
- 26. Classification criteria for the diagnosis of lupus according to the American College of Rheumatology (ACR) 1.
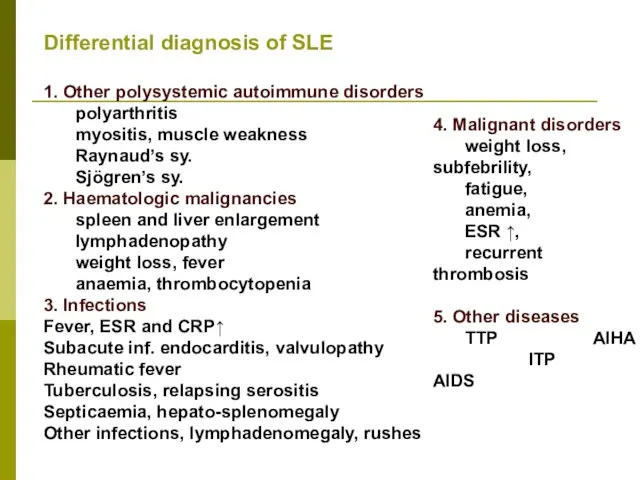
- 27. Differential diagnosis of SLE 1. Other polysystemic autoimmune disorders polyarthritis myositis, muscle weakness Raynaud’s sy. Sjögren’s
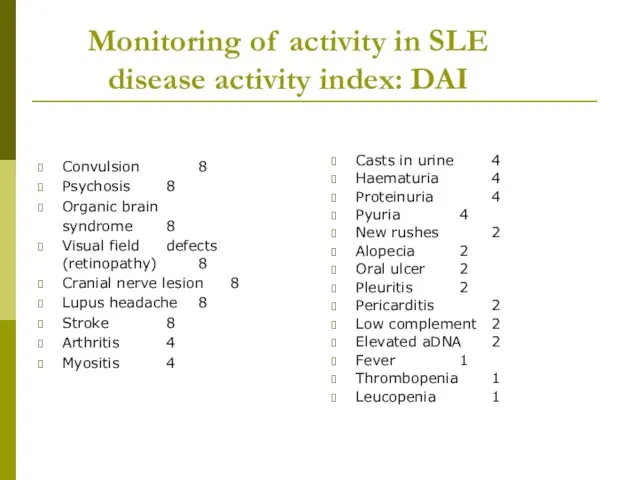
- 28. Monitoring of activity in SLE disease activity index: DAI Convulsion 8 Psychosis 8 Organic brain syndrome
- 29. Subgroups in SLE Subacute cutan lupus erythematosus Neonatal lupus erythematosus Drug-induced lupus SLE in elderly SLE
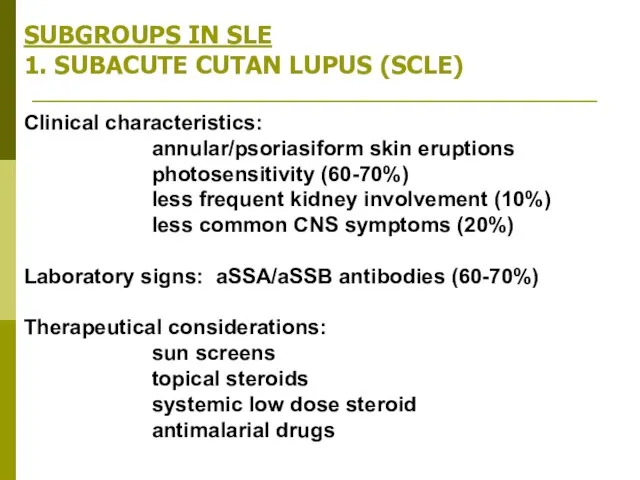
- 30. SUBGROUPS IN SLE 1. SUBACUTE CUTAN LUPUS (SCLE) Clinical characteristics: annular/psoriasiform skin eruptions photosensitivity (60-70%) less
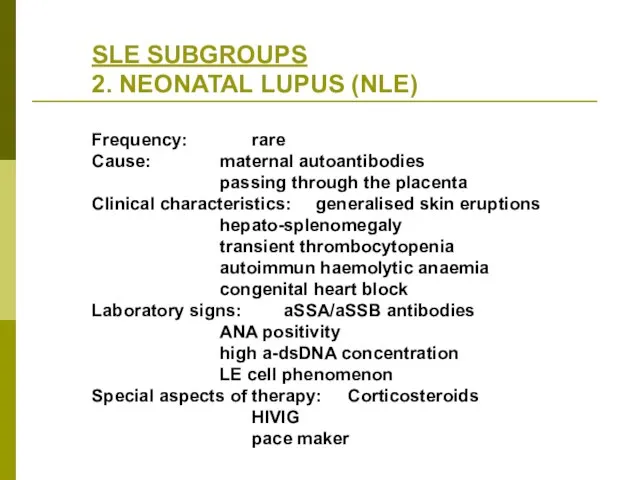
- 31. SLE SUBGROUPS 2. NEONATAL LUPUS (NLE) Frequency: rare Cause: maternal autoantibodies passing through the placenta Clinical
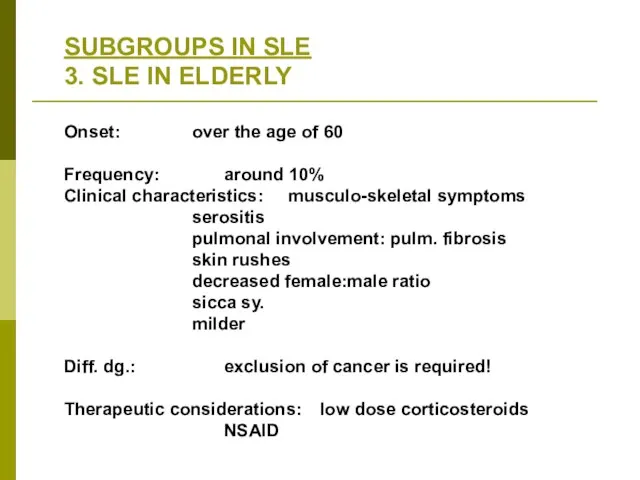
- 32. SUBGROUPS IN SLE 3. SLE IN ELDERLY Onset: over the age of 60 Frequency: around 10%
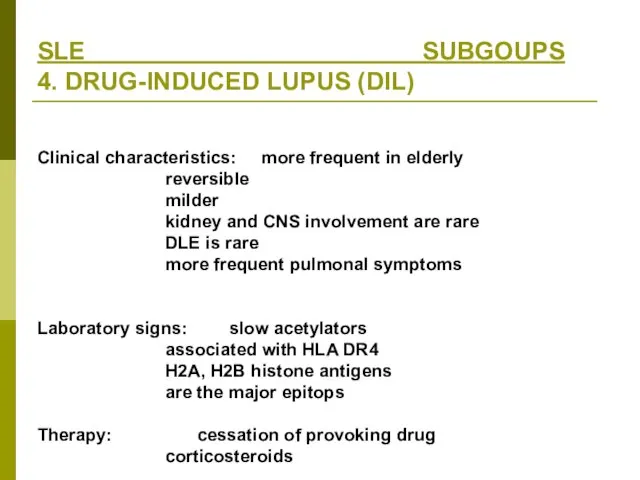
- 33. SLE SUBGOUPS 4. DRUG-INDUCED LUPUS (DIL) Clinical characteristics: more frequent in elderly reversible milder kidney and
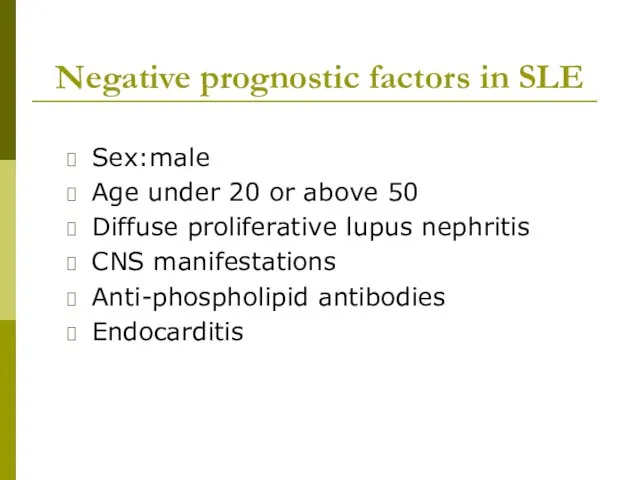
- 34. Negative prognostic factors in SLE Sex:male Age under 20 or above 50 Diffuse proliferative lupus nephritis
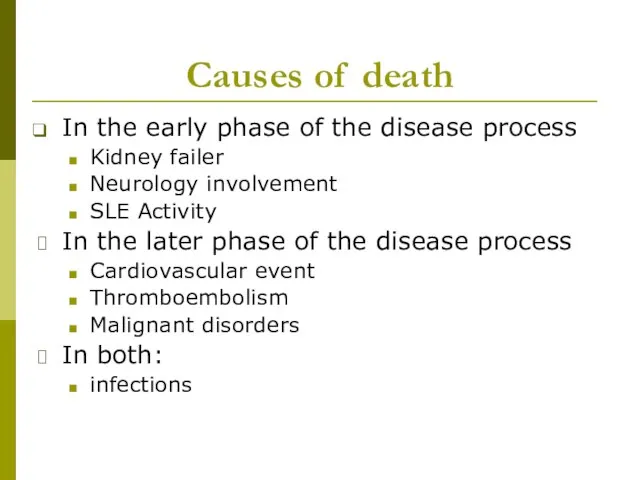
- 35. Causes of death In the early phase of the disease process Kidney failer Neurology involvement SLE
- 36. Therapy of lupus - General procedures Avoidance of UV lights Sunscreens Termination of the use of
- 37. Therapy of SLE Antimalarial drugs: hydroxichlorouin, chloroquin (Delagil) In the cases of arthralgia, arthritis, skin symptoms,
- 38. Therapy of SLE Steroids: methylpednisolon (Solu-Medrol, Medrol, Methypred) In acute flares and relapses in neonatal lupus:
- 39. Immunosupressives Methotrexat (Trexan) 7.5-20 mg/week, treatment of polyarthritis, vasculitis CAVE: bonemarrow and liver toxicity Azathiorpin (Imuran)
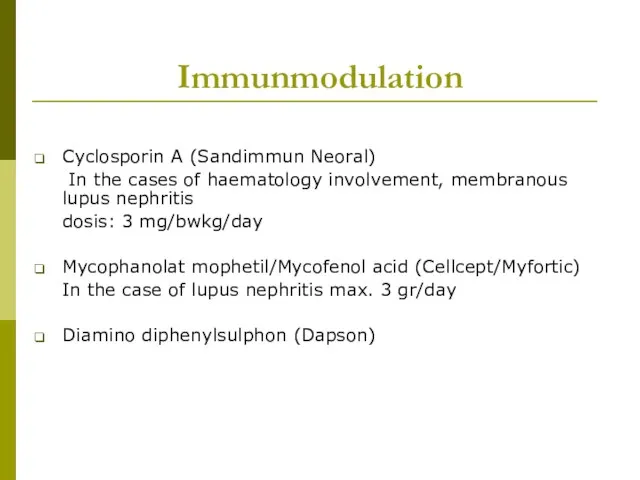
- 40. Immunmodulation Cyclosporin A (Sandimmun Neoral) In the cases of haematology involvement, membranous lupus nephritis dosis: 3
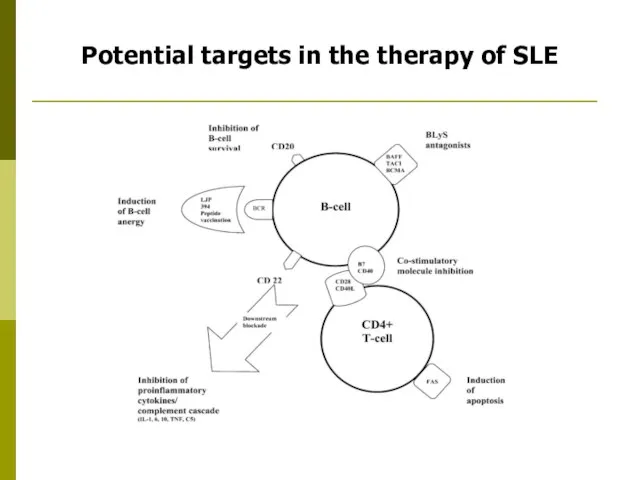
- 41. Potential targets in the therapy of SLE
- 43. Скачать презентацию


 С Днём учителя!
С Днём учителя! Golf GTI
Golf GTI Как я отдыхала летом в Одессе
Как я отдыхала летом в Одессе Mystic Places
Mystic Places Здания высоких технологий
Здания высоких технологий 20161029_pravovoy_turnir
20161029_pravovoy_turnir Электроснабжение объектов агропромышленного комплекса
Электроснабжение объектов агропромышленного комплекса Классный час Школьный этикет
Классный час Школьный этикет Супергидрофобты беттің мұздануға қарсы жүйеге әсері
Супергидрофобты беттің мұздануға қарсы жүйеге әсері Многоэтажные жилые дома
Многоэтажные жилые дома Измерительная система регистрации аварийных режимов полета самолета (вертолета) типа МСРП-12
Измерительная система регистрации аварийных режимов полета самолета (вертолета) типа МСРП-12 Теоретические основы технологического образования школьников
Теоретические основы технологического образования школьников Растровая и векторная анимация
Растровая и векторная анимация bezudarnye_okonchaniya_imen_prilagatelnyh
bezudarnye_okonchaniya_imen_prilagatelnyh космос группа №1
космос группа №1 Диафильм Серая Шейка
Диафильм Серая Шейка Информационное проектирование стратегических бизнес-процессов предприятия
Информационное проектирование стратегических бизнес-процессов предприятия Общежитие №7 Ул. Профессора Дедюкина, дом 22
Общежитие №7 Ул. Профессора Дедюкина, дом 22 Очень просто про самозанятость
Очень просто про самозанятость Виды оборудования для упаковки хлебобулочных изделий
Виды оборудования для упаковки хлебобулочных изделий Приближённые решения алгебраических и трансцендентных уравнений
Приближённые решения алгебраических и трансцендентных уравнений Свойства транспортируемых грузов
Свойства транспортируемых грузов 20150224_prezentatsiya_dekabristy_na_kubani
20150224_prezentatsiya_dekabristy_na_kubani Зашумлённый текст
Зашумлённый текст Stadii_i_zakony_razvitia_kollektiva_narodnogo_khudozhestvennogo
Stadii_i_zakony_razvitia_kollektiva_narodnogo_khudozhestvennogo 20160316_issled.rab_tradeskantsiya
20160316_issled.rab_tradeskantsiya The shades and ceiling lamps are made from natural materials
The shades and ceiling lamps are made from natural materials Ноутбук у нашому житті
Ноутбук у нашому житті