Содержание
- 2. anxiety- definition A condition with physical, cognitive and emotional manifestations that cause them to experience an
- 3. Определение понятия Тревога Это душевное состояние , характеризующееся психологическими, физиологическими и когнитивными изменениями, вызывающие у того,
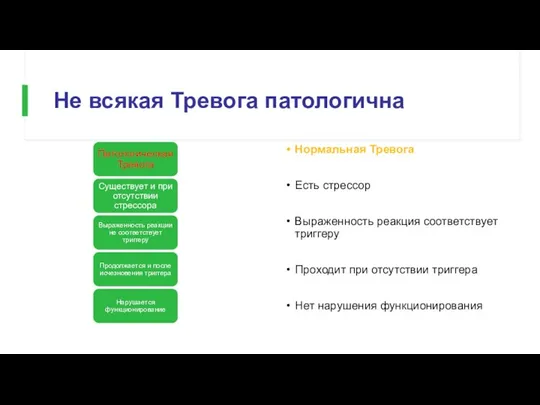
- 4. Не всякая Тревога патологична Нормальная Тревога Есть стрессор Выраженность реакция соответствует триггеру Проходит при отсутствии триггера
- 5. תפקידה החיובי של חרדה מוכנות- אנו נוטים להגיב יותר לאיומים המוכרים לנו מאלפי שנות אבולוציה (נחש,
- 6. Что хорошего в Тревоге? Готовность – мы легко реагируем на угрозы, знакомые нам в процессе тысячелетней
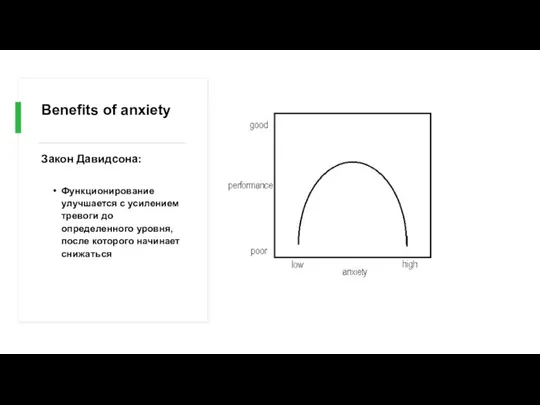
- 8. Benefits of anxiety Закон Давидсона: Функционирование улучшается с усилением тревоги до определенного уровня, после которого начинает
- 9. General considerations for anxiety disorders Often have an early onset- teens or early twenties Show 2:1
- 10. Общие сведения о тревожных расстройствах Часто имеют раннее начало - в подростковом возрасте или в начале
- 11. The differential diagnosis of anxiety. Psychiatric and Medical disorders. Psychiatr Clin North Am 1985 Mar;8(1):3-23 Primary
- 12. Primary versus Secondary Anxiety Тревога может быть вызвано одним из основных тревожных расстройств ИЛИ вторичным, в
- 13. What characteristics of primary anxiety disorders predict subsequent major depressive disorder. J Clin Psychiatry 2004 May;65(5):618-25
- 14. Comorbid diagnoses После постановки диагноза тревожного расстройства критически важно провести скрининг на наличие других психиатрических диагнозов,
- 15. Anxiety disorders Specific phobia Social anxiety disorder (SAD) Panic disorder (PD) Agoraphobia Generalized anxiety disorder (GAD)
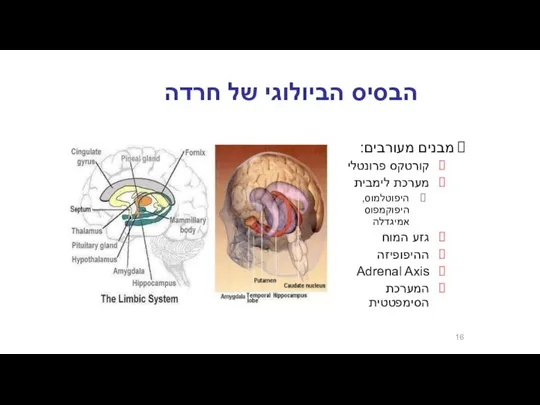
- 16. הבסיס הביולוגי של חרדה מבנים מעורבים: קורטקס פרונטלי מערכת לימבית היפוטלמוס, היפוקמפוס אמיגדלה גזע המוח ההיפופיזה
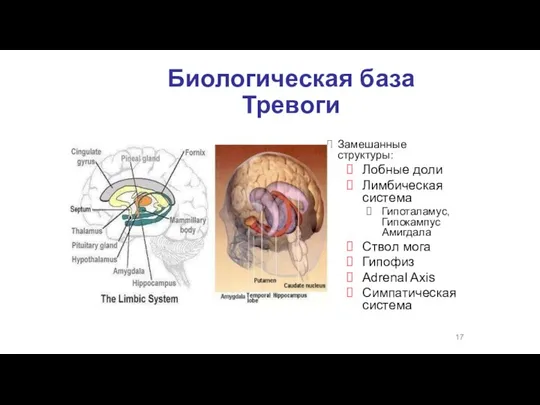
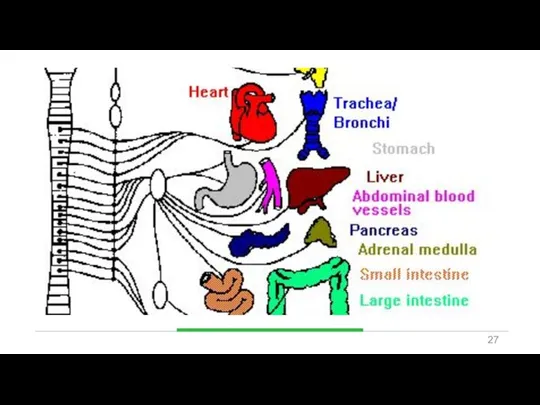
- 17. Биологическая база Тревоги Замешанные структуры: Лобные доли Лимбическая система Гипоталамус, Гипокампус Амигдала Ствол мога Гипофиз Adrenal
- 18. חרדה- מודלים ביולוגיים אמנם המחקר העכשווי מתמקד במבנים אנטומיים כגון האמיגדלה, ההיפוקמפוס ומסלולים נוירואנדוקרינים אבל... תגובות
- 19. אריק קנדל, חתן פרס נובל לרפואה/פיזיולוגיה לשנת 2000
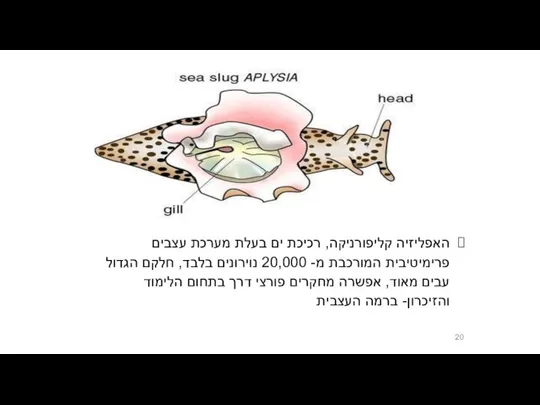
- 20. האפליזיה קליפורניקה, רכיכת ים בעלת מערכת עצבים פרימיטיבית המורכבת מ- 20,000 נוירונים בלבד, חלקם הגדול עבים
- 21. נגיעה בסיפון של האפליזיה גורמת לרתיעה נגיעה חוזרת בסיפון של האפליזיה מפחיתה את הרתיעה = הביטואציה
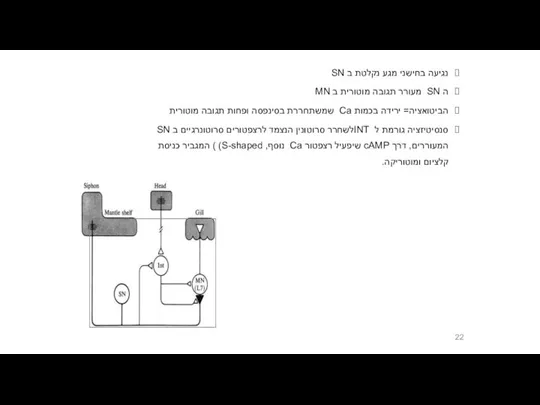
- 22. נגיעה בחישני מגע נקלטת ב SN ה SN מעורר תגובה מוטורית ב MN הביטואציה= ירידה בכמות
- 23. תגובת דחק Fight or Flight תגובה פיזיולוגית לדחק מווסתת דרך ההיפותלמוס ומבנים נוספים מאפשרת להתגונן בפני
- 24. Fight or Flight Физиологическая реакция на стресс Адаптируется с помощью гипоталамуса и других мозговоых структур Позволяет
- 25. מה קורה בתגובה הסימפתטית? מתרחשת על ידי אדרנלין ונוראדרנלין מעלה קצב לב והתכווצות הלב קצב נשימה
- 26. Что происходи при реакции симпатической системы? Происходит с помошью адреналина и норадреналина Усиливает частоту и силу
- 28. Pierre Janet לכל אדם יש כבאנטום מובנה של אנרגיה נפשית ובמצב תקין אין פעילות מנטאלית תת
- 29. Sigmund Freud דחפים מיניים ואגרסיביים מסולקים מעל פני השטח בגלל מוסכמות ואיסורים (סופר אגו) והקונפליקט יוצר
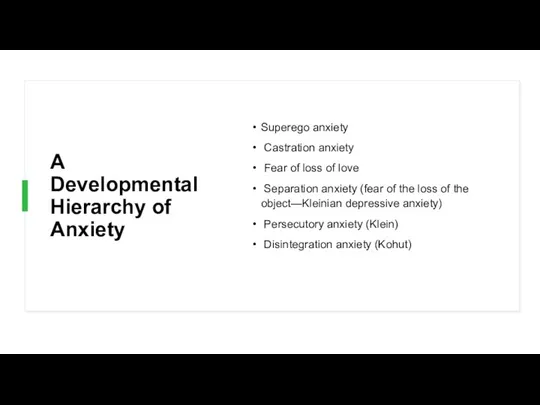
- 30. A Developmental Hierarchy of Anxiety Superego anxiety Castration anxiety Fear of loss of love Separation anxiety
- 34. To Be or NOT to Be
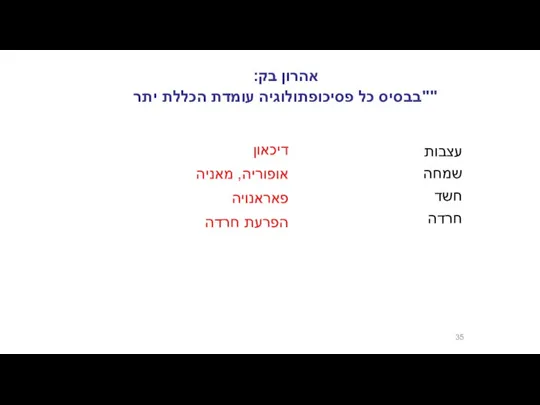
- 35. אהרון בק: "בבסיס כל פסיכופתולוגיה עומדת הכללת יתר" דיכאון אופוריה, מאניה פאראנויה הפרעת חרדה עצבות שמחה
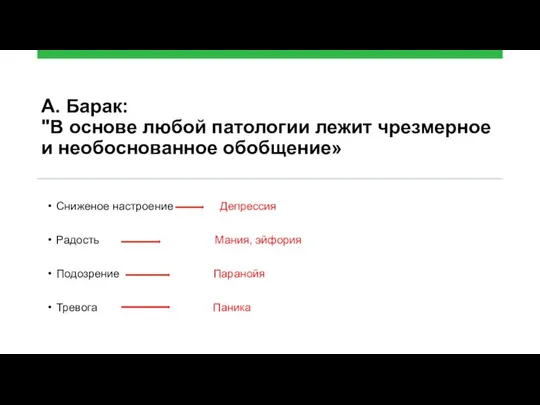
- 36. А. Барак: "В основе любой патологии лежит чрезмерное и необоснованное обобщение» Сниженое настроение Депрессия Радость Мания,
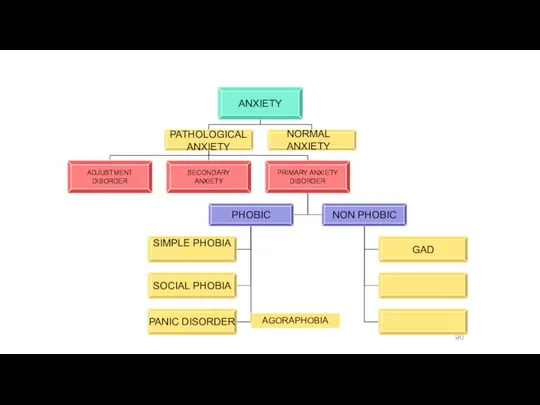
- 37. Pathological Anxiety כחלק מהפרעת הסתגלות כחלק ממחלה / הפרעה נפשית אחרת הפרעת חרדה ראשונית Maale Carmel
- 38. Pathological Anxiety
- 39. Primary Anxiety Disorders Нефобические тревожные реакции: GENERAILIZED ANXIETY DISORDER Фобические тревожные реакции: SIMPLE PHOBIA SOCIAL PHOBIA
- 40. אפידמיולוגיה ברוב המקרים נשים סובלות יותר, במיוחד בגילים בין 16 ל – 40. פחד קהל פי
- 41. Эпидемиология В большинстве своем женщины страдают чаще мужчин, в основном в возрасте 16-40 лет Социофобия в
- 42. Genetic Epidemiology of Anxiety Disorders Существует значительная семейная наследсвенность PD, GAD, OCD and phobias. Исследования близнецов
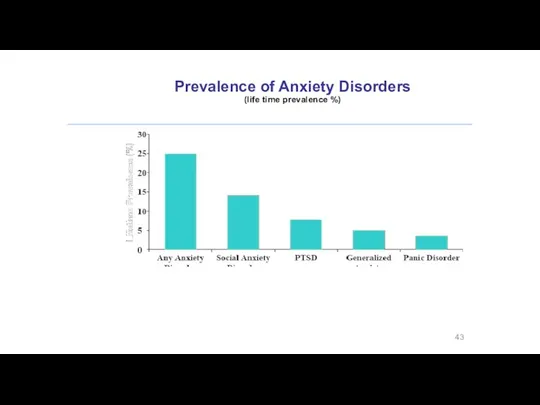
- 43. Prevalence of Anxiety Disorders (life time prevalence %)
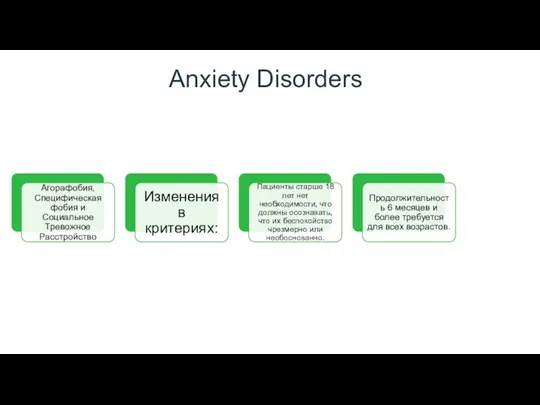
- 44. Anxiety Disorders
- 45. Panic Attacks and Agoraphobia are “unlinked” in DSM- 5 DSM- IV terminology describing different types of
- 46. Specific Phobia
- 47. SPECIFIC PHOBIA Animal Type Natural Environment Type (e.g., heights, storms, water) Blood-Injection-Injury Type Situational Type (e.g.,
- 48. Specific Phobia Выраженный или постоянный страх (> 6 месяцев), чрезмерный или необоснованный, вызванный присутствием или ожиданием
- 49. Specific Phobia Marked or persistent fear (>6 months) that is excessive or unreasonable cued by the
- 50. SPECIFIC PHOBIA Вне ситуации нормальное функционирование Избегание обеспечивает нормальное функционирование Высокая частота расстройства – до 20%
- 51. SPECIFIC PHOBIA The rest of the time normal functioning Avoidance allows for a normal life High
- 52. SOCIAL PHOBIA Подобно простой фобии, но здесь бессмысленный страх социального взаимодействия, отсюда: Более выраженные функциональные нарушения
- 53. SOCIAL PHOBIA Similar to simple phobia but here the senseless fear of social interaction, hence: More
- 54. SAD epidemiology 7% населения в целом Возраст наступления подростковый; чаще встречается у женщин. У половины пациентов
- 55. SAD epidemiology 7% of general population Age of onset teens; more common in women. Stein found
- 56. SAD A more problematic diagnosis (personality disorder) Two types: LIMITED PERVASIVE
- 57. What is going on in their brains?? Study of 16 SAD patients and 16 matched controls
- 58. What is going on in their brains?? Изучение 16 пациентов SAD и 16 контроля, во время
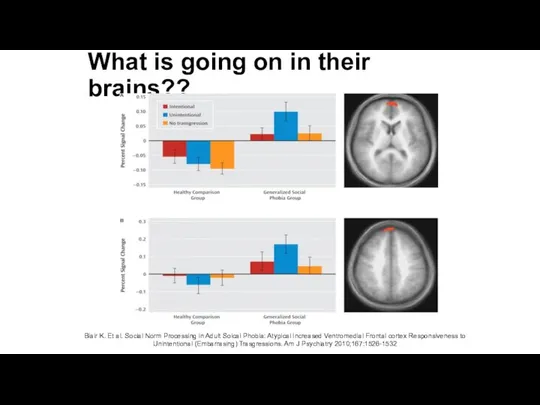
- 59. What is going on in their brains?? Both groups ↑ medial prefrontal cortex activity in response
- 60. What is going on in their brains?? Обе группы – обнаружена медиальная и префронтальная активность коры
- 61. What is going on in their brains?? Blair K. Et al. Social Norm Processing in Adult
- 62. Functional imaging studies in SAD Several studies have found hyperactivity of the amygdala even with a
- 63. Functional imaging studies in SAD Несколько исследований обнаружили гиперактивность Amygdala даже при слабой форме провокации (представление
- 64. Social Anxiety Disorder treatment Social skills training, behavior therapy, cognitive therapy Medication – SSRIs, SNRIs, MAOIs,
- 65. PANIC DISORDER Horror attack, extreme anxiety Spontaneous appears (at least at the beginning of the disease)
- 66. Panic Disorder Recurrent unexpected panic attacks and for a one month period or more of: Persistent
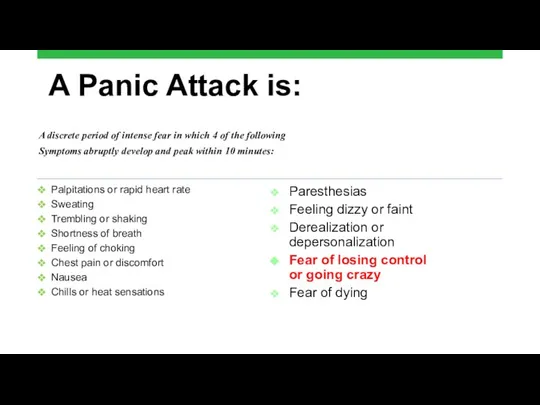
- 67. A Panic Attack is: Palpitations or rapid heart rate Sweating Trembling or shaking Shortness of breath
- 68. Panic disorder epidemiology 2-3% of general population; 5-10% of primary care patients. Onset in teens or
- 69. Things to keep in mind A panic attack ≠ panic disorder Panic disorder often has a
- 70. Panic Attacks with Agoraphobia Fear or avoidance of being in places or situations where there is
- 71. Panic Attacks with Agoraphobia Treatment: Combination of CBT treatment and medications: 1. Antidepressants 2. Anxiolytics for
- 72. Panic Disorder Comorbidity 50-60% have lifetime Major Depression One third have Current Depression 20-25% have history
- 73. Panic Disorder Etiology Drug/Alcohol Genetics Social learning Cognitive theories Neurobiology/conditioned fear Psychosocial stressors Prior separation anxiety
- 74. Treatment See 70% or better treatment response Education, reassurance, elimination of caffeine, alcohol, drugs, OTC stimulants
- 75. Agoraphobia Marked fear or anxiety for more than 6 months about two or more of the
- 76. Agoraphobia The individual fears or avoids these situations because escape might be difficult or help might
- 77. Prevalence 2% of the population Females to males - 2:1 Mean onset is 17 years 30%
- 78. Generalized Anxiety Excessive fear or anxiety, without any grasp of reality, is accompanied by expressions of
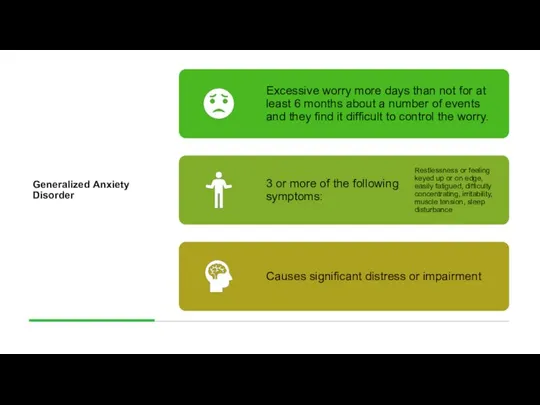
- 79. Generalized Anxiety Disorder
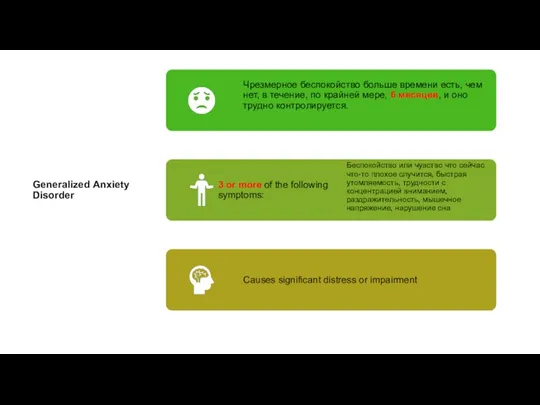
- 80. Generalized Anxiety Disorder
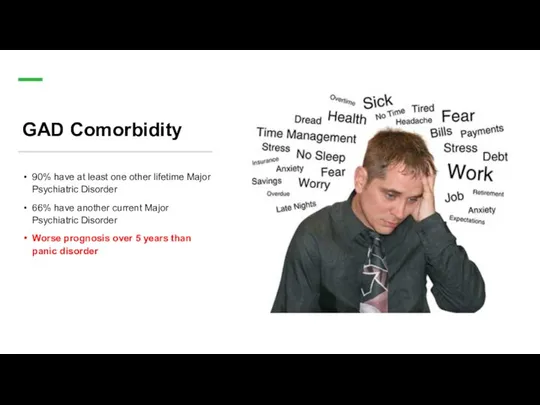
- 81. GAD Comorbidity 90% have at least one other lifetime Major Psychiatric Disorder 66% have another current
- 82. Long-Term Treatment Of GAD Need to treat long-term Full relapse in approximately 25% of patients 1
- 83. Pharmacotherapy for Anxiety Disorders Antidepressants Serotonin Selective Reuptake Inhibitors (SSRIs) Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) Atypical Antidepressants
- 84. Discontinuation of Treatment for Anxiety Disorders Withdrawal/rebound more common with Bzd than other anxiolytic treatment Relapse:
- 85. Strategies for Anxiolytic Discontinuation Slow taper Switch to longer-acting agent for taper Cognitive-Behavioral therapy Adjunctive Antidepressant
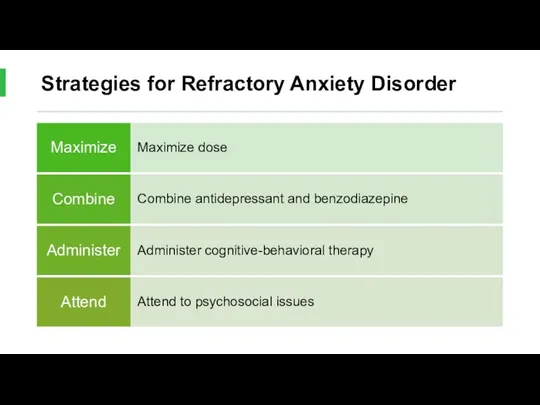
- 86. Strategies for Refractory Anxiety Disorder
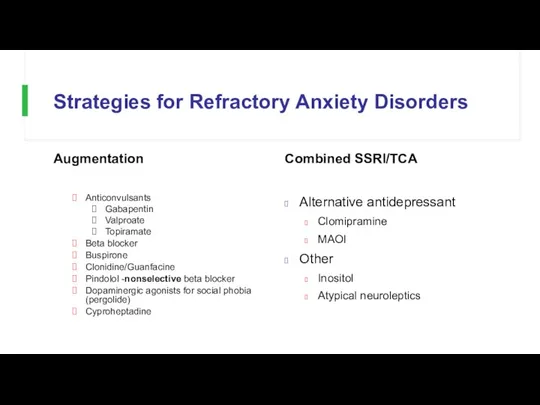
- 87. Strategies for Refractory Anxiety Disorders Augmentation Anticonvulsants Gabapentin Valproate Topiramate Beta blocker Buspirone Clonidine/Guanfacine Pindolol -nonselective
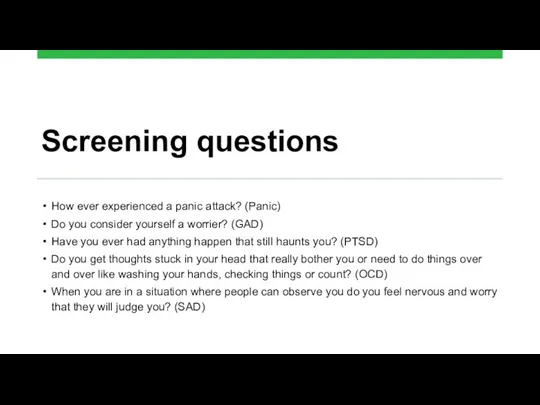
- 88. Screening questions How ever experienced a panic attack? (Panic) Do you consider yourself a worrier? (GAD)
- 89. Screening questions Как часто испытываете приступы паники? Опишите, что Вы называете Паникой Считаете ли Вы себя
- 90. AGORAPHOBIA
- 93. Trauma- and Stressor-Related Disorders New chapter in DSM-5 brings together anxiety disorders that are preceded by
- 94. Trauma- and Stressor-Related Disorders Новая глава в DSM-5 объединяет тревожные расстройства, которым предшествует тревожное или травматическое
- 95. Trauma- and Stressor-Related Disorders Acute Stress Disorder A. PTSD A Criterion B. No mandatory (e.g., dissociative,
- 96. ACUTE STRESS DISORDER A. Exposure to actual or threatened death, serious injury, or sexual violation in
- 97. ACUTE STRESS DISORDER A. Воздействие фактической или вероятной смерти, серьезных травм или сексуальных действий одним (или
- 98. ACUTE STRESS DISORDER B. Presence of nine (or more) of the following symptoms from any of
- 99. ACUTE STRESS DISORDER Intrusion symptoms: 1. Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).
- 100. ACUTE STRESS DISORDER Intrusion symptoms: 1. Повторяющиеся, непроизвольные и навязчивые тревожные воспоминания о травматическом событии (ы).
- 101. ACUTE STRESS DISORDER Negative Mood 5. Persistent inability to experience positive emotions (e.g., inability to experience
- 102. ACUTE STRESS DISORDER Negative Mood 5. Постоянная неспособность испытывать положительные эмоции (например, неспособность испытывать счастье, удовлетворение
- 103. ACUTE STRESS DISORDER Avoidance Symptoms 8. Efforts to avoid distressing memories, thoughts, or feelings about or
- 104. ACUTE STRESS DISORDER Avoidance Symptoms 8. Усилия, чтобы избежать тревожных воспоминаний, мыслей или чувств тесно связанных
- 105. ACUTE STRESS DISORDER Arousal Symptoms 10. Sleep disturbance (e.g., difficulty falling or staying asleep, restless sleep).
- 106. ACUTE STRESS DISORDER C. Duration of the disturbance (symptoms in Criterion B) is 3 days to
- 107. ACUTE STRESS DISORDER C. Продолжительность нарушения (симптомы критериев B) составляет от 3 дней до 1 месяца
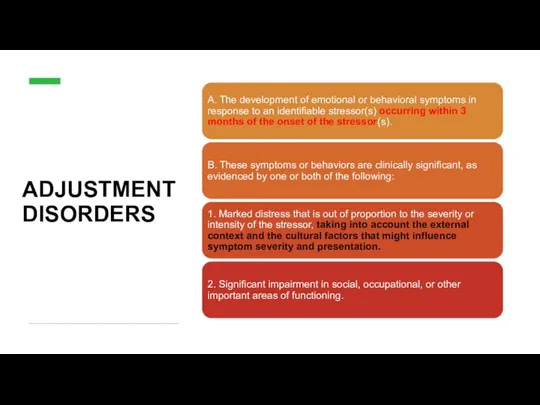
- 108. ADJUSTMENT DISORDERS
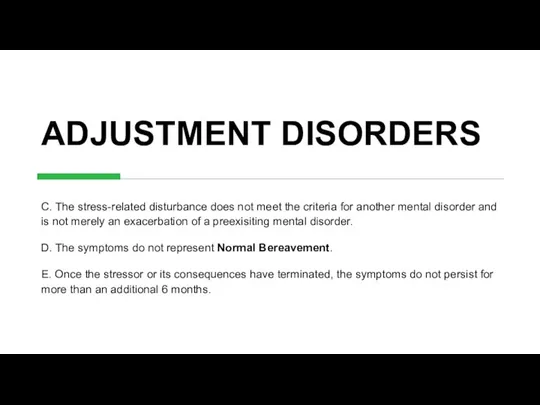
- 109. ADJUSTMENT DISORDERS C. The stress-related disturbance does not meet the criteria for another mental disorder and
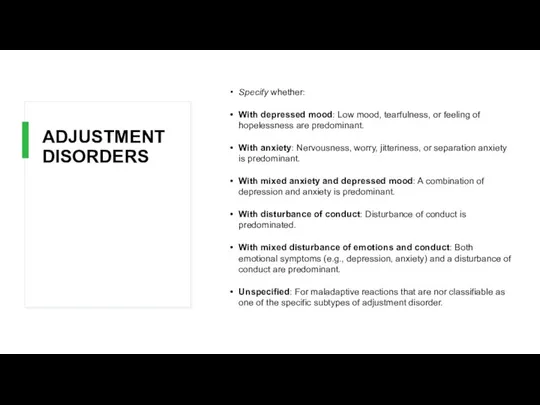
- 110. ADJUSTMENT DISORDERS Specify whether: With depressed mood: Low mood, tearfulness, or feeling of hopelessness are predominant.
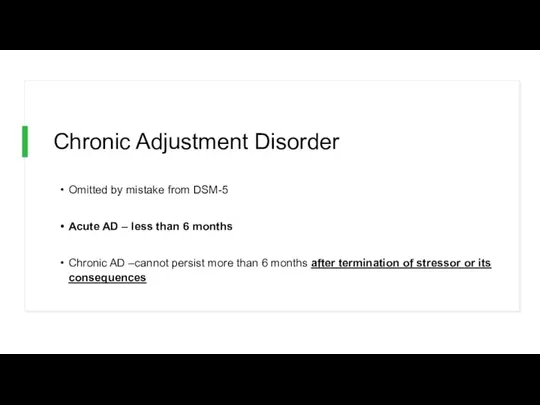
- 111. Chronic Adjustment Disorder Omitted by mistake from DSM-5 Acute AD – less than 6 months Chronic
- 112. Other Specified Trauma/Stressor-Related Disorder AD with duration more than 6 months without prolonged duration of stressor
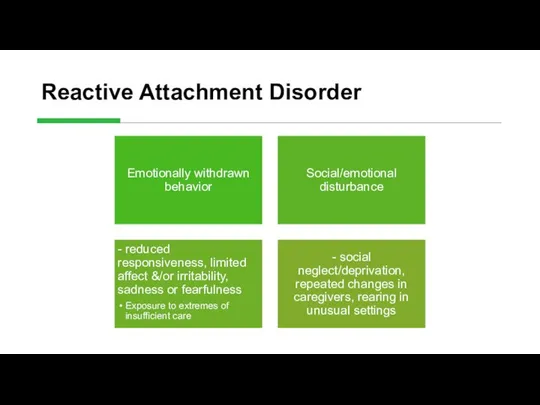
- 113. Reactive Attachment Disorder
- 114. Persistent Complex Bereavement Disorder Onset > 12 months after death of loved one Yearning/Sorrow/Pre-occupation with deceased
- 115. Persistent Complex Bereavement Disorder (PCBD) Diagnostic Criteria-ICD The person experienced the death of a close relative
- 116. Persistent Complex Bereavement Disorder (PCBD) Диагностические критерии-МКБ Человек пережил смерть близкого родственника или друга по крайней
- 117. Persistent Complex Bereavement Disorder (PCBD) Preoccupation with the circumstances of the death. In children, this preoccupation
- 118. Persistent Complex Bereavement Disorder (PCBD) Озабоченность обстоятельствами смерти. У детей эта забота об умерших может быть
- 119. Reactive Distress to the Death Marked difficulty accepting the death. In children, this is dependent on
- 120. Reactive Distress to the Death Значительные трудности принятия факта смерти. У детей это зависит от способности
- 121. Social/Identity Disruption A desire to die in order to be with the deceased. Difficulty trusting other
- 122. Social/Identity Disruption Стремление умереть, чтобы быть с покойным. Трудность доверять другим людям после смерти. Чувство одиночества
- 123. Specify if: With Traumatic Bereavement: Following a death that occurred under traumatic circumstances (homicide, suicide, disaster,
- 124. Specify if: С травматической утратой: После смерти, которая произошла при травматических обстоятельствах (убийство, самоубийство, катастрофа, или
- 125. Take home points Anxiety, and Related, and Trauma and Stressor-related disorders are common, common, common! There
- 127. Trauma- and Stressor-Related Disorders Changes in PTSD Criteria Четыре кластера симптомов, а не три Re-experiencing Avoidance
- 128. Trauma- and Stressor-Related Disorders Changes in PTSD Criteria DSM-5 more clearly defines what constitutes a traumatic
- 129. Trauma- and Stressor-Related Disorders Changes in PTSD Criteria DSM-5 более четко определяет, что представляет собой травматическое
- 130. Trauma- and Stressor-Related Disorders Changes in PTSD Criteria Recognition of PTSD in Young children Developmentally sensitive:
- 131. DSM-5: PTSD Criterion A A. The person was exposed to death, threatened death, actual or threatened
- 132. Criterion A (continued): 3. Indirectly, by learning that a close relative or close friend was exposed
- 133. Criterion A (continued): 3. Косвенно, узнать, что близкий родственник или близкий друг травмированы. Если событие связано
- 134. CRITERION B - Intrusion (5 Sx – Need 1) Recurrent, involuntary and intrusive recollections * *
- 135. C. Persistent effortful avoidance of distressing trauma-related stimuli after the event (1/2 symptoms needed): Trauma-related thoughts
- 136. CRITERION D – negative alterations in cognition & Mood (7 Sx – Need 2) Inability to
- 137. CRITERION D – negative alterations in cognition & Mood (7 Sx – Need 2) Неспособность вспомнить
- 138. CRITERION E – Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic
- 139. CRITERION E – Trauma-related alterations in arousal and reactivity that began or worsened after the traumatic
- 140. PTSD Criteria for DSM-5 F. Persistence of symptoms (in Criteria B, C, D and E) for
- 141. Preschool Subtype: 6 Years or Younger Relative to broader diagnosis for adults (or those over 6
- 142. A. In children (younger than 6 years), exposure to actual or threatened death, serious injury, or
- 143. DSM-5: Preschool PTSD Criterion B B. Presence of one or more intrusion symptoms associated with the
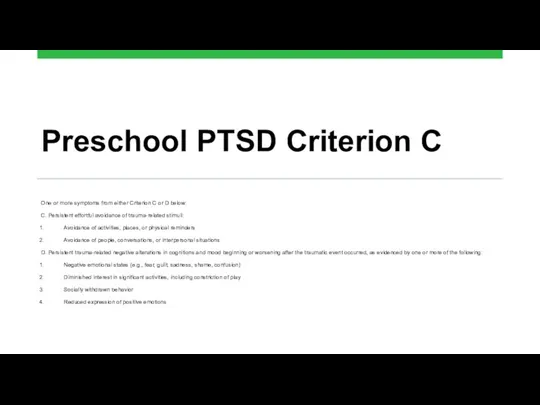
- 144. Preschool PTSD Criterion C One or more symptoms from either Criterion C or D below: C.
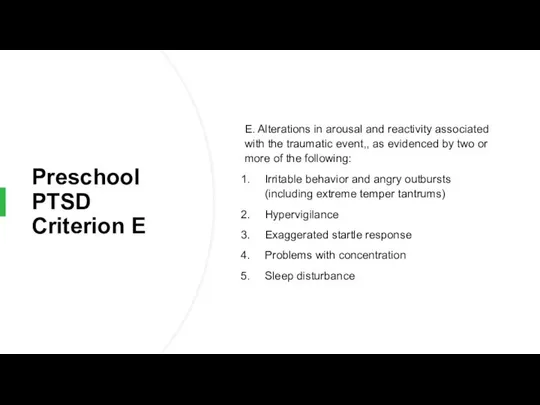
- 145. Preschool PTSD Criterion E E. Alterations in arousal and reactivity associated with the traumatic event,, as
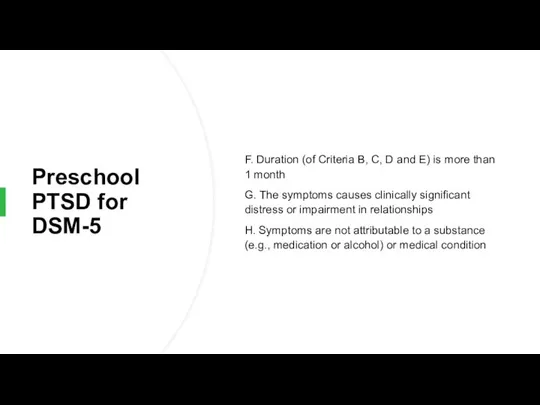
- 146. Preschool PTSD for DSM-5 F. Duration (of Criteria B, C, D and E) is more than
- 147. Summary: PTSD in DSM-5 Perhaps PTSD should be re-conceptualized as a spectrum disorder in which several
- 148. Summary: PTSD in DSM-5 Возможно, ПТСР следует ре-концептуализировать как расстройство спектра, при котором несколько различных патологических
- 149. Dissociative Subtype of PTSD New subtype for both age groupings of PTSD diagnosis: Meets PTSD diagnostic
- 150. specifiers Specify whether: With dissociative symptoms: The individual’s symptoms meet the criteria for PTSD, and in
- 151. specifiers Укажите, есть ли: С диссоциативными симптомами: Симптомы человека отвечают критериям ПТСР, и, кроме того, в
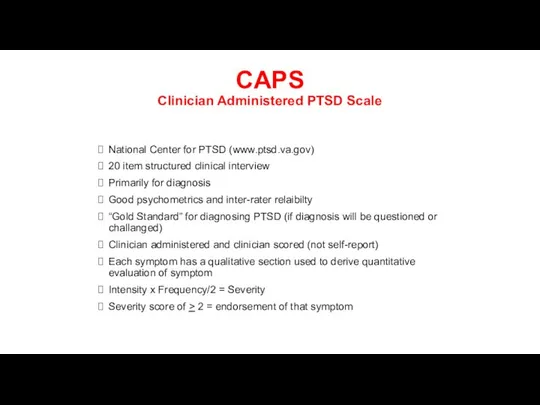
- 152. CAPS Clinician Administered PTSD Scale National Center for PTSD (www.ptsd.va.gov) 20 item structured clinical interview Primarily
- 153. 1. (B1) Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). Note: In children older
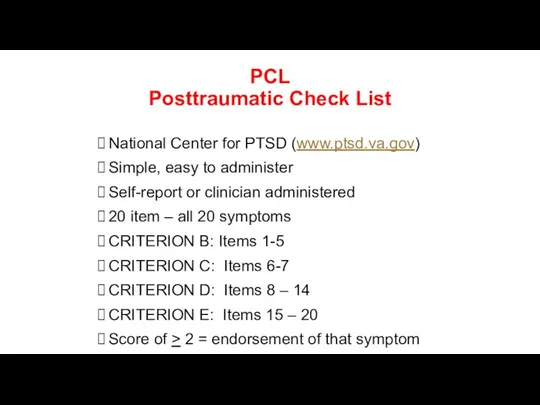
- 154. PCL Posttraumatic Check List National Center for PTSD (www.ptsd.va.gov) Simple, easy to administer Self-report or clinician
- 155. TRS Trauma Recovery Scale Gentry, 1996 Developed as an outcome instrument Good psychometrics (Chronbach’s a =
- 156. Early Sessions Graphic Time Line of life including ALL significant traumatic experiences Verbal Narrative using GTL
- 157. PTSD Epidemiology 7-9% of general population 60-80% of trauma victims 30% of combat veterans 50-80% of
- 158. PTSD Epidemiology Among the few diagnoses in DSM that speaks of etiology It is a severe
- 159. PTSD Epidemiology Среди немногих диагнозов в DSM, где известна этиология говорит об этиологии Это тяжелая умственная
- 160. Comorbidities Depression Other anxiety disorders Substance use disorders Somatization Dissociative disorders
- 161. Types of PTSD Acute PTSD - symptoms less than three months Chronic PTSD - symptoms more
- 162. Age of Onset and Cultural Features Can occur at any age, including childhood, and can affect
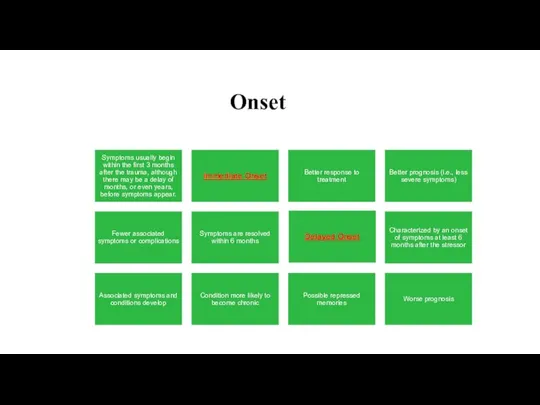
- 163. Onset
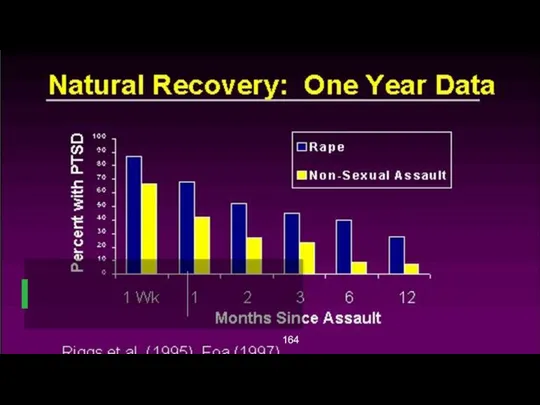
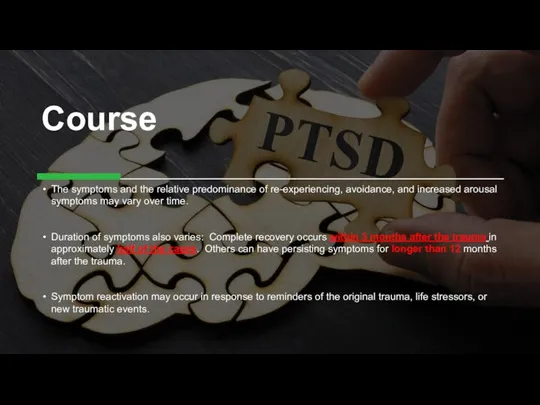
- 165. Course The symptoms and the relative predominance of re-experiencing, avoidance, and increased arousal symptoms may vary
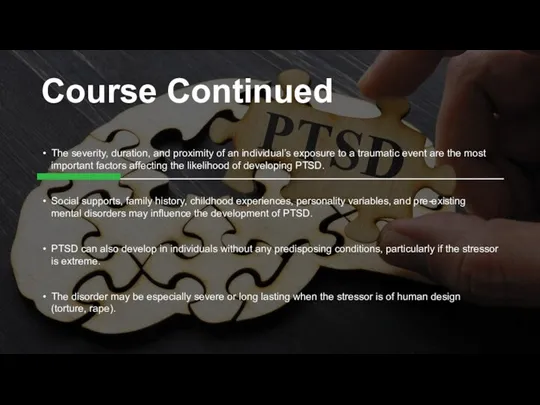
- 166. Course Continued The severity, duration, and proximity of an individual’s exposure to a traumatic event are
- 167. Course Continued Тяжесть, продолжительность и близость воздействия травматического события являются наиболее важными факторами, влияющими на вероятность
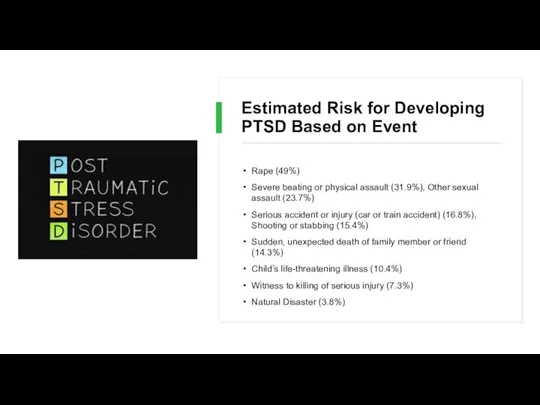
- 168. Estimated Risk for Developing PTSD Based on Event Rape (49%) Severe beating or physical assault (31.9%),
- 169. Differential Diagnosis Anxiety disorders Acute Stress Disorder Obsessive compulsive disorder Adjustment disorder Depressive disorders Substance Abuse
- 170. PTSD Compared to Other Disorders While the symptoms of posttraumatic stress disorder (PTSD) may seem similar
- 171. Differences between Acute Stress Disorder In general, the symptoms of acute stress disorder must occur within
- 172. Differences between PTSD and Obsessive-Compulsive Disorder Both have recurrent, intrusive thoughts as a symptom, but the
- 173. Differences Between PTSD and Adjustment Disorder PTSD symptoms can also seem similar to adjustment disorder because
- 174. Differences Between PTSD and Depression Depression after trauma and PTSD both may present numbing and avoidance
- 175. Who's more for it? Stressor Volume Sudden (Unexpected) Inability to control what is happening Sexual as
- 176. An adult's risk for psychological distress will increase as the number of the following factors increases:
- 177. An adult's risk for psychological distress will increase as the number of the following factors increases:
- 178. Why PTSD Victims Might Be Resistant to Getting Help Sometimes hard because people expect to be
- 179. Why PTSD Victims Might Be Resistant to Getting Help Потому что люди ожидают, что смогут справиться
- 180. During a Traumatic Event Norepinephrine- Mobilizing fear, the flight response, sympathetic activation, consolidating memory Too much
- 181. Treatment Individual Therapy Group Support (especially for Chronic PTSD) Medication
- 182. Treatment Continued For PTSD in children, adolescents, and geriatrics the preferred treatment is psychotherapy Acute PTSD
- 183. Treatment Continued Exposure Therapy- Education about common reactions to trauma, breathing retraining, and repeated exposure to
- 184. Treatment Continued Exposure Therapy- Объяснение об общих реакциях на травмы, обучение дыханию, и неоднократные обсуждения прошлых
- 185. Treatment Continued “Cognitive Restructuring involved teaching and reinforcing self-monitoring or thoughts and emotions, identifying automatic thoughts
- 186. Medications SSRIs – Sertraline, Paroxetine, Escitalopram, Fluvoxamine, Fluoxetine Affects the concentration and activity of the neurotransmitter
- 187. Medications Continued Tricyclic Antidepressants- Clomipramine , Doxepin, Nortriptyline, Amitriptyline, Maprotiline, Desipramine Affects concentration and activity of
- 188. Treatment With treatment, symptoms should improve after 3 months In Chronic PTSD cases, 1-2 years
- 189. Treatment Combination of antidepressant and anxiety medication In practice, you get to the whole spectrum of
- 190. Future Direction of Treatment Continued “Early Diagnosis and intervention- either psychotherapeutic or pharmacological- following trauma may
- 191. PTSD Myths PTSD is a complex disorder that often is misunderstood. Not everyone who experiences a
- 192. PTSD Myths MYTH: People should be able to move on with their lives after a traumatic
- 193. PTSD Myths Continued FACT: Many people who experience an extremely traumatic event go through an adjustment
- 194. PTSD Myths Continued FACT: Многие люди, которые испытывают чрезвычайно травматическое событие проходят через период адаптации после
- 195. PTSD Myths Continued MYTH: People suffer from PTSD right after they experience a traumatic event. FACT:
- 196. What is Prolonged Exposure? PE is a type of CBT, which is designed to specifically target
- 197. education about common reactions to trauma breathing retraining (or relaxation training) prolonged (repeated) exposure to trauma
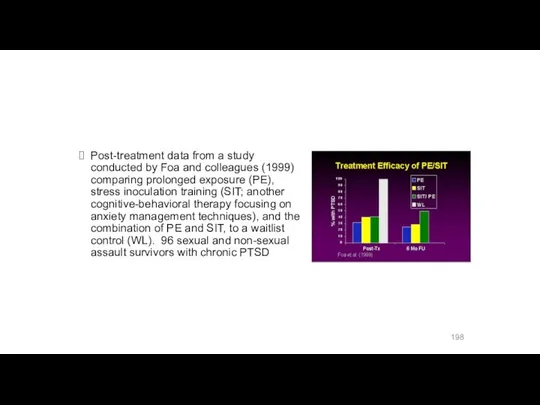
- 198. Post-treatment data from a study conducted by Foa and colleagues (1999) comparing prolonged exposure (PE), stress
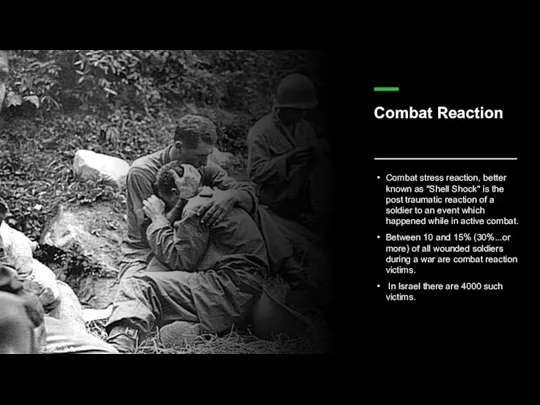
- 199. Combat Reaction Combat stress reaction, better known as "Shell Shock" is the post traumatic reaction of
- 200. The Background of Combat Reaction The transition from civilian life to military life is acute. The
- 201. The Background of Combat Reaction In wartime, a new and even more acute transition is added
- 202. The Background of Combat Reaction On the other hand, the soldier feels solidarity with his unit,
- 203. Risk Factors All the factors that influence the incidence of post-traumatic reactions in general, plus: Physical
- 204. Risk Factors Enforced passivity. When the soldier is deprived of activity and is in a state
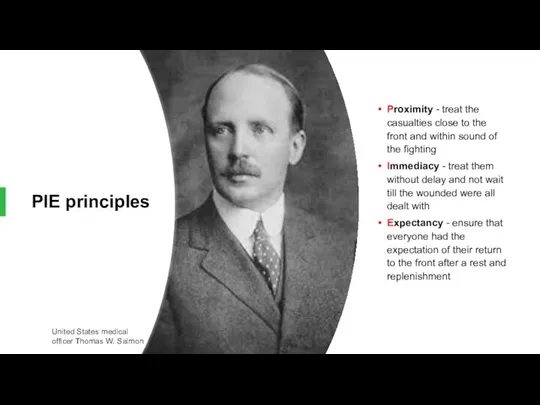
- 205. PIE principles Proximity - treat the casualties close to the front and within sound of the
- 206. The US services recently use BICEPS principles: Brevity Immediacy Centrality or Contact Expectancy Proximity Simplicity
- 207. The US services recently use BICEPS principles: Краткости (Brevity ) Непосредственности (Immediacy) Центральность или контакт (Centrality
- 208. Treatment results Data from the 1982 Lebanon war showed that with proximal treatment 90% of CSR
- 209. Controversy Throughout wars but notably during the Vietnam War there has been a conflict amongst doctors
- 210. Controversy На протяжении войн, но особенно во время войны во Вьетнаме, был конфликт между врачами об
- 211. Holocaust syndrome First generation Second generation
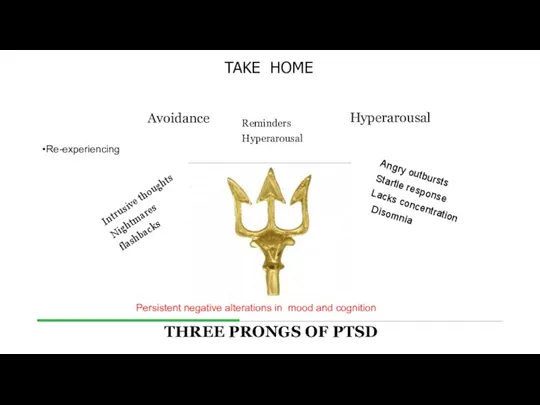
- 212. Re-experiencing Intrusive thoughts Nightmares flashbacks Avoidance Hyperarousal Reminders Hyperarousal Angry outbursts Startle response Lacks concentration Disomnia
- 214. Скачать презентацию












 ДА Ауруханаға дейінгі акушерлік гинекологиялық көмек көрсету. Жүктілерді диспансеризациялау. Жүктілік диагностикасы
ДА Ауруханаға дейінгі акушерлік гинекологиялық көмек көрсету. Жүктілерді диспансеризациялау. Жүктілік диагностикасы Синдром системной воспалительной реакции - SIRS
Синдром системной воспалительной реакции - SIRS Движение крови по сосудам. Отделы сосудистого русла. Основные параметры гемодинамики
Движение крови по сосудам. Отделы сосудистого русла. Основные параметры гемодинамики Наследственные заболевания
Наследственные заболевания Патология терморегуляции. Гипертермия и лихорадка. Стадии, виды, значение
Патология терморегуляции. Гипертермия и лихорадка. Стадии, виды, значение Психологические составляющие профессионального самоопределения личности
Психологические составляющие профессионального самоопределения личности Дорсопатиялар. Дорсопатия. Жалпы ұғым. Симптомдары және формалары
Дорсопатиялар. Дорсопатия. Жалпы ұғым. Симптомдары және формалары Гиповолемический шок
Гиповолемический шок Диетология. Измерения
Диетология. Измерения Cellexon®globa. Новые возможности в косметологии
Cellexon®globa. Новые возможности в косметологии Система гуморального иммунитета. Роль системы комплемента в иммунном ответе
Система гуморального иммунитета. Роль системы комплемента в иммунном ответе Онкологические заболевания челюстно-лицевой области
Онкологические заболевания челюстно-лицевой области Заболевания органов пищеварения у детей
Заболевания органов пищеварения у детей Физиология сосудов
Физиология сосудов Концепция развития медицинской науки до 2020 года в РК (организация проведения научных исследований в медицине)
Концепция развития медицинской науки до 2020 года в РК (организация проведения научных исследований в медицине) Туберкулез. Туберкулез бактериялары
Туберкулез. Туберкулез бактериялары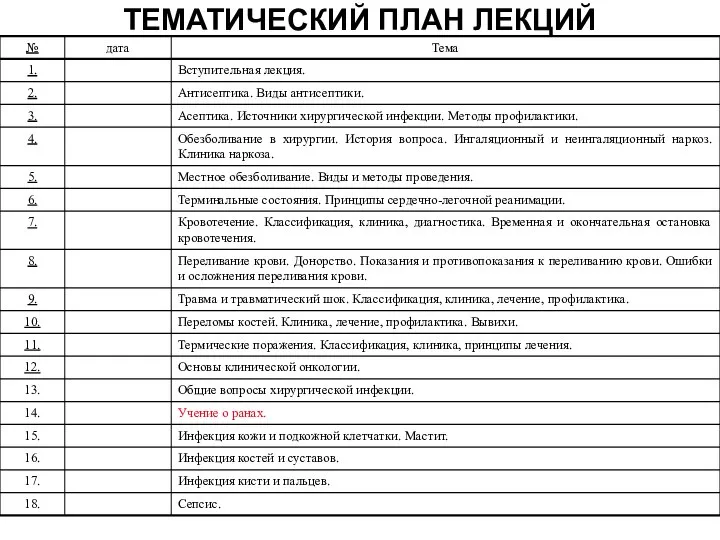 Раны. Раневой процесс
Раны. Раневой процесс Повышение качества диализной терапии
Повышение качества диализной терапии Основные синдромы в нефрологии
Основные синдромы в нефрологии Остеомиелит челюсти
Остеомиелит челюсти Существительные. Использование существительных в стандартных рецептурных формулировках
Существительные. Использование существительных в стандартных рецептурных формулировках Жүрек қан тамырлар жүйесіндегі герентологиялық өзгерістер
Жүрек қан тамырлар жүйесіндегі герентологиялық өзгерістер Духовное здоровье
Духовное здоровье Невролог – терапевту: различная этиология общих симптомов в практике двух специальностей. (Часть I)
Невролог – терапевту: различная этиология общих симптомов в практике двух специальностей. (Часть I) Патофизиология системы внешнего дыхания
Патофизиология системы внешнего дыхания Кремний. Симптомы недостатка и избытка кремния в организме
Кремний. Симптомы недостатка и избытка кремния в организме Бағаналы жасушалар
Бағаналы жасушалар Генные (точечные) мутации обмена веществ
Генные (точечные) мутации обмена веществ