Содержание
- 2. Allergy definition Type of hypersensitivity reactions of the immune system. may involve more than one type
- 3. Important factors Host factors; heredity, gender, race, and age. Environmental factor; infectious diseases during early childhood,
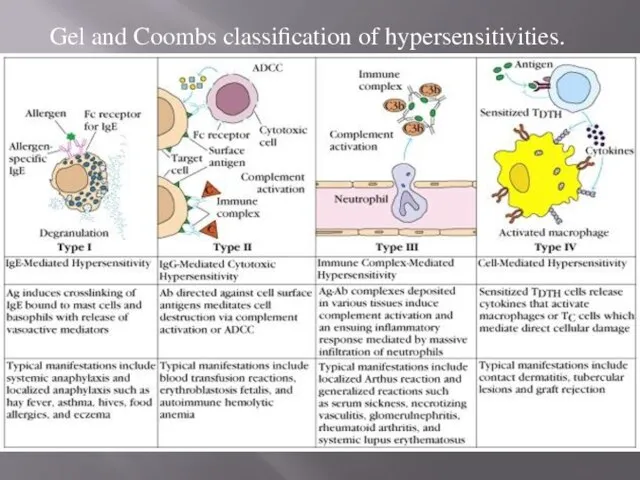
- 4. Gel and Coombs classification of hypersensitivities Type I -immediate hypersensitivity - IgE-mediated. Type II - antibody-dependent
- 5. Gel and Coombs classification of hypersensitivities.
- 6. Sell et al. classification Inactivation/activation antibody reactions Cytotoxic or cytolytic antibody reactions Immune-complex reactions Allergic reactions
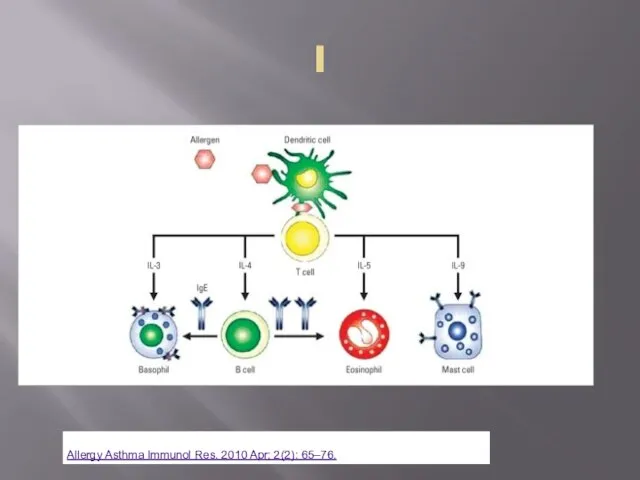
- 7. Pathogenesis Allegren processing and presenting peptides from allergens on MHCII class: dendritic cells in mucosal surface
- 8. I
- 9. Type I Antigen binds to IgE bound to tissue mast cells and blood basophils release of
- 10. Main mediators: Pre-existing Histamine (H1, H2 receptors): smooth muscles contraction in airways and GI, vasodilation and
- 11. Main mediators: newly synthesized Leucotriens: B4 (Neutrophils, vessels permeability); C4, D4 – bronchoconstriction, vessels permeability, arteriolar
- 12. Type II antibody-dependent cytotoxic hypersensitivity antibody binds to cell surface antigens or to a molecule coupled
- 13. Type III reactions (immune complex disease) circulating antigen-antibody immune complexes deposited in vessels or tissue. activate
- 14. Type IV reactions (delayed hypersensitivity) T cells, sensitized after contact with a specific antigen, are activated
- 15. Type I: Atopic and Allergic Disorders Allergy: is any abnormal immune response to a foreign antigen
- 16. Spectrum of atopic diseases Nose - allergic rhinitis Eyes - allergic conjunctivitis Skin: extrinsic atopic dermatitis,
- 17. Latex Sensitivity Abnormal immune response to water-soluble proteins in latex products (rubber gloves, dental dams, condoms,
- 18. Etiology: multifactorial Environment Genetic Site specific
- 19. Genetic: familial inheritance association between atopy and HLA loci (peptides promoting Th2 response). polymorphisms of genes:
- 20. Environmental factors: Allergens Proteins: serum, vaccines Pollen: rye grass, timothy grass, birch trees, ragweed and lots…
- 21. Environmental factors and Th2 reponce Environmental factors interact with genetic ones to maintain type 2 helper
- 22. Late exposure to indoor and outdoor environmental factors in infants early childhood exposure to bacterial and
- 23. Indian Journal of Allergy, Asthma and Immunology | Jan-Jun 2013 @BULLET Volume 27 @BULLET Issue 1
- 24. Site-specific factors adhesion molecules in bronchial epithelium/ skin molecules in the GI tract that direct TH2
- 25. Pathophysiology Mast cells are widely distributed but are most concentrated in skin, lungs, and GI mucosa
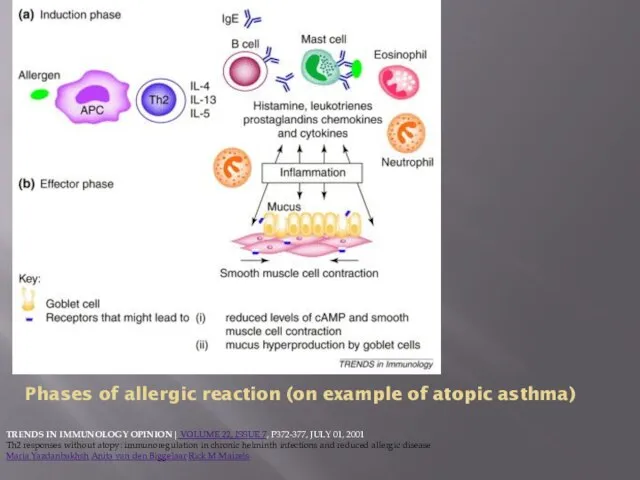
- 26. Phases of allergic reaction (on example of atopic asthma) TRENDS IN IMMUNOLOGY OPINION| VOLUME 22, ISSUE
- 27. Immediate Hypersensitivity Reactions Updated: Feb 09, 2015 Author: Becky Buelow, MD, MS; Chief Editor: Michael A
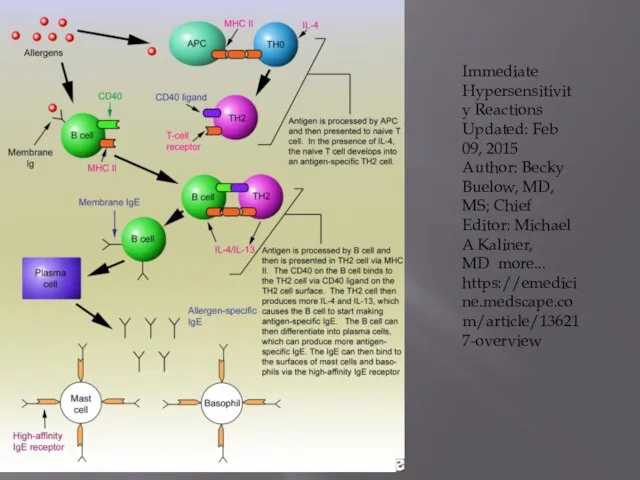
- 28. Other than histamin mediators pre-formed in mast cells granules Cytokines TNF-α, IL-1, IL-6. Chemoattractants for Neutrophils
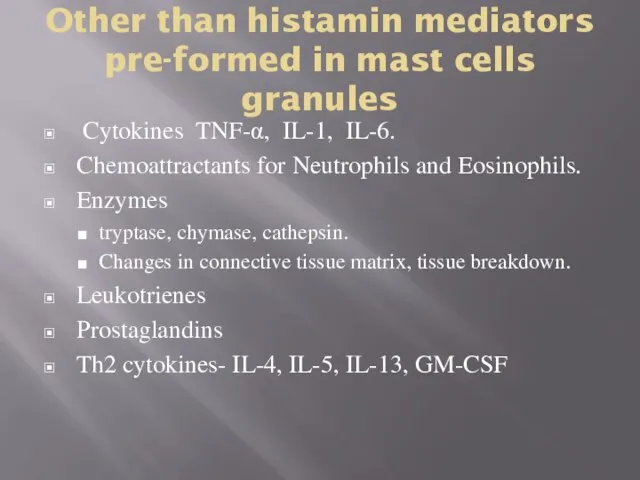
- 29. Histamine effects Local vasodilation (causing erythema) Increased capillary permeability and edema (producing a wheal) Vasodilation of
- 30. Frequent histamine release: potent arteriolar dilator causes extensive peripheral pooling of blood and hypotension cerebral vasodilation
- 31. Non-specific/non-allergic histamin liberation physical disruption of tissue and various substances (tissue irritants, opiates, surface-active agents, complement
- 32. Continuation of sensitization cycle Eosinophils Eosinophils play key role in late phase reaction. Eosinophils make enzymes,
- 33. Types of allergens Pollen Dust Epidermal Food Drugs Insect – venom, cocroaches etc Latex
- 34. Pollen Canada (shortened) Moote, W., Kim, H. Allergen-specific immunotherapy. All Asth Clin Immun 7, S5 (2011).
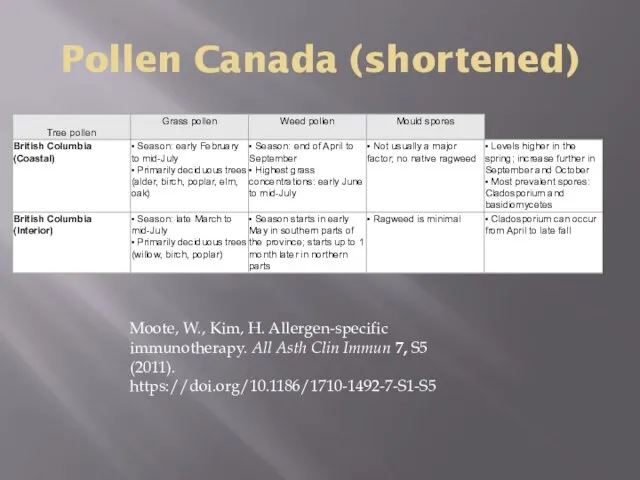
- 35. Common symptoms upper respiratory tract: rhinorrhea, sneezing, and nasal congestion, itching, nasal turbinate edema, sinus pain
- 36. Diagnosis Clinical evaluation CBC serum IgE levels skin testing and allergen-specific serum IgE testing (specific tests)
- 37. Clinical evaluation frequency and duration of attacks and changes over time Identification of triggering factors Relation
- 38. Allergologic anamnesis 1. Allergic diseases in case history: asthma, pollinosis, urticaria, quincjedema, migraine, exema, allertic rhinitis,
- 39. 5. Drug reaction (what/when) ; anaphylactic shock, urticaria, quickedema, bronchospasm, dermatites of different types, itching, allergic
- 40. 6. seasonal exacerbations (summer, autumn, winter, spring) 7. climate influence on the disease course 8. weather
- 41. 12. where is worse – at home, at the working place, in the street, in the
- 42. Non-specific tests CBC: eosinophilia (except patients taking corticosteroids); normal eosinophil count does not exclude allergy. Total
- 43. Specific tests: Allergen-specific serum IgE tests: enzyme-labeled anti-IgE antibody Performed when skin testing might be ineffective
- 44. Skin tests standardized concentrations of antigen introduced directly into skin higher positive predictive values for diagnosing
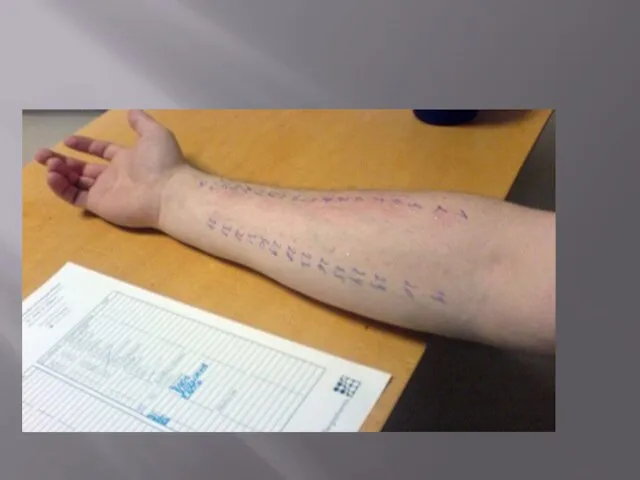
- 45. Two skin test techniques can be used: Percutaneous (prick) Intradermal
- 46. Percutaneous (prick): drop of antigen extract is placed on the skin skin is tented up and
- 47. Intradermal more sensitive less specific can be used to evaluate sensitivity to allergens when prick test
- 48. Necessary for both Negative control: diluent Positive control - histamine (10 mg/mL for prick tests, 0.01
- 49. Drugs which can interfere with results and should be be stopped a few days to a
- 50. Positive test results Diluent – negative Histamin - positive Causative allergen: positive Postive means wheal and
- 51. Negative test result Diluent – negative Histamin - positive Causative allergen: negative Skin reacts on histamin
- 52. False positive Diluent – positive Histamine – positive Allergen - positive Cause may be dermatographism (a
- 53. False negative Diluent – negative Histamine – negative Allergen - negative If used from one kit
- 54. False negative-2 Histamine is positive, allergens are negative, but there is strong evidence of allergy histamine
- 55. Individual allergens Concrete house dust taken from patients home Epidermis of the concrete cat, dog etc
- 57. Other specific tests Provocative testing : exposure of the mucosae to allergen and is indicated for
- 58. Treatment Removal or avoidance of allergic triggers H1 blockers Mast cell stabilizers Anti-inflammatory corticosteroids and leukotriene
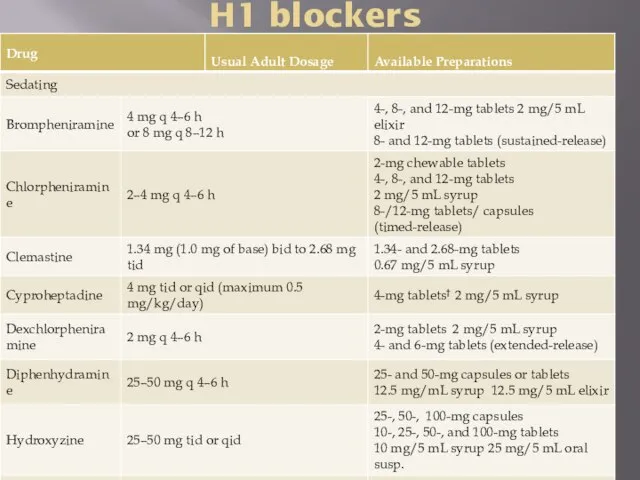
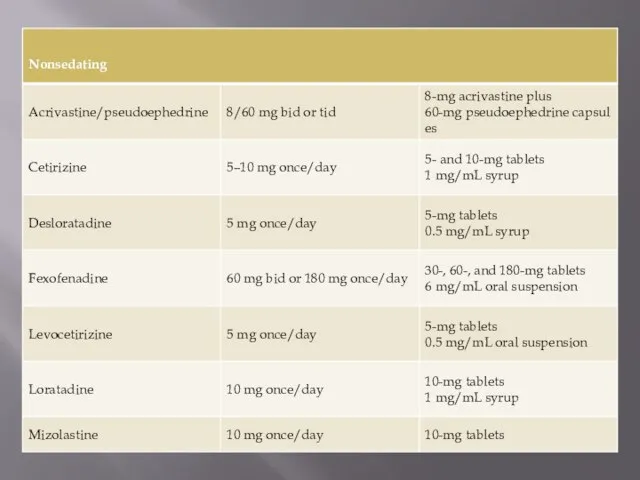
- 59. H1 blockers
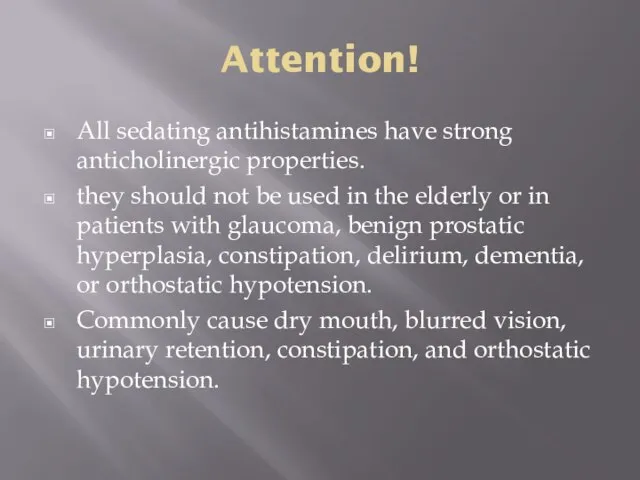
- 61. Attention! All sedating antihistamines have strong anticholinergic properties. they should not be used in the elderly
- 62. Specific immune therapy Performed in remission only In period without allergens exposure (not in pollen exposure
- 63. Indications allergic rhinitis, conjunctivitis, hay fever, atopic asthma of mild course of the disease (all with
- 64. Contraindications: 3-5 step of asthma treatment (moderate/severe course) Non Th2-variant (non-atopic, low IgE) Current use of
- 65. Special considerations: • Children
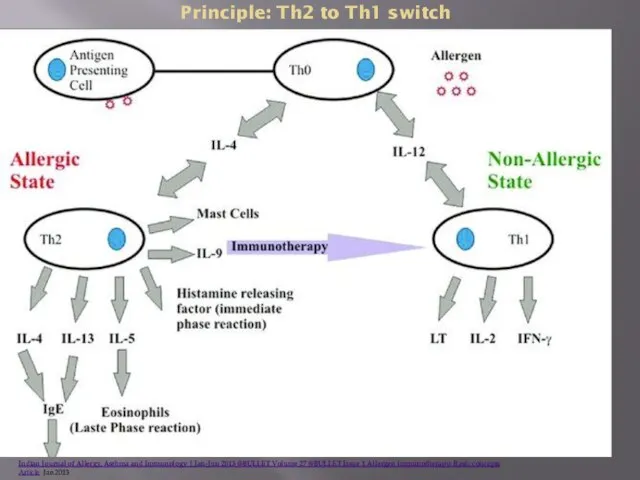
- 66. Principle induction of IgG antibodies IgGs compete with IgE for allergen or block IgE from binding
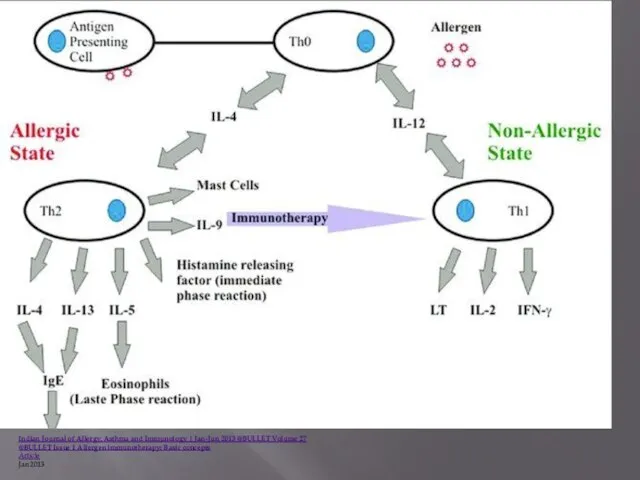
- 67. Principle: Th2 to Th1 switch Indian Journal of Allergy, Asthma and Immunology | Jan-Jun 2013 @BULLET
- 68. Classification Preseasonal Preseasonal-seasonal Whole year
- 69. Principle injections are given monthly. Dose: start dose from 0.1 to 1.0 biologically active units (BAU),
- 70. Build-up (induction) phase weekly injections starting with a very low dose, gradual increases in dose over
- 71. maintenance phase every 4–6 weeks for venom and every 4 weeks for inhalant allergens period of
- 72. Principle Observation of patients 30 min postinjection (risk of anaphylaxy) Appearance of blood during injectionis the
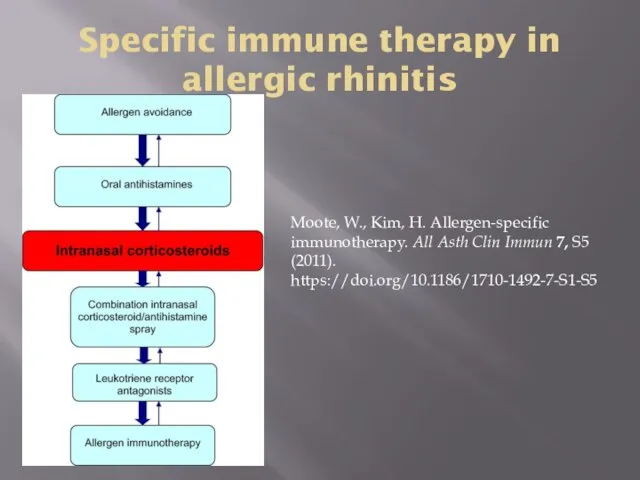
- 73. Specific immune therapy in allergic rhinitis Moote, W., Kim, H. Allergen-specific immunotherapy. All Asth Clin Immun
- 74. Sublingual immunotherapy placing a tablet of allergen extract under the tongue until it is dissolved available
- 75. Prevention synthetic fiber pillows and impermeable mattress covers Frequently washing bed sheets, pillowcases, and blankets in
- 76. Food allergy Some food antigens stimulate innate immune responses peanut allergen Ara h1 binds to CD209
- 78. Скачать презентацию
 Синтетические лекарственные средства
Синтетические лекарственные средства Болезнь Бехтерева
Болезнь Бехтерева Медикаментозное лечение в сестринской практике
Медикаментозное лечение в сестринской практике Вспомогательные материалы в зубопротезировании. Классификация вспомогательных материалов. Воски и абразивы
Вспомогательные материалы в зубопротезировании. Классификация вспомогательных материалов. Воски и абразивы Дені сау нәрестеге үйде патронаж жасап амбулаториялық оқу картасын толтыру
Дені сау нәрестеге үйде патронаж жасап амбулаториялық оқу картасын толтыру Первая помощь при обморожении
Первая помощь при обморожении Заболевания органов пищеварения
Заболевания органов пищеварения Тактика персонала при легочном кровотечении
Тактика персонала при легочном кровотечении Группы расстройств кровообращения
Группы расстройств кровообращения Эмболия околоплодными водами
Эмболия околоплодными водами Спелеотерапия. Физиологическое и лечебное действие. Показания и противопоказания к терапии
Спелеотерапия. Физиологическое и лечебное действие. Показания и противопоказания к терапии Бюджетирование в здравоохранении
Бюджетирование в здравоохранении Сердечно-легочная и церебральная реанимация
Сердечно-легочная и церебральная реанимация Diphtheria
Diphtheria Тромбоз. Что это такое?
Тромбоз. Что это такое? Халықты халықпен, адамды адаммен теңестіретін - білім. М.Әуезов
Халықты халықпен, адамды адаммен теңестіретін - білім. М.Әуезов Акушерские кровотечения в родах и послеродовом периоде. Тема 3
Акушерские кровотечения в родах и послеродовом периоде. Тема 3 مفهوم درد وتسکین درد
مفهوم درد وتسکین درد Choroby alergiczne
Choroby alergiczne Рак легкого
Рак легкого Бихевиоризм (от английского Behavior - поведение)
Бихевиоризм (от английского Behavior - поведение) Медико-биологические и социальные основы здоровья
Медико-биологические и социальные основы здоровья Восприятие. Виды восприятия
Восприятие. Виды восприятия Психикалық және наркологиялық науқастарға жүргізілетін экспертиза түрлері
Психикалық және наркологиялық науқастарға жүргізілетін экспертиза түрлері Рекомендуемые препараты для лечения гипоманиии в остром периоде
Рекомендуемые препараты для лечения гипоманиии в остром периоде Ишемическая болезнь сердца. Этиология,патогенез, классификация, клинические формы. Стенокардия. Клиника, диагностика, лечение
Ишемическая болезнь сердца. Этиология,патогенез, классификация, клинические формы. Стенокардия. Клиника, диагностика, лечение Осложнения инфаркта миокарда
Осложнения инфаркта миокарда Память
Память