Содержание
- 2. Lecture Plan Blood volume changes Anemia classifications Clinical features and specific signs of anemias Erythrocytosis (Polycytemia)
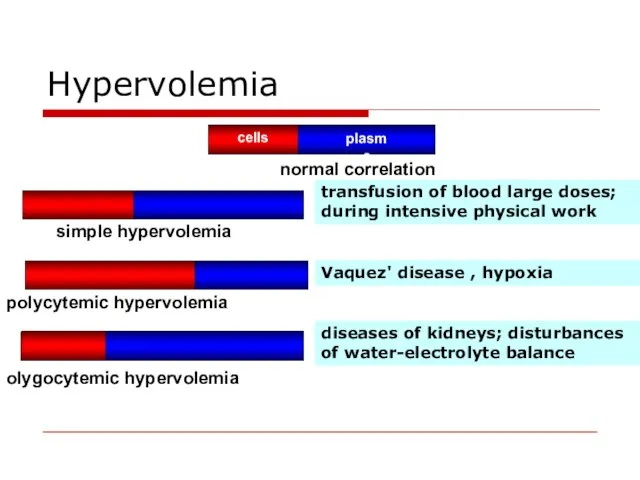
- 3. Hypervolemia transfusion of blood large doses; during intensive physical work Vaquez' disease , hypoxia diseases of
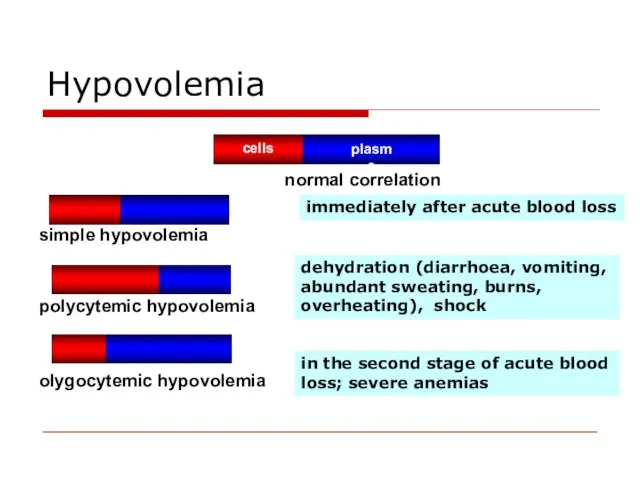
- 4. Hypovolemia dehydration (diarrhoea, vomiting, abundant sweating, burns, overheating), shock in the second stage of acute blood
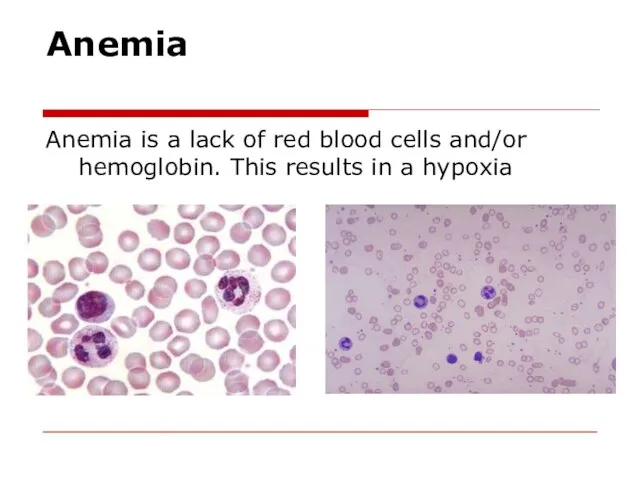
- 5. Anemia Anemia is a lack of red blood cells and/or hemoglobin. This results in a hypoxia
- 6. Anemia classifications Pathogenic classification. Posthemorrhagic (acute or chronic). Haemolytic - acute and chronic. Chronic haemolytic anaemias
- 7. Anemia classifications Classification due to haemoglobin content in RBC. Normally haemoglobin content in erythrocyte is 0,8—1,05.
- 8. Anemia classifications Classification based on the on the type of RBC maturation. erythroblastic anemias megaloblastic anemias
- 9. Clinical features of anemia olygocythemic normovolemia (in most anemias); hypovolemia (acute posthemorrhagic anaemia, pernicious anaemia); paleness
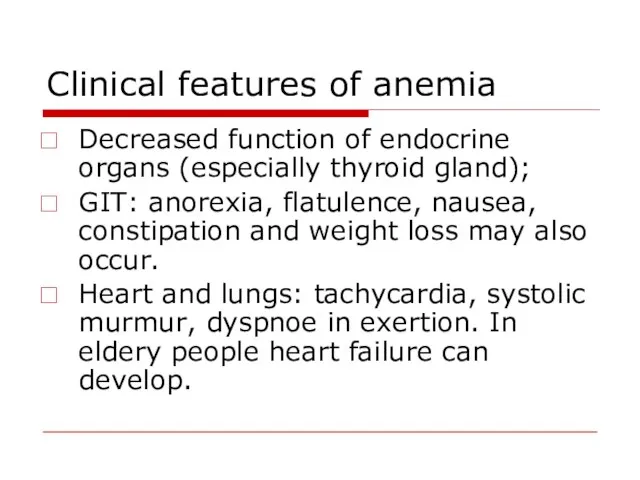
- 10. Clinical features of anemia Decreased function of endocrine organs (especially thyroid gland); GIT: anorexia, flatulence, nausea,
- 11. Specific signs of anemias Posthemorrhagic anaemia – signs of blood loss from different organs; Iron deficiency
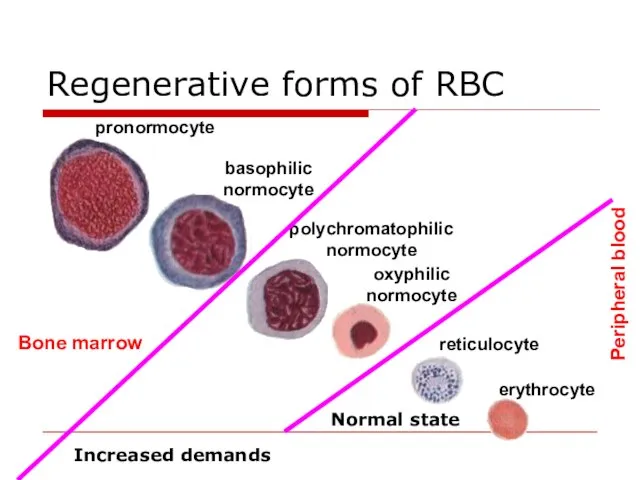
- 12. Regenerative forms of RBC Bone marrow Peripheral blood Normal state Increased demands
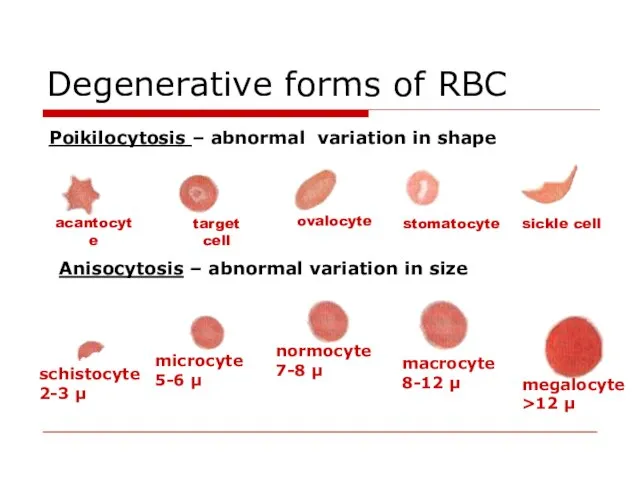
- 13. Degenerative forms of RBC Poikilocytosis – abnormal variation in shape target cell sickle cell Anisocytosis –
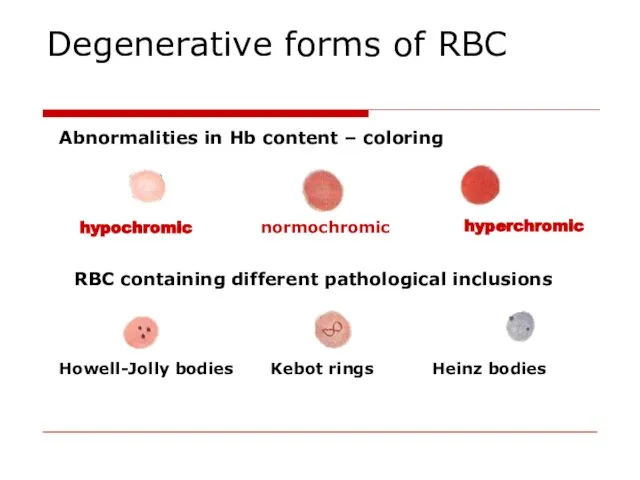
- 14. Degenerative forms of RBC Abnormalities in Hb content – coloring hypochromic normochromic RBC containing different pathological
- 15. Anemia of blood loss The main reasons of blood loss: blood vessels or heart walls safety
- 16. Acute posthemorrhagic anemia 1st stage – heart rate and blood vessel tonus are increased, centralization of
- 17. Principles of blood loss therapy Etiologic treatment: the increasing of blood coagulation, the reconstruction of vessel
- 18. Chronic posthemorrhagic anaemia RBC number and Hb content is decreased Hypochromic (colour index is 0,6-0,4) This
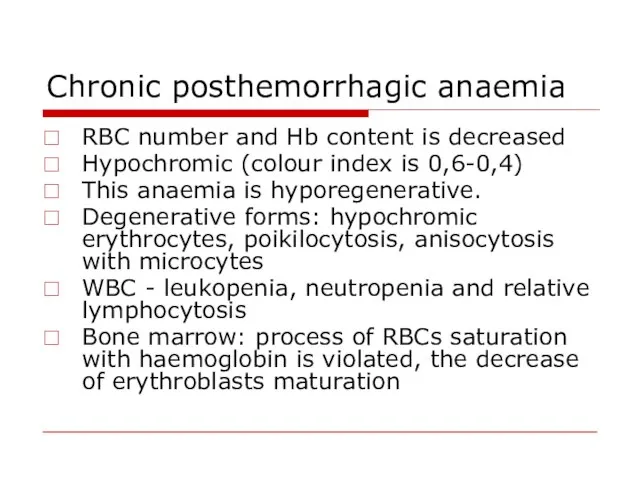
- 19. Chronic posthemorrhagic anaemia Regeneratory stage: Hb, RBC, colour index are lower that normal. Its duration depends
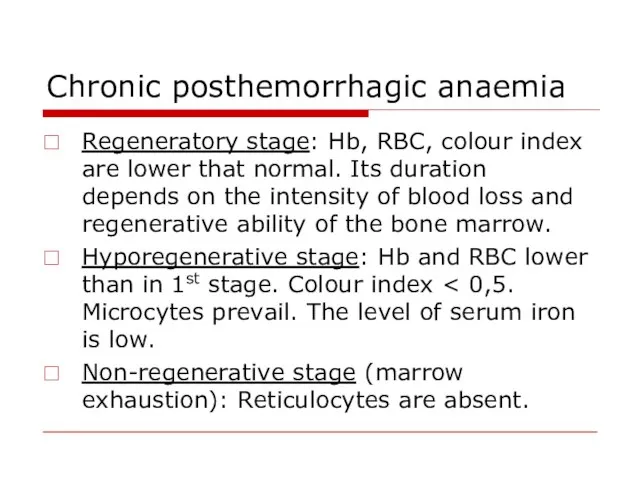
- 20. Hemolytic Anemias Types of hemolysis Extravascular (common) – occurs in phagocytic cells of the spleen, liver,
- 21. Hemolytic Anemias Classification Acute Chronic Acquired Inherited immune mechanical injury toxic effects RES hyperactivity
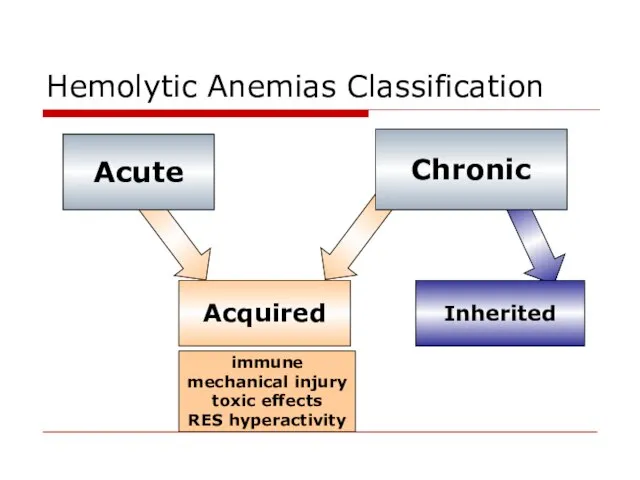
- 22. Acquired hemolytic anemias Immune abnormalities due to antibodies production: against own undamaged RBC (autoimmune hemolytic anemia);
- 23. Acquired hemolytic anemias Mechanical injury of RBC due to abnormalities of microcirculation. during high physical activity
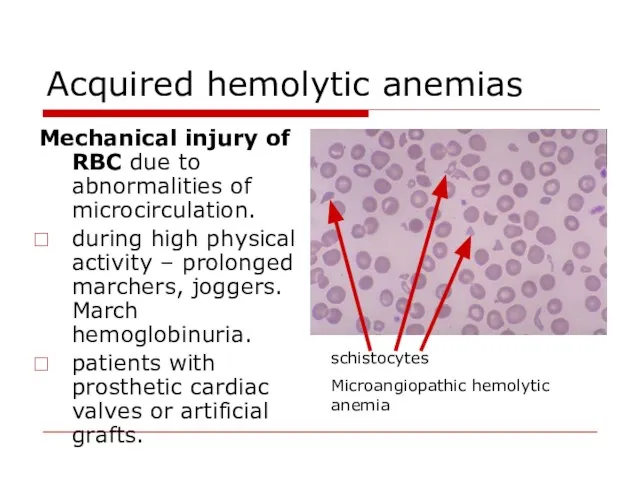
- 24. Acquired hemolytic anemias Direct toxic effect Infectious agents toxic effect (α- or β-hemolytic streptococci, meningococci) Invasion
- 25. Hereditary hemolytic anemias Pathology of RBC membrane Hereditary spherocytosis autosomal dominant disease defects in erythrocyte membrane
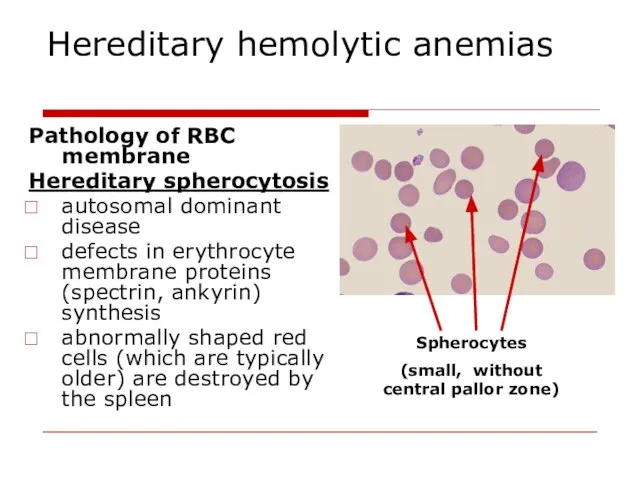
- 26. Hereditary hemolytic anemias Pathology of RBC enzymes Glucose-6-phosphate dehydrogenase deficiency. X-linked recessive G6PD is necessary for
- 27. Hereditary hemolytic anemias Pathology of haemoglobin Sickle cell disease is a qualitative disorder of Hb (abnormal
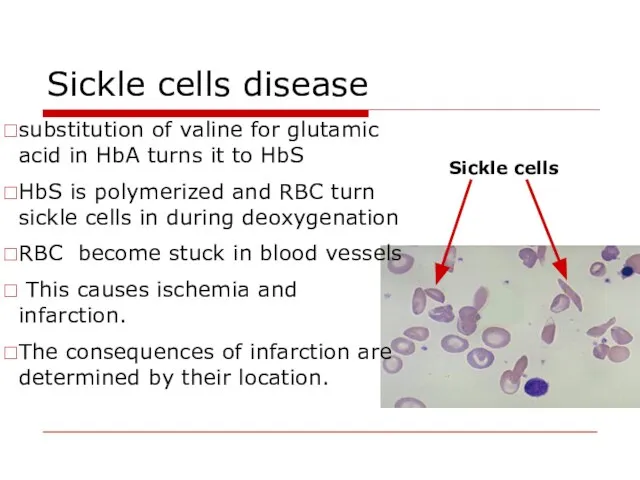
- 28. Sickle cells disease substitution of valine for glutamic acid in HbA turns it to HbS HbS
- 29. Thalassemia classification α thalassemia, the production of α globin is deficient β thalassemia the production of
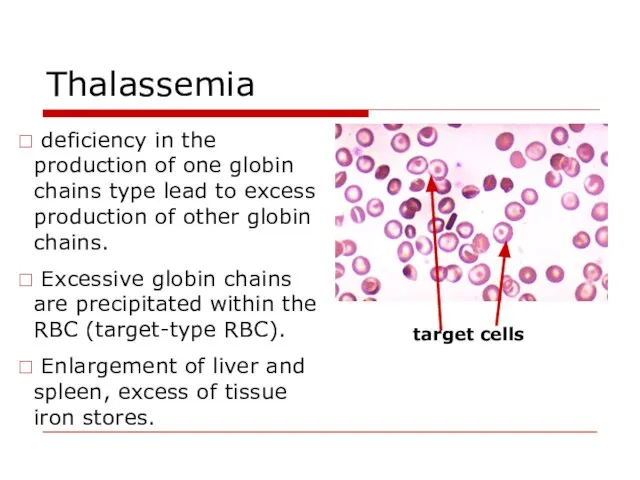
- 30. Thalassemia deficiency in the production of one globin chains type lead to excess production of other
- 31. Anemias caused by disturbances of haemopoiesis Iron deficiency reasons: chronic blood losses due to - excessive
- 32. Anemias caused by disturbances of haemopoiesis nails (koilonychia or spoon-shaped nails), tongue (atrophic glossitis) mouth (angular
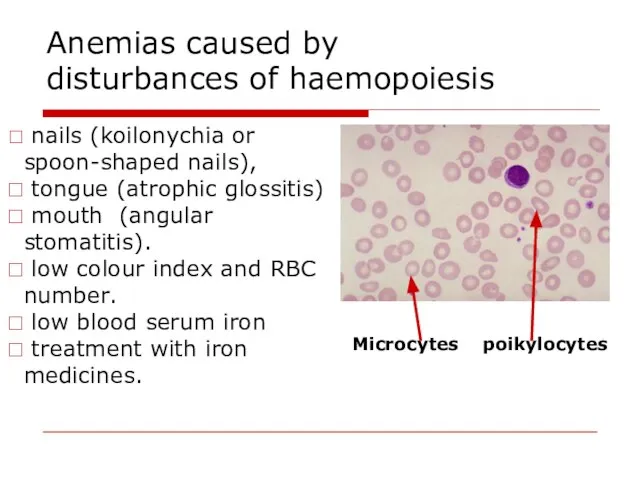
- 33. Anemias caused by disturbances of haemopoiesis Syderoblastic anemia (refractory to iron) defect enzymes that include iron
- 34. Anemias caused by disturbances of haemopoiesis Megaloblastic anaemia deficiency of vitamin B12 and folic acid. impaired
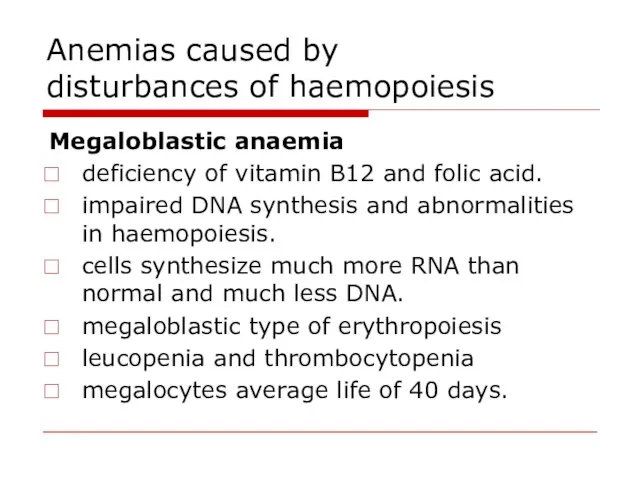
- 35. Megaloblastic anemia The reasons of B12 deficiency: inadequate dietary intake (strict vegetarians) inadequate production of intrinsic
- 36. Vitamin B12 metabolism transport by transcobalamin haemopoiesis combines with intrinsic factor absorption myelination of nervous fibers
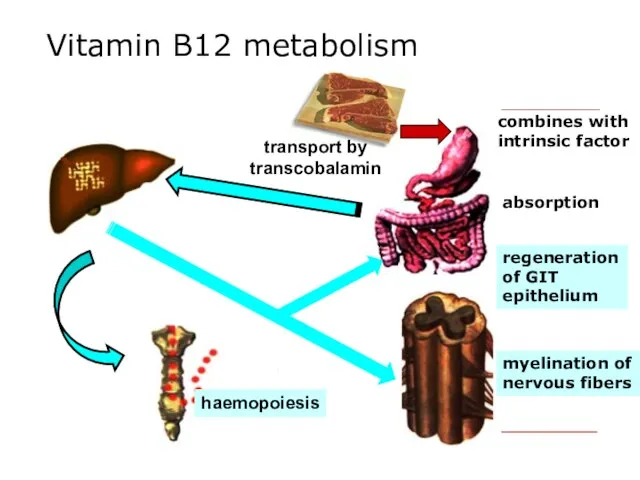
- 37. Megaloblastic anemia hyperchromic, macrocytic, hyporegenerative hypersegmented neutrophil RBC with Howell Jolly bodies Megalocyte
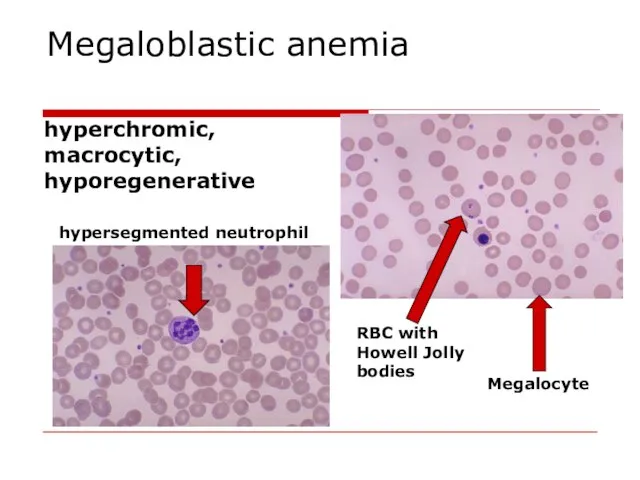
- 38. Megaloblastic anemia Specific clinical features of megaloblastic anemia: glossitis (inflammation of the tongue; smooth, beefy, red
- 39. Anemias caused by disturbances of haemopoiesis Hypoplastic and aplastic anaemias etiology: medicines with myelotoxic effect (amidopyrine,
- 40. Anemias caused by disturbances of haemopoiesis The picture of blood – pancytopenia – decrease of all
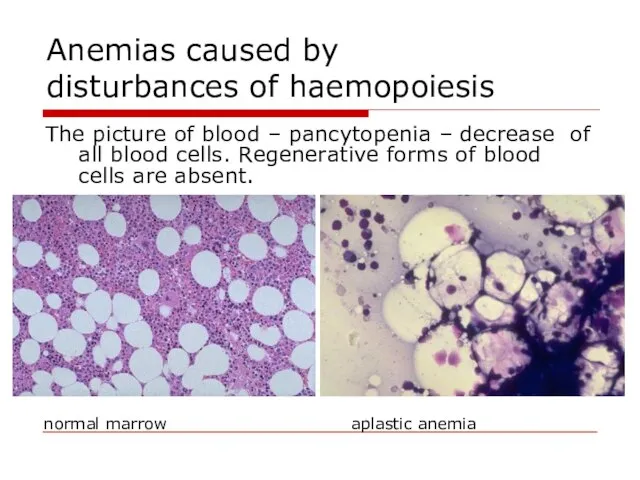
- 41. Anemias caused by disturbances of haemopoiesis Metaplastic anaemias etiology: leukemic metaplasia of bone marrow (it consists
- 42. Erythrocytosis (Polycytemia) RBC count: more than 4,7*1012//L in women and more than 5,0*1012//L in men. Erythrocytosis
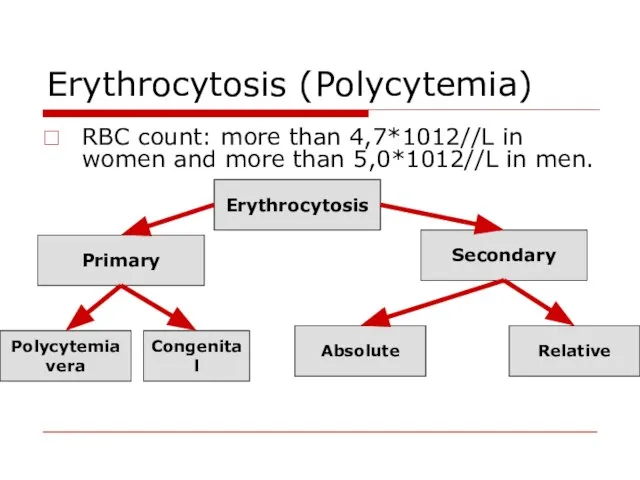
- 43. Vaquez’ disease (Polycythemia vera) Tumor induced hyperplasia of bone marrow Normal blood smear Polycytemia vera
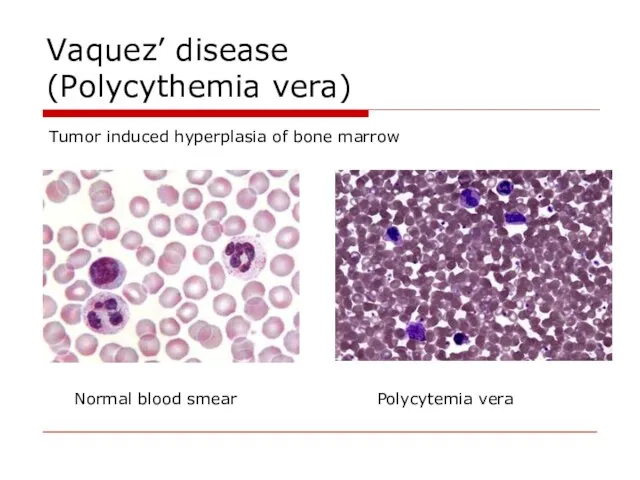
- 44. Vaquez’ disease (Polycythemia vera) Blood count: increased number of RBC, reticulocytes, WBC and platelets. Blood volume
- 45. Vaquez’ disease (Polycythemia vera) Clinical signs arterial hypertension ; plethora with congested mucous membranes conjunctiva and
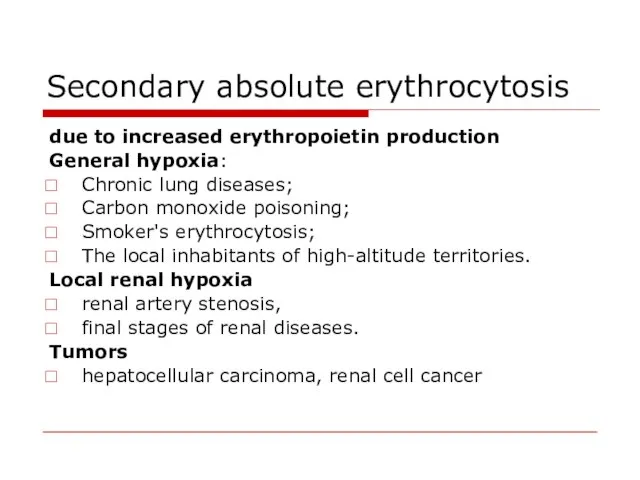
- 46. Secondary absolute erythrocytosis due to increased erythropoietin production General hypoxia: Chronic lung diseases; Carbon monoxide poisoning;
- 48. Скачать презентацию
 Всемирная неделя иммунизации, 2019 г
Всемирная неделя иммунизации, 2019 г Әкелерді қатыстыру
Әкелерді қатыстыру Медициналық этика мен деонтология
Медициналық этика мен деонтология Микробиология холеры
Микробиология холеры Рациональная антимикробная терапия
Рациональная антимикробная терапия Приобретенные пороки сердца
Приобретенные пороки сердца Заболевания щитовидной железы
Заболевания щитовидной железы Детские инфекции у детей: дифтерия, менингококковая инфекция
Детские инфекции у детей: дифтерия, менингококковая инфекция Механизм опухолевой трансформации клетки
Механизм опухолевой трансформации клетки Мочевые органы мочевыделительной системы
Мочевые органы мочевыделительной системы Проблемы межполушарной асимметрии и межполушарного взаимодействия
Проблемы межполушарной асимметрии и межполушарного взаимодействия Дыхательная гимнастика, разработанная А.Н. Стрельниковой. Применение в ЛФК
Дыхательная гимнастика, разработанная А.Н. Стрельниковой. Применение в ЛФК Иерсиниозы. Клиника и современные методы диагностики
Иерсиниозы. Клиника и современные методы диагностики Ауыл тұрғындарына ,бастапқы медико – санитарлық көмекті ұйымдастыру
Ауыл тұрғындарына ,бастапқы медико – санитарлық көмекті ұйымдастыру Familial Mediterranean fever (FMF)
Familial Mediterranean fever (FMF) Взаимосвязь уровня тревожности и акцентуаций характера у студентов ВУЗа
Взаимосвязь уровня тревожности и акцентуаций характера у студентов ВУЗа Современные проблемы многоплодной беременности
Современные проблемы многоплодной беременности Система и задачи судебной медицины
Система и задачи судебной медицины АИВ инфекциясымен ауыратын науқастағы вирусты гепатиттердің алдын алу және емдеудің ерекшеліктері
АИВ инфекциясымен ауыратын науқастағы вирусты гепатиттердің алдын алу және емдеудің ерекшеліктері Малярия
Малярия Ми қан айналым бұзылыс синдромдары
Ми қан айналым бұзылыс синдромдары Отбасыны сипаттау жүйесі
Отбасыны сипаттау жүйесі Здоровый образ жизни
Здоровый образ жизни Мутацияның молекулалық негіздері
Мутацияның молекулалық негіздері Болезнь Паркинсона
Болезнь Паркинсона Песочная терапия и её возможности в логопедической практике (часть 2)
Песочная терапия и её возможности в логопедической практике (часть 2) Ортопедиялық стоматологиядағы минимальды интервенция тұжырымдамасы
Ортопедиялық стоматологиядағы минимальды интервенция тұжырымдамасы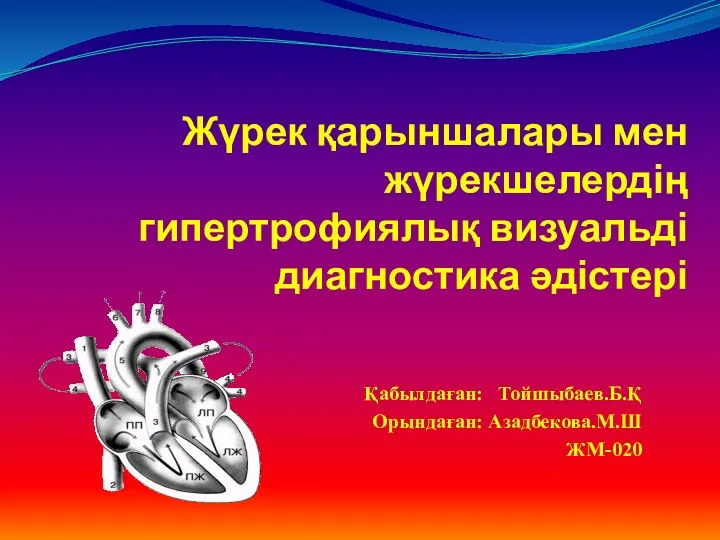 Жүрек қарыншалары мен жүрекшелердің гипертрофиялық визуальді диагностика әдістері
Жүрек қарыншалары мен жүрекшелердің гипертрофиялық визуальді диагностика әдістері