Содержание
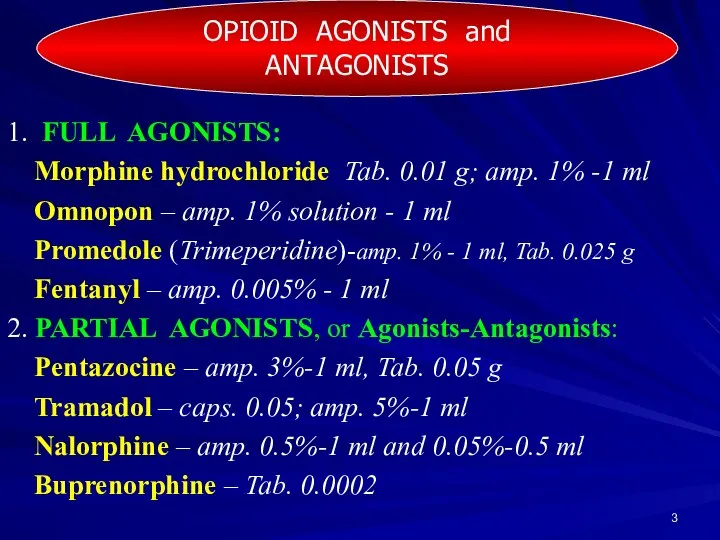
- 3. 1. FULL AGONISTS: Morphine hydrochloride Tab. 0.01 g; amp. 1% -1 ml Omnopon – amp. 1%
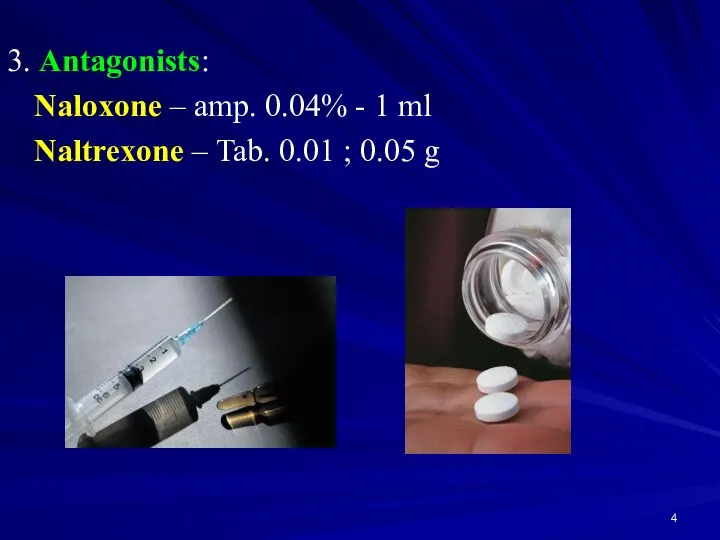
- 4. 3. Antagonists: Naloxone – amp. 0.04% - 1 ml Naltrexone – Tab. 0.01 ; 0.05 g
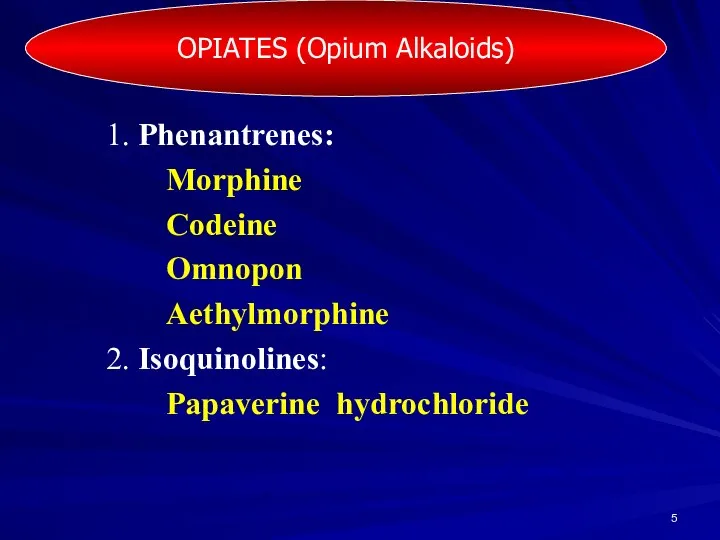
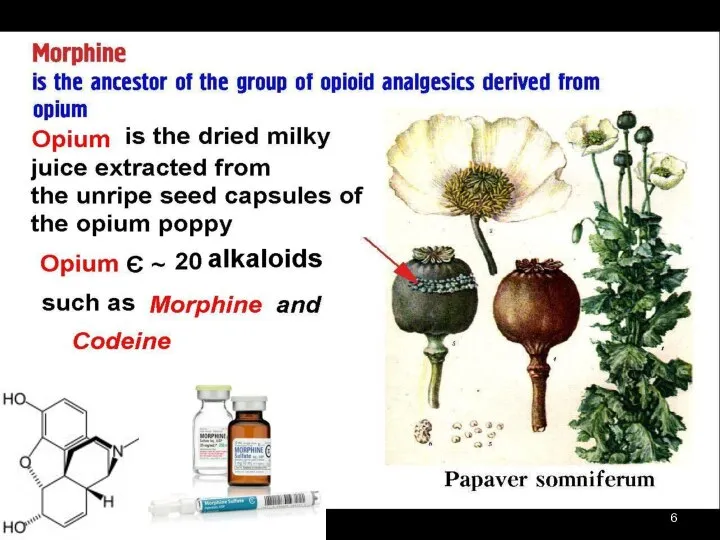
- 5. 1. Phenantrenes: Morphine Codeine Omnopon Aethylmorphine 2. Isoquinolines: Papaverine hydrochloride OPIATES (Opium Alkaloids)
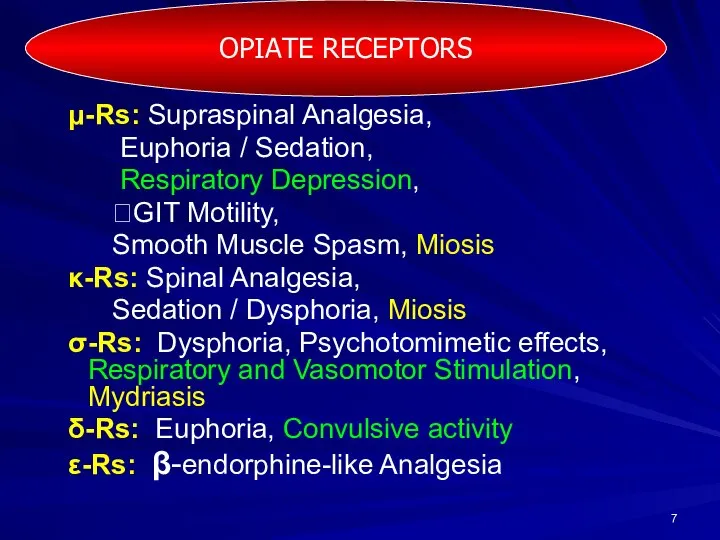
- 7. μ-Rs: Supraspinal Analgesia, Euphoria / Sedation, Respiratory Depression, ?GIT Motility, Smooth Muscle Spasm, Miosis κ-Rs: Spinal
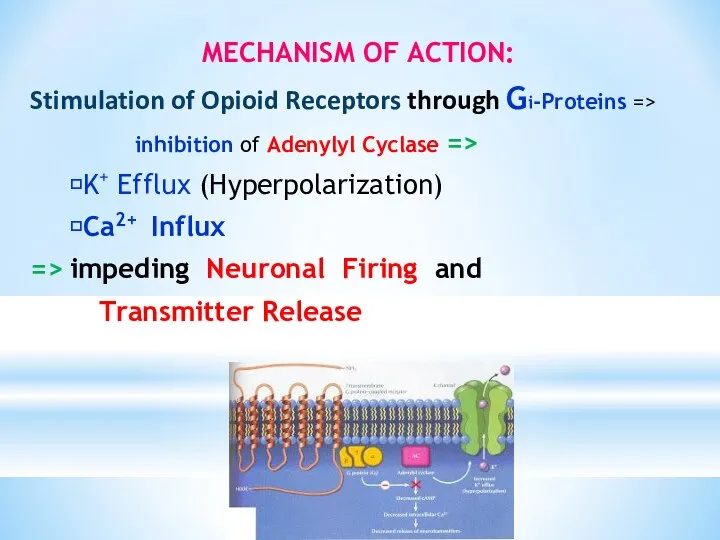
- 8. MECHANISM OF ACTION: Stimulation of Opioid Receptors through Gi-Proteins => inhibition of Adenylyl Cyclase => ?K+
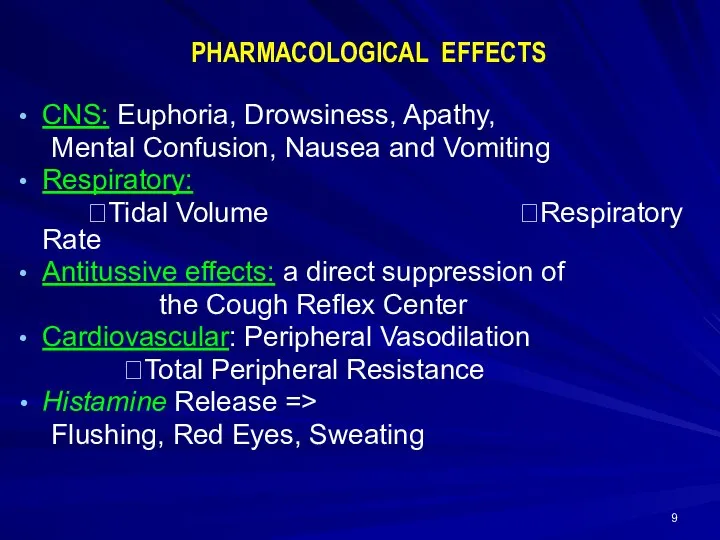
- 9. CNS: Euphoria, Drowsiness, Apathy, Mental Confusion, Nausea and Vomiting Respiratory: ?Tidal Volume ?Respiratory Rate Antitussive effects:
- 10. GIT: Inhibition of peristalsis => Constipation Sphincter of Oddi spasm, nausea ⭣Gastric, Biliary, and Pancreatic Secretions
- 11. Clinicall uses of MORPHINE ⮟ ANALGESIA: Renal or Biliary Colic Myocardial Infarction Acute Trauma Postoperative Pain
- 12. OVERDOSE with MORFINE Respiratory and CNS Depression, Miosis ?BP ?HR ? t° Skin is bluish and
- 13. Treatment of overdose with Morphine Narcotic antagonist: NALOXONE 0.4 mg/ml IV bolus 0.8-2 mg (2-5 ml)
- 14. Promedole amp. 1% -1 ml, Tab. 0.025 g, a synthetic opioid, Piperidine Compound Binds to opioid
- 15. Fentanyl amp. 0.005%-1 ml ∙ is chemically related to Promedole, ∙ has 80 times the analgesic
- 16. Pentazocine amp. 3%-1 ml,Tab. 0.05 agonist - κ-Rs and σ-Rs antagonist - μ and δ-Rs Activates
- 17. TRAMADOL caps. 0.05 g; amp. 5%-1 ml a centrally acting weak synthetic opioid with μ agonist
- 18. Naloxone amp. 0.04%-1 ml - a pure Antagonist. antagonizes most of the opioid effects: respiratory depression,
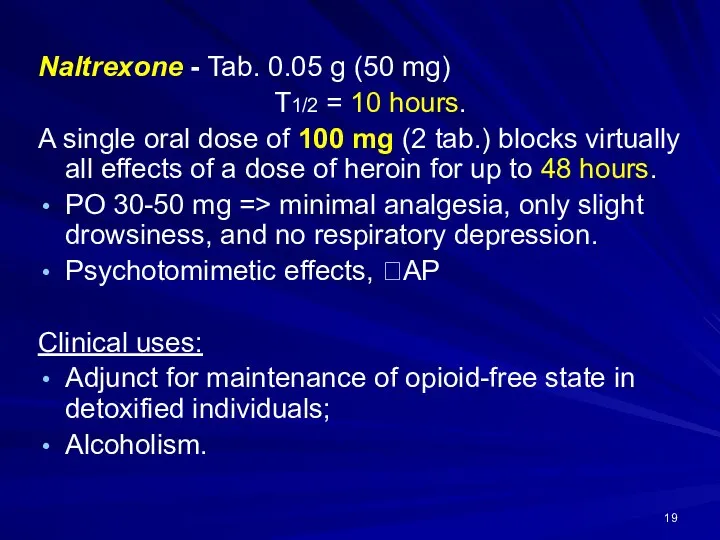
- 19. Naltrexone - Tab. 0.05 g (50 mg) T1/2 = 10 hours. A single oral dose of
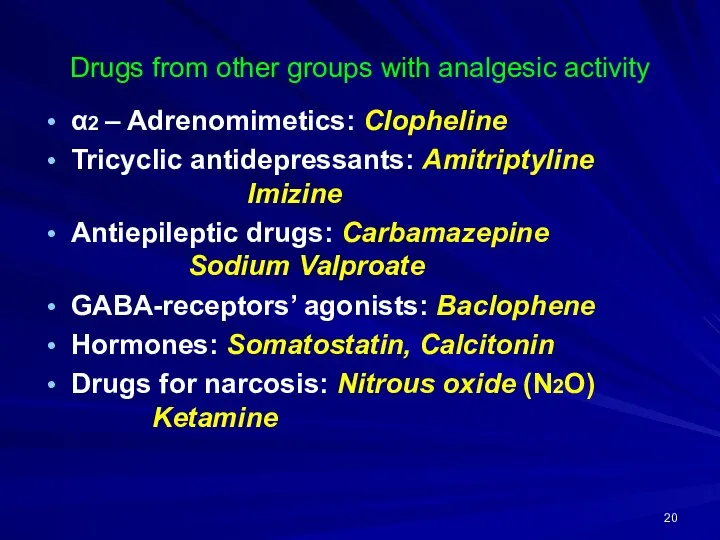
- 20. Drugs from other groups with analgesic activity α2 – Adrenomimetics: Clopheline Tricyclic antidepressants: Amitriptyline Imizine Antiepileptic
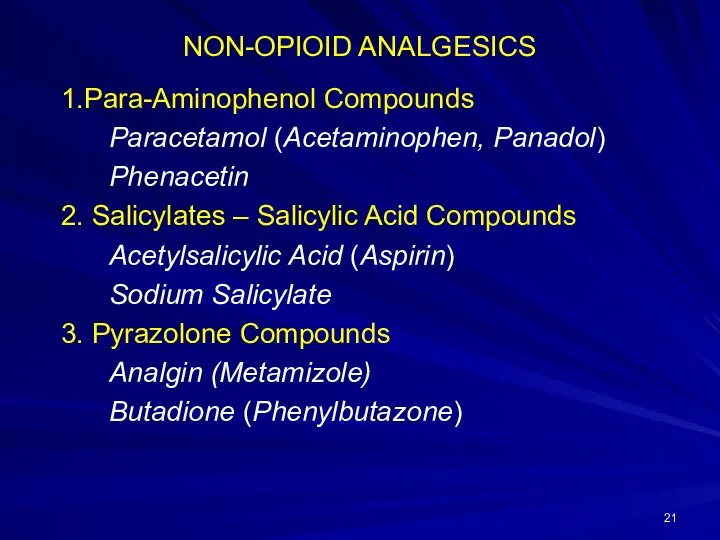
- 21. NON-OPIOID ANALGESICS 1.Para-Aminophenol Compounds Paracetamol (Acetaminophen, Panadol) Phenacetin 2. Salicylates – Salicylic Acid Compounds Acetylsalicylic Acid
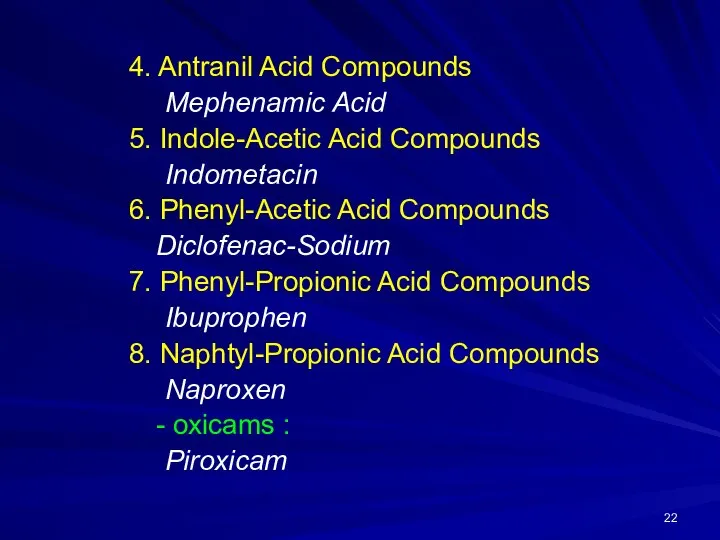
- 22. 4. Antranil Acid Compounds Mephenamic Acid 5. Indole-Acetic Acid Compounds Indometacin 6. Phenyl-Acetic Acid Compounds Diclofenac-Sodium
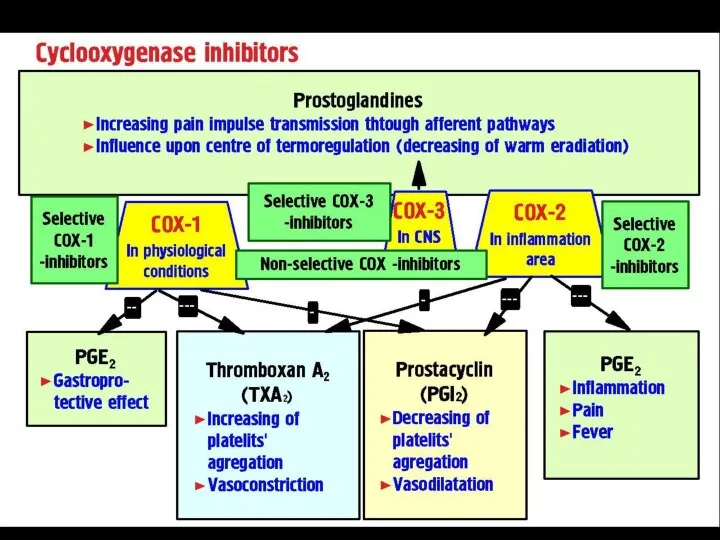
- 24. COX-2 inhibitors: Meloxicam Celecoxib Nimesulide COX-1 is structural and responsible for PROTECTIVE PROPERTIES of GIT. COX-2
- 25. Para-Aminophenol Compounds: ● Paracetamol ● Phenacetin Mechanism of action: inhibition of COX-3 1) Antipyretic action: Inhibition
- 26. ADVERSE EFFECTS Hemologic: hemolytic anemia, neutropenia, leukopenia, thrombocytopenia Hepatic: Liver Damage (toxic doses), Rash, Hypoglycemia ?Hepatic
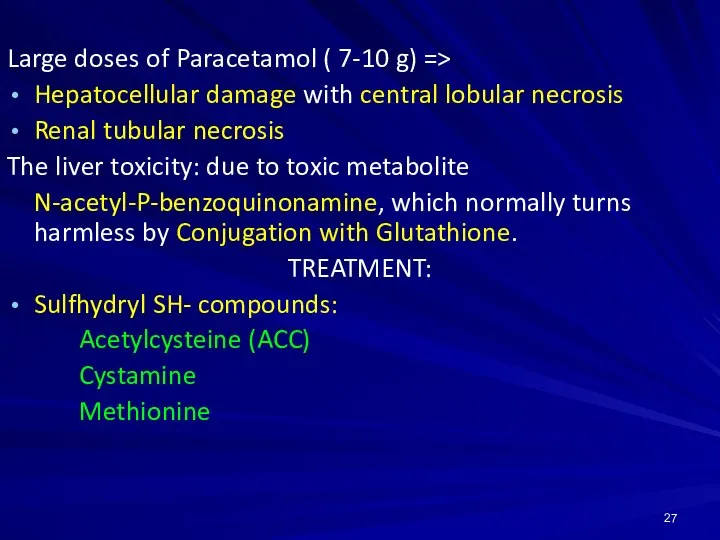
- 27. Large doses of Paracetamol ( 7-10 g) => Hepatocellular damage with central lobular necrosis Renal tubular
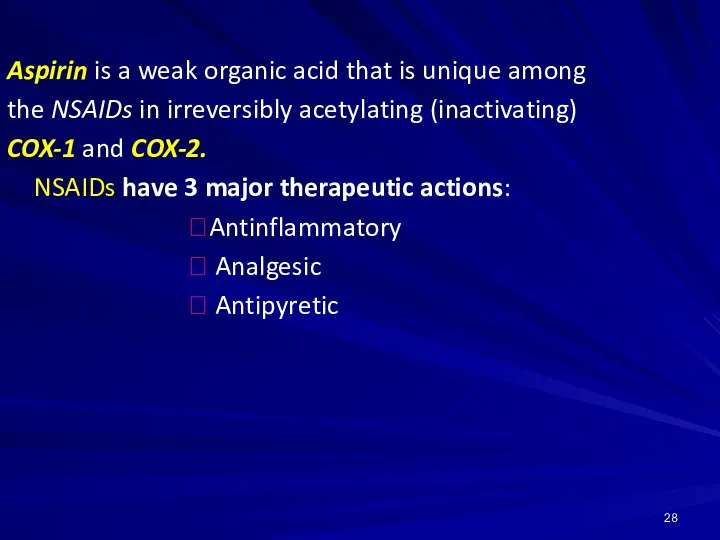
- 28. Aspirin is a weak organic acid that is unique among the NSAIDs in irreversibly acetylating (inactivating)
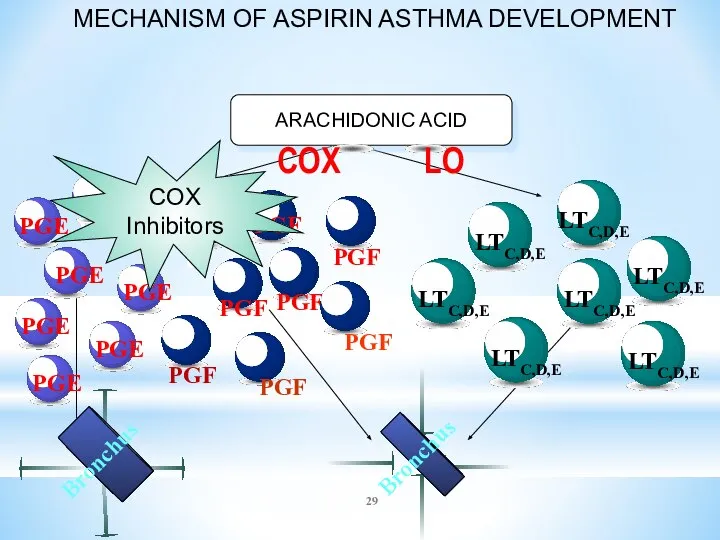
- 29. MECHANISM OF ASPIRIN ASTHMA DEVELOPMENT ARACHIDONIC ACID COX Inhibitors
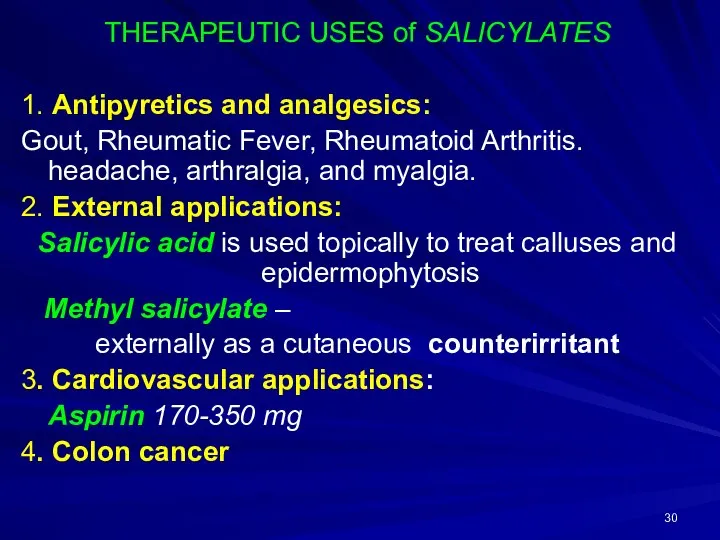
- 30. THERAPEUTIC USES of SALICYLATES 1. Antipyretics and analgesics: Gout, Rheumatic Fever, Rheumatoid Arthritis. headache, arthralgia, and
- 31. ADVERSE EFFECTS of SALICYLATES 1. GIT: nausea, vomiting, bleeding, ulceration 2. Blood: ?Prothrombin Aspirin should not
- 32. SALICYLISM - a condition of mild salicylate intoxication: nausea, vomiting, hyperventilation, headache, mental confusion, dizziness, tinnitus
- 33. Analgin (Metamizole) Tab. 0.5 g, amp. 25%-2 ml Antipyretic action - by direct action on the
- 34. Analgin is a major cause of AGRANULOCYTOSIS Phenylbutazone (Butadion) Diclofenac-natrium Indometacin can cause APLASTIC ANEMIA. =>
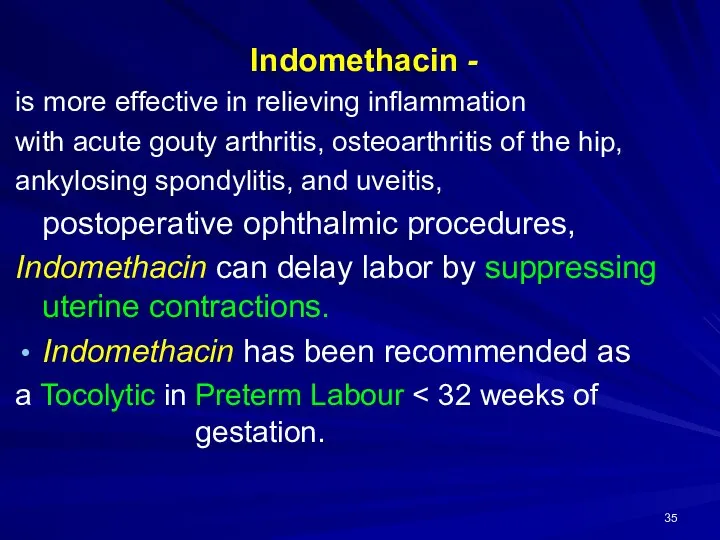
- 35. Indomethacin - is more effective in relieving inflammation with acute gouty arthritis, osteoarthritis of the hip,
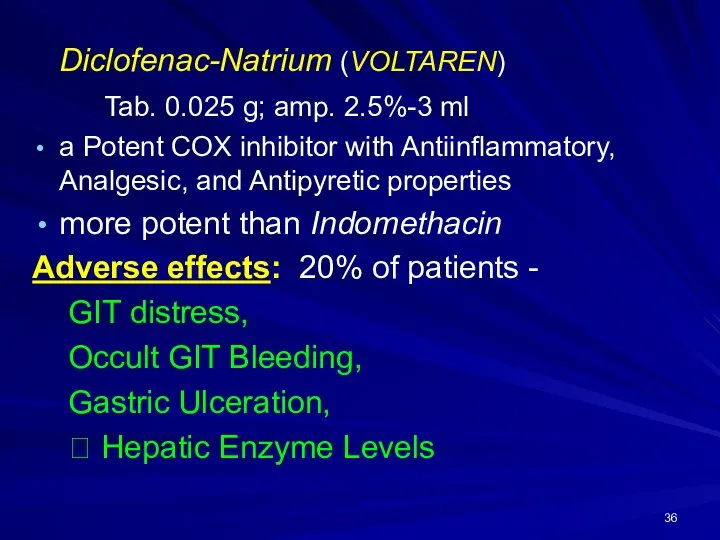
- 36. Diclofenac-Natrium (VOLTAREN) Tab. 0.025 g; amp. 2.5%-3 ml a Potent COX inhibitor with Antiinflammatory, Analgesic, and
- 37. Ketorolac Tab. 10 mg (0.01 g), amp. 3%-1 ml IM, ophthalmic drops: 0.5% solution Effective Analgesic
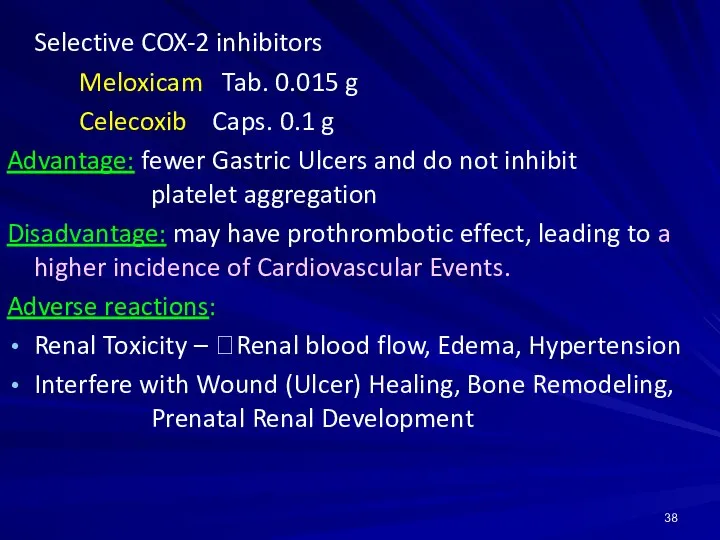
- 38. Selective COX-2 inhibitors Meloxicam Tab. 0.015 g Celecoxib Caps. 0.1 g Advantage: fewer Gastric Ulcers and
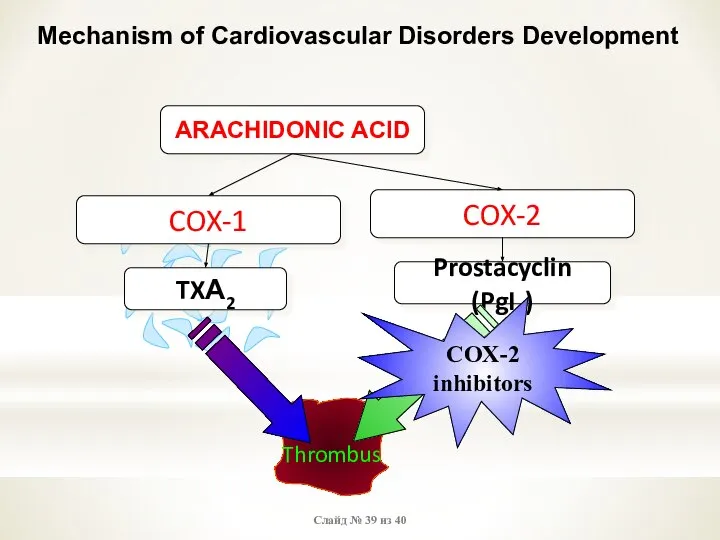
- 39. Слайд № из 40 Mechanism of Cardiovascular Disorders Development Thrombus ARACHIDONIC ACID COX-1 COX-2 TXА2 Prostacyclin
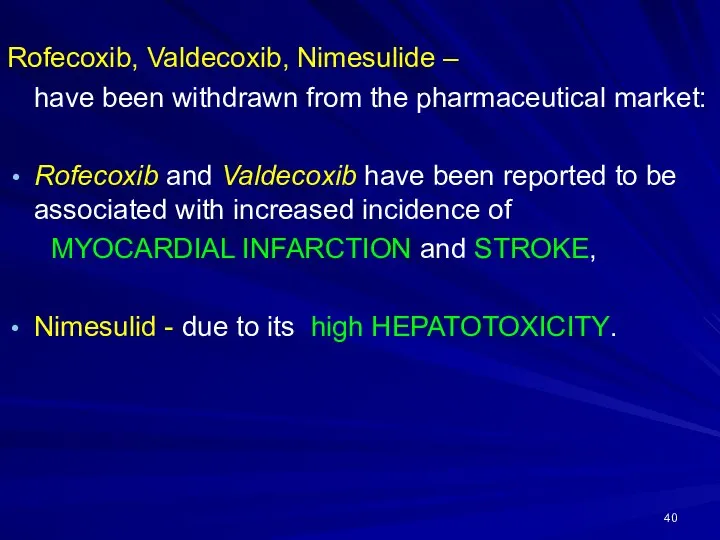
- 40. Rofecoxib, Valdecoxib, Nimesulide – have been withdrawn from the pharmaceutical market: Rofecoxib and Valdecoxib have been
- 42. Скачать презентацию


 Законы, регулирующие лечение психически больных в государстве израиль
Законы, регулирующие лечение психически больных в государстве израиль Метаболический синдром, мужской гипогонадизм
Метаболический синдром, мужской гипогонадизм Возбудитель коклюша Bordetella pertussis
Возбудитель коклюша Bordetella pertussis Кандидоз, мерез, туберкулез, Венсан стоматиті. Этиологиясы, патогенезі, клиникалық белгілері, диагноз қою, сараптамалы нақтама
Кандидоз, мерез, туберкулез, Венсан стоматиті. Этиологиясы, патогенезі, клиникалық белгілері, диагноз қою, сараптамалы нақтама Вакцины. BioNTech. Fosun Pharma. Pfiser (BNT162b2)
Вакцины. BioNTech. Fosun Pharma. Pfiser (BNT162b2) Нарушения пищевого поведения
Нарушения пищевого поведения Принципы проведения реанимационных мероприятий при терминальных нарушениях ритма
Принципы проведения реанимационных мероприятий при терминальных нарушениях ритма Клиническая смерть
Клиническая смерть Наследственные заболевания человека
Наследственные заболевания человека Психопатологическая семиотика. Психопатологическая синдромология. Определение
Психопатологическая семиотика. Психопатологическая синдромология. Определение Кенелік энцефалит
Кенелік энцефалит Созылмалы бүйрек жетіспеушілігі
Созылмалы бүйрек жетіспеушілігі Упражнения для трезвого ума и ясной памяти
Упражнения для трезвого ума и ясной памяти Особенности ведения родов при аномалиях таза
Особенности ведения родов при аномалиях таза Профессиональные заболевания исполнителей косметических услуг и производные факторы, их вызывающие
Профессиональные заболевания исполнителей косметических услуг и производные факторы, их вызывающие Контрастный массаж – неограниченные возможности. Семинар
Контрастный массаж – неограниченные возможности. Семинар Противовоспалительные средства
Противовоспалительные средства Сердечно-сосудистая система
Сердечно-сосудистая система Введение в гистологию, история науки, задачи и методы исследования
Введение в гистологию, история науки, задачи и методы исследования Кровь
Кровь Аборты, их виды и последствия
Аборты, их виды и последствия Фізична терапія дітей із захворюваннями серцево-судинної системи
Фізична терапія дітей із захворюваннями серцево-судинної системи Нарушения проводимости
Нарушения проводимости Клинический синдром гипотиреоз
Клинический синдром гипотиреоз Дифференциальная диагностика пароксизмальных состояний
Дифференциальная диагностика пароксизмальных состояний Иммунопрофилактика инфекционных заболеваний
Иммунопрофилактика инфекционных заболеваний Стоматологиядағы менеджмент және маркетинг
Стоматологиядағы менеджмент және маркетинг Травматические повреждения (часть 1)
Травматические повреждения (часть 1)