Содержание
- 2. Theoretical part Etiology Gonorrhoea is caused by the Gram-negative diplococci. Gonococci are lentil-shaped cocci about 1.5
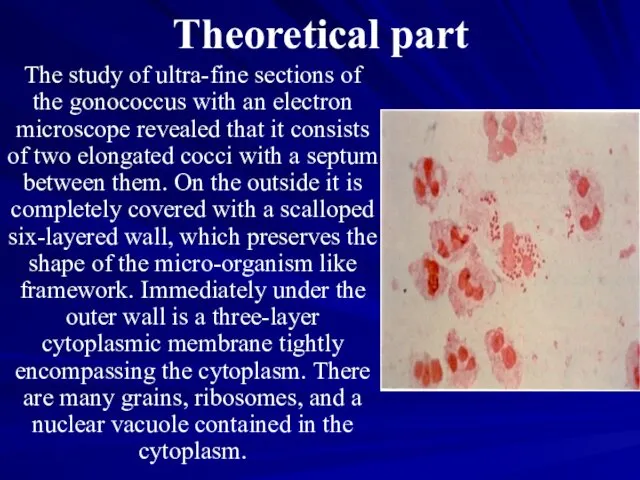
- 3. Theoretical part The study of ultra-fine sections of the gonococcus with an electron microscope revealed that
- 4. Transmission of the infection The basic way of transmission for males is normal sexual intercourse and
- 5. Pathogenesis Neither congenital, no acquired immunity to gonococcus develops in humans. The formed antibodies do not
- 6. Clinical features of gonorrhoea Present classification of gonorrhoea: Fresh: acute, subacute, torpid. Chronic.
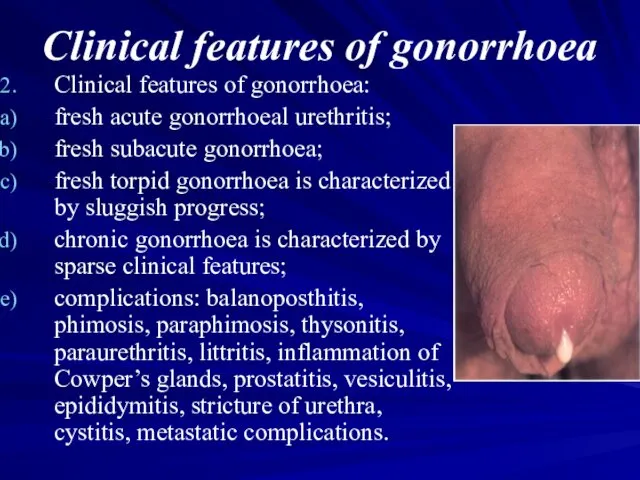
- 7. Clinical features of gonorrhoea Clinical features of gonorrhoea: fresh acute gonorrhoeal urethritis; fresh subacute gonorrhoea; fresh
- 8. Clinical features of gonorrhoea Gonorrhoea in small girls. As a result of anatomical and physiological peculiarities
- 9. Complications of gonorrhoeal urethritis in males. Acute gonorrhoeal urethritis, especially in males with a long and
- 10. Complications of gonorrhoeal urethritis in males. Abscess of the preputial gland is a rare local complication
- 11. Complications of gonorrhoeal urethritis in males. Littre's alveolar, tubular mucous glands and Morgagni's lacunae found in
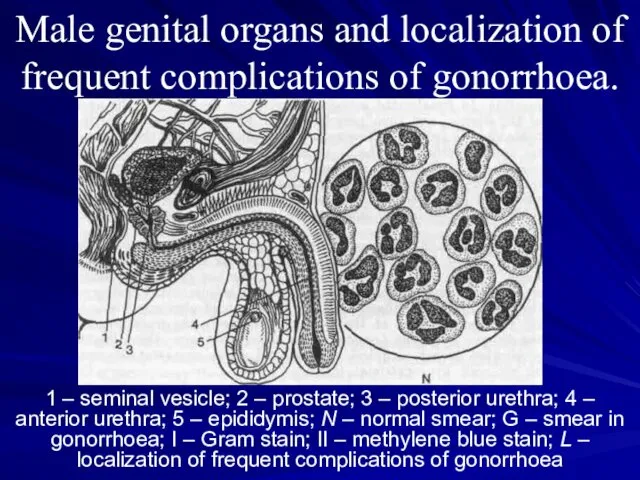
- 12. Male genital organs and localization of frequent complications of gonorrhoea. 1 – seminal vesicle; 2 –
- 13. Male genital organs and localization of frequent complications of gonorrhoea. Epididymitis, inflammation of the epididymis, was
- 14. Male genital organs and localization of frequent complications of gonorrhoea. Chronic prostatitis, on the contrary, is
- 15. Diagnosis of gonorrhoea The diagnosis of gonorrhoea may be established only when the causative agent has
- 16. Diagnosis of gonorrhoea In acute fresh gonorrhoea the causative agents are usually detected easily by microscopy
- 17. Diagnosis of gonorrhoea For the identification of gonococci by microscopy and in cultures, the pathological material
- 18. Treatment of gonorrhoea Gonorrhoea is managed by means of antigonococcal agents, methods for stimulating specific and
- 19. Non-gonorrhoeal venereal urethritis Venereal non-gonorrhoeal urethritis is found more often than gonorrhoeal; mostly accompanies gonorrhoea. Bacterial
- 20. Bacterial urethritis Pathogen: staphylococcus, diplococcus, streptococcus, E.coli, pseudo-diphtherial bacilli, enterococcus. Clinical features: incubation period is 5-10
- 21. Trichomonal urethritis Pathogen: Trichomonas vaginalis. Pathogenesis: reactive condition of the organism; accompanying diseases contribute to the
- 22. Mycotic urethritis At the beginning in most cases balanoposthitis develops and afterwards urethritis. Pathogen: yeast like
- 24. Скачать презентацию
 Оценка гемодинамической значимости желудочковой эктопии
Оценка гемодинамической значимости желудочковой эктопии Перекрут ножки опухоли яичника
Перекрут ножки опухоли яичника Анатомия и физиология как предмет. Краткий исторический очерк развития анатомии. Лекция №1. Часть 2
Анатомия и физиология как предмет. Краткий исторический очерк развития анатомии. Лекция №1. Часть 2 Лейкоцитозы, лейкопении
Лейкоцитозы, лейкопении Карбоновый пилинг
Карбоновый пилинг Распределение типов медицинских исследований
Распределение типов медицинских исследований Проявления действия яда на организм животных
Проявления действия яда на организм животных Лейкозы и лейкемойдные реакции. Раздел 2, тема 2.3
Лейкозы и лейкемойдные реакции. Раздел 2, тема 2.3 Заболевания желудка
Заболевания желудка Понятие «психологическая коррекция»
Понятие «психологическая коррекция» Современные технологии физиотерапии в реабилитации больных деформирующим остеоартрозом (остеоартритом)
Современные технологии физиотерапии в реабилитации больных деформирующим остеоартрозом (остеоартритом) Зерттеу әдістері. Гинекологиялық аурулардың пропедевтикасы
Зерттеу әдістері. Гинекологиялық аурулардың пропедевтикасы Гипергликемиялық кома
Гипергликемиялық кома Аортальный стеноз
Аортальный стеноз Методы исследования
Методы исследования Ситуационные задачи. Медицина и право
Ситуационные задачи. Медицина и право Средства влияющие на сердечно-сосудистую систему
Средства влияющие на сердечно-сосудистую систему Клинико-фармакологическая экспертиза. Ошибки и необоснованные назначения
Клинико-фармакологическая экспертиза. Ошибки и необоснованные назначения Гистологиялық препараттардың электрондық нұсқасы
Гистологиялық препараттардың электрондық нұсқасы ИБС. Стенокардия. Инфаркт миокарда
ИБС. Стенокардия. Инфаркт миокарда Мероприятия в очаге. Эпидемический паротит
Мероприятия в очаге. Эпидемический паротит Клиническая и инструментальная диагностика глиом
Клиническая и инструментальная диагностика глиом Психологическая подготовка к экзаменам
Психологическая подготовка к экзаменам Особенности развития психических расстройств у пораженного медицинского персонала и спасателей ЧС различного характера
Особенности развития психических расстройств у пораженного медицинского персонала и спасателей ЧС различного характера Женские половые гормоны
Женские половые гормоны Інфекційні захворювання
Інфекційні захворювання Симптомды жатыр миомасында жатыр артериясының эмболизациясы мен лапароскопиялық консервативті миомаэктомияның тиімділігі
Симптомды жатыр миомасында жатыр артериясының эмболизациясы мен лапароскопиялық консервативті миомаэктомияның тиімділігі Репаративные методы лечения болезней пародонта. Лекция 3
Репаративные методы лечения болезней пародонта. Лекция 3