Содержание
- 2. 61 SPINAL CORD DISEASES: The spinal cord consists of that portion of the nervous system that
- 3. 62 Differential Diagnosis for Paraparesis/ Paraplegia: D: Degenerative Disk Disease, Degenerative Myelopathy, Lumbosacral stenosis Neoplastic (extradural,
- 4. 63 With age, the nucleus pulposus may undergo either 1. chondroid metaplasia or 2. fibrinoid metaplasia.
- 5. 64 access to disk material in the spinal canal and usually results in adequate decompression of
- 6. 65 most cases, the lesions are progressive, resulting in gradual deterioration of neurologic function over time.
- 7. 66 paresthesias (unpleasant sensations). Milder cases may be difficult to distinguish from hip dysplasia or other
- 8. 67 DX: Degenerative myelopathy is suspected in any older large–breed dog with chronic, progressive paraparesis. Unfortunately,
- 9. 68 DX: Ventral compartment spinal abnormalities are readily apparent on survey radiographs. Since most are not
- 10. 69 DX: Spinal cord malformations are not visible with conventional radiographic procedures. Computerized tomography or Magnetic
- 11. 70 PX: Growth stops spontaneously when normal bone growth ceases. Rarely, the lesion may later become
- 12. 71 AA: CBC = + neutrophilic leukocytosis Urinalysis = + bacteria, WBC Blood culture = +
- 13. 72 clinical signs, laboratory abnormalities, and response to steroids suggest that all are variants of the
- 14. 73 cells and supporting glia are evident by four hours. Over the course of days, these
- 15. 74 for acute type 1 disc disease apply to spinal trauma. The absence of deep pain
- 17. Скачать презентацию
61
SPINAL CORD DISEASES:
The spinal cord consists of that portion of the
61
SPINAL CORD DISEASES:
The spinal cord consists of that portion of the
LUMBOSACRAL SIGNS
Injury to spinal cord segments L4–S3 damages the LMNs to the pelvic limbs and results in weakness or paralysis of the pelvic limbs, diminished or absent spinal reflexes, and rapid muscle atrophy. Thoracic limb function is normal since both the LMNs and UMNs controlling their movement are unaffected.
THORACOLUMBAR SIGNS
Injury to spinal cord segments T2–L3 damages the UMN tracts to the rear limbs. These animals may also exhibit weakness or paralysis in the pelvic limbs, but spinal reflexes are exaggerated and abnormal reflexes such as crossed extensor and babinski reflexes are seen. Thoracic limb function is again usually normal.
CERVICOTHORACIC SIGNS:
Injury to spinal cord segments C6–T2 damages the LMNs to the thoracic limbs resulting in weakness or paralysis of these limbs, rapid muscle atrophy and diminished or absent reflexes. Most of these injuries will affect UMN axons to the pelvic limbs as well, causing pelvic limb weakness or paralysis, exaggerated and occasionally abnormal reflexes in the pelvic limbs. Clinical signs of Horner’s syndrome (miosis, ptosis and enophthalmus) may also be seen with cervicothoracic signs because the cell bodies of the first order neuron for sympathetic innervation to the head is located in the spinal cord grey matter at T1–2.
These sympathetic neurons exit the spinal canal with the ventral roots before forming the vagosympathetic trunk.
CERVICAL SIGNS:
Injury to spinal cord segments C1–C6 damages the UMN axons that regulate movement in all 4 limbs. Clinical signs associated with injury in this region include paresis or paralysis of all four limbs, exaggerated reflexes and abnormal reflexes in all four limbs.
Respiratory compromise may be produced by damage to the phrenic nerve located between C5–C7, and respiratory paralysis can result from severe cervical lesions that destroy UMNs that coordinate intercostal muscle movement.
The next 4 lectures will concentrate on diseases that affect the spinal cord. Note that many diseases can affect all 4 areas of the spinal cord. Clinical signs of paraparesis or quadriparesis vary with location rather than disease. Therefore, all spinal cord diseases will be discussed together. Tables outlining differential diagnosis for different clinical problems follow.
Differential Diagnosis for UMN Quadriparesis/Quadriplegia
D: Intervertebral disk disease; Cervical vertebral stenosis (malformation/malarticulation; wobblers);
A: Congenital vertebral anomalies (hemivertebrae, block vertebrae, butterfly vertebrae - rare); atlantoaxial subluxation; multiple cartilaginous exostosis
M:
N: Hypervitaminosis A in cats
N: Extradural; Intradural/extramedullary; or Intramedullary tumors
I: Diskospondylitis; Canine distemper myelitis; Feline infectious peritonitis myelitis; feline polioencephalomyelitis
I: Granulomatous meningoencephalomyelitis/reticulosis T: Cervical vertebral fractures/subluxations
T:
V: Fibrocartilaginous infarct P:
62
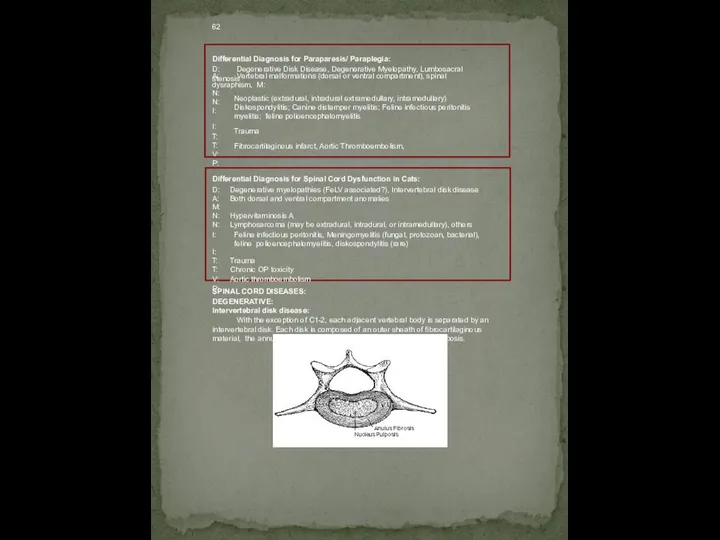
Differential Diagnosis for Paraparesis/ Paraplegia:
D: Degenerative Disk Disease, Degenerative Myelopathy, Lumbosacral stenosis
Neoplastic
62
Differential Diagnosis for Paraparesis/ Paraplegia:
D: Degenerative Disk Disease, Degenerative Myelopathy, Lumbosacral stenosis
Neoplastic
Trauma
Fibrocartilaginous infarct, Aortic Thromboembolism,
A: Vertebral malformations (dorsal or ventral compartment), spinal dysraphism, M:
N:
N:
I:
I:
T:
T:
V:
P:
Differential Diagnosis for Spinal Cord Dysfunction in Cats:
D: Degenerative myelopathies (FeLV associated?), Intervertebral disk disease A: Both dorsal and ventral compartment anomalies
M:
N: Hypervitaminosis A
N: Lymphosarcoma (may be extradural, intradural, or intramedullary), others
I: Feline infectious peritonitis, Meningomyelitis (fungal, protozoan, bacterial), feline polioencephalomyelitis, diskospondylitis (rare)
I:
T: Trauma
T: Chronic OP toxicity
V: Aortic thromboembolism P:
SPINAL CORD DISEASES:
DEGENERATIVE:
Intervertebral disk disease:
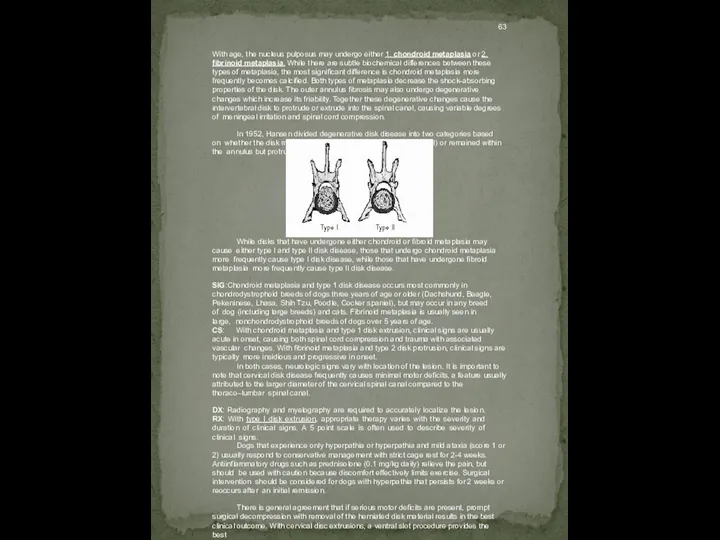
With the exception of C1-2, each adjacent vertebral body is separated by an intervertebral disk. Each disk is composed of an outer sheath of fibrocartilaginous material, the annulus fibrosis, and a gelatinous center, the nucleus pulposis.
63
With age, the nucleus pulposus may undergo either 1. chondroid metaplasia
63
With age, the nucleus pulposus may undergo either 1. chondroid metaplasia
In 1952, Hansen divided degenerative disk disease into two categories based on whether the disk material was extruded from the annulus (type I) or remained within the annulus but protruded dorsally into the spinal canal (type II).
While disks that have undergone either chondroid or fibroid metaplasia may cause either type I and type II disk disease, those that undergo chondroid metaplasia more frequently cause type I disk disease, while those that have undergone fibroid metaplasia more frequently cause type II disk disease.
SIG:Chondroid metaplasia and type 1 disk disease occurs most commonly in chondrodystrophoid breeds of dogs three years of age or older (Dachshund, Beagle, Pekeninese, Lhasa, Shih Tzu, Poodle, Cocker spaniel), but may occur in any breed of dog (including large breeds) and cats. Fibrinoid metaplasia is usually seen in large, nonchondrodystrophoid breeds of dogs over 5 years of age.
CS: With chondroid metaplasia and type 1 disk extrusion, clinical signs are usually acute in onset, causing both spinal cord compression and trauma with associated vascular changes. With fibrinoid metaplasia and type 2 disk protrusion, clinical signs are typically more insidious and progressive in onset.
In both cases, neurologic signs vary with location of the lesion. It is important to note that cervical disk disease frequently causes minimal motor deficits, a feature usually attributed to the larger diameter of the cervical spinal canal compared to the thoraco–lumbar spinal canal.
DX: Radiography and myelography are required to accurately localize the lesion. RX: With type I disk extrusion, appropriate therapy varies with the severity and duration of clinical signs. A 5 point scale is often used to describe severity of clinical signs.
Dogs that experience only hyperpathia or hyperpathia and mild ataxia (score 1 or
2) usually respond to conservative management with strict cage rest for 2-4 weeks. Antiinflammatory drugs such as prednisolone (0.1 mg/kg daily) relieve the pain, but should be used with caution because discomfort effectively limits exercise. Surgical intervention should be considered for dogs with hyperpathia that persists for 2 weeks or reoccurs after an initial remission.
There is general agreement that if serious motor deficits are present, prompt surgical decompression with removal of the herniated disk material results in the best clinical outcome. With cervical disc extrusions, a ventral slot procedure provides the best
64
access to disk material in the spinal canal and usually results
64
access to disk material in the spinal canal and usually results
With type II disk protrusion, medical management with corticosteroids may result in temporary improvement. However, surgical decompression, preferably with removal of the protruding mass, is the only definitive treatment. Some neurosurgeons report worsening of clinical signs after release of chronic spinal cord compression. Regardless of whether clinical signs worsen or remain the same, chronic spinal cord compression does not respond to surgery as readily as acute spinal cord compression and warrants a more guarded prognosis.
PX: Recovery rates of 80-96% have been reported for dogs with type I disk diseases that are treated appropriately. Once deep pain appreciation is lost, the prognosis quickly declines. Recovery rates of 56% are reported for those patients that have lost deep pain but are surgically decompressed within 12 hours of developing clinical signs. This success rate drops to less than 5% if surgery is delayed for 48 hours.
Cervical Vertebral Stenosis (malformation/malarticulation; spondylomyelopathy; caudal cervical vertebral instability; spondylolesthesis; Wobbler syndrome):
This is a syndrome characterized by chronic progressive spinal cord compression secondary to one or more of the following:
type II disk protrusion
hypertrophy of the dorsal longitudinal ligament
hypertrophy of the ligamentum flavum
vertebral malformation
proliferation of articular facets
vertebral instability with subluxation
Although the exact cause is unknown, genetic, environmental, degenerative and nutritional imbalances are all possible contributing factors. The caudal cervical vertebrae (C5, C6, C7) are most commonly affected in Doberman pinchers and Great danes.
Basset hounds are most commonly affected at C2, C3 or C4.
SIG: Older Dobermans (3-9 years of age), young danes (less than 2 years); other large breeds occasionally.
NE: Pelvic limb ataxia and cervical pain are the most striking clinical signs. Extensor rigidity of the thoracic limbs and eventually quadriparesis occurs later in the course of the disease.
AA: EMG – mild denervation of cervical paraspinal muscles and shoulder muscles;
Survey radiographs - may be normal or may show narrowing of affected disk spaces and spondylosis. Caudal cervical vertebrae often appear to tip upwards so that the cranial edge of the vertebral body impinges on the canal.
Myelogram – is required to identify stenosis and to determine whether the compressive material is dorsal or ventral to the spinal cord.
RX: Medical therapy consisting of anti–inflammatory agents such as prednisolone and restricted neck movement has successfully been used in some patients. However, in
65
most cases, the lesions are progressive, resulting in gradual deterioration of
65
most cases, the lesions are progressive, resulting in gradual deterioration of
Due to the variety of lesions no single therapeutic regime can be recommended for all cases. Instead, treatment must be tailored to address the changes demonstrated in each case. Surgical intervention is indicated if significant compression or instability can be demonstrated radiographically.
Dogs with type II disc protrusion have been successfully treated with ventral decompression. If the compression radiographically appears alleviated by linear traction on the head and neck, fusion of the distracted vertebrae in extension may be of benefit. Fusion may be accomplished by bone wedge held in place with a spinal plate or polymethylmethacrylate bridging cancellous bone screws or steinmann pins. Those cases that have predominantly dorsal compression or bony stenosis of the spinal canal require dorsal decompression. Continuous dorsal laminectomy from C4 to T1 resulted in excellent neurologic recovery in 8 cases with multiple areas of compression.
PX: The prognosis varies with duration and severity of spinal cord compression as well as the type of compression and ability to relieve it surgically. Dogs with relatively recent onset of type II disc protrusion and minimal neurologic deficits respond well to ventral decompressive techniques with or without stabilization. Reported success rates for this type of lesion varies from 66 to 80% (Chambers, Oliver, Bjorling 1986; Ellison, Seim, Clemmons 1988). Incomplete removal of disc material is the most common cause of therapeutic failure in these cases. Decompression techniques are less successful when there are multiple levels of compression, or both dorsal and ventral compression is present. As with any chronic compressive myelopathy, the probability of successful return to function decreases with duration of the compression.
LUMBOSACRAL STENOSIS:
Spinal canal stenosis is defined as any type of narrowing of the spinal canal or intervertebral foramina or both. Like cervical vertebral stenosis, lumbosacral stenosis can be produced by one or more pathologic changes. These include congenital vertebral malformations, type II disc protrusion, hypertrophy/hyperplasia of the interarcuate ligament, proliferation of the articular facets, and subluxation/instability of the lumbosacral junction. Again based on the variety of changes present, this syndrome has acquired a variety of names including lumbosacral instability, lumbosacral malformation/malarticulation, lumbar spinal stenosis, lumbosacral spondylolesthesis, and cauda equina syndrome.
SIG: There appears to be two distinct subtypes of this syndrome, congenital and acquired lumbosacral stenosis. Congenital lumbosacral stenosis is a relatively rare condition that occurs primarily in small to medium–sized dogs. Affected vertebrae characteristically have shortened pedicals (lateral bony wall of the canal), thickened and sclerotic lamina and articular processes. Although the vertebral malformation is congenital, signs do not appear until middle to old age in dogs when additional narrowing of the spinal canal occurs secondary to degenerative disc disease and ligamentous hypertrophy.
Acquired degenerative lumbosacral stenosis appears much more commonly than the congenital form of the disease. This is seen primarily in large–breed dogs Males may be affected more commonly than females and German shepherds may be predisposed. Affected dogs are usually mature adults (median age 6.8 years, range 2–14)
CS: Clinical signs with both forms are usually gradual in onset and progressive. Stenosis of the lumbosacral spinal canal causes compression of L7–coccygeal spinal nerve roots. Therefore, lower motor neuron signs to the tail, perineum and sciatic nerves is expected. Muscle atrophy in caudal thigh and distal limb muscles, paraparesis, tail weakness, urinary and anal sphincter disturbances are common. Clinical signs may be asymmetrical with one limb more severely affected than the other. Nerve root compression also typically causes sensory disturbances that vary from overt pain to
66
paresthesias (unpleasant sensations). Milder cases may be difficult to distinguish from
66
paresthesias (unpleasant sensations). Milder cases may be difficult to distinguish from
DX: Survey radiographs usually show spondylosis at the lumbosacral junction. Occasionally the sacrum appears ventrally displaced relative to the lumbar vertebrae. Both of these changes should be interpreted with caution as they can be seen in normal dogs.
Myelography is rarely of benefit because the subarachnoid space usually does not extend to the lumbosacral junction, however it does rule out lesions rostral to the sixth lumbar vertebrae. Epidurography may outline space occupying mass over the lumbosacral disc space, but these studies may be difficult to interpret without experience. Injection of contrast material into the coccygeal vertebral sinuses (intraosseous venography) is technically difficult and appears to be even less reliable than epidurography. Injection of contrast material into the disc space (discography) has helped highlight elevation of the dorsal annulus fibrosis in some cases. Computed tomography, magnetic resonance imaging and electromyography may enhance the ability to diagnose this condition.
TX: Strict confinement and restricted leash walks either alone or combined with corticosteroids frequently alleviates the pain associated with this condition. However, clinical signs often return. Decompressive laminectomy of the L7–S1 vertebrae has been effective at relieving the compression in most cases. If compression of the spinal nerves by spondylitic bone is suspected, a dorsal laminectomy can be combined with facetectomy or foraminotomy. In cases with instability demonstrated radiographically or visualized during surgery, fusion of the lumbosacral joint may be necessary. This may be accomplished by dorsal approach with fixation of the L7–S1 articular processes to the wing of the ilium or by a ventral approach where a ileal graft is placed in a ventral slot similar to stabilization procedures described in Dobermans with cervical vertebral stenosis.
PX: Prognosis varies with the severity of signs. Dogs with hyperpathia and mild neurologic deficits have a good prognosis following surgery. Dogs with bladder atony and fecal incontinence have a poor prognosis.
DEGENERATIVE MYELOPATHY:
Degenerative myelopathy (or chronic degenerative radiculomyelopathy) is a chronic, progressive, degenerative condition affecting spinal cord white matter tracts and occasionally nerve roots.
SIG: Originally reported in German shepherd dogs, numerous large–breeds of dogs appear susceptible. Most cases begin between 5 and 14 years of age with mild paraparesis and ataxia. The rate of progression is variable, but most animals are paralyzed within 6 months to a year after diagnosis.
CS: Histologically, the disease is characterized by both demyelination, and axonal loss, primarily in the thoracic spinal cord. Both ascending and descending tracts are affected, and lesions are frequently worse on one side of the spinal cord. Therefore, affected animals have asymmetric postural reaction deficits in the pelvic limbs with exaggerated rear limb reflexes and no evidence of thoracolumbar hyperpathia.
Degenerative changes have been reported in dorsal nerve roots of dogs in the United Kingdom. The incidence of this change appears to be relatively low in the United States with less than 10% of cases having evidence of lower motor dysfunction in the pelvic limbs.
67
DX: Degenerative myelopathy is suspected in any older large–breed dog with chronic,
67
DX: Degenerative myelopathy is suspected in any older large–breed dog with chronic,
TX: There is no current therapy that will resolve the histologic changes associated with degenerative myelopathy. An antiprotease agent, e–aminocaproic acid (Amicar, Lederle), may slow the progression of the disease. Recommended dosage is 500 mg, PO, TID. Since the course of the disease is variable, it is difficult to verify the efficacy of this treatment. Side effects appear limited to gastrointestinal disturbances in a relative small percentage of dogs and so the only draw–back of e–aminocaproic acid therapy is cost which may exceed $100.00 per month. Unfortunately, there are no other treatment options for this incapacitating disease.
CONGENITAL SPINAL CORD AND VERTEBRAL ABNORMALITIES:
Vertebral and spinal cord abnormalities may be divided into two categories based largely on embryological origins of the tissues 1. VENTRAL COMPARTMENT and 2. DORSAL COMPARTMENT. The ventral compartment consists of vertebral body and intervertebral disk. The dorsal compartment consists of vertebral arch and spinal cord itself. These divisions are useful because when multiple abnormalities occur, they usually occur within the same compartment. That is, abnormal development of the vertebral dorsal arch is frequently associated with abnormal spinal cord development. However, the spinal cord is usually normal with ventral compartment abnormalities unless the vertebrae are sufficiently misshapen to cause secondary spinal cord compression.
Disorders associated with Ventral Compartment Malformations: Hemivertebrae, Block vertebrae, Butterfly vertebrae:
Block vertebrae appear radiographically as fusion of two vertebrae. This may involve the vertebral bodies, the vertebral arches, or the entire vertebrae. The sacrum is a form of block vertebrae.
Butterfly vertebrae (cleft vertebrae) appear radiographically as a dorsal–ventral cleft in the vertebral body that results from incomplete fusion of the right and left halves of the vertebral bodies. On a dorsal–ventral radiograph, the cranial and caudal vertebral endplates have a v shape, giving the overall appearance of a butterfly.
Hemivertebrae are shortened, wedge shaped vertebrae, that frequently result in significant curvature of the spine in either a dorsal (kyphosis), ventral (lordosis) or lateral (scoliosis) plane. They result from incomplete development of vertebral bodies either from displacement of left and right somatic halves, or from incomplete formation of the adjacent half (Done et al, 1975).
SIG: Ventral compartment abnormalities are relatively common in brachycephalic breeds selectively bred for "screw–tailed" conformation (i.e. English bulldogs, Boston terriers, Pugs). Multiple coccygeal hemivertebrae is responsible for the kinked tail in these breeds. Hemivertebrae also occur in German short–haired pointers as an autosomal recessive disorder (Kramer et al, 1982).
CS: All ventral compartment abnormalities are usually incidental findings. Only rarely do they compromise stability or result in sufficient spinal angulation to cause spinal cord compression. When this occurs, gradual, progressive deterioration in spinal cord function results in para or quadriparesis.
68
DX: Ventral compartment spinal abnormalities are readily apparent on survey radiographs. Since
68
DX: Ventral compartment spinal abnormalities are readily apparent on survey radiographs. Since
TX: Spinal cord compression may be alleviated by surgical decompression with stabilization if necessary. While concurrent dorsal compartment abnormalities are rare, several cases have been reported. Therefore, all cases should have a guarded prognosis.
Disorders that result from Dorsal Compartment Malformations: Spina Bifida and Spinal Dysraphism:
Spina Bifida:
Spina bifida refers to the condition where the vertebral arches fail to fuse resulting in a bony defect in the dorsal portions or the vertebrae. Spina bifida may occur alone (spina bifida occulta) or a portion of the meninges (spina bifida cystica) or spinal cord (spina bifida manifesta) may protrude through the defect. Any open dysraphic disorder that results in potential communication between the nervous system and the environment may be referred to as spina bifida aperta.
SIG: There is a relatively high incidence of spina bifida in bulldogs and manx cats. This is again, likely related to genetic selection for kinked or absent tails in these breeds.
Tetratogens and nutritional deficiencies may be responsible for the sporadic incidence of spina bifida in other breeds (Bailey and Morgan 1992).
CS: vary with both the location and severity of the anomaly. Spina bifida occulta usually produced no neurologic deficits while spina bifida aperta may present as open regions of the spinal canal, frequently draining cerebrospinal fluid. Less severe lesions may result in palpable depressions of the vertebral canal often with whorls of misdirected hair growth.
DX: Survey radiographs usually demonstrate vertebral arch deficits. Myelography is often necessary to outline any associated neural or meningeal abnormalities.
PX: Surgical correction of the existing defect may be possible in selected cases. Unfortunately, there are frequently other neural deficits that may not be radiographically apparent. Therefore, the prognosis in all cases with dorsal compartment malformations should be guarded to grave.
Spinal Dysraphism:
Spinal dysraphism correctly refers to the spinal cord defect that results from failure of fusion of the neural tube. This creates a dorsal sagittal defect in the spinal cord. In many clinical cases, this term has been loosely applied to any developmental defect of the spinal cord itself.
SIG: Weimeraner dogs develop an inherited myelodysplasia commonly referred to as spinal dysraphism. Abnormal migration of cells in the developing lumbosacral spinal cord result in disorganization of the normal cytoarchitecture In weimeraners, the disease is inherited as a co–dominant gene with variable expressivity.
CS: There is some variation in the degree of spinal cord disorganization in these animals. This is reflected in different degrees of paraparesis. Typical clinical signs include a symmetrical hopping gait, hindlimb abduction, and slow postural reactions in the pelvic limbs. Withdrawal reflex typically produces flexion of both pelvic limbs. Other associated physical defects includes misshapen thorax, disproportion in length of the extremities and body, kinking of the tail, and abnormal hair patterns along the dorsal trunk.
69
DX: Spinal cord malformations are not visible with conventional radiographic procedures. Computerized
69
DX: Spinal cord malformations are not visible with conventional radiographic procedures. Computerized
PX/TX: No treatment is available for intrinsic spinal cord malformations. Clinical signs rarely progress beyond a few months of life. Therefore, prognosis varies with the severity of deficits.
Disorders that result from abnormalities in chondrification or ossification of developing vertebrae. Vertebral Malformations:
Atlanto–Axial Subluxation:
The articulation between first two cervical vertebrae differs from the rest of the spinal cord. There is no intervertebral disk. Instead, the vertebrae are joined by a series of ligaments, most of which attach a prominent rostral projection from the body of C2, the dens, to either the occipital bone (apical ligament and paired alar ligaments) or C1 (transverse ligament of the atlas). Malformation of the dens results in instability between the first two cervical vertebrae and subsequent subluxation.
SIG: The actual incidence is unknown, but congenital absence of the dens occurs most commonly in miniature and toy breeds of dogs. Abnormal angulation of the dens has been reported in two dogs and absence of the transverse ligament of the atlas has been reported in one dog. With few exceptions, dogs are usually less than one year of age when initially presented
CS: Malformation or absence of the dens results in instability between the atlas and axis. Subsequent vertebral subluxation results in compression of the cervical spinal cord. Clinical signs vary from intermittent pain to complete transection of the cervical spinal cord and death.
DX: Abnormal conformation of the dens may be seen on survey radiographs. This is best visualized on ventrodorsal views or oblique lateral views. A greater than normal distance between the vertebral arch of C1 and C2 may be apparent on lateral views.
Extreme caution should be exercised when anesthetizing and positioning these patients for radiographs to prevent further spinal cord trauma. DO NOT FLEX THE NECK IN THESE PATIENTS.
TX: Animals with acute exacerbation of clinical signs should be treated for spinal trauma. Several techniques have been described to stabilize the atlanto–axial joint. External support may be beneficial during the initial phases of recovery, especially when severe spinal trauma has occurred. Surgical stabilization may be accomplished through either a dorsal or ventral approach.
Multiple Cartilaginous Exostoses (Osteochondromatosis):
Exuberant (benign) proliferation of cartilage in epiphyseal regions has been reported in dogs and cats. All bones formed by endochondral ossification may be affected and multiple lesions develop in most cases. Clinical signs of spinal cord compression result from extension of the exostoses into the spinal canal.
SIG: Young (<1 year of age) dogs and cats. No breed or sex predisposition.
NE: Progressive transverse myelopathy anywhere along the spinal canal. Neurologic deficits are often asymmetric.
DX: radiographs and myelography
TX: surgical excision of exostoses
70
PX: Growth stops spontaneously when normal bone growth ceases. Rarely, the lesion
70
PX: Growth stops spontaneously when normal bone growth ceases. Rarely, the lesion
NUTRITIONAL:
Hypervitaminosis A of Cats:
Chronic excess of vitamin A in the diet of cats fed large amounts of liver results in vertebral exostosis. Lesions are most severe in the cervical and thoracic spine. Compression of the spinal nerve roots occurs if the new bone growth extends into the intervertebral foramina.
SIG: Cats of all ages
NE: cervical pain, rigidity, thoracic limb lameness, ataxia.
DX: radiographs and diet history
RX: change diet prevents further exostosis
PX: cats are usually resistant to dietary changes
NEOPLASTIC:
The spinal cord may be affected by several different neoplastic processes. For simplicity, these are best divided into extradural; intradural/ extramedullary; and intramedullary.
Extradural: These tumors develop outside the dura and include vertebral tumors and metastatic soft tissue tumors. Lymphosarcoma is the most common metastatic tumor and can cause meningeal, nerve root, or spinal cord infiltration or extradural mass lesions.
Osteosarcomas, fibrosarcomas, multiple myelomas, adenocarcinomas, and chondrosarcomas of the vertebrae may cause spinal cord compression resulting in spinal cord pain to paralysis. Radiographs may identify bony lysis, however myelography is frequently necessary to outline spinal cord compression. Long term prognosis is poor for all types of spinal cord neoplasia.
Intradural/ Extramedullary: These tumors develop inside the dura, but outside the spinal cord itself. Meningiomas and nerve root tumors are the most common. Usually, these cases present with chronic progressive lameness and pain. Myelography is necessary to outline the mass. Surgical removal is beneficial. Unfortunately, many cases reoccur, probably due to incomplete removal of all neoplastic cells.
Intramedullary: These tumors develop within the spinal cord parenchyma. Astrocytomas, ependymomas and gliomas can affect any age dog or cat. Boxers and Boston terriers are most commonly affected. Pain is usually absent in these cases (as opposed to extradural or intradural/extramedullary tumors where pain is a prominent feature). Myelography is necessary to outline the mass. Prognosis is poor because the tumor can not be removed.
INFECTIOUS/ INFLAMMATORY DISEASES OF VERTEBRAE:
Diskospondylitis:
Infection of the intervertebral disk with concurrent osteomyelitis of contiguous vertebrae. Concurrent cystitis or bacteremia may be present and the diskospondylitis often occurs secondarily to one of these primary foci of infection. Staphylococcus intermedius (coagulase positive staph) is most frequently isolated. Others: Brucella canis, Streptococcus. Fungal infections and migration of foreign bodies may also cause diskospondylitis.
SIG: Usually adult, large breeds of dogs are affected. Males are affected twice as often as females.
CC: CS are variable. Stiff gait, pain, hyperesthesia, are the most common clinical signs. Neurologic deficits may develop later either due to spinal cord compression by inflammatory tissue, or extension of the infection into the spinal canal.
PE: + systemic signs e.g., fever, anorexia, depression, heart murmur, orchitis, epididymitis
71
AA: CBC = + neutrophilic leukocytosis
Urinalysis = + bacteria, WBC Blood culture
71
AA: CBC = + neutrophilic leukocytosis
Urinalysis = + bacteria, WBC Blood culture
Brucellosis test = + positive tube agglutination CSF = + increased protein and cells
EMG = changes in paraspinal muscles at site of lesion(s)
Radiographs = Lysis of adjacent vertebral end–plates with varying degrees of bone production. Severely destructive lesions may cause vertebral luxation and spinal cord compression resulting in paraplegia or quadriplegia. Occasionally radiographic lesions aren't detected in early cases. In some cases there are multiple affected areas of the vertebral column.
RX: Appropriate antibiotics in cases of bacterial etiology. If bacteria can't be isolated, Tribrissen or Cephalosporin for 4–6 wks is a good choice. Vertebral decompression and stabilization is occasionally done if cord compression or vertebral instability is present.
PX: Good with all bacterial etiologies except Brucella (difficult to resolve). Poor with fungal etiologies.
INFECTIOUS/INFLAMMATORY DISEASES OF THE SPINAL CORD AND MENINGES:
Meningitis and myelitis refer to inflammation of the meninges and spinal cord respectively. Meningomyelitis is the most appropriate term when the two occur together. Inflammation of the nervous system can occur secondary to both infectious and non–infectious etiologies.
Infectious causes of Meningomyelitis:
Reported infectious causes of Meningomyelitis are include viral, fungal, protozoan, and bacterial causes. Most of these organisms cause multifocal neurologic disease and are discussed in more detail in other lectures. Occasionally these agents can localize to the spinal cord and meninges causing para or quadriparesis as the presenting complaint. The predominant signs of viral, protozoal, and parasitic diseases are of parenchymal involvement. Rickettsial and fungal diseases may display parenchymal as well as meningeal signs. Bacterial diseases most commonly present with meningeal signs with secondary spread to the spinal cord parenchyma.
Non–infectious causes of Meningomyelitis:
Two diseases considered with encephalitis, canine granulomatous Meningomyelitis and feline polioencephalomyelitis can initially present with signs of meningitis or myelitis. Both of these diseases are discussed in detail with behavioral diseases. Another disease, steroid responsive meningitis, typically presents with neurologic signs localized to the meninges and spinal cord.
Steroid Responsive Meningitis
There have been several reports of dogs with clinical and laboratory data consistent with a suppurative meningitis for which an infectious cause can not be identified. Antimicrobial therapy has not been effective, but most dogs respond to corticosteroids. The first report of an aseptic, suppurative meningitis appeared in the literature in 1978 and numerous cases have appeared subsequently. It is difficult to prove whether this reflects an increased incidence or only increased awareness of this syndrome, but clinical impression indicates the disease is gaining in frequency.
SIG: Initial reports described breed specific syndromes in Beagles, Pointers , and Bernese mountain dogs. More recently, a number of cases were reported in other large–breeds of dogs as well as mixed breed dogs over 40lbs in weight. Similarities in
72
clinical signs, laboratory abnormalities, and response to steroids suggest that all
72
clinical signs, laboratory abnormalities, and response to steroids suggest that all
CS: Cervical pain is the most consistent clinical sign. Most dogs also were febrile, and were lethargic and anorexic. No or only mild neurologic deficits have been reported in most affected dogs. The exception is Bernese mountain dogs and Pointers that have a more intense inflammatory reaction resulting in myelitis and cranial nerve deficits. A spontaneously waxing and waning course early in the disease has been reported in some dogs.
DX: Clinical pathology abnormalities are confined to CBC and CSF analysis. Leukocytosis, occasionally with a non–regenerative anemia has been reported in peripheral blood. Cerebrospinal fluid typically has a marked leukocytosis (100 to over 10,000 cells per mm3) with non–degenerate neutrophils predominating. Absence of an identifiable organism, unresponsiveness to antibiotics, and rapid response to steroids all support an immune–mediated pathogenesis. Occasional cases have non–erosive polyarthritis, but other evidence of a systemic immune–mediated disease process has not been reported. Most cases are ANA negative. All of the dogs in a recent series had been vaccinated with a multivalent modified–live virus vaccine within 9 months of the onset of clinical signs. While an association was suggested, it is difficult to prove because most young dogs that receive extensive veterinary care have been recently vaccinated. A genetic predisposition has been suggested for Beagles.
TX: Prednisolone (2–4 mg/kg/day ) results in rapid resolution of signs of meningitis. Neurologic deficits should improve or resolve depending on severity over the following weeks. The treatment regime can usually be slowly tapered to alternate day therapy and then discontinued after 2–6 months. Clinical signs can recur if steroids are withdrawn too rapidly. Readministration of prednisolone and more gradual tapering is usually successful in these cases.
PX: There is insufficient numbers of pointers and Bernese mountain dogs reported to accurately predict the outcome in these breeds. A high incidence of relapse has been reported in Beagles after steroid withdrawal which resulted in euthanasia. Complete resolution of clinical signs has been reported in other cases.
SPINAL CORD TRAUMA:
Spinal trauma occurs with any rapid deformation of the spinal cord. This is commonly associated with external trauma such as automobile accidents, falls, fights with other animals. However, other causes of spinal cord deformation such as intervertebral disc extrusion or luxation due to congenital vertebral instability also cause significant spinal cord trauma.
With any traumatic event, there is an immediate effect of the mechanical forces acting on the spinal cord. This immediate effect is commonly referred to as the primary injury.
Clearly, primary injury may vary in severity to mild contusion to complete severance of the spinal cord. There is now extensive evidence that the primary injury initiates a series of biochemical events that result in additional neurologic injury referred to as secondary or delayed injury . Using experimental models, a sequence of both histologic and biologic events have been identified that occur at specific intervals after trauma. Petechial hemorrhage, primarily in the gray matter develops immediately after trauma. Within 30 minutes attenuation of myelin in the surrounding white matter and enlargement of the periaxonal space develops. By two hours, these changes have progressed to gray matter necrosis and edema of the white matter. Chromatolysis and vacuolation of nerve
73
cells and supporting glia are evident by four hours. Over the
73
cells and supporting glia are evident by four hours. Over the
While the exact mechanism of secondary spinal cord trauma is not know with certainty, experimental evidence has accumulated to support the roles of endogenous opiods and excitatory amino acids released after injury as well as eicosanoids and leukotrines, compounds generated from the byproducts of cellular membrane damage. All of these changes stimulate the generation of unstable free radicals, which in turn cause further membrane damage and perpetuate the cycle.
SIG: Spinal trauma occurs in all ages and breeds of domestic animals.
CS: The clinical signs exhibited by the animal vary with location of the trauma. With severe injury to the thoraco–lumbar spinal cord, a clinical syndrome characterized by flaccid paralysis of the rear limbs and involuntary extension of the thoracic limbs and neck may be seen. Postural reactions are intact in the front limbs despite their apparent rigidity. The term Schiff–Sherrington syndrome has been applied to these clinical signs. They result from loss of inhibitory interneurons in the spinal cord that normally limit extensor tonus in the thoracic limbs and persist for 10 to 14 days after the injury. The presence of Schiff–Sherrington syndrome indicates severe but not irreversible injury to the spinal cord.
DX: Spinal cord trauma should be suspected in any animal with acute, rapidly progressive para/quadriparesis or paralysis. Spinal cord trauma occurs with a wide variety of insults. Vertebral fractures and luxations should be considered in all animals with external evidence of trauma. These animals should be immobilized on a stretcher or other rigid surface while the full extent of their injuries are evaluated. Neurologic examination should be restricted to assessment of consciousness, cranial and spinal nerves until a fracture can be ruled out radiographically. In most cases, survey radiographs are sufficient to rule out fractures and displacement of the vertebral segments. Concussive injuries including traumatic disc herniations can occur without obvious vertebral trauma. Myelography is necessary to fully evaluate the extent of these injuries.
TX: Spinal trauma is a biphasic phenomenon. Therefore, treatment should be directed at correcting the primary event and preventing any further mechanical trauma, as well as mitigating the effects of secondary spinal trauma.
A number of clinical trials have been conducted to evaluate specific antagonists for each of the punitive chemical mediators of secondary neural trauma. The only compound that has been consistently useful is methylprednisolone sodium succinate.
Methylprednisolone is a potent antioxidant, that inhibits free radical induced membrane injury. It also inhibits the formation of eicosanoids and leukotrines, and may directly support cellular energy metabolism while it inhibits vasospasm.
Methylprednisolone should be administered at 30 mg/kg IV as soon as possible after the injury. Higher and lower doses are not as efficacious. The half–life of methylprednisolone is cat spinal tissue is only 2–6 hours, therefore repeat doses are necessary. Current recommendations are to administer repeat injections of 15 mg/kg IV 2 hrs and 6 hours after the initial dose, followed by a constant infusion of 2.4 mg/kg/hour for the next 42 hours.
High doses of methylprednisolone have been associated with increased wound contamination in human patients. This together with other undesirable characteristics of corticosteroids, has prompted the development of nonglucocorticoid 21–aminosteroid compounds that have similar antioxidant properties as methylprednisolone. One of these, U74006F (trilazad mesylate) has shown promise in experimental studies, and is currently undergoing clinical trials.
PX: The prognosis varies with severity of the injury, and the ability to prevent further injury if significant vertebral instability is present. In general, the same guideline described
74
for acute type 1 disc disease apply to spinal trauma. The
74
for acute type 1 disc disease apply to spinal trauma. The
VASCULAR:
Fibrocartilaginous Infarct:
Material similar to the nucleus pulposus enters the arterial and/or venous blood supply to the spinal cord at any level and causes ischemic or hemorrhagic necrosis of cord tissue. Onset is acute and signs progress over few hours to 1 or 2 days. Signs are usually asymmetrical and the animal isn't painful (spinal cord has no pain fibers). Underlying cause and the exact origin of the emboli are unknown (it is not associated with herniated discs).
SIG: Any age/ breed. Most frequently adults esp Schnauzers, Great Danes, Labs, St. Bernards.
CC: Acute quadriplegia, hemiplegia, paraplegia, or monoplegia. One limb may have shown signs first. Dog may have cried out and suddenly developed signs.
NE: Signs vary with the location. Example: If caudal cervical area became ischemic the most involved side would show flaccid paralysis of thoracic limb and spastic paralysis of ipsilateral pelvic limb. The contralateral limbs would be more functional. Pain perception may or may not be present in the most involved thoracic limb. Horner's syndrome may be seen on the most involved side.
AA: EMG = may indicate focal cervical lesion but can't be evaluated until 5 days post onset.
CSF = usually has increased protein with normal or very slightly elevated cell count. Xanthochromia may be present.
Radiographs = normal.
Myelogram = normal or diffuse swelling of cord in the acute stage.
RX: Corticosteroids. Time.
PX: Varies with location of lesion. If LMN signs are present prognosis isn't as good as for UMN signs. If no deep pain present after 24–48 hours, prognosis for return of function of limb(s) is poor. The most involved limb is usually the last one to improve/recover.
Some animals may never regain complete function.
PATH: Ischemic or hemorrhagic necrosis of cord with fibrocartilage in spinal arteries and veins.
 Девиантное поведение. Устойчивое поведение личности, отклоняющееся от общепринятых, наиболее распространённых
Девиантное поведение. Устойчивое поведение личности, отклоняющееся от общепринятых, наиболее распространённых Современные методы исследования пищеварительного тракта
Современные методы исследования пищеварительного тракта Личная гигиена тяжелобольного пациента
Личная гигиена тяжелобольного пациента Цели и задачи ухода за больными детьми
Цели и задачи ухода за больными детьми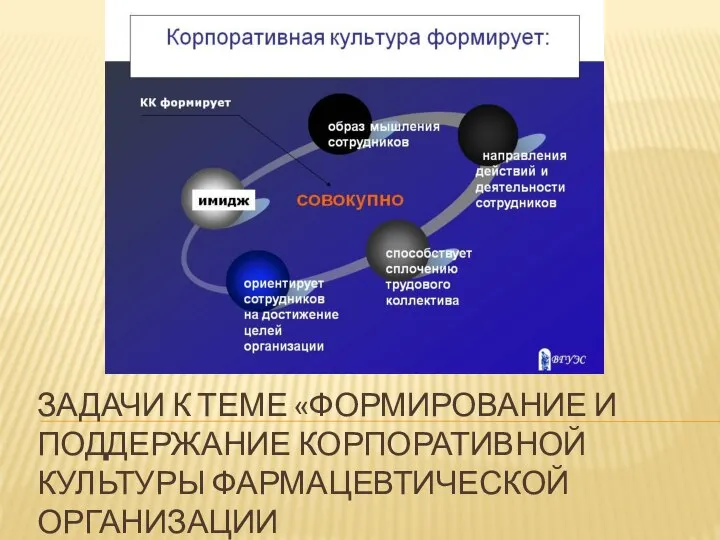 Формирование и поддержание корпоративной культуры фармацевтической организации
Формирование и поддержание корпоративной культуры фармацевтической организации Костная онкология
Костная онкология Паренхиматозды мүшелердің жабық жарақаты
Паренхиматозды мүшелердің жабық жарақаты Гормондық заттардың жіктелуі. Гормондармен емдеудің принциптері. Гипо-, гипертиреозда қолданылатын препараттар
Гормондық заттардың жіктелуі. Гормондармен емдеудің принциптері. Гипо-, гипертиреозда қолданылатын препараттар Организация ухода за больными гастроэнтерологического профиля
Организация ухода за больными гастроэнтерологического профиля Консультирование бесплодной пары
Консультирование бесплодной пары Роль пожилого и старческого возраста в развитии патологии
Роль пожилого и старческого возраста в развитии патологии CAD/CAM система в ортопедической стоматологии
CAD/CAM система в ортопедической стоматологии Состав грудного молока
Состав грудного молока Проксемика – это пространственное расположение и ориентация партнеров по общению, дистанция между ними
Проксемика – это пространственное расположение и ориентация партнеров по общению, дистанция между ними Отёк Рейнке - причины, диагностика, подходы к лечению
Отёк Рейнке - причины, диагностика, подходы к лечению ИБС. Стенокардия. Инфаркт миокарда
ИБС. Стенокардия. Инфаркт миокарда Энурез. Эпидемиология
Энурез. Эпидемиология Основы рационального питания. Ожирение. Целлюлит
Основы рационального питания. Ожирение. Целлюлит ВМФ-дистанционный
ВМФ-дистанционный Клинико-иммунологические особенности пациентов с хроническим генерализованным пародонтитом
Клинико-иммунологические особенности пациентов с хроническим генерализованным пародонтитом Побочные действия. Антибиотики
Побочные действия. Антибиотики Дыхательная недостаточность
Дыхательная недостаточность Нефротический синдром
Нефротический синдром Диаскинтест. Методы ранней диагностики туберкулеза
Диаскинтест. Методы ранней диагностики туберкулеза Лекарства и беременность
Лекарства и беременность Патологическая анатомия отдельных врождённых пороков сердца
Патологическая анатомия отдельных врождённых пороков сердца Интубация трахеи. Виды, техника, осложнения. Алгоритм трудной интубации
Интубация трахеи. Виды, техника, осложнения. Алгоритм трудной интубации ОРВИ. Этиология, клинические проявления, диагностика. Тактика медицинского работника
ОРВИ. Этиология, клинические проявления, диагностика. Тактика медицинского работника