Содержание
- 2. Atherosclerosis (athere – latin gruel) is a chronic disease which is characterized by formation of vascular
- 3. 1. Age (reducing of sex hormones synthesis and tissue regeneration, i.e. reducing of cholesterol consumption by
- 4. 1. Development of focal regions of chronic endothelial injury leading to increased vascular permeability and increased
- 5. 5. Adhesion of platelets to the focal areas of endothelial injury. 6. Release of biologically active
- 6. 8. Enhanced accumulation of lipids both within cells (macrophages and smooth muscle cells) and extracellularly. 9.
- 7. Aorta is usually the most involved vessel, the aortic lesions tend to be much more prominent
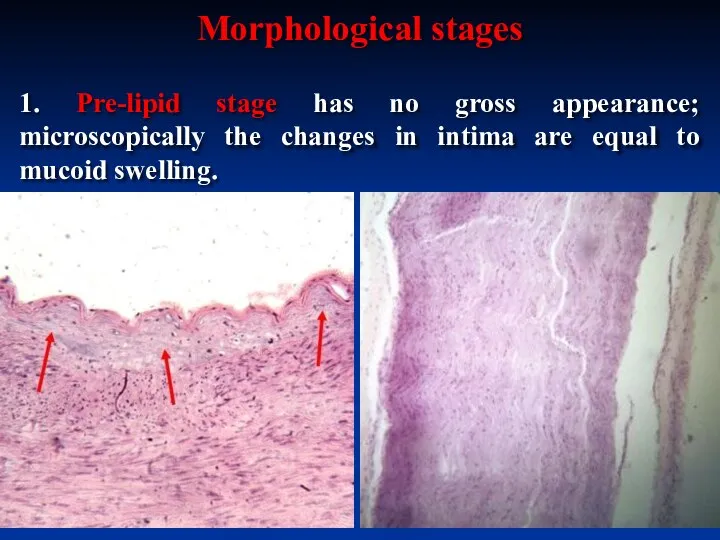
- 8. 1. Pre-lipid stage has no gross appearance; microscopically the changes in intima are equal to mucoid
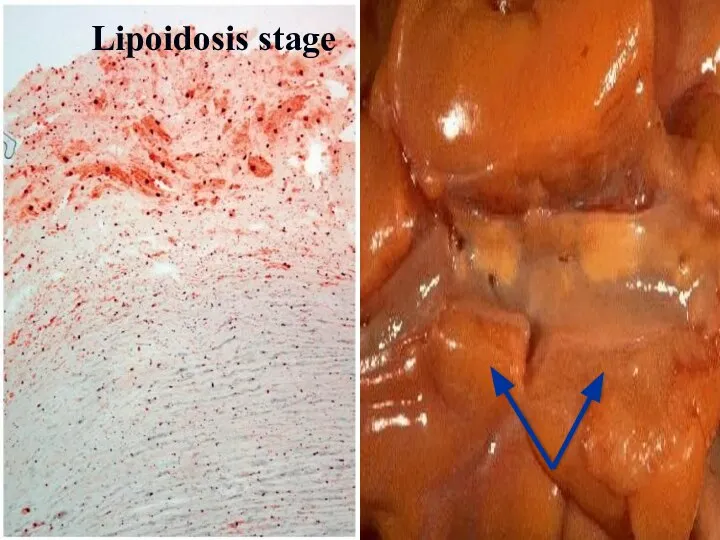
- 9. 2. In lipidosis stage the accumulation of lipids in the intima leads to formation of fatty
- 10. Atherosclerosis of aorta, lipidosis stage. Fatty streaks
- 11. Lipoidosis stage
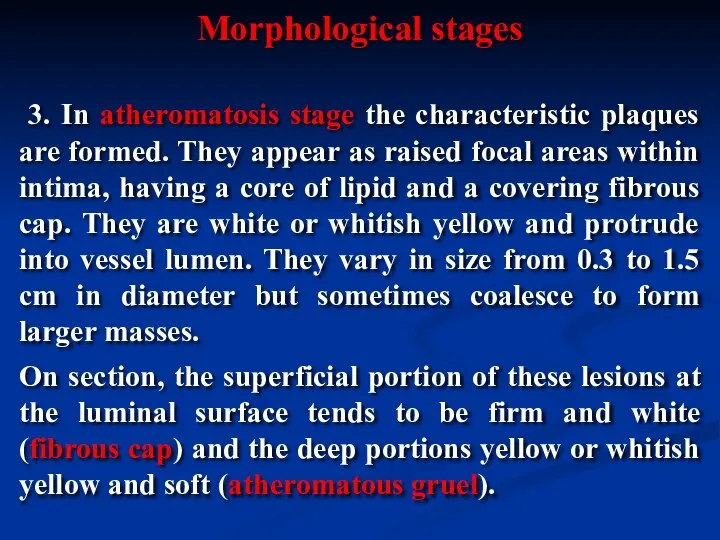
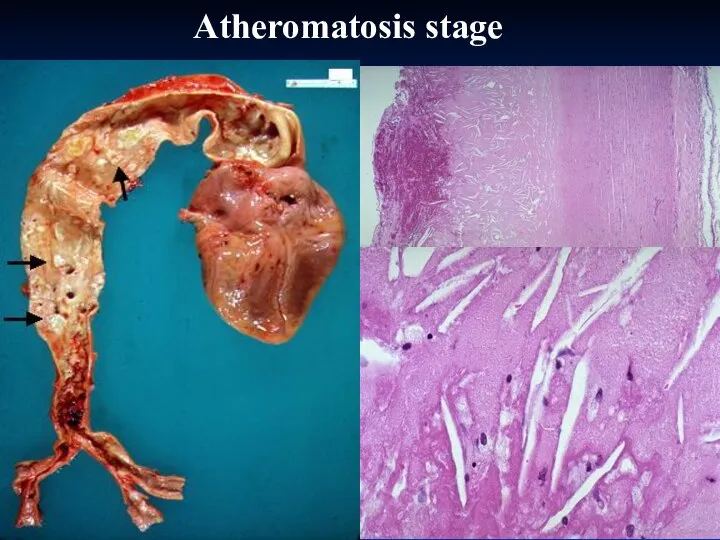
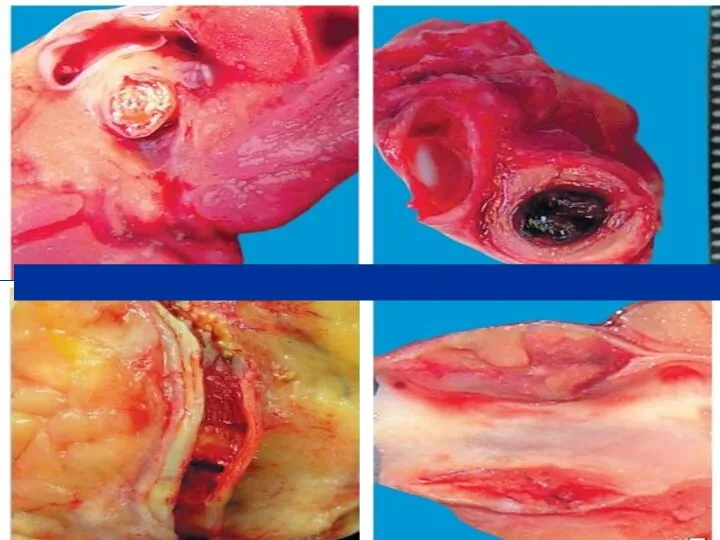
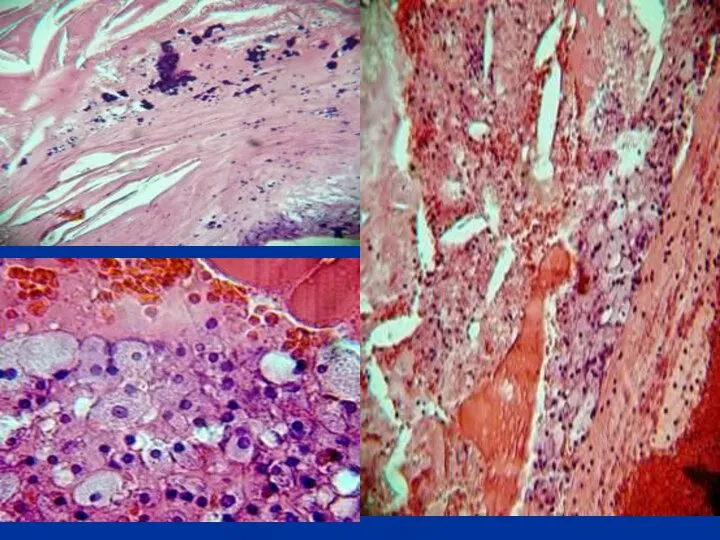
- 12. 3. In atheromatosis stage the characteristic plaques are formed. They appear as raised focal areas within
- 13. Atheromatosis stage
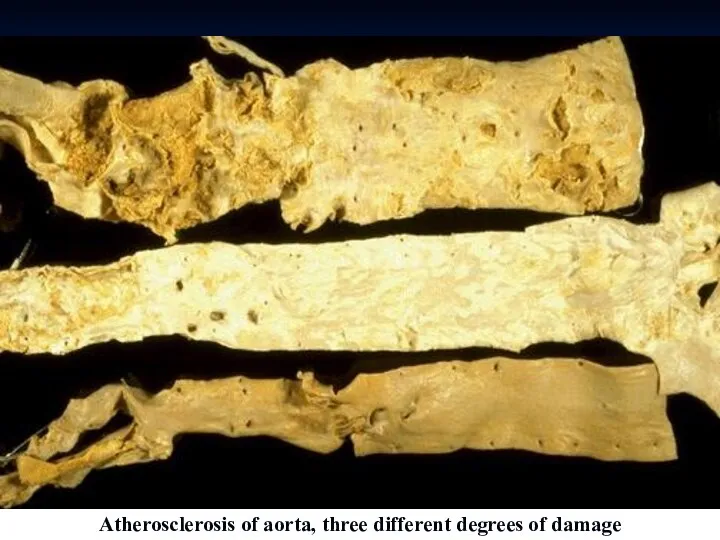
- 14. Atherosclerosis of aorta, three different degrees of damage
- 15. Atherosclerosis of coronary artery
- 16. АТЕРОСКЛЕРОЗ ВІНЦЕВИХ АРТЕРІЙ СЕРЦЯ
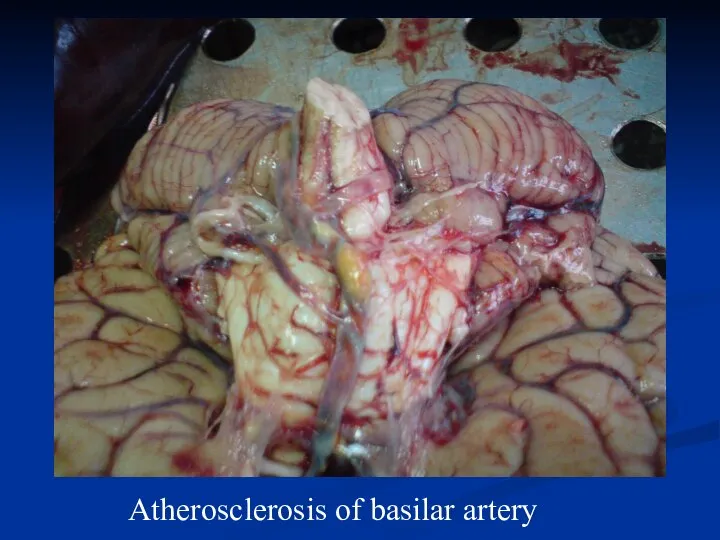
- 17. Atherosclerosis of basilar artery
- 18. Atheromatosis plague
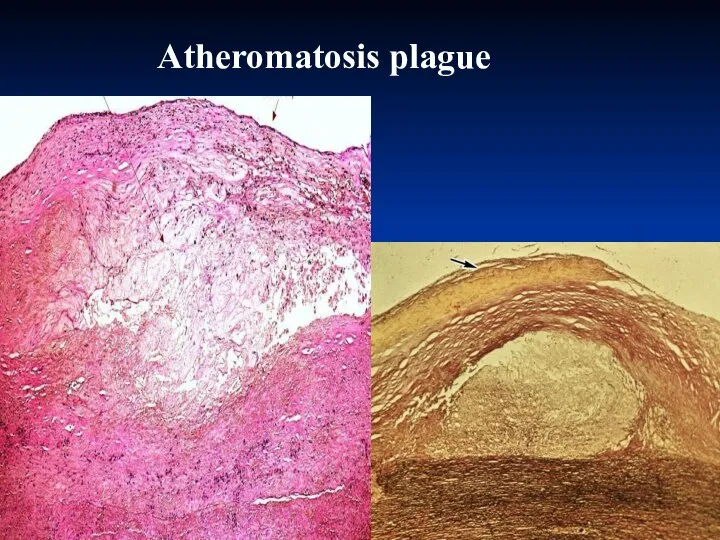
- 19. Atherosclerosis of coronary artery, 40 magnification, H&E stain
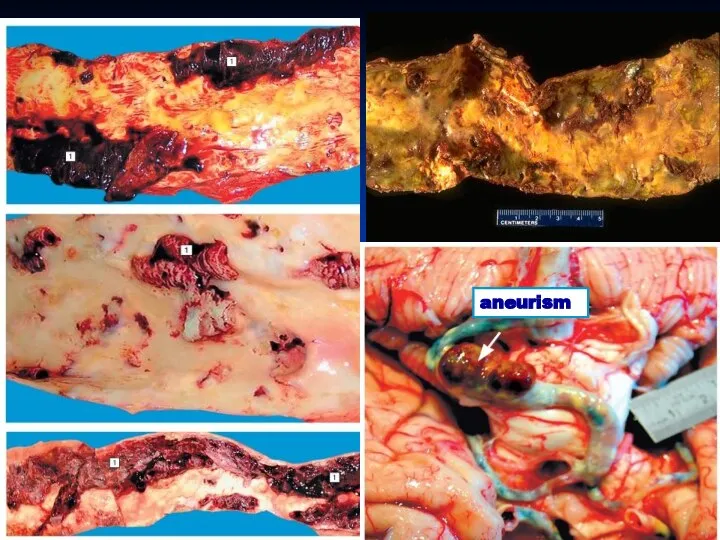
- 20. 4. Stage of complications. Atherosclerotic complications may be acute and chronic. It is believed that prominent
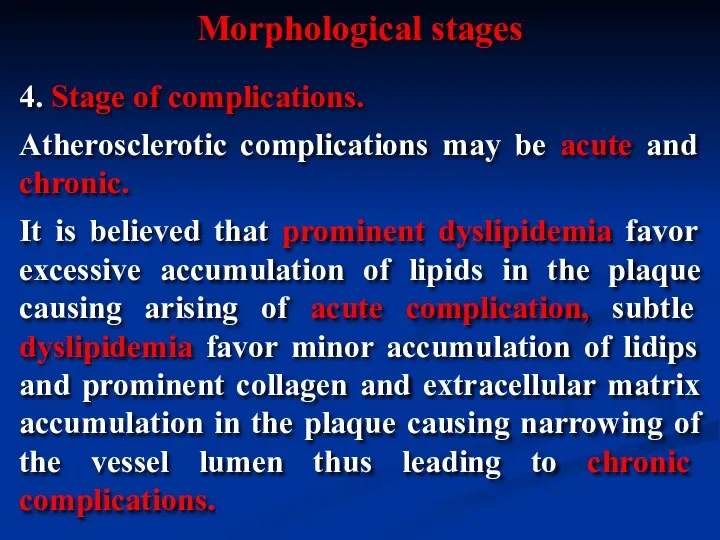
- 21. aneurism
- 23. 1. Focal rupture or gross ulceration, or both, of the luminal surface of atheromatous plaques may
- 24. 3. Superimposed thrombosis usually occurs on disrupted lesions (those with rupture, ulceration, erosion, or hemorrhage). Thrombi
- 25. Dry gangrene of foot Necrosis in heart wall
- 26. Gangrene of intestine
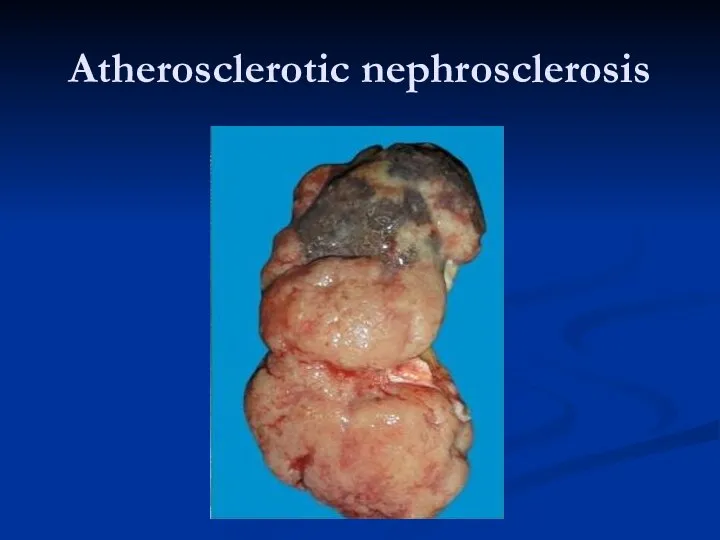
- 27. Atherosclerotic nephrosclеrosis
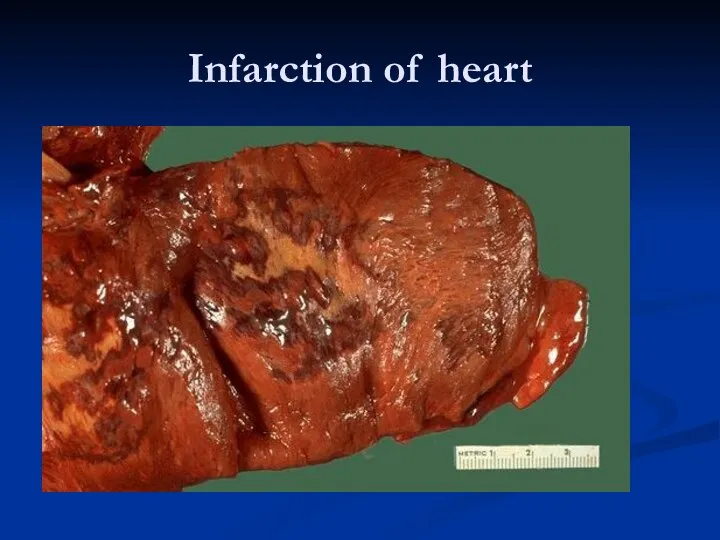
- 28. Infarction of heart
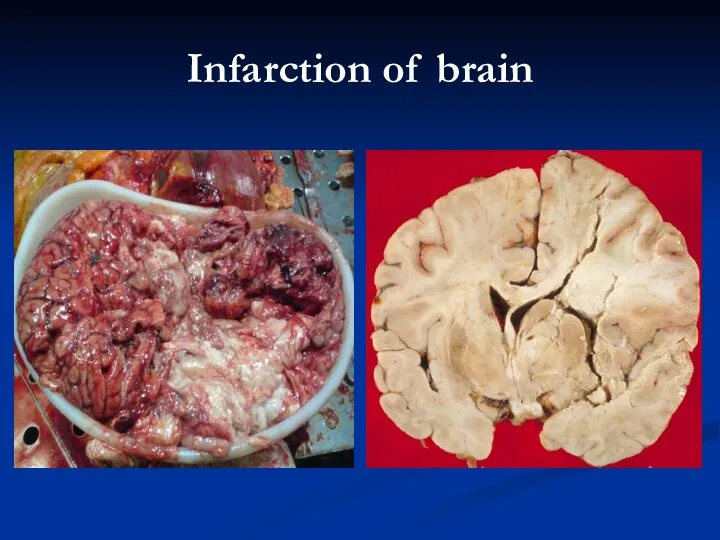
- 29. Infarction of brain
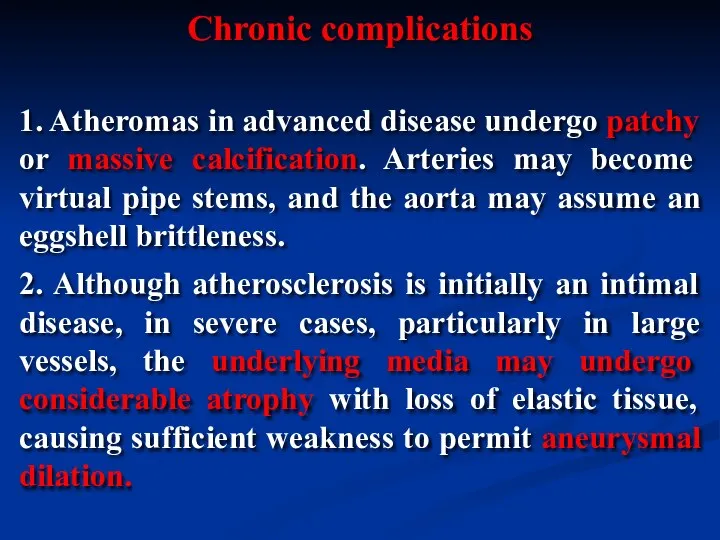
- 30. 1. Atheromas in advanced disease undergo patchy or massive calcification. Arteries may become virtual pipe stems,
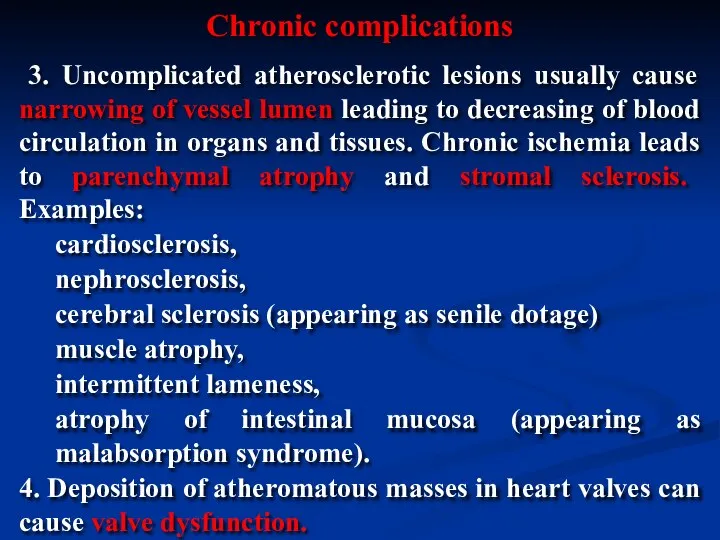
- 32. 3. Uncomplicated atherosclerotic lesions usually cause narrowing of vessel lumen leading to decreasing of blood circulation
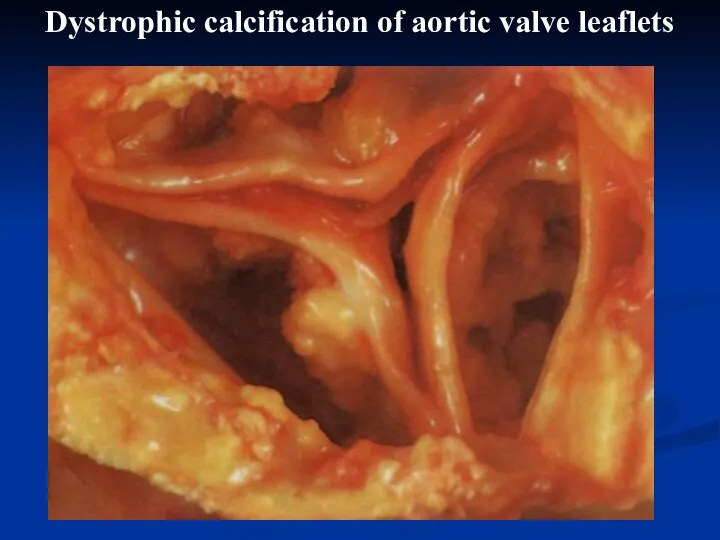
- 33. Dystrophic calcification of aortic valve leaflets
- 34. Hypertensive disease is a chronic disease which is characterized by chronic elevation of blood pressure that
- 35. Primary (idiopathic, essential) hypertension (90-95%): benign; malignant (or accelerated). Secondary hypertension that may be caused by:
- 36. 1. Age. 2. Environmental factors (e.g. frequent stresses, increased salt intake, increased estrogen level). 3. Genetic
- 37. In hypertensive disease both increased cardiac output and increased peripheral resistance due to constriction of vessel
- 38. In this stage there are periodical elevations of blood pressure. Morphologically this stage is characterized by
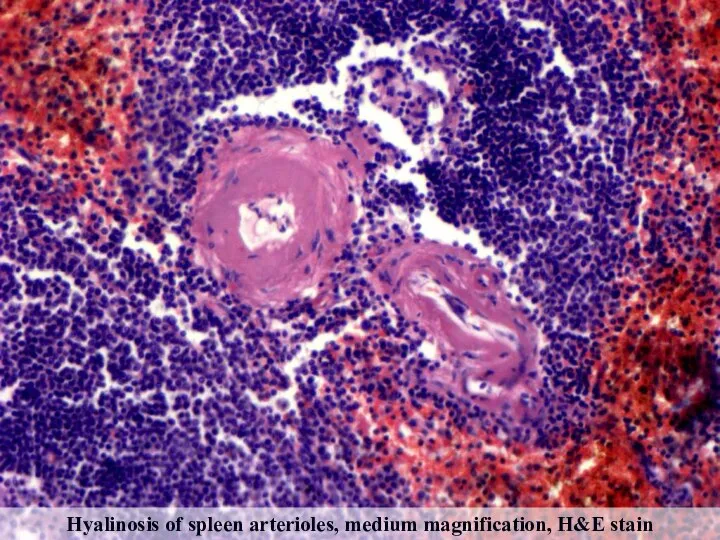
- 39. In benign hypertensive diseases the prolonged periods of arterioles constriction lead to narrowing of vessels, decreased
- 40. Hyalinosis of spleen arterioles, medium magnification, H&E stain
- 41. The muscular-elastic arteries firstly show adaptive changes – thickening and reduplication of the intimal elastic lamina
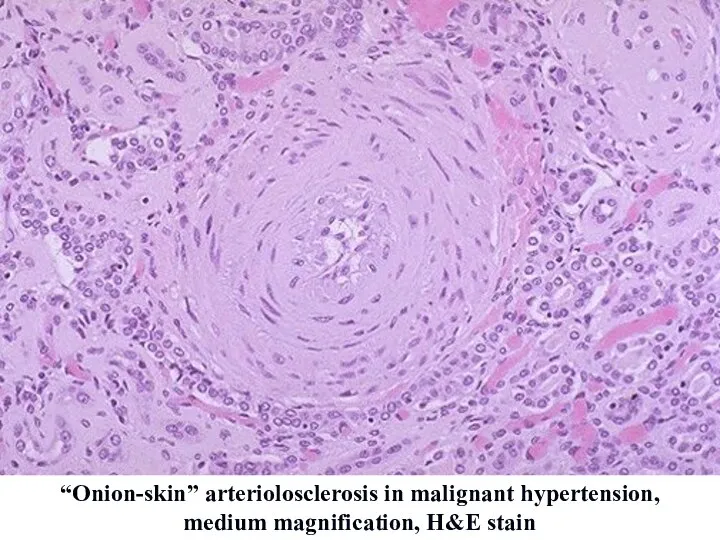
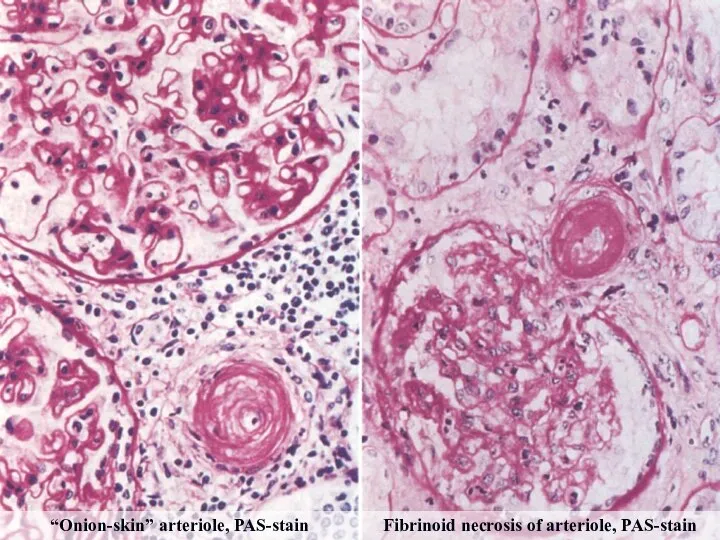
- 42. In malignant hypertension rapid and sharp elevation of blood pressure is caused by extremely severe vasoconstriction
- 43. “Onion-skin” arteriolosclerosis in malignant hypertension, medium magnification, H&E stain
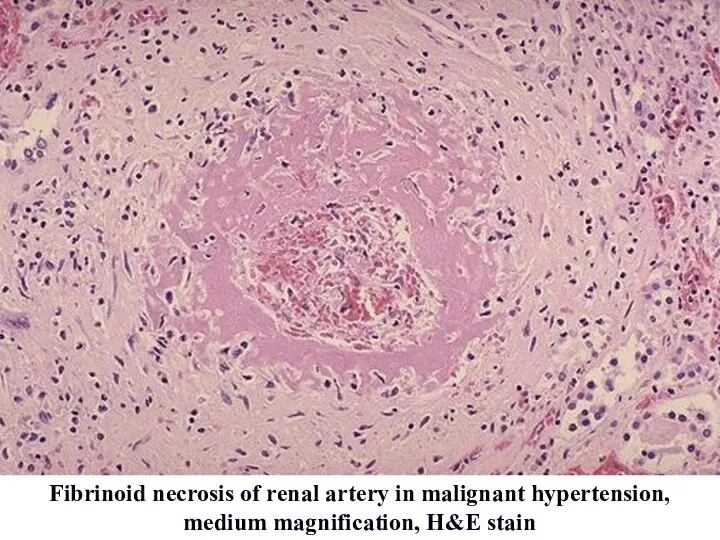
- 44. Fibrinoid necrosis of renal artery in malignant hypertension, medium magnification, H&E stain
- 45. “Onion-skin” arteriole, PAS-stain Fibrinoid necrosis of arteriole, PAS-stain
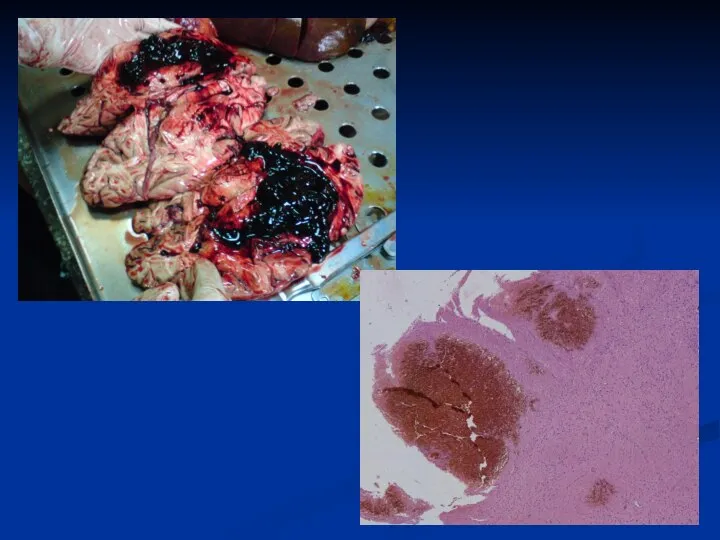
- 46. Acute complications: - infarction (myocardial, brain); - hemorrhages due to rupture of vessels affected with atherosclerosis).
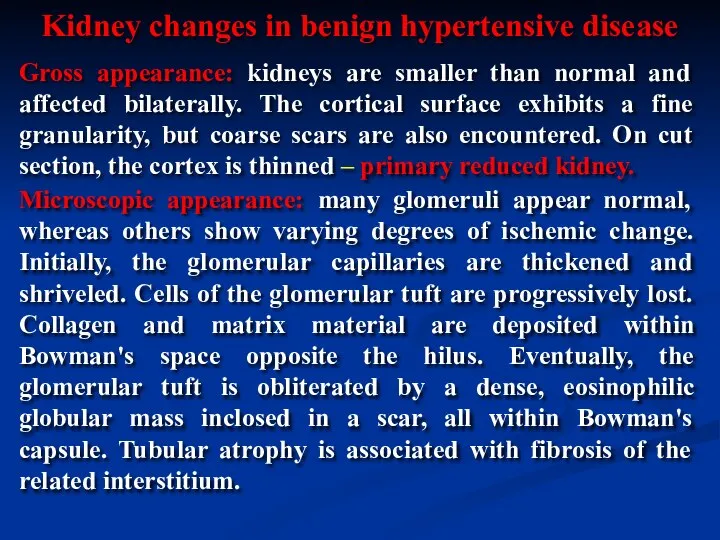
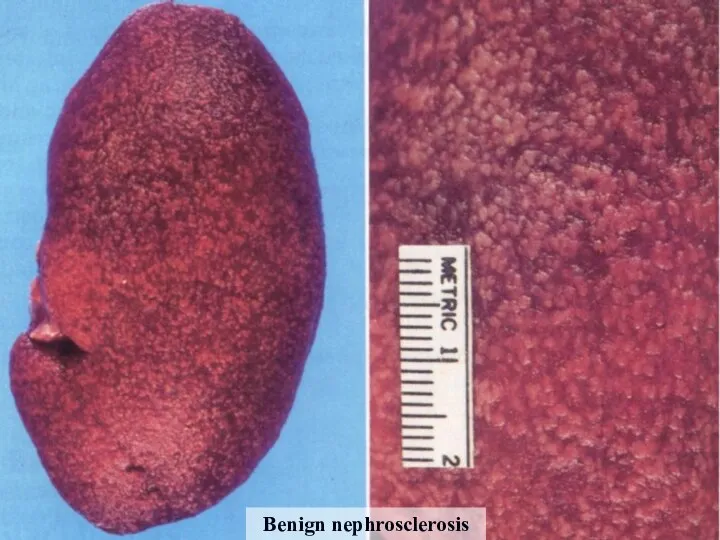
- 48. Gross appearance: kidneys are smaller than normal and affected bilaterally. The cortical surface exhibits a fine
- 49. Benign nephrosclerosis
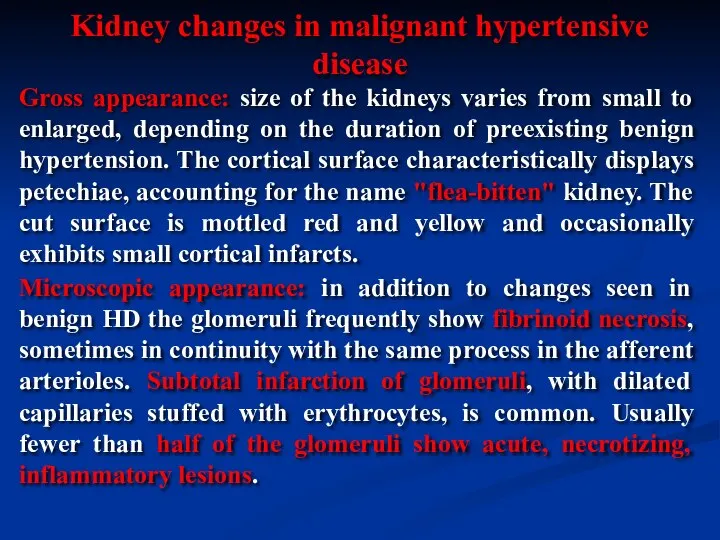
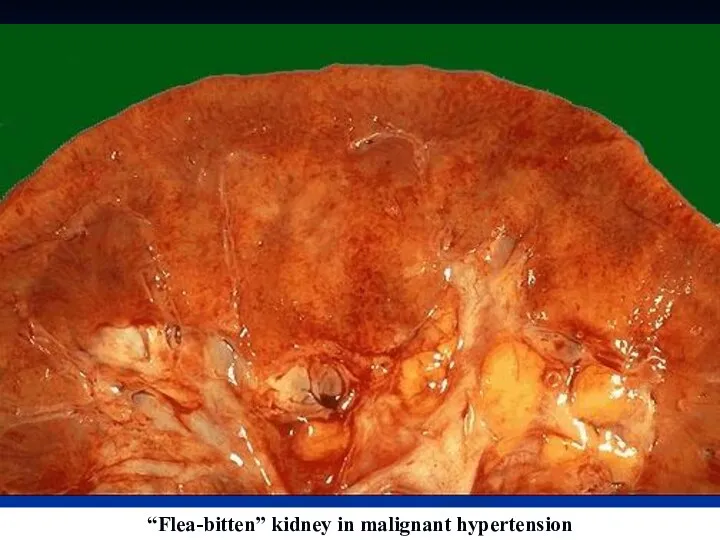
- 50. Gross appearance: size of the kidneys varies from small to enlarged, depending on the duration of
- 51. “Flea-bitten” kidney in malignant hypertension
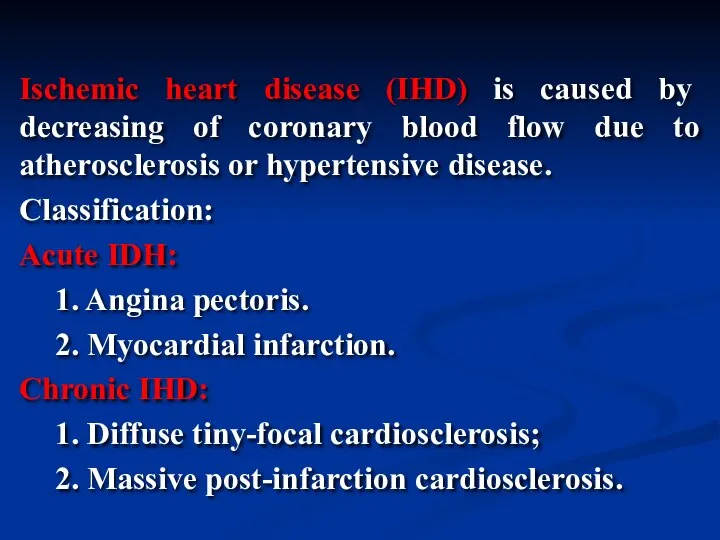
- 52. Ischemic heart disease (IHD) is caused by decreasing of coronary blood flow due to atherosclerosis or
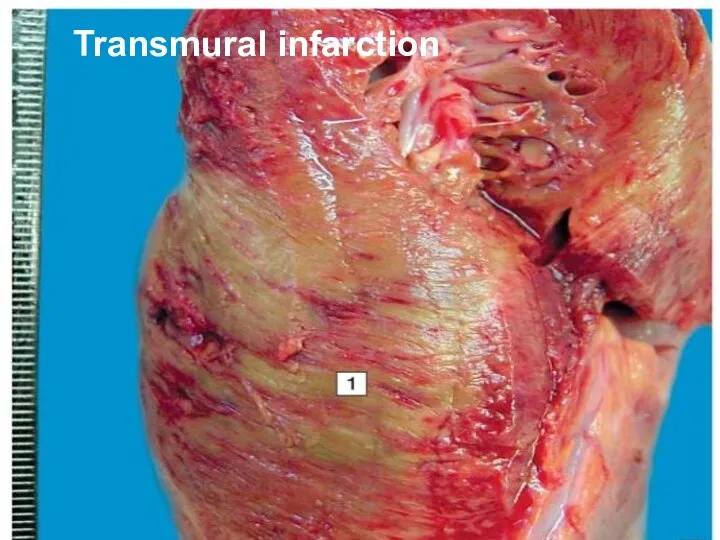
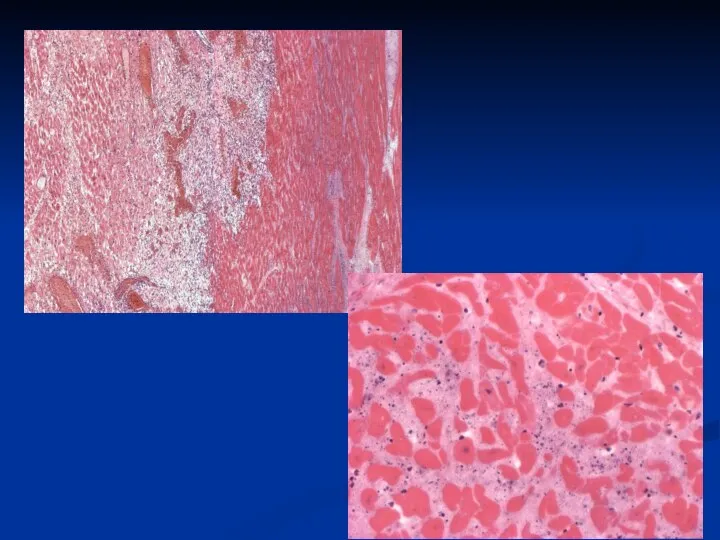
- 53. Transmural infarction
- 54. 18-24 hours ago
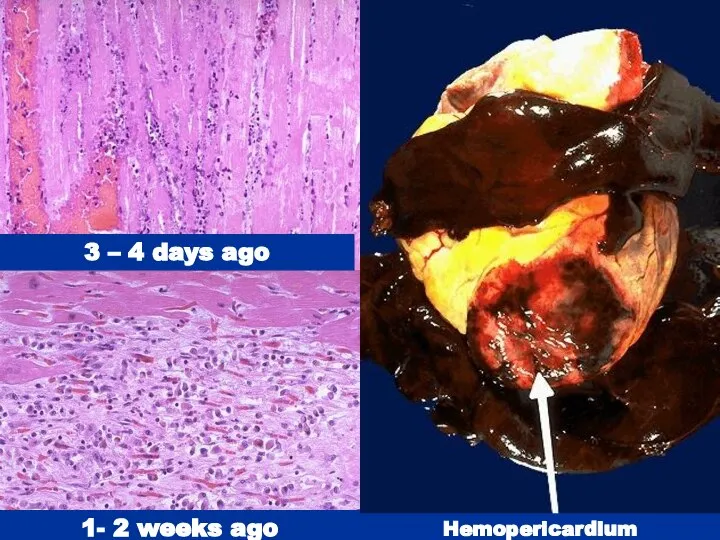
- 55. 3 – 4 days ago 1- 2 weeks ago Hemopericardium
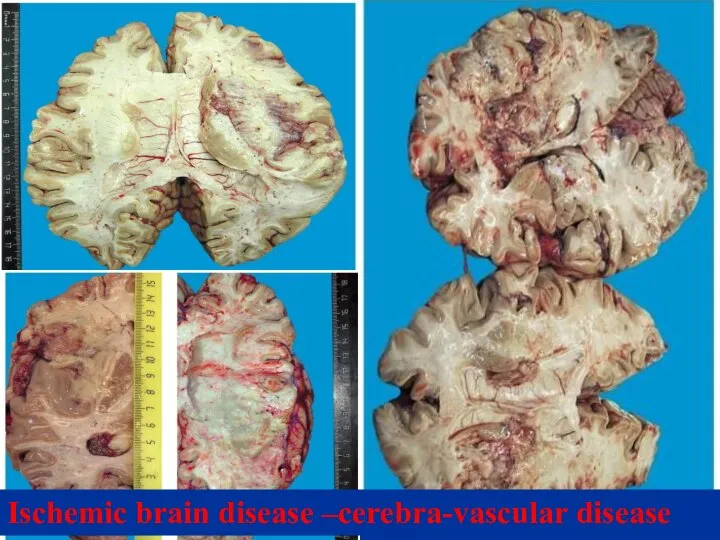
- 59. Ischemic brain disease –cerebra-vascular disease
- 61. Скачать презентацию









 "Акме" в професійному розвитку людини
"Акме" в професійному розвитку людини Нарушение гемостаза
Нарушение гемостаза Ингаляционная анестезия
Ингаляционная анестезия Рак толстого кишечника
Рак толстого кишечника Качества жизни в современной медицине
Качества жизни в современной медицине Каноны этических требований к моральному облику врача
Каноны этических требований к моральному облику врача Ишемический инсульт
Ишемический инсульт Эпикриз. Часть 2
Эпикриз. Часть 2 Основы рационального питания. Принципы формирования диет. Кормление пациента
Основы рационального питания. Принципы формирования диет. Кормление пациента Наркозные средства. Спирт этиловый
Наркозные средства. Спирт этиловый Человеческие зависимости
Человеческие зависимости Ғылым және ғылыми зерттеулер. Ғылым және олардың жіктеулері. Ғылыми зерттеулер және олардың мәні
Ғылым және ғылыми зерттеулер. Ғылым және олардың жіктеулері. Ғылыми зерттеулер және олардың мәні Адаптация. Степени тяжести адаптации
Адаптация. Степени тяжести адаптации Основные характеристики ВИЧ - инфекции
Основные характеристики ВИЧ - инфекции Функциональные заболевания желудочно-кишечного тракта у детей
Функциональные заболевания желудочно-кишечного тракта у детей СП при колитах
СП при колитах Роль рентгеновского излучения в медицине
Роль рентгеновского излучения в медицине Возрастные особенности строения и топографии лор-органов у взрослых
Возрастные особенности строения и топографии лор-органов у взрослых Герпетический энцефалит
Герпетический энцефалит Правильное питание и последствия его нарушения
Правильное питание и последствия его нарушения Антисекреторные препараты (ингибиторы протонной помпы, блокаторы гистаминовых Н2-рецепторов)
Антисекреторные препараты (ингибиторы протонной помпы, блокаторы гистаминовых Н2-рецепторов) Пороки сердца (продолжение). Лекция 2
Пороки сердца (продолжение). Лекция 2 История сердечно-сосудистой хирургии и интервенционной кардиоангиологии
История сердечно-сосудистой хирургии и интервенционной кардиоангиологии Современная инсулинотерапия
Современная инсулинотерапия Общие сведения о ядах и отравлениях (основы судебной токсикологии)
Общие сведения о ядах и отравлениях (основы судебной токсикологии) Здоровьесберегающие технологии в условиях загородного лагеря
Здоровьесберегающие технологии в условиях загородного лагеря Виды психокоррекционных групп
Виды психокоррекционных групп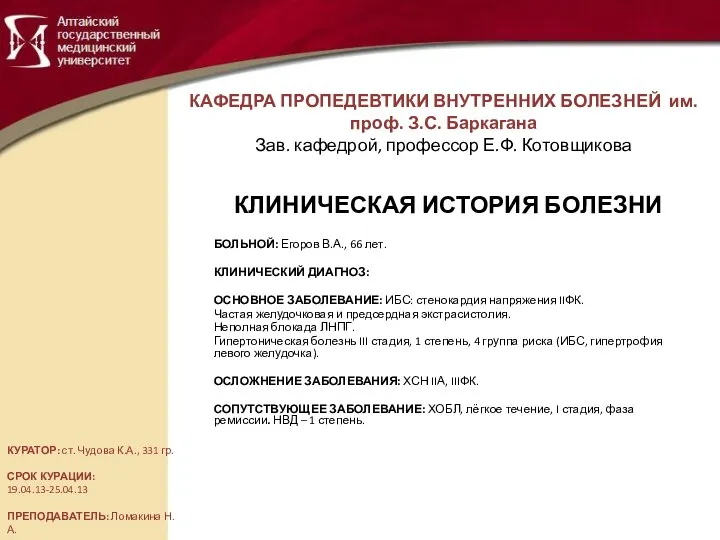 Клиническая история болезни
Клиническая история болезни