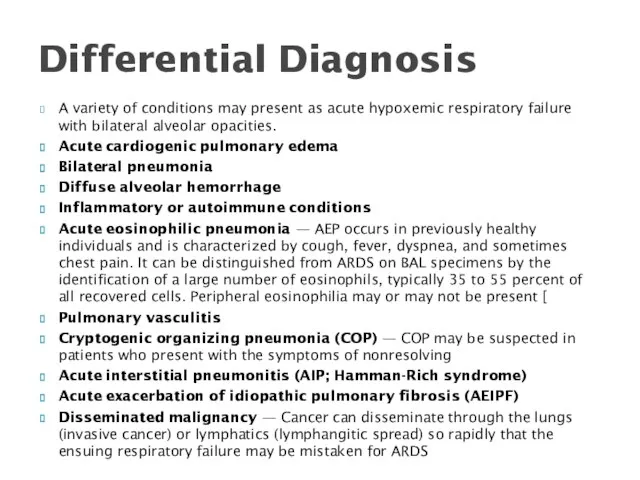
A variety of conditions may present as acute hypoxemic respiratory failure
with bilateral alveolar opacities.
Acute cardiogenic pulmonary edema
Bilateral pneumonia
Diffuse alveolar hemorrhage
Inflammatory or autoimmune conditions
Acute eosinophilic pneumonia — AEP occurs in previously healthy individuals and is characterized by cough, fever, dyspnea, and sometimes chest pain. It can be distinguished from ARDS on BAL specimens by the identification of a large number of eosinophils, typically 35 to 55 percent of all recovered cells. Peripheral eosinophilia may or may not be present [
Pulmonary vasculitis
Cryptogenic organizing pneumonia (COP) — COP may be suspected in patients who present with the symptoms of nonresolving
Acute interstitial pneumonitis (AIP; Hamman-Rich syndrome)
Acute exacerbation of idiopathic pulmonary fibrosis (AEIPF)
Disseminated malignancy — Cancer can disseminate through the lungs (invasive cancer) or lymphatics (lymphangitic spread) so rapidly that the ensuing respiratory failure may be mistaken for ARDS
Differential Diagnosis

 АИВ-инфекциясының терапиясы және алдын алуы
АИВ-инфекциясының терапиясы және алдын алуы Брюшина. Брюшная полость
Брюшина. Брюшная полость Отравление рыбой
Отравление рыбой Ступени развития любви к себе
Ступени развития любви к себе Цереброваскулярлы аурулар. Жіктелуі, патогенезі, жедел бас ми қан айналымының клиникасы
Цереброваскулярлы аурулар. Жіктелуі, патогенезі, жедел бас ми қан айналымының клиникасы Врожденные пороки сердца у детей
Врожденные пороки сердца у детей Патология щитовидной железы. Тиреотоксикоз
Патология щитовидной железы. Тиреотоксикоз Лекарства
Лекарства Preventive measures of neurological diseases
Preventive measures of neurological diseases Первая медицинская помощь при поражении электрическим током
Первая медицинская помощь при поражении электрическим током Тубулоинтерстициальные нефропатии
Тубулоинтерстициальные нефропатии Адамды клондаудың моральды мәселелері
Адамды клондаудың моральды мәселелері Temporary fillings
Temporary fillings Дети с нарушением речи
Дети с нарушением речи Мотивация. Успех любого намерения зависит от цели. Урок №2
Мотивация. Успех любого намерения зависит от цели. Урок №2 Периферическая нервная система. Спинномозговые нервы
Периферическая нервная система. Спинномозговые нервы Психосоматика
Психосоматика Хронические лимфопролиферативные заболевания
Хронические лимфопролиферативные заболевания Дезинфекция растворами, газами, аэрозолями
Дезинфекция растворами, газами, аэрозолями Особенности питания детей, нуждающихся в паллиативной медицинской помощи
Особенности питания детей, нуждающихся в паллиативной медицинской помощи Рецептура (receptum). Образец рецепта
Рецептура (receptum). Образец рецепта Логопедическая ритмика в системе коррекционно – речевой работы с детьми - дошкольниками
Логопедическая ритмика в системе коррекционно – речевой работы с детьми - дошкольниками Рациональное питание
Рациональное питание Сестринский уход при объемных процессах центральной нервной системы. Эпилепсия. Судорожный синдром
Сестринский уход при объемных процессах центральной нервной системы. Эпилепсия. Судорожный синдром Бактеріальні хвороби риб
Бактеріальні хвороби риб Глобальная регуляция экспрессии генов
Глобальная регуляция экспрессии генов Балалардағы мальабсорбция синдромы. Целиакия. Дисахаридазды жетіспеушілік. Экссудативті энтеропатия
Балалардағы мальабсорбция синдромы. Целиакия. Дисахаридазды жетіспеушілік. Экссудативті энтеропатия Культура питания. Примерные рекомендации пациентам по правильному питанию
Культура питания. Примерные рекомендации пациентам по правильному питанию