Содержание
- 2. Plague (pestis, black death) Identification: the acutest, naturally-focal, trans-missible disease characterized by: high fever, exitation, septicemia
- 3. Ancient illness animal and man: - The VIth сentury of AD - «Justinian the plague »
- 4. ETIOLOGY Y. pestis ( F. Enterobacteriaceae. K. Yersinia) – this is oval rod by a size
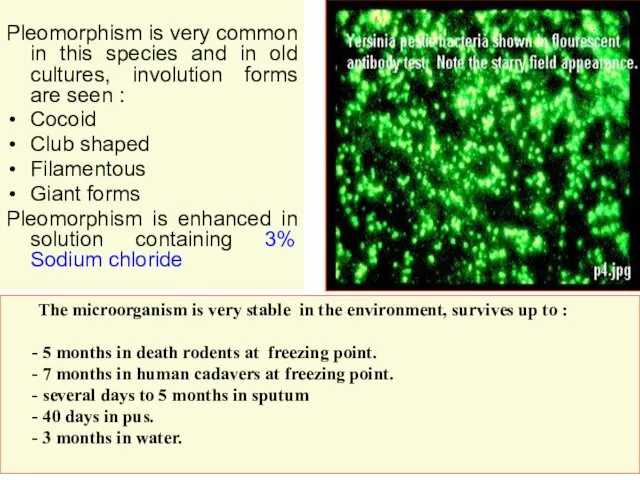
- 7. Pleomorphism is very common in this species and in old cultures, involution forms are seen :
- 8. At warming up to 70 d.C perish in 10 minutes and at boiling in 1 minute.
- 9. the coagulase- promotes forms of thrombuses with subsequent by violation of microcirculation in tissues - mouse’s
- 10. - the hemolysin - intensifys a hemolysis of erythrocytes - bacteriolysins: pesticin 1 and pesticin 2-
- 11. Epidprocess among rodents proceeds as enzootic or epizootic. At enzootic - the agent permanently circulates among
- 12. In urban the sources (synonyms- port’s, rat’s, ship’s plague) the main role belongs rats: grey, black,
- 13. The plague can be transmitted and other ways: - contact way – at taking of hides
- 21. The patient with the pulmonary form represent most danger for the surroundings. The patients with the
- 22. PATHOGENY and PATHOMORPHOLOGY Yersinias after penetrated through a skin or mucous in the lymphatic system of
- 23. 4. At aerogenic infection the primary pneumonia with subsequent the hematosepsis and death of the patient
- 24. CLINIC The incubation interval at a bubonic plague from 2 to 6 days, at the pneumonic
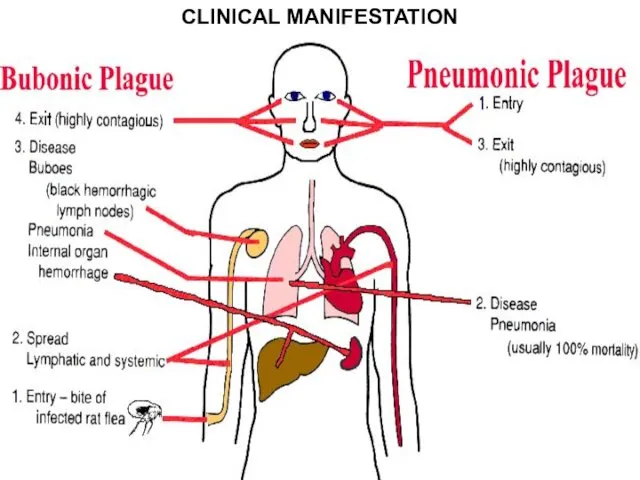
- 25. CLINICAL MANIFESTATION
- 26. The dermal form in a place of implantation occurs a hyperemia and infiltration, which fast passes
- 30. The bubonic form - starts acutely, without a prodrome. - chill and fast rise of temperature
- 31. Features of buboes at a plague: - the damage of lymph nodi starts with pain, without
- 32. - the buboes of the 2nd and the 3rd order proceed without a periadenitis - in
- 36. The pneumonic form of a plague Differs by extremely rapid current but the signs of a
- 37. - tachypnea it is revealed for all patients and always not matches to an expressiveness of
- 38. - More often proceeds as pleuropneumonias with strong by pains in a thorax, is especial at
- 41. The septic form of a plague - initially develops only for 1- 3 % of cases,
- 42. Differential diagnosis: The dermal form (antrax, tularemia, malleus) The bubonic form (purulent lymphadenitis, tularemia, lymphogranulomatos, lymphoreticulosis)
- 43. Differential diagnostics with a tularemia: The dermal form - a minimum intoxication, sluggish creation of a
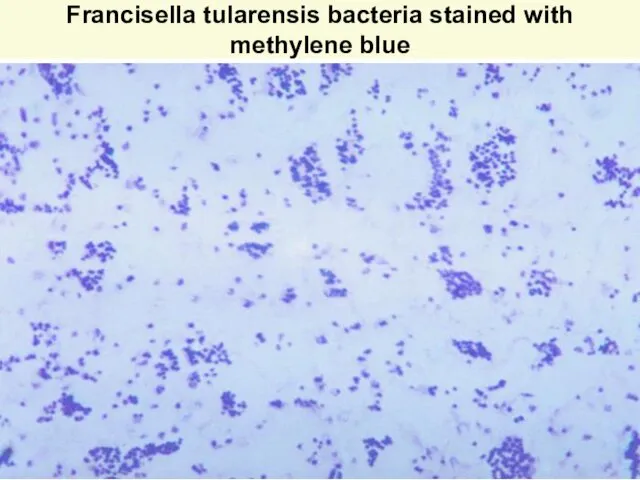
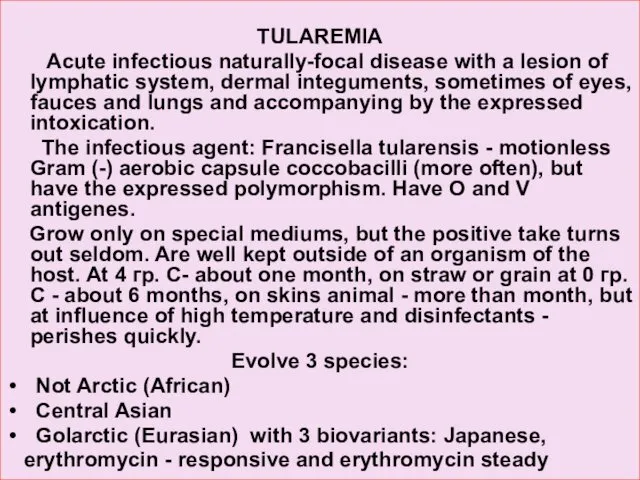
- 44. Francisella tularensis bacteria stained with methylene blue
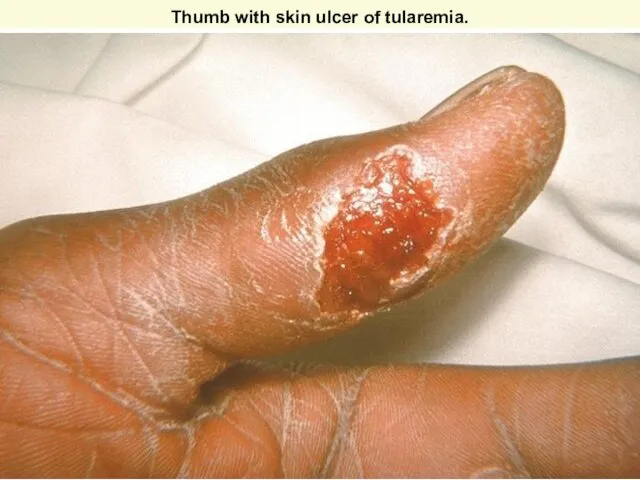
- 45. Thumb with skin ulcer of tularemia.
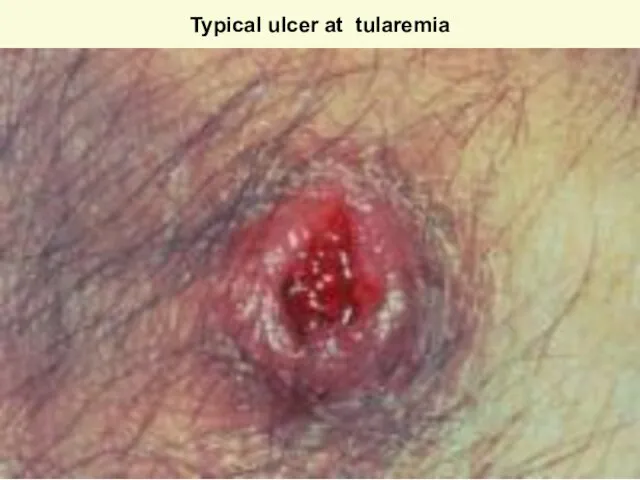
- 46. Typical ulcer at tularemia
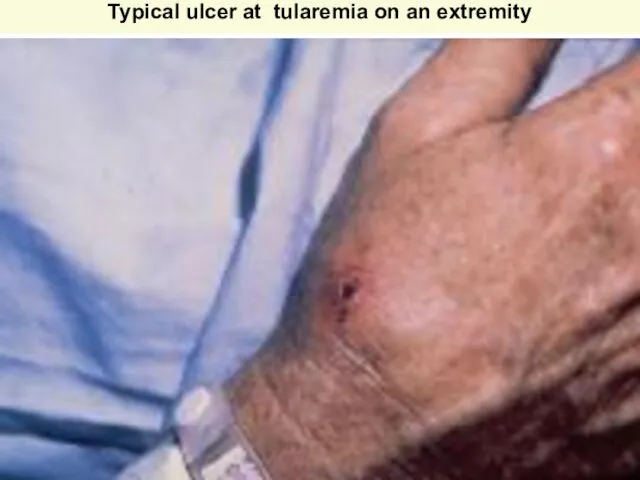
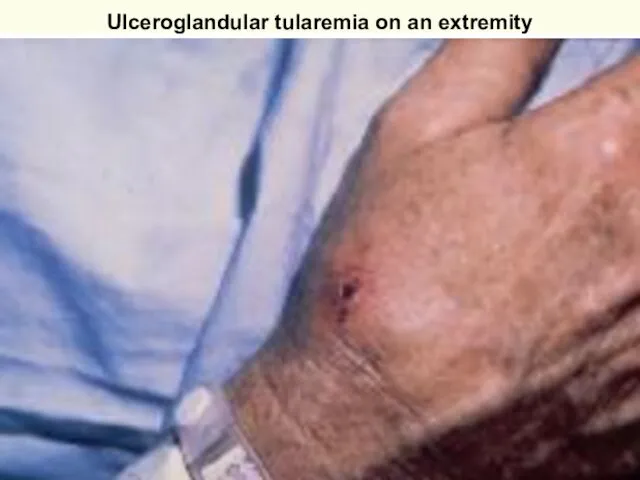
- 47. Typical ulcer at tularemia on an extremity Courtesy of Dr Hon http://www.emedicine.com/derm/topic905.htm
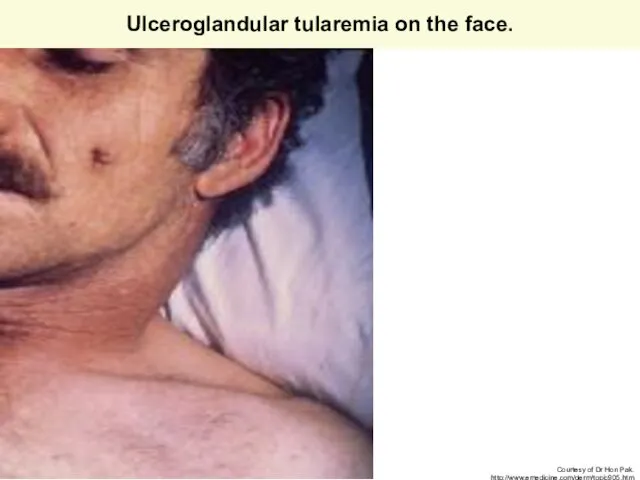
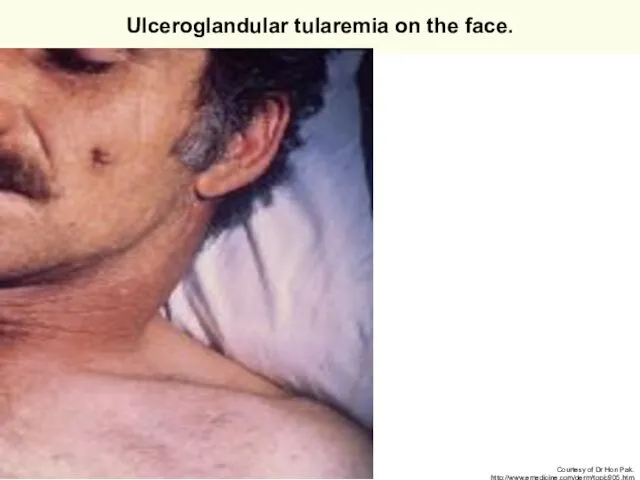
- 48. Ulceroglandular tularemia on the face. Courtesy of Dr Hon Pak. http://www.emedicine.com/derm/topic905.htm
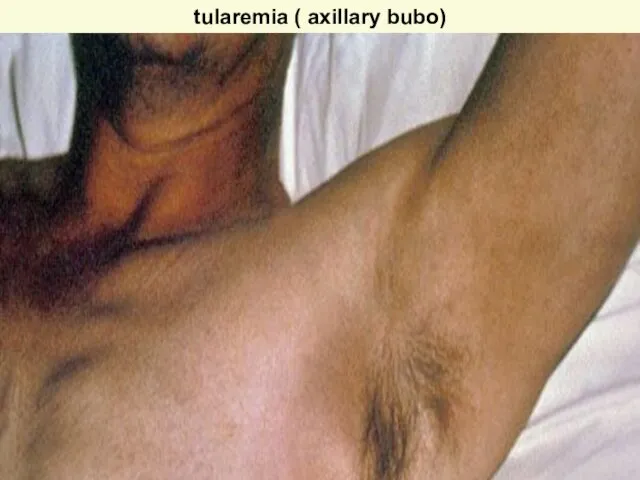
- 49. tularemia ( axillary bubo)
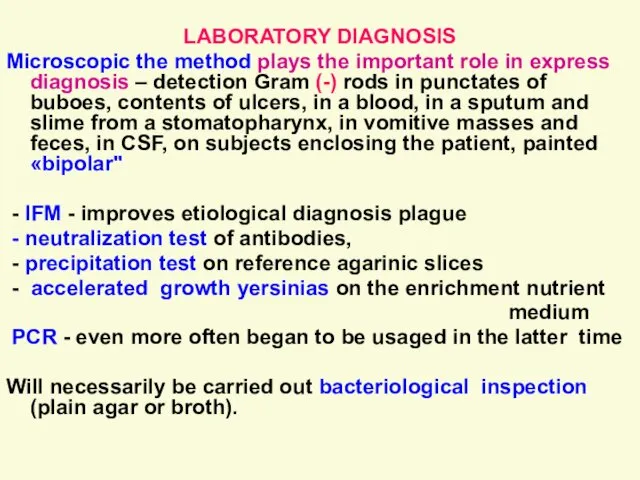
- 50. LABORATORY DIAGNOSIS Microscopic the method plays the important role in express diagnosis – detection Gram (-)
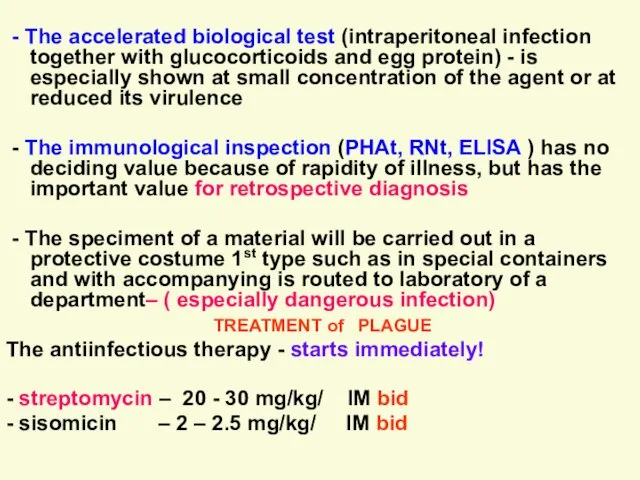
- 51. - The accelerated biological test (intraperitoneal infection together with glucocorticoids and egg protein) - is especially
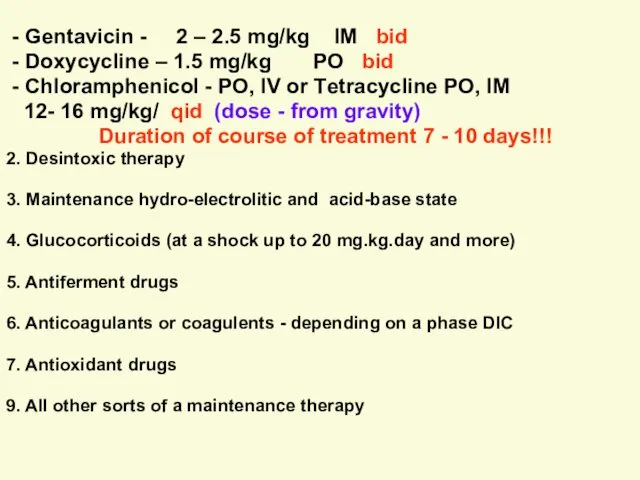
- 52. - Gentavicin - 2 – 2.5 mg/kg IM bid - Doxycycline – 1.5 mg/kg PO bid
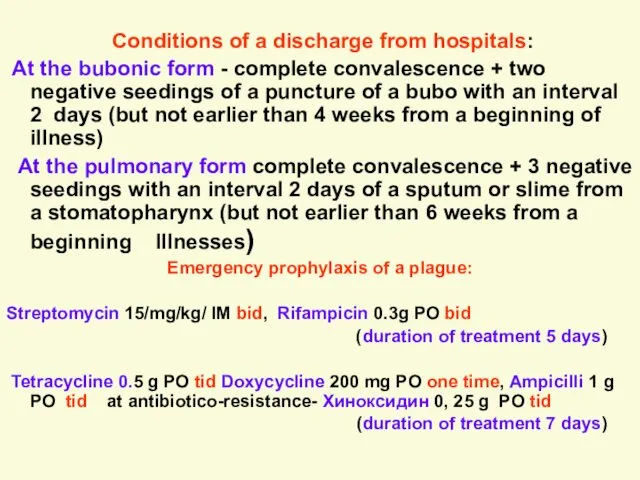
- 53. Conditions of a discharge from hospitals: At the bubonic form - complete convalescence + two negative
- 54. Antiepidemic measures in the center of a plague: The information about falling sick or suspicious transmitted
- 55. ТУЛЯРЕМИЯ ( TULAREMIA ) Острое инфекционное природно-очаговое заболевание с поражением лимфатических узлов, кожных покровов, иногда глаз,
- 56. TULAREMIA Acute infectious naturally-focal disease with a lesion of lymphatic system, dermal integuments, sometimes of eyes,
- 57. Francisella tularensis bacteria stained with methylene blue
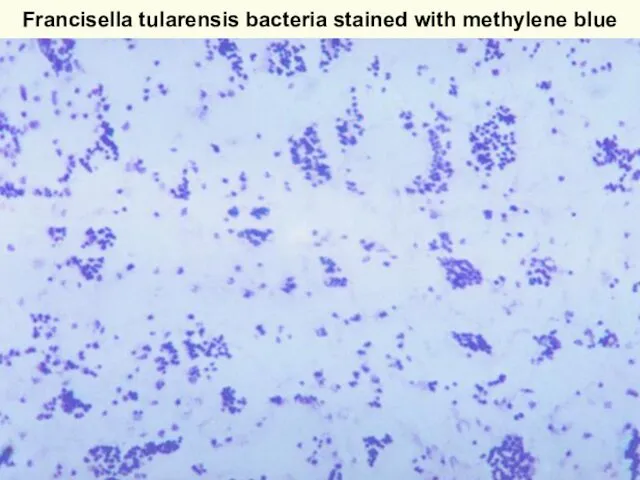
- 58. ЭПИДЕМИОЛОГИЯ Туляремия – распространенное природно-очаговое заболевание умеренного климатического пояса Северного полушария. Типы очагов – лесной, степной,
- 59. EPIDEMIOLOGY Tularemia – propagated naturally-focal disease of a moderate climatic girdle of Northern hemisphere. Phylums of
- 60. PATHOGENY Bacteria penetrate through a skin, mucosas of eyes, respiratory tracts, GASTROINTESTINAL TRACT. At a puncture
- 61. ПАТОГЕНЕЗ Бактерии проникают через кожу, слизистые оболочки глаз, дыхательных путей, ЖКТ. При укусе насекомых-часто развивается первичный
- 62. КЛИНИКА Инкубационный период 3- 7 дней ( от 1 до 30 дней). Выделяют следующие формы туляремии:
- 63. Относительная брадикардия, гипотония, гепатосплено-мегалия. ОАК- умеренный лейкоцитоз с нейтрофилией со сменой в дальнейшем на лимфомоноцитоз. СОЭ
- 64. Подмышечный бубон при туляремии
- 65. 2.Язвенно- бубонная чаще при трансмиссивном заражении В месте внедрения появляется пятно, папула, везикула, пустула, неглубокая язва
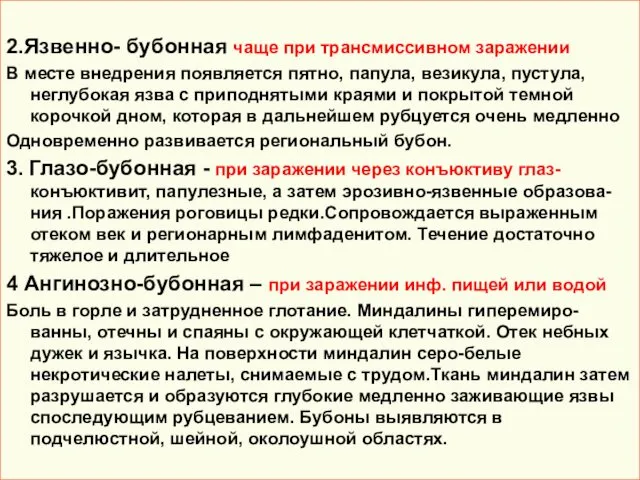
- 66. The typical ulcer of tularemia
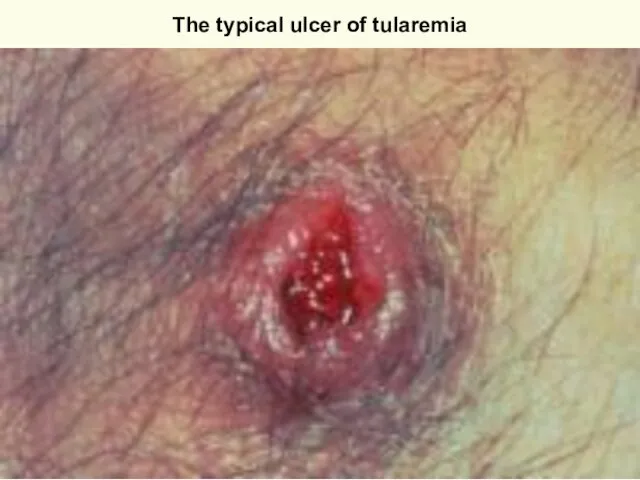
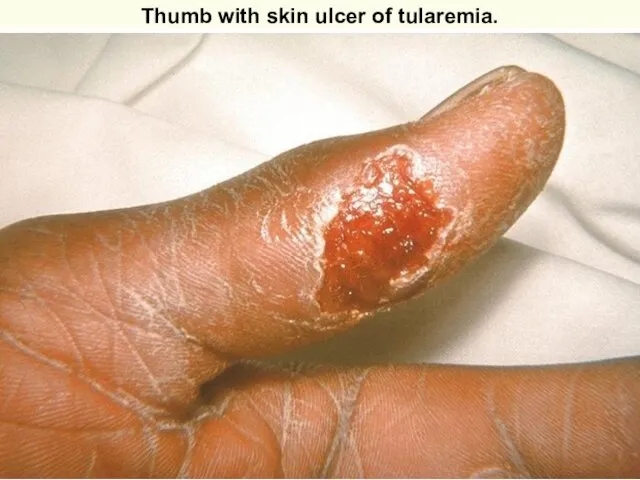
- 67. Thumb with skin ulcer of tularemia.
- 68. Ulceroglandular tularemia on an extremity Courtesy of Dr Hon http://www.emedicine.com/derm/topic905.htm
- 69. Ulceroglandular tularemia on the face. Courtesy of Dr Hon Pak. http://www.emedicine.com/derm/topic905.htm
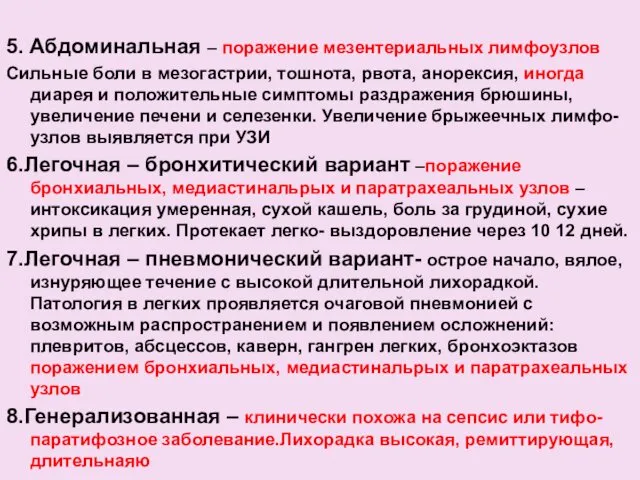
- 70. 5. Абдоминальная – поражение мезентериальных лимфоузлов Сильные боли в мезогастрии, тошнота, рвота, анорексия, иногда диарея и
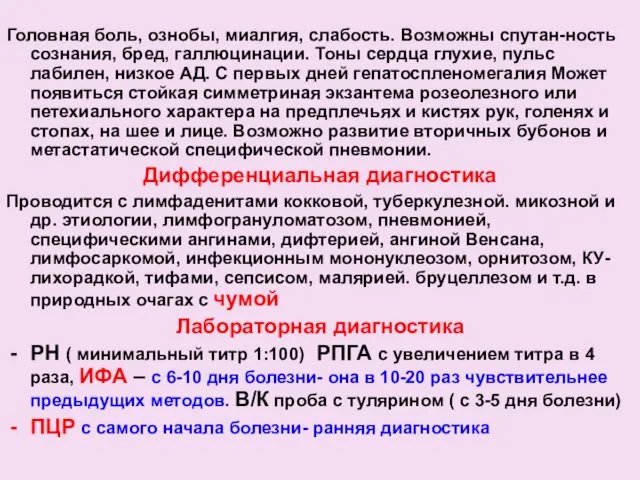
- 71. Головная боль, ознобы, миалгия, слабость. Возможны спутан-ность сознания, бред, галлюцинации. Тоны сердца глухие, пульс лабилен, низкое
- 72. ЛЕЧЕНИЕ Антиинфекционная терапия ( доза – от тяжести) –Streptomycin - 15-20 mg/kg/day IM в 2 приема
- 74. Скачать презентацию



















 Доброкачественные заболевания женской репродуктивной системы
Доброкачественные заболевания женской репродуктивной системы Интеллект и интеллектуальная недостаточность
Интеллект и интеллектуальная недостаточность Врожденная гипоплазия легких
Врожденная гипоплазия легких Лимфопролиферативный синдром
Лимфопролиферативный синдром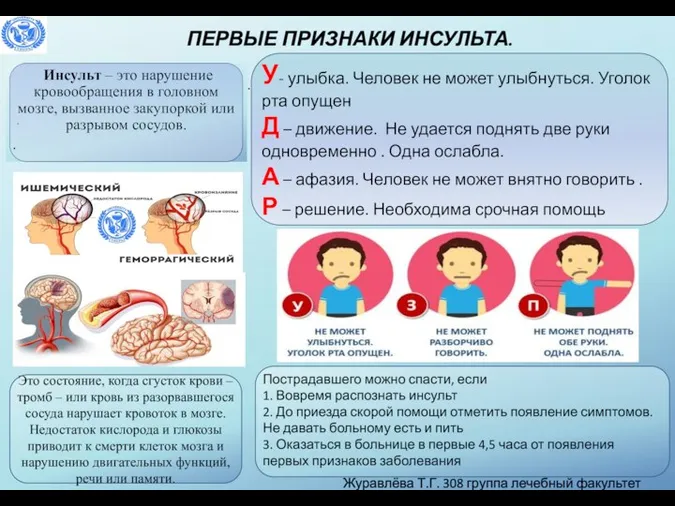 Первые признаки инсульта
Первые признаки инсульта Акушерський травматизм
Акушерський травматизм Лихорадка Денге
Лихорадка Денге Аурухана ішілік инфекцияны бақылауды ұйымдастыру
Аурухана ішілік инфекцияны бақылауды ұйымдастыру Жіті тыныстың жеткіліксіздігі
Жіті тыныстың жеткіліксіздігі Кардиомегалии. Дифференциальная диагностика
Кардиомегалии. Дифференциальная диагностика Ультразвуковое исследование. Ультразвуковая диагностика в педиатрии
Ультразвуковое исследование. Ультразвуковая диагностика в педиатрии Аменорея у девушек
Аменорея у девушек Деятельность Российского общества Красного Креста в годы Первой мировой войны
Деятельность Российского общества Красного Креста в годы Первой мировой войны Эпизоотии и эпифитотии
Эпизоотии и эпифитотии Особенности конструирования зубных протезов при опоре на имплантаты. Принципы выбора рациональных структур имплантатов
Особенности конструирования зубных протезов при опоре на имплантаты. Принципы выбора рациональных структур имплантатов Нарушение этики молодёжью
Нарушение этики молодёжью Tema 7. Morfologia articulatiilor
Tema 7. Morfologia articulatiilor Сестринская помощь при остром коронарном синдроме
Сестринская помощь при остром коронарном синдроме Наблюдение пациентов с ЭКС. Правила проведения контрольных визитов
Наблюдение пациентов с ЭКС. Правила проведения контрольных визитов Өзін-өзі тәрбиелеу – педагог-психологтың кәсіби шеберлігінің қалыптасу шарты ретінде
Өзін-өзі тәрбиелеу – педагог-психологтың кәсіби шеберлігінің қалыптасу шарты ретінде Пространство развития и творчества
Пространство развития и творчества Instrumenti. Ķirurģisko instrumentu iedalījums
Instrumenti. Ķirurģisko instrumentu iedalījums Применение металлопластмассовых зубных протезов: лекция 3
Применение металлопластмассовых зубных протезов: лекция 3 Үсік шалған кездегі алғашқы көмек
Үсік шалған кездегі алғашқы көмек Фиброзно-кавернозный и цирротический туберкулез. Внелегочный туберкулез: туберкулез ЦНС, костей и суставов,
Фиброзно-кавернозный и цирротический туберкулез. Внелегочный туберкулез: туберкулез ЦНС, костей и суставов, Амбулаторлық карта
Амбулаторлық карта Қазақстандағы денсаулық сақтау ұйымы және бағдарламалары
Қазақстандағы денсаулық сақтау ұйымы және бағдарламалары Вакцинация детей с перинатальным контактом по ВИЧ и ВИЧ-инфицированных
Вакцинация детей с перинатальным контактом по ВИЧ и ВИЧ-инфицированных